ABSTRACT
PURPOSE:
To investigate if the association of fat grafts and platelet-rich plasma (PRP) improves graft viability in female rats.
METHODS:
This is an experimental, randomized and blinded study, which involved 47 rats. Fat was harvested from the inguinal region and grafted to the cranial region. The experimental group consisted of PRP-enriched fat grafts (n=22) whilst the control group consisted of fat graft only (n=25). After a 100-day period, the animals were euthanised and the fat grafts were analyzed using scores from 0 (absent) to 4 (abundant), in optical microscopy by two independent and blinded pathologists.
RESULTS:
Regarding fat graft cell viability, the PRP group scored moderate/abundant in 63% of cases and the fat graft only group scored absent/slight in 72% of cases (p=0.03). The PRP group also presented lower fat necrosis scores when compared to the fat graft only group (p=0.03). Tumors (dermoid cysts) within the fat grafts were observed in three animals in which the grafts were mixed with PRP.
CONCLUSION:
Platelet-rich plasma improves the viability and integration of fat grafts in rats, but more studies are needed to fully understand the exact mechanisms that lead to this improvement and assess the safety of the method for use in humans.
Key words:
Adipose Tissue; Graft Survival; Platelet-Rich Plasma; Rats
Introduction
Fat is an ideal, easily available filler because of it's autologous character and low surgical-related morbidity11 Biazus JV, Falcão CC, Parizotto AC, Stumpf CC, Cavalheiro JA, Schuh F, Cericatto R, Zucatto ÂE, Melo MP. Immediate reconstruction with autologous fat transfer following breast-conserving surgery. Breast J. 2015 May-Jun;21(3):268-75. doi: 10.1111/tbj.12397.
https://doi.org/10.1111/tbj.12397....
,22 Coleman SR. Long-term survival of fat transplants: controlled demonstrations. Aesthetic Plast Surg. 1995;19:421-5. PMID: 8526158.. However, the resorption rate is unpredictable and this biological phenomenon often results in the formation of scar tissue or oil cysts33 Gutowski KA, ASPS Fat Graft Task Force. Current applications and safety of autologous fat grafts: a report of the ASPS fat graft task force. Plast Reconstr Surg. 2009;124:272-80. doi: 10.1097/PRS.0b013e3181a09506.
https://doi.org/10.1097/PRS.0b013e3181a0...
. This led surgeons to seek techniques that improve the viability and quality of fat grafts44 Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg. 2007;119:775-85. PMID: 17312477..
Platelet-rich plasma (PRP) consists of a blood plasma fraction with elevated levels of platelets, obtained by centrifugation and separation of the different cellular fractions55 Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62:489-96. PMID: 15085519.. Platelets contain growth factors that stimulate neoangiogenesis and cell differentiation55 Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62:489-96. PMID: 15085519.
6 Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004;91:4-15. PMID: 14691563.-77 Choi HN, Han YS, Kim SR, Kim HK, Kim H, Park JH. The effect of platelet-rich plasma on survival of the composite graft and the proper time of injection in a rabbit ear composite graft model. Arch Plast Surg. 2014;41:647-53. doi: 10.5999/aps.2014.41.6.647.
https://doi.org/10.5999/aps.2014.41.6.64...
. Platelets in PRP are obtained in anticoagulated state, therefore inert and require activation (usually accomplished by the addition of calcium chloride and / or thrombin) to release their growth factors88 Cervelli V, Gentile P, Scioli MG, Grimaldi M, Casciani CU, Spagnoli LG, Orlandi A. Application of platelet-rich plasma in plastic surgery: clinical and in vitro evaluation. Tissue Eng Part C Methods. 2009;15:625-34. doi: 10.1089/ten.TEC.2008.0518.
https://doi.org/10.1089/ten.TEC.2008.051...
,99 Fukaya M, Ito A. A New economic method for preparing platelet-rich plasma. Plast Reconstr Surg Glob Open. 2014;2:e162. PMID: 25289355..
Activated platelets secrete growth factors and cytokines, which make them applicable to repair tissues and induce blood vessel formation66 Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004;91:4-15. PMID: 14691563.,1010 Sommeling CE, Heyneman A, Hoeksema H, Verbelen J, Stillaert FB, Monstrey S. The use of platelet-rich plasma in plastic surgery: a systematic review. J Plast Reconstr Aesthet Surg. 2013;66:301-11. doi: 10.1016/j.bjps.2012.11.009.
https://doi.org/10.1016/j.bjps.2012.11.0...
