CASE REPORT
Serviço de Cardiologia - Hospital de Santa Cruz, Centro Hospitalar de Lisboa Ocidental - Lisboa - Portugal
Mailing Address
Keywords: Coronary Occlusion/diagnosis; Takotsubo Cardiomyopathy/diagnosis; Coronary Angiography; Cardiac catheterization; Contrast Media.
Introduction
Hemodynamic instability during coronary angiography is more common in patients with severe coronary disease, particularly in the acute coronary syndrome setting. Rarely, it can occur in an elective context, in the absence of coronary disease, due to inadvertent gas embolism and increased coronary vessel reactivity1,2.
Coronary vasospasm has been implicated as one of the possible pathophysiological mechanisms that are involved in Takotsubo cardiomyopathy (TCM), though a few cases substantiating this association have been described in the literature3.
We hereby present the case of a patient with transient hemodynamic instability with evidence of multivessel vasospasm and findings suggestive of TCM during elective coronary angiography.
Case Report
We present the case of a 70-year-old male patient, a long term smoker with no known risk factors and no cardiovascular history. In May 2004, he was submitted to exercise testing due to fatigue complaints. The exam revealed ST segment changes that were interpreted as silent ischemia. Subsequently, a coronary angiography did not show significant coronary disease, and the patient remained asymptomatic from the cardiovascular point of view.
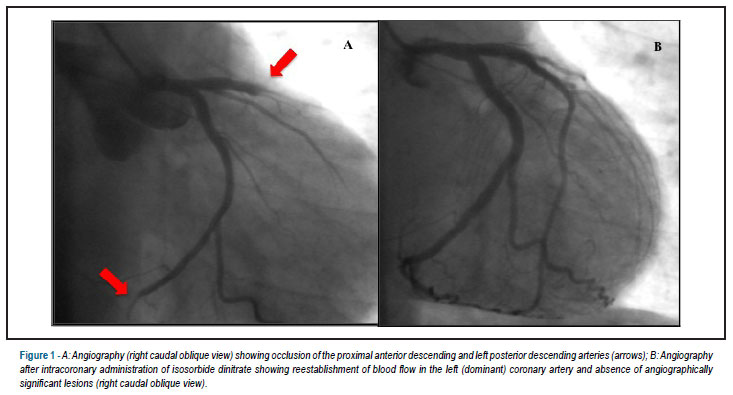
In March 2011, he complained of fatigue on moderate effort again. He was submitted to exercise testing with normal functional capacity (10.7 METs), adequate blood pressure response and ST changes suggesting ischemia: upsloping ST depression at lateral and inferior leads, starting on the second stage and getting back to normal on the first minute of recovery. He was submitted again to coronary angiography as requested by the attending physician. At the first injection in left coronary artery (dominant vessel), slow flow was observed with occlusion of the proximal anterior descending, left posterior descending and distal circumflex arteries (Figure 1A). These findings were followed by increasing chest pain, generalized elevation of the ST segment, progressive bradycardia and pump failure, and atropine and dopamine had to be given.
Due to the possibility of vasospasm and in spite of hemodynamic instability, intracoronary isosorbide dinitrate was given with ST segment normalization and hemodynamic stabilization. The following injections (> 5 minutes after beginning of the symptoms) revealed reestablishment of blood flow in the coronary tree as a whole and no evidence of significant angiography lesions (Figure 1B). Transthoracic echocardiography showed akinesis with apical ballooning (Figures 2A and 2B) e hyperkinesis of the left ventricle (LV) inferior segments. The patient was admitted to the Coronary Unit and remained stable. Lab investigations revealed increased levels of myocardial necrosis biomarkers - troponin I (normal values <0.04 µg/l): 1.29 (< 2 h) - 5.77 (24 h) - 4.89 (36 h) - 0.23 (96 h) µg/L. On the fifth day of hospitalization, an echocardiogram revealed normalization of wall motility and LV systolic function and the patient was discharged (Figures 2C and 2D).
One month later, magnetic resonance imaging showed myocardial edema without evidence of late enhancement or segmental contractility changes (Figures 2D and 2F). On follow-up, after twelve months, the patient is asymptomatic and has not presented any cardiovascular event.
Discussion
TCM is a low frequency entity with estimated prevalence of 0.7-2.5% of the patients with suspected acute coronary syndrome4. It is called Takotsubo syndrome due to the morphologic similarity between the LV aspect during systole at ventriculography and a ceramic object with the same name used as an octopus trap in fishing communities in Japan, where it was originally described. Although all ventricular segments can be affected, the most typical finding is the medioapical akinesis affecting all cardiac walls associated to inferior hyperkinesis. On occasion, the anterior leaflet of the mitral valve can move with systole, and the ejection fraction is reduced in the acute phase5. In approximately 1 to 5% of the cases, hemodynamic instability develops, often requiring the adoption of emergency measures such as intraaortic balloon implantation6.
