Abstract
OBJECTIVE:
To assess the influence of central obesity on the magnitude of the error of estimate of maximal oxygen uptake in maximal cycling exercise testing.
METHOD:
A total of 1,715 adults (68% men) between 18-91 years of age underwent cardiopulmonary exercise testing using a progressive protocol to volitional fatigue. Subjects were stratified by central obesity into three quartile ranges: Q1, Q2-3 and Q4. Maximal oxygen uptake [mL.(kg.min)-1] was estimated by the attained maximal workload and body weight using gender- and population-specific equations. The error of estimate [mL.(kg.min)-1] and percent error between measured and estimated maximal oxygen uptake values were compared among obesity quartile ranges.
RESULTS:
The error of estimate and percent error differed (mean ± SD) for men (Q1=1.3±3.7 and 2.0±10.4; Q2-3=0.5±3.1 and -0.5±13.0; and Q4=-0.3±2.8 and -4.5±15.8 (p<0.05)) and for women (Q1=1.6±3.3 and 3.6±10.2; Q2-3=0.4±2.7 and -0.4±11.8; and Q4=-0.9±2.3 and -10.0±22.7 (p<0.05)).
CONCLUSION:
Central obesity directly influences the magnitude of the error of estimate of maximal oxygen uptake and should be considered when direct expired gas analysis is unavailable.
Cardiorespiratory Fitness; Obesity; Cardiopulmonary Exercise Testing; Aerobic Fitness; Body Composition
INTRODUCTION
There is strong evidence that cardiorespiratory fitness is inversely associated with cardiovascular and all-cause mortality (11. Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN. Fitness vs. fatness on all-cause mortality: a meta-analysis. Prog Cardiovasc Dis. 2014;56(4):382-90, http://dx.doi.org/10.1016/j.pcad.2013.09.002.
http://dx.doi.org/10.1016/j.pcad.2013.09...
). Cardiorespiratory fitness can be accurately assessed by directly measuring maximal oxygen consumption (VO2max) at peak exercise during cardiopulmonary exercise testing (CPET). However, due to the limited availability of metabolic testing resources, VO2max is more commonly estimated, rather than directly measured, by applying equations that take into consideration the maximal workload achieved or the exercise duration (22. Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85(4):546-62, http://dx.doi.org/10.1016/0002-8703(73)90502-4.
http://dx.doi.org/10.1016/0002-8703(73)9...
,33. Storer TW, Davis JA, Caiozzo VJ. Accurate prediction of VO2max in cycle ergometry. Med Sci Sports Exerc. 1990;22(5):704-12.). Although measured and estimated VO2max are strongly associated, the error of estimate (EE) for a given subject tends to be substantial, averaging 10-20%, which far exceeds the normal error of other clinical and laboratory measurements (44. Araújo CG, Herdy AH, Stein R. Maximum oxygen consumption measurement: valuable biological marker in health and in sickness. Arq Bras Cardiol. 2013;100(4):e51-3, http://dx.doi.org/10.5935/abc.20130085.
http://dx.doi.org/10.5935/abc.20130085...
).
The ability to utilize oxygen to perform work is related to an individual’s mechanical efficiency (55. Whipp BJ, Wasserman K. Efficiency of muscular work. J Appl Physiol. 1969;26(5):644-8.). Therefore, when applying a given equation to estimate VO2max, it is generally assumed that all subjects have the same mechanical efficiency, which is biologically incorrect and likely explains most of the EE of VO2max.
Among the factors that likely influence mechanical efficiency, one of the most clinically relevant is body composition, primarily due to the increased prevalence of obesity in recent decades. Obesity and, more particularly, central obesity may hinder the mobilization of the lower limbs, possibly reducing the mechanical efficiency for activities such as cycling or walking (66. Berry MJ, Storsteen JA, Woodard CM. Effects of body mass on exercise efficiency and VO2 during steady-state cycling. Med Sci Sports Exerc. 1993;25(9):1031-7, http://dx.doi.org/10.1249/00005768-199309000-00010.
http://dx.doi.org/10.1249/00005768-19930...
); therefore, there may be an increased EE of VO2max in overweight and obese subjects. Currently, there is very little data available regarding the role of central obesity as a modulator of the EE of VO2max.
Therefore, the current study was performed to determine the influence of central obesity, based on the waist to height ratio (WHtR), in the EE of VO2max.
MATERIALS AND METHODS
Sample
Our study population included volunteer adult subjects in an exercise medicine clinic who initially underwent CPET using a progressive cycle ergometer protocol between January 2008 and June 2014. All patients were evaluated for exercise prescription purposes and provided informed consent. All patients authorized the de-identified use of their collected data for research purposes. The study and retrospective data analysis were approved by the institutional ethics committee. Subjects were excluded based on the following criteria: those who had previously been tested in our clinic, those who were younger than 18 years of age, those who had undergone treadmill testing, and those who did not fulfill the criteria for a maximal CPET. An additional 100 subjects who had incomplete data were excluded. The final population sample included 1,715 subjects.