. Therefore, PRP has been studied associated to fat grafts, dental implants, orthopedic surgery, repair of tendons and muscles, recovery of skin lesions, ophthalmologic surgery, plastic surgery and other situations that require a stimulus to tissue repair1111 Gentile P, Bottini DJ, Spallone D, Curcio BC, Cervelli V. Application of platelet-rich plasma in maxillofacial surgery: clinical evaluation. J Craniofac Surg. 2010;21:900-4. doi: 10.1097/SCS.0b013e3181d878e9.
https://doi.org/10.1097/SCS.0b013e3181d8...
12 Gentile P, Di Pasquali C, Bocchini I, Floris M, Eleonora T, Fiaschetti V, Floris R, Cervelli V. Breast reconstruction with autologous fat graft mixed with platelet-rich plasma. Surg Innov. 2013;20:370-6. doi: 10.1177/1553350612458544.
https://doi.org/10.1177/1553350612458544...
-1313 P Waiker V, Shivalingappa S. Comparison between conventional mechanical fixation and use of autologous platelet rich plasma (PRP) in wound beds prior to resurfacing with split thickness skin graft. World J Plast Surg. 2015;4:50-9. PMID: 25606477..
The association of fat grafts and PRP began to be studied in recent years77 Choi HN, Han YS, Kim SR, Kim HK, Kim H, Park JH. The effect of platelet-rich plasma on survival of the composite graft and the proper time of injection in a rabbit ear composite graft model. Arch Plast Surg. 2014;41:647-53. doi: 10.5999/aps.2014.41.6.647.
https://doi.org/10.5999/aps.2014.41.6.64...
,1414 Serra-Mestre JM, Serra-Renom JM, Martinez L, Almadori A, D'Andrea F. Platelet-rich plasma mixed-fat grafting: a reasonable pro survival strategy for fat grafts? Aesthetic Plast Surg. 2014;38:1041-9. doi: 10.1007/s00266-014-0374-7.
https://doi.org/10.1007/s00266-014-0374-...
. This association is justifiable due to the pursuit of PRP as a mechanism to improve the viability and quality of fat grafts, mainly by stimulating neovascularization of the grafts. Further studies showed variable results and without any standardization of the methodology.
In this animal study, we evaluated the combination of PRP with fat grafts to develop surgical approaches with better graft viability and long-lasting clinical outcomes.
Methods
This blind and randomized in vivo research protocol was conducted in the Mastology Program of the University Hospital of the Universidade Federal de Goiás (HC-UFG). The research was approved by the hospital´s Ethics Research Committee (protocol 070/2011) and supervised by a veterinarian, so as not to violate any ethical concept of research in animals and to avoid any injury or suffering to them.
Few experimental studies with rats comparing fat grafting techniques are reported in the literature, making it difficult to estimate the likely difference between methods and stipulate the power of the test to be used. The sample size was chosen taking into account the availability of animals in the vivarium of HC-UFG, cost-effective increase in the number of cases and the ethical concern to minimize the use of animal experimentation. Fifty rats were considered a satisfactory number after the analysis of the before mentioned factors.
We used fifty adult female rats of the species Rattus norvegicus Wistar lineage, of similar size (average weight of 400g) and older than 60 days following the recommendations of the Brazilian College of Animal Experimentation (COBEA). The sample was divided into two groups (group with no PRP and group with PRP), and each animal received an autologous fat graft in the subcutaneous portion of the cranial area.
Surgical procedure
The animals were anesthetized with a solution of saline, ketamine (80mg/kg) and xylazine (10mg/kg) for veterinary use via the peritoneal route. Fat grafts (measuring 0,5 by 1.5 cm) were harvested from the inguinal region. This region was chosen because of its abundant deposit of fat in these animals (Figure 1). The graft was prepared with 0.1 ml of saline solution at 0.9% (control group) or 0.1 ml of platelet-rich plasma, activated with calcium chloride at 10% (case group), according to the randomization table previously established. The prepared graft was inserted subcutaneously in the cranial region (Figure 2).
The platelet-rich plasma was obtained by cardiac puncture and collection of 10 ml blood of rats. The syringe with collected blood was placed in a centrifuge and first spun at a speed of 1500 rpm for ten minutes, obtaining three fractions of blood (Figure 3). With a pipette, the middle fraction was collected (PRP mixed with white blood cells and plasma) and placed in another sterile syringe. This syringe was then centrifuged at a speed of 3000 rpm for 5 minutes, obtaining two fractions (Figure 4). In this step the top fraction consisted of cell-poor plasma and the lower composed of PRP (plasma with high concentration of platelets).