TCM etiopathology remains to be elucidated and one of the proposed mechanisms is the hyper stimulation of the sympathetic nervous system. This mediating mechanism may justify the association of the condition with stressful situations (cases were reported in association with anxiety, stress, administration of cathecolamines and in patients with pheochromocytoma)7. The fact that the apex and the medium LV segments (specially the anterior wall) are affected is probably related to the greater density of the sympathetic innervation in these areas.
Coronary vasospasm, which can result from sympathetic hyperactivity, is another proposed etiology. Currently, the only known mechanism that can explain the segmental motility changes similar to the ones evidenced in TCM is myocardial stunning, usually related to transient coronary occlusion. This hypothesis can explain the reversibility of contractile changes, the absence of significant damage, the reduced cardiac enzymes release and the rapid recovery of electrocardiographic changes. Multivessel vasospasm may justify changes observed on TCM. The segmental alterations, which do not correlate to the segmental distribution of coronary circulation, may be explained by LV apex spasm involving the terminal portion of the three subsidiary coronary territories. However, it is important to clarify if vasospasm is the "essential phenomenon", leading to transient myocardial hypoxia, or if it occurs in parallel to other mechanisms that, on acting directly on cardiomyocytes, interfere with the electrochemical coupling of the mitochondrias. Though rare, there are documented cases of TCM during diagnostic coronary angiography showing generalized coronary vasospasm8. The exam circumstances themselves may lead to emotional stress and TCM. This condition is probably a model of anxiety somatization with massive neurotransmitter discharge causing vasomotricity disturbance.
Cardiac resonance magnetic imaging allows morphologic evaluation, helps in differential diagnosis and is the gold standard for studying LV function9.
The prognosis for TCM is favorable. Cardiogenic shock and tachyarrhythmia are the most prevalent complications10.
In the case above described, coronary vasospasm was probably the cause of the episode. Although not possible to exclude, gas embolism was not angiographically documented. Acute phase echocardiogram revealed segmental contractility typical of TCM, with subsequent normalization. This finding can indicate that the changes are not specific for this condition or, alternatively, that its pathophysiology can include transient coronary occlusion. Troponin elevation, without evidence of myocardial necrosis on magnetic resonance, is probably related to cytoplasmic troponin pool release, resulting in increased cellular permeability induced by ischemia, eventually following vasospasm, without irreversible myofibril damage.
Coronary angiography is a safe exam, but is not devoid of complications and the indications for its use, even for diagnostic purposes, must be carefully weighted. The absence of pain (similar to the exercise testing previously performed) and the absence of coronary disease on angiography may favor the selection of an alternative test for obstructive disease exclusion, such as computed tomography angiography, which has high negative predictive value.
This presentation of TCM is not widely described in literature3. However, its possibility must be considered when hemodynamic instability develops during coronary angiography in the absence of confirmed coronary disease and other triggering factor.
Author contributions
Conception and design of the research: Dores H, Raposo L; Acquisition of data: Dores H; Analysis and interpretation of the data: Dores H, Raposo L, Ferreira J, Andrade MJ, Almeida M; Critical revision of the manuscript for intellectual content: Raposo L, Ferreira J, Andrade MJ, Almeida M, Mendes M.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any post-graduation program.
References
- 1. Khan M, Schmidt DH, Bajwa T, Shalev Y. Coronary air embolism: incidence, severity and suggested approaches to treatment. Cathet Cardiovasc Diagn.1995;36(4):313-8.
- 2. Lee WL, Chin CS, Lai CJ, Ho HY,Ting CT. Successful resuscitation of patient with massive coronary air embolism occluding two vessels during coronary angiography: a case report. Angiology.2001;52(2):155-9.
- 3. Haghi D M, Suselbeck T, Wolpert C. Severe multivessel coronary vasospasm and left ventricular ballooning syndrome. Circ Cardiovasc Interv.2009;2(3):268-9.
- 4. Nef HN, Mollmann H, Elsasser A. Tako-tsubo cardiomyopathy (apical ballooning). Heart.2007;93(10):1209-15.
- 5. Bybee K, Kara T, Prasad A, Lerman A, Barsness GW, Wright RS, et al.. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med.2004;141(11):858-65.
- 6. Abdulla I, Ward MR. Tako-tsubo cardiomyopathy: how stress can mimic acute coronary occlusion. Med J Aust.2007;187(6):357-60.
- 7. Wittstein IS, Thiemanny DR, Lima JA,Baughman KL, Schulman SP, Gerstenblith G, et al.. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med.2005;352(6):539-48.
- 8. Nojima Y, Kotani J. Global coronary artery spasm caused takotsubo cardiomyopathy. J Am Coll Cardiol.2010;55(9):e17.
- 9. Eitel I, Behrendt F, Schindler K, Gutberlet M, Schuler G, Thiele H. Differential diagnosis of suspected apical ballooning syndrome using contrast enhanced magnetic resonance imaging. Eur Heart J.2008;29(21):2651-9.
- 10. Turley A, Graham R, Hall J. Takotsubo cardiomyopathy in two female patients: two case reports. Cases J.2008;1(1):325.
Apical ballooning syndrome during diagnostic coronary angiography
Publication Dates
-
Publication in this collection
06 May 2013 -
Date of issue
Apr 2013