Anthropometric measurements
Body weight was measured to the nearest 0.1 kg while the subject was barefoot and wearing light clothing. Height and waist circumference were obtained to the nearest 0.1 cm. The latter was measured in the upright position, at the umbilicus level (77. de Oliveira A, Cocate PG, Hermsdorff HH, Bressan J, de Silva MF, Rodrigues JA, et al. Waist circumference measures: cutoff analyses to detect obesity and cardiometabolic risk factors in a Southeast Brazilian middle-aged men population--a cross-sectional study. Lipids Health Dis. 2014;13:141, http://dx.doi.org/10.1186/1476-511X-13-141.
http://dx.doi.org/10.1186/1476-511X-13-1...
), with an anthropometric tape. The WHtR, obtained by dividing waist circumference by body height, was used as an index for central obesity, as it is a more reliable and proportional measure of obesity than the waist circumference alone.
Maximal cardiopulmonary exercise testing
Maximal CPET was conducted using an electromagnetically braked cycle ergometer (Inbrasport CG-04, Inbrasport, Brazil) and an individualized ramp protocol designed to achieve voluntary exhaustion between 8 and 12 minutes. All CPET was performed under direct medical supervision in a properly equipped laboratory. Subject seat height and body position were carefully adjusted on the cycle ergometer to provide a comfortable cycling movement. The pedaling rate was maintained between 65 and 75 revolutions per minute.
One lead CM5 or CC5 digital ECG continuous monitoring (ErgoPC Elite, Micromed, Brazil) was obtained at rest, during exercise and at 5-minute recovery periods. Resting, exercise and post-exercise measurements of heart rate (HR) (bpm) and blood pressure (mmHg) were obtained from ECG recordings and by auscultation of the right brachial artery, respectively.
During CPET, subjects expired through a mouthpiece and a pneumotachograph Prevent (MedGraphics, United States) with the nose occluded. Ventilatory analysis was accomplished using a metabolic analyzer VO2000 (MedGraphics, United States) that was calibrated daily. During exercise, expired gases were continuously collected, and the results were recorded at 10-second intervals. The data from six consecutive 10-second intervals were averaged and reported for each minute during CPET. VO2max represents the highest oxygen uptake value obtained, expressed as mL.(kg.min)-1, during CPET.
A CPET session was defined as maximum if it was not prematurely terminated due to adverse signs/symptoms and if it fulfilled physiological criteria (88. Ramos PS, Sardinha A, Nardi AE, de Araújo CG. Cardiorespiratory optimal point: a submaximal exercise variable to assess panic disorder patients. PLoS One. 2014;9(8):e104932, http://dx.doi.org/10.1371/journal.pone.0104932.
http://dx.doi.org/10.1371/journal.pone.0...
). Additionally, measures of perceived exertion were obtained to assess somatic exhaustion, a score of 10 on the 0-10 Borg scale (99. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377-81, http://dx.doi.org/10.1249/00005768-198205000-00012.
http://dx.doi.org/10.1249/00005768-19820...
), which was further indicated by the inability to maintain the required pedal cadence (65-75 rev/min) despite strong verbal encouragement. The highest HR attained was not solely used as the criterion for considering a CPET session as the maximum.
Predicting maximum VO2 and HR
To better characterize the study sample, VO2max [mL.(kg.min)-1] values were predicted by gender-specific equations (1010. Jones NL, Campbell EJM, Edwards RHT, Robertson DG. Clinical Exercise Testing. WB Saunders. Philadelphia;1995. pp 202.): 60 - 0.55 x age (years) for men and 48 - 0.37 x age (years) for women. Maximum values of HR were age-predicted by a previously validated equation: HR max (bpm) = 208 - 0.7 x age (years) (1111. Duarte CV, Araujo CG. Cardiac vagal index does not explain age-independent maximal heart rate. Int J Sports Med. 2013;34(6):502-6.).
Estimating VO2max
VO2max [mL.(kg.min)-1] was estimated by the gender-specific equations that were previously validated for a similar population in our exercise lab as follows: C-MEN = [maximal workload (watts)/weight (kg)] x 10.79 + 7 and C-WOMEN = [maximal workload (watts)/weight (kg)] x 9.82 + 7 (1212. Souza e Silva CG, Araújo CG. Sex-specific equations to estimate maximum oxygen uptake in cycle ergometry. Arq Bras Cardiol. 2015;105(4):381-9, http://dx.doi.org/10.5935/abc.20150089.
http://dx.doi.org/10.5935/abc.20150089...
).
Comparing measured and estimated VO2max
To compare measured and estimated VO2max, subjects were categorized by gender (1,172 men and 543 women) and then divided into three quartile ranges according to WHtR: Q1, Q2-3 (combining Q2 and Q3) and Q4. For each of these quartile ranges, VO2max per kg of body weight, EE (measured VO2max - estimated VO2max) in mL.(kg.min)-1 and percent error (%E; [(measured VO2max - estimated VO2max)/measured VO2max] x 100) were calculated for both men and women. Negative values of EE and %E signified that the estimated VO2max was higher than the measured VO2max, that is, the equation overestimated VO2max.