Aspect of blood after second centrifugation process used to obtain platelet rich plasma. PRP observed at the bottom of syringe.
At 100 days of the first surgery, the rats were anesthetized as described earlier and a block of the cranial skin, the fat graft and underlying muscle tissue was obtained. These blocks were fixed with formaldehyde and submitted to five micron cross-sections and stained with hematoxylin-eosin for analysis by optical microscope by the researchers responsible for the histological analysis of the material.
Histological evaluation
Histological analysis of the material was done by two medical pathologists (MARM, MAPCC), who made independent and blind analysis of each blade, assigning scores to each variable analyzed. The slides were evaluated according to the following variables: graft viability (percentage of the intact fat cells), necrotic area (percentage of area with necrotic / dead cell tissue), inflammation area (percentage of area with infiltration of inflammatory cells) and fibrosis area (area percentage with fibrous material / collagen fibers). The values obtained were classified with the aid of a histological score of the graft, scored 0 (absent) to 4 (heavy). For statistical analysis, the scores were grouped in Sparse (scores 0, 1 and 2) or Abundant (scores 3 and 4) (Table 1). The kappa statistic was used to calculate the concordance coefficient.
Statistical analysis
The sample was characterized by calculating the absolute and relative frequencies for the variables under study. Subsequently, we performed the analysis of central tendencies and dispersion measures as means and standard deviation for the age variable. Analyses to determine the association or independence between the variables were performed by Fisher test with the calculation of the relative risks using contingency tables to verify the average risk between the variables with a 95% confidence interval and level of significance level of 0.05.
Results
From the sample of fifty animals, two were used as PRP donors and a third died and was not included in the analysis. Thus, we studied 47 animals of the same breed, sex, weight and age. After randomization 22 rats were placed in the group with PRP and the other 25 in the control group without PRP. One animal died postoperatively, with no apparent cause after necropsy. Postoperative wound dehiscence of the donor area occurred in five animals. These wounds were left to heal by secondary intention being cleaned daily. There was total closure of dehiscence in all cases after seven days.
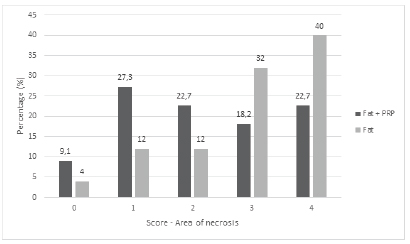
The score values assigned by both pathologists with almost perfect concordance (κ = 94%). The percentual distribution of these scores can be seen in Figures 5 to 8. It was observed that the viability of the graft, assessed by the presence of intact fat cells, with scores 3 and 4, was significantly higher in fat grafting group associated with PRP, compared to the control group who didn't receive PRP (p=0.03) (Table 1, Figure 9).
Percentages of scores regarding presence of inflammatory cells in fat only and fat + PRP groups.
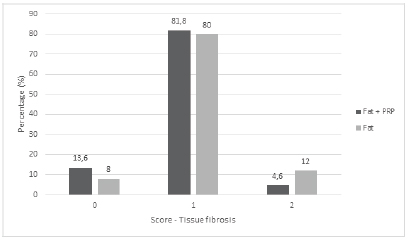
Percentages of scores regarding histological signs of fibrosis in fat only and fat + PRP groups.
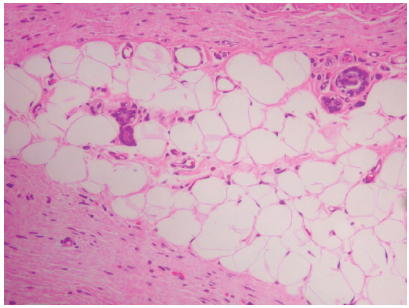
Photomicrograph (HE x100). Intact fat cells and blood vessels in fat graft that received platelet rich plasma.
As for the variable area of necrosis, which supports the analysis of the viability of the grafts, we observed in the group with PRP (n = 22), that fourteen grafts (63.6%) had a score 0,1 or 2 and eight grafts (36.4%) with score 3 or 4. This difference was statistically significant (p=0.03), showing a lower percentage of necrosis of fat cells in the group with PRP and consequently higher percentage rate of the intact fat cells (Table 1, Figure 9).
In the analysis of local inflammation we observed in the group receiving PRP that up to 85% of the grafts had low scores (0.1 or 2), compared to 64% in the group without PRP, showing that the grafts mixed with PRP had better preservation of adipose cells, fewer dead cells and consequently a smaller amount of tissue inflammation (Table 1, Figure 10).
Photomicrograph (HE x100). Sparse intact fat cells and abundant inflammatory cell infiltrate in fat graft without the addition of platelet rich plasma.
In the analysis of the variable presence of tissue fibrosis, it was observed that both groups had low fibrosis rates (score 4 not given to any graft by either evaluators), with no statistical difference between the two groups (Figure 8). As an incidental finding, we noted the presence of dermoid cysts in the fat grafts of three animals, all allocated in graft group with PRP (Figure 11).
Photomicrograph (HE x25). Bulky dermoid cyst in fat graft that received platelet rich plasma.
Discussion
Recently there has been an increase in studies on fat grafts1515 Li F, Guo W, Li K, Yu M, Tang W, Wang H, Tian W. Improved fat graft survival by different volume fractions of platelet-rich plasma and adipose-derived stem cells. Aesthet Surg J. 2015 Mar;35(3):319-33. doi: 10.1093/asj/sju046.
https://doi.org/10.1093/asj/sju046...
,1616 Largo RD, Tchang LA, Mele V, Scherberich A, Harder Y, Wettstein R, Schaefer DJ. Efficacy, safety and complications of autologous fat grafting to healthy breast tissue: a systematic review. J Plast Reconstr Aesthet Surg. 2014;67:437-48. doi: 10.1016/j.bjps.2013.11.011.
https://doi.org/10.1016/j.bjps.2013.11.0...
. Many studies propose new techniques for grafts, to counteract the resorption rate and increase the aiming less resorption and increased viability of the fat. Upon revision of literature it is noted that there is no consensus on PRP preparation. Various methods are described with different protocols and concentrations, but most techniques have some points in common1717 Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants. 1999;14:529-35. PMID: 10453668.
18 Mazzucco L, Balbo V, Cattana E, Guaschino R, Borzini P. Not every PRP-gel is born equal. Evaluation of growth factor availability for tissues through four PRP-gel preparations: Fibrinet, RegenPRP-Kit, Plateltex and one manual procedure. Vox Sang. 2009;97:110-8. doi: 10.1111/j.1423-0410.2009.01188.x.
https://doi.org/10.1111/j.1423-0410.2009...
19 Gentile P, Orlandi A, Scioli MG, Di Pasquali C, Bocchini I, Curcio CB, Floris M, Fiaschetti V, Floris R, Cervell V. Comparative translational study: the combined use of enhanced stromal vascular fraction and platelet-rich plasma improves fat grafting maintenance in breast reconstruction. Stem Cells Transl Med. 2012;1(4):341-51. doi: 10.5966/sctm.2011-0065.
https://doi.org/10.5966/sctm.2011-0065...
-2020 Piasecki JH, Gutowski KA, Lahvis GP, Moreno KI. An experimental model for improving fat graft viability and purity. Plast Reconstr Surg. 2007;119:1571-83. PMID: 17415252..
To produce PRP autologous blood is generally obtained by peripheral venipuncture prior to any surgical procedure and added to an anticoagulant. The blood is then centrifuged which yield two phases of blood: platelet-rich plasma (PRP) and platelet poor plasma (PPP). In a recent review article Sommeling et al.1010 Sommeling CE, Heyneman A, Hoeksema H, Verbelen J, Stillaert FB, Monstrey S. The use of platelet-rich plasma in plastic surgery: a systematic review. J Plast Reconstr Aesthet Surg. 2013;66:301-11. doi: 10.1016/j.bjps.2012.11.009.
https://doi.org/10.1016/j.bjps.2012.11.0...
noted that in forty papers about the use of PRP in plastic surgery, nine used a single centrifugation step, eighteen two centrifugation steps and in thirteen papers the number of centrifugations was not mentioned. In the present series we used two centrifugations in order to obtain PRP, with evidence of platelet concentration observed by light microscopy, although we didn't quantify the increase in this platelet number in absolute terms since our method of centrifugation was not automated but manual.