Data analysis
Descriptive statistics are presented as mean and standard deviation or as percent. Demographic characteristics and CPET variables were compared by t-test or chi-square test for each gender. Pearson product-moment correlation was also calculated for measured and estimated VO2max in men and women. One-way ANOVA was used to compare EE and %E among the quartile ranges for each gender. Statistical analysis was performed using Prism 6 (GraphPad, USA), with 5% probability as the criterion for statistical significance.
RESULTS
The average age of our subjects (n=1,715) was 52±15 years, with men representing 68.3% of the total sample. Considering the entire study population, 20.8% were apparently healthy, 17.2% had known coronary artery disease, and the remaining subjects exhibited diverse clinical conditions, including arterial hypertension, diabetes mellitus, obesity, pulmonary disease, or combinations thereof. Based on body mass index (BMI), 41.5% and 23.2% of the subjects were classified as overweight and obese, respectively, including 1.4% of the total sample that was morbidly obese. Regarding prescribed medications, 23.0% of the subjects were taking β-blockers, 34.9% were on angiotensin-converting enzyme inhibitors or angiotensin II receptor antagonists use, and 39.8% were using cholesterol-lowering medications.
As estimated by the WHtR, central obesity was higher in men was higher than in women (0.565±0.070 vs. 0.526±0.082, p<0.01). The WHtR results for each of the quartile ranges for men were as follows: Q1=0.378 to 0.515, Q2-3=0.515 to 0.612, and Q4=0.612 to 0.900. The WHtR results for each one of the quartile ranges for women were as follows: Q1=0.332 to 0.467, Q2-3=0.467 to 0.571, and Q4=0.572 to 0.813. Additional demographic and CPET data, with specific reference to progressive WHtR ranges, are presented in Tables 1 and 2.
Maximal cardiopulmonary exercise testing results
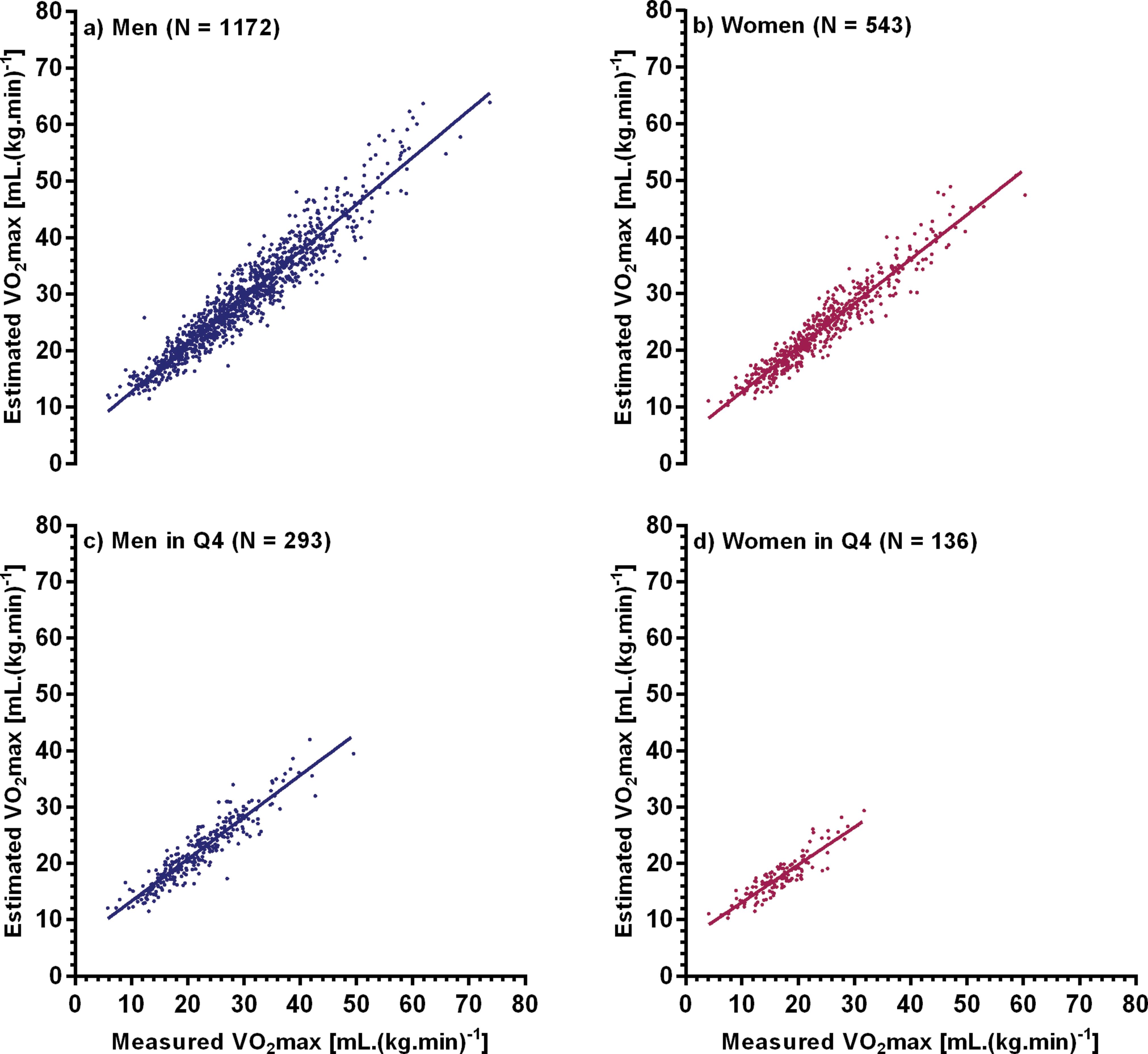
The duration of CPET averaged 10±2 minutes, with 70% of all tests lasting between 8 and 12 minutes. The maximum HR, when expressed as a percentage of the age-predicted value, was similar for men and women (92.2% vs. 93.0%, respectively, p=0.15). The maximal attained workload was higher for men than for women (172±70 vs. 111±45 watts, respectively, p<0.01). As a group, men achieved a higher VO2max than women (29.4±10.5 vs. 24.1±9.0 mL.(kg.min)-1, respectively, p<0.01). Measured VO2max ranged from 5.8 to 73.3 mL.(kg.min)-1 in men and from 4.1 to 60.1 mL.(kg.min)-1 in women. For both genders, these values were consistently lower for those classified in the Q4 cohort of WHtR (21.9±7.0 the expression “for men” and 16.6±5.1 mL.(kg.min)-1 the expression “for women”, p<0.01). Measured and estimated values of VO2max were strongly correlated in both sexes (r=0.95, p<0.01). For the Q4 subset, the measured versus estimated VO2max relationship remained highly significant (r=0.93 and r=0.90 for men and women, respectively) (Figure 1).