The combination of fat grafts and PRP was evaluated by few studies, with variable results and without any standardization of the methodology2121 Jin R, Zhang L, Zhang YG. Does platelet-rich plasma enhance the survival of grafted fat? An update review. Int J Clin Exp Med. 2013;6:252-8. PMID: 23641301.. PRP, after being activated, releases large amounts of growth factors and cytokines, stimulating increased cell replication, increased collagen production, recruitment of other cells to the site of injury, stimulating neoangiogenesis and differentiation induction55 Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62:489-96. PMID: 15085519.. In animal studies2222 Rodríguez-Flores J, Palomar-Gallego MA, Enguita-Valls AB, Rodríguez-Peralto JL, Torres J. Influence of platelet-rich plasma on the histologic characteristics of the autologous fat graft to the upper lip of rabbits. Aesthetic Plast Surg. 2011;35:480-6. doi: 10.1007/s00266-010-9640-5.
https://doi.org/10.1007/s00266-010-9640-...
,2323 Nakamura S, Ishihara M, Takikawa M, Murakami K, Kishimoto S, Nakamura S, Yanagibayashi S, Kubo S, Yamamoto N, Kiyosawa T. Platelet-rich plasma (PRP) promotes survival of fat-grafts in rats. Ann Plast Surg. 2010;65:101-6. doi: 10.1097/SAP.0b013e3181b0273c.
https://doi.org/10.1097/SAP.0b013e3181b0...
the association of fat with PRP increased graft take, whereas Por et al.2424 Por YC, Yeow VK, Louri N, Lim TK, Kee I, Song IC. Platelet-rich plasma has no effect on increasing free fat graft survival in the nude mouse. J Plast Reconstr Aesthet Surg. 2009;62:1030-4. doi: 10.1016/j.bjps.2008.01.013.
https://doi.org/10.1016/j.bjps.2008.01.0...
observed that this association is not beneficial for increasing the viability of the grafts. In the latter work, there is no mention of the PRP activation, a fact that may have contributed to the absence of benefits of PRP on the viability of the grafted fat.
Another criticism made by some authors is that the PRP obtained in small animals studies is not autologous, but from a donor animal that produces sufficient PRP for the remainder of the experiment55 Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62:489-96. PMID: 15085519., since it is impossible for PRP to be obtained in sufficient quantity without having to euthanise the donor animal due to the large volume of blood required. In our work, we show positive results of the PRP and fat graft association, even though the PRP utilized is of homologous origin (donor animal of the same species) and not autologous. Other authors shared the same conclusions in their studies with animals2222 Rodríguez-Flores J, Palomar-Gallego MA, Enguita-Valls AB, Rodríguez-Peralto JL, Torres J. Influence of platelet-rich plasma on the histologic characteristics of the autologous fat graft to the upper lip of rabbits. Aesthetic Plast Surg. 2011;35:480-6. doi: 10.1007/s00266-010-9640-5.
https://doi.org/10.1007/s00266-010-9640-...
,2323 Nakamura S, Ishihara M, Takikawa M, Murakami K, Kishimoto S, Nakamura S, Yanagibayashi S, Kubo S, Yamamoto N, Kiyosawa T. Platelet-rich plasma (PRP) promotes survival of fat-grafts in rats. Ann Plast Surg. 2010;65:101-6. doi: 10.1097/SAP.0b013e3181b0273c.
https://doi.org/10.1097/SAP.0b013e3181b0...
.
In PRP associated with fat grafts studies in humans there are also conflicting data. While the group led by Cervelli in successive papers88 Cervelli V, Gentile P, Scioli MG, Grimaldi M, Casciani CU, Spagnoli LG, Orlandi A. Application of platelet-rich plasma in plastic surgery: clinical and in vitro evaluation. Tissue Eng Part C Methods. 2009;15:625-34. doi: 10.1089/ten.TEC.2008.0518.
https://doi.org/10.1089/ten.TEC.2008.051...
,2525 Cervelli V, Gentile P, De Angelis B, Calabrese C, Di Stefani A, Scioli MG, Curcio BC, Felici M, Orlandi A. Application of enhanced stromal vascular fraction and fat grafting mixed with PRP in post-traumatic lower extremity ulcers. Stem Cell Res. 2011;6:103-11. doi: 10.1016/j.scr.2010.11.003.
https://doi.org/10.1016/j.scr.2010.11.00...