Relationship between measured and estimated VO2max: (a) 1,172 men, (b) 543 women, (c) men at Q4 waist-height ratio, and (d) women at Q4 waist-height ratio.
Measured VO2max tended to be lower than age-predicted VO2max, corresponding to 96.6±26.9% and 81.7±24.5% for men and women, respectively. Considering only Q4 subjects, measured VO2max corresponded to an even lower percent of age-predicted VO2max in men and women, 80.0±20.3% and 64.5±14.4%, respectively.
The values of EE were 0.5±3.2 mL.(kg.min)-1 for men and 0.4±2.9 mL.(kg.min)-1 for women (p=0.54). The values of %E were 0.9±13.4% for men and -1.8±15.8% for women (p=0.20). An analysis of %E for the three WHtR quartile ranges revealed a clear trend, with Q1 showing a slight tendency to underestimate VO2max and Q4 showing a strong tendency to overestimate VO2max for both sexes. For Q4 men, the %E was -4.5±15.8%, which was significantly larger than the %E for Q1 and Q2-3 (2.0±10.4 and -0.5±13.0%, respectively, p<0.01). For women, an even larger %E was identified in Q4 (-10.0±22.7%, p<0.01), and as observed in men, comparably lower %E values were seen in Q1 and Q2-3 (3.6±10.2 and -0.4±11.8%, respectively, p<0.01). When comparing EE and %E by sex in each of the three quartile ranges, no differences were observed between men and women (p>0.05). Nevertheless, by analyzing the magnitude of the variability of the EE and %E results, as reflected by the standard deviation of the means, it is apparent that the EE of VO2max remained high for any given subject, especially among those with a higher WHtR.
DISCUSSION
Although cardiorespiratory fitness is most accurately measured during CPET (22. Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85(4):546-62, http://dx.doi.org/10.1016/0002-8703(73)90502-4.
http://dx.doi.org/10.1016/0002-8703(73)9...
), in most cases worldwide, VO2max is estimated rather than directly measured (44. Araújo CG, Herdy AH, Stein R. Maximum oxygen consumption measurement: valuable biological marker in health and in sickness. Arq Bras Cardiol. 2013;100(4):e51-3, http://dx.doi.org/10.5935/abc.20130085.
http://dx.doi.org/10.5935/abc.20130085...
,1313. Lang PB, Latin RW, Berg KE, Mellion MB. The accuracy of the ACSM cycle ergometry equation. Med Sci Sports Exerc. 1992;24(2):272-6, http://dx.doi.org/10.1249/00005768-199202000-00019.
http://dx.doi.org/10.1249/00005768-19920...
), often resulting in significant errors for any given subject. Our study addresses this issue by attempting to identify the impact, if any, of central obesity in the EE of VO2max. This may be especially relevant in the current era of obesity (66. Berry MJ, Storsteen JA, Woodard CM. Effects of body mass on exercise efficiency and VO2 during steady-state cycling. Med Sci Sports Exerc. 1993;25(9):1031-7, http://dx.doi.org/10.1249/00005768-199309000-00010.
http://dx.doi.org/10.1249/00005768-19930...
). While it is reasonable to estimate VO2max, these equations should be population-specific to account for the specific features of different populations, including body habitus.
Our study was uniquely focused on reducing the magnitude of error in estimating VO2max by considering separate population-specific equations for men and women. The merit of this approach was substantiated by noting that the magnitude of EE of VO2max was similar for men and women and that there were no other significant gender differences related to VO2max. After having previously developed these equations (1212. Souza e Silva CG, Araújo CG. Sex-specific equations to estimate maximum oxygen uptake in cycle ergometry. Arq Bras Cardiol. 2015;105(4):381-9, http://dx.doi.org/10.5935/abc.20150089.
http://dx.doi.org/10.5935/abc.20150089...
), in this study, we attempted to evaluate the influence of another potential modulator, central obesity, on the EE of VO2max. This was based on the assumption that this variable may adversely decrease mechanical efficiency and, consequently, increase the EE. In the current analysis, rather than proposing specific equations that could correct for central obesity, we focused on analyzing the consistency of these influences and potential gender differences.
When estimating VO2max from the peak workload achieved during maximal exercise testing, some variables may influence the EE, including body composition. First, the relationship between workload and oxygen consumption during cycling, that is, the net mechanical efficiency, has been shown to vary among lean and obese individuals. Hulens et al. (1414. Hulens M, Vansant G, Lysens R, Claessens AL, Muls E. Exercise capacity in lean versus obese women. Scand J Med Sci Sports. 2001;11(5):305-9, http://dx.doi.org/10.1034/j.1600-0838.2001.110509.x.
http://dx.doi.org/10.1034/j.1600-0838.20...
) examined differences in exercise capacity in a large sample of lean and obese women undergoing maximal cycle ergometer testing. Net mechanical efficiency, calculated as the ratio between workload and oxygen consumed above rest to maximal exercise, was lower in women with higher relative body fat. Similarly, Lafortuna et al. (1515. Lafortuna CL, Proietti M, Agosti F, Sartorio A. The energy cost of cycling in young obese women. Eur J Appl Physiol. 2006;97(1):16-25, http://dx.doi.org/10.1007/s00421-006-0137-5.
http://dx.doi.org/10.1007/s00421-006-013...
) compared expenditure during cycling in young women of varied body habitus. Women with higher fat body mass demonstrated reduced mechanical efficiency, presumably due to the extra energy required to facilitate the associated body movement. Anton-Kuchly et al. (1616. Anton-Kuchly B, Roger P, Varene P. Determinants of increased energy cost of submaximal exercise in obese subjects. J Appl Physiol Respir Environ Exerc Physiol. 1984;56(1):18-23.) found that obese men and women exhibited a higher energy cost during submaximal exercise than their leaner counterparts, possibly due to the added energy requirements associated with muscular postural activity and/or moving the lower extremities.
Another possible explanation for our results is a difference in resting VO2. As previously described (1212. Souza e Silva CG, Araújo CG. Sex-specific equations to estimate maximum oxygen uptake in cycle ergometry. Arq Bras Cardiol. 2015;105(4):381-9, http://dx.doi.org/10.5935/abc.20150089.
http://dx.doi.org/10.5935/abc.20150089...
), gender-specific equations used to estimate VO2max assume that all individuals consume 3.5 mL of oxygen per kg of body weight per minute at rest. However, subjects with increased fat mass may have a higher absolute resting VO2 (1717. Ravussin E, Burnand B, Schutz Y, Jéquier E. Twenty-four-hour energy expenditure and resting metabolic rate in obese, moderately obese, and control subjects. Am J Clin Nutr. 1982;35(3):566-73.). Unfortunately, due to difficulties in establishing a standardized protocol for the accurate measurement of resting VO2 and, therefore, for its use in routine clinical practice (1818. Cunha FA, Midgley AW, Monteiro W, Freire R, Lima T, Farinatti PT. How long does it take to achieve steady state for an accurate assessment of resting VO? in healthy men? Eur J Appl Physiol. 2013;113(6):1441-7, http://dx.doi.org/10.1007/s00421-012-2571-x.
http://dx.doi.org/10.1007/s00421-012-257...
), we were unable to quantify this variable in our study.
Previous studies have addressed other variables in obese individuals that may influence the cardiovascular response to exercise. Gondoni et al. (1919. Gondoni LA, Titon AM, Nibbio F, Augello G, Caetani G, Liuzzi A. Heart rate behavior during an exercise stress test in obese patients. Nutr Metab Cardiovasc Dis. 2009;19(3):170-6, http://dx.doi.org/10.1016/j.numecd.2008.07.001.
http://dx.doi.org/10.1016/j.numecd.2008....