,2626 Cervelli V, Scioli MG, Gentile P, Doldo E, Bonanno E, Spagnoli LG, Orlandi A. Platelet-rich plasma greatly potentiates insulin-induced adipogenic differentiation of human adipose-derived stem cells through a serine/threonine kinase Akt-dependent mechanism and promotes clinical fat graft maintenance. Stem Cells Transl Med. 2012;1:206-20. doi: 10.5966/sctm.2011-0052.
https://doi.org/10.5966/sctm.2011-0052...
presented results that indicate an improvement of the viability of the grafts with PRP association, the study of Salgarello et al.2727 Salgarello M, Visconti G, Rusciani A. Breast fat grafting with platelet-rich plasma: a comparative clinical study and current state of the art. Plast Reconstr Surg. 2011;127:2176-85. doi: 10.1097/PRS.0b013e3182139fe7.
https://doi.org/10.1097/PRS.0b013e318213...
showed no benefits in this association. In the latter article, PRP was obtained using a automated method, which may have resulted in an insufficient concentration of PRP added to the grafts2727 Salgarello M, Visconti G, Rusciani A. Breast fat grafting with platelet-rich plasma: a comparative clinical study and current state of the art. Plast Reconstr Surg. 2011;127:2176-85. doi: 10.1097/PRS.0b013e3182139fe7.
https://doi.org/10.1097/PRS.0b013e318213...
. Other authors analyzed that differences in concentration of growth factors in the PRP obtained by automated methods are dependent of the device or technique utilized1818 Mazzucco L, Balbo V, Cattana E, Guaschino R, Borzini P. Not every PRP-gel is born equal. Evaluation of growth factor availability for tissues through four PRP-gel preparations: Fibrinet, RegenPRP-Kit, Plateltex and one manual procedure. Vox Sang. 2009;97:110-8. doi: 10.1111/j.1423-0410.2009.01188.x.
https://doi.org/10.1111/j.1423-0410.2009...
,2828 Pallua N, Wolter T, Markowicz M. Platelet-rich plasma in burns. Burns. 2010;36:4-8. doi: 10.1016/j.burns.2009.05.002.
https://doi.org/10.1016/j.burns.2009.05....
,2929 Del Vecchio DA, Bucky LP. Breast augmentation using pre expansionand autologous fat transplantation: a clinical radiographic study. Plast Reconstr Surg. 2011;127:2441-50. doi: 10.1097/PRS.0b013e3182050a64.
https://doi.org/10.1097/PRS.0b013e318205...
.
In the current study, histological variables were classified in increasing scores and then categorized into two groups, sparse or abundant. This categorization allowed the observation of increased tissue viability and reduced area of necrosis in the animals subjected to grafts with PRP association. Moreover, there was a perfect interobserver agreement. We understand that the best way to analyze the feasibility of the grafts would be through histology, easily performed in animal studies, but of great difficulty in human studies. Thus, the current study provides important information on the histological evaluation of the association between fat grafts and PRP.
Dermoid cysts can be described as cystic tumors covered with epithelium and skin appendages, being found in different species and considered as resulting from the entrapment of the epidermal and dermal anexal structures during embryonic development, with low malignant potential3030 Golden BA, Jaskolka MS, Ruiz RL. Craniofacial and orbital dermoids in children. Oral Maxillofac Surg Clin North Am. 2012;24:417-25. doi: 10.1016/j.coms.2012.04.006.
https://doi.org/10.1016/j.coms.2012.04.0...
. In our study we observed the presence of dermoid cysts within the fat graft in three animals of the 47 evaluated, coincidentally all treated with graft associated with PRP. We cannot conclude that fat grafts associated with PRP had causal relationship in the formation of these tumors, but considering the hypothesis that these tumors were previously present in the groin fat used for grafting, the fact that they remained viable within the graft and possibly increased in size after grafting draws our attention, as they were not observed macroscopically during the surgical stage of completion of the grafts.
Conclusions
Platelet-rich plasma (PRP) improves the viability and integration of fat grafts in rats. The PRP group also presented lower fat necrosis and local inflammation scores when compared to the fat graft only group.
References
-
1Biazus JV, Falcão CC, Parizotto AC, Stumpf CC, Cavalheiro JA, Schuh F, Cericatto R, Zucatto ÂE, Melo MP. Immediate reconstruction with autologous fat transfer following breast-conserving surgery. Breast J. 2015 May-Jun;21(3):268-75. doi: 10.1111/tbj.12397.
» https://doi.org/10.1111/tbj.12397. -
2Coleman SR. Long-term survival of fat transplants: controlled demonstrations. Aesthetic Plast Surg. 1995;19:421-5. PMID: 8526158.
-
3Gutowski KA, ASPS Fat Graft Task Force. Current applications and safety of autologous fat grafts: a report of the ASPS fat graft task force. Plast Reconstr Surg. 2009;124:272-80. doi: 10.1097/PRS.0b013e3181a09506.