) compared the HR response to progressive exercise in obese and lean individuals and reported that obese subjects had a blunted HR response and a reduced associated exercise tolerance. Fornitano et al. (2020. Fornitano LD, Godoy MF. Exercise testing in individuals with morbid obesity. Obes Surg. 2010;20(5):583-8, http://dx.doi.org/10.1007/s11695-008-9692-7.
http://dx.doi.org/10.1007/s11695-008-969...
) noted differing clinical, electrocardiographic and hemodynamic responses to conventional exercise testing in morbidly obese individuals versus their overweight counterparts, reinforcing the notion that body composition should be considered when evaluating exercise performance.
This study has some methodologic features that strengthen the relevance of our findings. All CPET data were collected by four physicians in the same clinic, using the same equipment, under controlled environmental conditions and having followed standardized criteria for VO2max determination. The retrospective analysis was undertaken by only one investigator who was not directly involved in data collection. The sample size was considerably large and most likely reflected the clinical profiles typically seen in a medically based office practice.
There are several limitations of this study that should be acknowledged. First, age is a potential confounding variable when considering mechanical efficiency (2121. Layec G, Hart CR, Trinity JD, Le Fur Y, Jeong EK, Richardson RS. Skeletal muscle work efficiency with age: the role of non-contractile processes. Clin Sci (Lond). 2015;128(3):213-23, http://dx.doi.org/10.1042/CS20140274.
http://dx.doi.org/10.1042/CS20140274...
). Indeed, there were significant age differences among our subjects, both men and women, in the different quartile ranges, with those categorized in Q4 being significantly older. However, these subjects also demonstrated low measured VO2max even when adjusted for age-predicted values, which suggests that age was not the only variable that contributed to the difference in mechanical efficiency. Second, subjects were not specifically evaluated based on the use of different medications (i.e., ß-blockers), which may affect mitochondrial function (2222. Desai CS, Martin SS, Blumenthal RS. Non-cardiovascular effects associated with statins. BMJ. 2014;349:g3743, http://dx.doi.org/10.1136/bmj.g3743.
http://dx.doi.org/10.1136/bmj.g3743...
,2323. Golomb BA, Evans MA. Statin adverse effects: a review of the literature and evidence for a mitochondrial mechanism. Am J Cardiovasc Drugs. 2008;8(6):373-418, http://dx.doi.org/10.2165/0129784-200808060-00004.
http://dx.doi.org/10.2165/0129784-200808...
), especially in the case of statins, and, in theory, the measured-estimated VO2max difference. Third, there are several techniques for categorizing obesity, ranging from more sophisticated approaches, such as computer tomography and DEXA, to simpler methods, such as bioimpedance or anthropometric measurements (2424. Duren DL, Sherwood RJ, Czerwinski SA, Lee M, Choh AC, Siervogel RM, et al. Body composition methods: comparisons and interpretation. J Diabetes Sci Technol. 2008;2(6):1139-46, http://dx.doi.org/10.1177/193229680800200623.
http://dx.doi.org/10.1177/19322968080020...
). Although anthropometric measurements are considered somewhat less precise, they are likely preferable and are considered reasonably accurate for rapidly evaluating the large number of subjects encountered during daily clinical practice. Accordingly, these issues should be considered in the design of future studies.
Therefore, in agreement with our previous reports (44. Araújo CG, Herdy AH, Stein R. Maximum oxygen consumption measurement: valuable biological marker in health and in sickness. Arq Bras Cardiol. 2013;100(4):e51-3, http://dx.doi.org/10.5935/abc.20130085.
http://dx.doi.org/10.5935/abc.20130085...
,1212. Souza e Silva CG, Araújo CG. Sex-specific equations to estimate maximum oxygen uptake in cycle ergometry. Arq Bras Cardiol. 2015;105(4):381-9, http://dx.doi.org/10.5935/abc.20150089.
http://dx.doi.org/10.5935/abc.20150089...
,2525. de Souza e Silva CG, Franklin BA, Forman DE, Araújo CG. Influence of age in estimating maximal oxygen uptake. J Geriatr Cardiol. 2016;13(2):126-31, http://dx.doi.org/10.11909/j.issn.1671-5411.2016.02.010.
http://dx.doi.org/10.11909/j.issn.1671-5...
), the application of a single equation to estimate VO2max may lead to modest errors in some subjects and to significant errors in others. In our study, the application of a sex-specific equation identified a distinct magnitude of error when subjects with higher and lower WHtR were compared. In subjects with higher central obesity, VO2max values were systematically overestimated, while the opposite occurred among subjects with less central obesity, although to a lesser degree.
Although the aforementioned studies used BMI to categorize obesity and its relationship to cardiorespiratory fitness and mechanical efficiency, it is widely recognized that BMI has numerous limitations in assessing body composition, because it fails to differentiate body fat from lean mass, and in providing indices of overall adiposity, fat distribution and metabolic risk (2626. Hsieh SD, Yoshinaga H, Muto T. Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes Relat Metab Disord. 2003;27(5):610-6, http://dx.doi.org/10.1038/sj.ijo.0802259.
http://dx.doi.org/10.1038/sj.ijo.0802259...
27. Ricardo DR, Araujo CG. Body mass index: a scientific evidence-based inquiry. Arq Bras Cardiol. 2002;79(1):61-78, http://dx.doi.org/10.1590/S0066-782X2002001000007.
http://dx.doi.org/10.1590/S0066-782X2002...
-2828. Smalley KJ, Knerr AN, Kendrick ZV, Colliver JA, Owen OE. Reassessment of body mass indices. Am J Clin Nutr. 1990;52(3):405-8.). Moreover, BMI may be influenced by age, gender and ethnicity (2626. Hsieh SD, Yoshinaga H, Muto T. Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes Relat Metab Disord. 2003;27(5):610-6, http://dx.doi.org/10.1038/sj.ijo.0802259.
http://dx.doi.org/10.1038/sj.ijo.0802259...
), further limiting its ability to differentiate normal weight, overweight and obese subjects.
In the present study, the WHtR provided a simple, non-invasive, anthropometric index to quantify central obesity. Moreover, unlike BMI, WHtR values are not significantly influenced by ethnic differences, age and sex, making it possible to compare central obesity among a heterogeneous cohort of men and women. Our selection of central obesity rather than overall obesity as the variable that may influence mechanical efficiency and the EE of VO2max was based on recent studies that have demonstrated that fat distribution has important clinical implications. Because central obesity is strongly related to visceral fat and increased cardiovascular risk (2929. Lee CM, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol. 2008;61(7):646-53, http://dx.doi.org/10.1016/j.jclinepi.2007.08.012.
http://dx.doi.org/10.1016/j.jclinepi.200...
), it seems likely that WHtR is a better prognostic discriminator than BMI (3030. Coutinho T, Goel K, Corrêa de Sá D, Carter RE, Hodge DO, Kragelund C, et al. Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease: role of "normal weight central obesity". J Am Coll Cardiol. 2013;61(5):553-60, http://dx.doi.org/10.1016/j.jacc.2012.10.035.
http://dx.doi.org/10.1016/j.jacc.2012.10...
,3131. Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117(13):1658-67, http://dx.doi.org/10.1161/CIRCULATIONAHA.107.739714.
http://dx.doi.org/10.1161/CIRCULATIONAHA...
,3232. Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275-86, http://dx.doi.org/10.1111/j.1467-789X.2011.00952.x.
http://dx.doi.org/10.1111/j.1467-789X.20...
).
In conclusion, central obesity as estimated by the WHtR influences the magnitude of the EE of VO2max, with a higher EE in those at the upper end of the WHtR distribution. For subjects classified in the upper WHtR quartile (men > 0.612 and women > 0.572), the use of currently available equations for estimating VO2max may lead to excessive errors and inaccuracies in clinical practice, especially when using functional capacity for risk stratification or in surgical clearance algorithms.
ACKNOWLEDGMENTS
Partial financial support for this study was provided by CNPq and FAPERJ. Preliminary data were presented at EUROPREVENT 2015.
REFERENCES
-
1Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN. Fitness vs. fatness on all-cause mortality: a meta-analysis. Prog Cardiovasc Dis. 2014;56(4):382-90, http://dx.doi.org/10.1016/j.pcad.2013.09.002
» http://dx.doi.org/10.1016/j.pcad.2013.09.002 -
2Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85(4):546-62, http://dx.doi.org/10.1016/0002-8703(73)90502-4
» http://dx.doi.org/10.1016/0002-8703(73)90502-4 -
3Storer TW, Davis JA, Caiozzo VJ. Accurate prediction of VO2max in cycle ergometry. Med Sci Sports Exerc. 1990;22(5):704-12.
-
4Araújo CG, Herdy AH, Stein R. Maximum oxygen consumption measurement: valuable biological marker in health and in sickness. Arq Bras Cardiol. 2013;100(4):e51-3, http://dx.doi.org/10.5935/abc.20130085
» http://dx.doi.org/10.5935/abc.20130085 -
5Whipp BJ, Wasserman K. Efficiency of muscular work. J Appl Physiol. 1969;26(5):644-8.
-
6Berry MJ, Storsteen JA, Woodard CM. Effects of body mass on exercise efficiency and VO2 during steady-state cycling. Med Sci Sports Exerc. 1993;25(9):1031-7, http://dx.doi.org/10.1249/00005768-199309000-00010
» http://dx.doi.org/10.1249/00005768-199309000-00010 -
7de Oliveira A, Cocate PG, Hermsdorff HH, Bressan J, de Silva MF, Rodrigues JA, et al. Waist circumference measures: cutoff analyses to detect obesity and cardiometabolic risk factors in a Southeast Brazilian middle-aged men population--a cross-sectional study. Lipids Health Dis. 2014;13:141, http://dx.doi.org/10.1186/1476-511X-13-141
» http://dx.doi.org/10.1186/1476-511X-13-141 -
8Ramos PS, Sardinha A, Nardi AE, de Araújo CG. Cardiorespiratory optimal point: a submaximal exercise variable to assess panic disorder patients. PLoS One. 2014;9(8):e104932, http://dx.doi.org/10.1371/journal.pone.0104932
» http://dx.doi.org/10.1371/journal.pone.0104932 -
9Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377-81, http://dx.doi.org/10.1249/00005768-198205000-00012
» http://dx.doi.org/10.1249/00005768-198205000-00012 -
10Jones NL, Campbell EJM, Edwards RHT, Robertson DG. Clinical Exercise Testing. WB Saunders. Philadelphia;1995. pp 202.