» https://doi.org/10.1097/PRS.0b013e3181a09506 -
4Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg. 2007;119:775-85. PMID: 17312477.
-
5Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62:489-96. PMID: 15085519.
-
6Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004;91:4-15. PMID: 14691563.
-
7Choi HN, Han YS, Kim SR, Kim HK, Kim H, Park JH. The effect of platelet-rich plasma on survival of the composite graft and the proper time of injection in a rabbit ear composite graft model. Arch Plast Surg. 2014;41:647-53. doi: 10.5999/aps.2014.41.6.647.
» https://doi.org/10.5999/aps.2014.41.6.647 -
8Cervelli V, Gentile P, Scioli MG, Grimaldi M, Casciani CU, Spagnoli LG, Orlandi A. Application of platelet-rich plasma in plastic surgery: clinical and in vitro evaluation. Tissue Eng Part C Methods. 2009;15:625-34. doi: 10.1089/ten.TEC.2008.0518.
» https://doi.org/10.1089/ten.TEC.2008.0518 -
9Fukaya M, Ito A. A New economic method for preparing platelet-rich plasma. Plast Reconstr Surg Glob Open. 2014;2:e162. PMID: 25289355.
-
10Sommeling CE, Heyneman A, Hoeksema H, Verbelen J, Stillaert FB, Monstrey S. The use of platelet-rich plasma in plastic surgery: a systematic review. J Plast Reconstr Aesthet Surg. 2013;66:301-11. doi: 10.1016/j.bjps.2012.11.009.
» https://doi.org/10.1016/j.bjps.2012.11.009 -
11Gentile P, Bottini DJ, Spallone D, Curcio BC, Cervelli V. Application of platelet-rich plasma in maxillofacial surgery: clinical evaluation. J Craniofac Surg. 2010;21:900-4. doi: 10.1097/SCS.0b013e3181d878e9.
» https://doi.org/10.1097/SCS.0b013e3181d878e9 -
12Gentile P, Di Pasquali C, Bocchini I, Floris M, Eleonora T, Fiaschetti V, Floris R, Cervelli V. Breast reconstruction with autologous fat graft mixed with platelet-rich plasma. Surg Innov. 2013;20:370-6. doi: 10.1177/1553350612458544.
» https://doi.org/10.1177/1553350612458544 -
13P Waiker V, Shivalingappa S. Comparison between conventional mechanical fixation and use of autologous platelet rich plasma (PRP) in wound beds prior to resurfacing with split thickness skin graft. World J Plast Surg. 2015;4:50-9. PMID: 25606477.
-
14Serra-Mestre JM, Serra-Renom JM, Martinez L, Almadori A, D'Andrea F. Platelet-rich plasma mixed-fat grafting: a reasonable pro survival strategy for fat grafts? Aesthetic Plast Surg. 2014;38:1041-9. doi: 10.1007/s00266-014-0374-7.
» https://doi.org/10.1007/s00266-014-0374-7 -
15Li F, Guo W, Li K, Yu M, Tang W, Wang H, Tian W. Improved fat graft survival by different volume fractions of platelet-rich plasma and adipose-derived stem cells. Aesthet Surg J. 2015 Mar;35(3):319-33. doi: 10.1093/asj/sju046.
» https://doi.org/10.1093/asj/sju046 -
16Largo RD, Tchang LA, Mele V, Scherberich A, Harder Y, Wettstein R, Schaefer DJ. Efficacy, safety and complications of autologous fat grafting to healthy breast tissue: a systematic review. J Plast Reconstr Aesthet Surg. 2014;67:437-48. doi: 10.1016/j.bjps.2013.11.011.
» https://doi.org/10.1016/j.bjps.2013.11.011 -
17Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants. 1999;14:529-35. PMID: 10453668.
-
18Mazzucco L, Balbo V, Cattana E, Guaschino R, Borzini P. Not every PRP-gel is born equal. Evaluation of growth factor availability for tissues through four PRP-gel preparations: Fibrinet, RegenPRP-Kit, Plateltex and one manual procedure. Vox Sang. 2009;97:110-8. doi: 10.1111/j.1423-0410.2009.01188.x.
» https://doi.org/10.1111/j.1423-0410.2009.01188.x -
19Gentile P, Orlandi A, Scioli MG, Di Pasquali C, Bocchini I, Curcio CB, Floris M, Fiaschetti V, Floris R, Cervell V. Comparative translational study: the combined use of enhanced stromal vascular fraction and platelet-rich plasma improves fat grafting maintenance in breast reconstruction. Stem Cells Transl Med. 2012;1(4):341-51. doi: 10.5966/sctm.2011-0065.
» https://doi.org/10.5966/sctm.2011-0065 -
20Piasecki JH, Gutowski KA, Lahvis GP, Moreno KI. An experimental model for improving fat graft viability and purity. Plast Reconstr Surg. 2007;119:1571-83. PMID: 17415252.
-
21Jin R, Zhang L, Zhang YG. Does platelet-rich plasma enhance the survival of grafted fat? An update review. Int J Clin Exp Med. 2013;6:252-8. PMID: 23641301.
-
22Rodríguez-Flores J, Palomar-Gallego MA, Enguita-Valls AB, Rodríguez-Peralto JL, Torres J. Influence of platelet-rich plasma on the histologic characteristics of the autologous fat graft to the upper lip of rabbits. Aesthetic Plast Surg. 2011;35:480-6. doi: 10.1007/s00266-010-9640-5.
» https://doi.org/10.1007/s00266-010-9640-5 -
23Nakamura S, Ishihara M, Takikawa M, Murakami K, Kishimoto S, Nakamura S, Yanagibayashi S, Kubo S, Yamamoto N, Kiyosawa T. Platelet-rich plasma (PRP) promotes survival of fat-grafts in rats. Ann Plast Surg. 2010;65:101-6. doi: 10.1097/SAP.0b013e3181b0273c.
» https://doi.org/10.1097/SAP.0b013e3181b0273c -
24Por YC, Yeow VK, Louri N, Lim TK, Kee I, Song IC. Platelet-rich plasma has no effect on increasing free fat graft survival in the nude mouse. J Plast Reconstr Aesthet Surg. 2009;62:1030-4. doi: 10.1016/j.bjps.2008.01.013.
» https://doi.org/10.1016/j.bjps.2008.01.013 -
25Cervelli V, Gentile P, De Angelis B, Calabrese C, Di Stefani A, Scioli MG, Curcio BC, Felici M, Orlandi A. Application of enhanced stromal vascular fraction and fat grafting mixed with PRP in post-traumatic lower extremity ulcers. Stem Cell Res. 2011;6:103-11. doi: 10.1016/j.scr.2010.11.003.
» https://doi.org/10.1016/j.scr.2010.11.003 -
26Cervelli V, Scioli MG, Gentile P, Doldo E, Bonanno E, Spagnoli LG, Orlandi A. Platelet-rich plasma greatly potentiates insulin-induced adipogenic differentiation of human adipose-derived stem cells through a serine/threonine kinase Akt-dependent mechanism and promotes clinical fat graft maintenance. Stem Cells Transl Med. 2012;1:206-20. doi: 10.5966/sctm.2011-0052.
» https://doi.org/10.5966/sctm.2011-0052 -
27Salgarello M, Visconti G, Rusciani A. Breast fat grafting with platelet-rich plasma: a comparative clinical study and current state of the art. Plast Reconstr Surg. 2011;127:2176-85. doi: 10.1097/PRS.0b013e3182139fe7.
» https://doi.org/10.1097/PRS.0b013e3182139fe7 -
28Pallua N, Wolter T, Markowicz M. Platelet-rich plasma in burns. Burns. 2010;36:4-8. doi: 10.1016/j.burns.2009.05.002.
» https://doi.org/10.1016/j.burns.2009.05.002 -
29Del Vecchio DA, Bucky LP. Breast augmentation using pre expansionand autologous fat transplantation: a clinical radiographic study. Plast Reconstr Surg. 2011;127:2441-50. doi: 10.1097/PRS.0b013e3182050a64.
» https://doi.org/10.1097/PRS.0b013e3182050a64 -
30Golden BA, Jaskolka MS, Ruiz RL. Craniofacial and orbital dermoids in children. Oral Maxillofac Surg Clin North Am. 2012;24:417-25. doi: 10.1016/j.coms.2012.04.006.
» https://doi.org/10.1016/j.coms.2012.04.006
-
Financial source:
none -
1
Research performed at Goiânia Mastology Research Network and Mastology Program, Teaching Hospital, Universidade Federal de Goiás, Goiania-GO, Brazil.
Publication Dates
-
Publication in this collection
Oct 2016
History
-
Received
14 June 2016 -
Reviewed
16 Aug 2016 -
Accepted
15 Sept 2016