-
11Duarte CV, Araujo CG. Cardiac vagal index does not explain age-independent maximal heart rate. Int J Sports Med. 2013;34(6):502-6.
-
12Souza e Silva CG, Araújo CG. Sex-specific equations to estimate maximum oxygen uptake in cycle ergometry. Arq Bras Cardiol. 2015;105(4):381-9, http://dx.doi.org/10.5935/abc.20150089
» http://dx.doi.org/10.5935/abc.20150089 -
13Lang PB, Latin RW, Berg KE, Mellion MB. The accuracy of the ACSM cycle ergometry equation. Med Sci Sports Exerc. 1992;24(2):272-6, http://dx.doi.org/10.1249/00005768-199202000-00019
» http://dx.doi.org/10.1249/00005768-199202000-00019 -
14Hulens M, Vansant G, Lysens R, Claessens AL, Muls E. Exercise capacity in lean versus obese women. Scand J Med Sci Sports. 2001;11(5):305-9, http://dx.doi.org/10.1034/j.1600-0838.2001.110509.x
» http://dx.doi.org/10.1034/j.1600-0838.2001.110509.x -
15Lafortuna CL, Proietti M, Agosti F, Sartorio A. The energy cost of cycling in young obese women. Eur J Appl Physiol. 2006;97(1):16-25, http://dx.doi.org/10.1007/s00421-006-0137-5
» http://dx.doi.org/10.1007/s00421-006-0137-5 -
16Anton-Kuchly B, Roger P, Varene P. Determinants of increased energy cost of submaximal exercise in obese subjects. J Appl Physiol Respir Environ Exerc Physiol. 1984;56(1):18-23.
-
17Ravussin E, Burnand B, Schutz Y, Jéquier E. Twenty-four-hour energy expenditure and resting metabolic rate in obese, moderately obese, and control subjects. Am J Clin Nutr. 1982;35(3):566-73.
-
18Cunha FA, Midgley AW, Monteiro W, Freire R, Lima T, Farinatti PT. How long does it take to achieve steady state for an accurate assessment of resting VO? in healthy men? Eur J Appl Physiol. 2013;113(6):1441-7, http://dx.doi.org/10.1007/s00421-012-2571-x
» http://dx.doi.org/10.1007/s00421-012-2571-x -
19Gondoni LA, Titon AM, Nibbio F, Augello G, Caetani G, Liuzzi A. Heart rate behavior during an exercise stress test in obese patients. Nutr Metab Cardiovasc Dis. 2009;19(3):170-6, http://dx.doi.org/10.1016/j.numecd.2008.07.001
» http://dx.doi.org/10.1016/j.numecd.2008.07.001 -
20Fornitano LD, Godoy MF. Exercise testing in individuals with morbid obesity. Obes Surg. 2010;20(5):583-8, http://dx.doi.org/10.1007/s11695-008-9692-7
» http://dx.doi.org/10.1007/s11695-008-9692-7 -
21Layec G, Hart CR, Trinity JD, Le Fur Y, Jeong EK, Richardson RS. Skeletal muscle work efficiency with age: the role of non-contractile processes. Clin Sci (Lond). 2015;128(3):213-23, http://dx.doi.org/10.1042/CS20140274
» http://dx.doi.org/10.1042/CS20140274 -
22Desai CS, Martin SS, Blumenthal RS. Non-cardiovascular effects associated with statins. BMJ. 2014;349:g3743, http://dx.doi.org/10.1136/bmj.g3743
» http://dx.doi.org/10.1136/bmj.g3743 -
23Golomb BA, Evans MA. Statin adverse effects: a review of the literature and evidence for a mitochondrial mechanism. Am J Cardiovasc Drugs. 2008;8(6):373-418, http://dx.doi.org/10.2165/0129784-200808060-00004
» http://dx.doi.org/10.2165/0129784-200808060-00004 -
24Duren DL, Sherwood RJ, Czerwinski SA, Lee M, Choh AC, Siervogel RM, et al. Body composition methods: comparisons and interpretation. J Diabetes Sci Technol. 2008;2(6):1139-46, http://dx.doi.org/10.1177/193229680800200623
» http://dx.doi.org/10.1177/193229680800200623 -
25de Souza e Silva CG, Franklin BA, Forman DE, Araújo CG. Influence of age in estimating maximal oxygen uptake. J Geriatr Cardiol. 2016;13(2):126-31, http://dx.doi.org/10.11909/j.issn.1671-5411.2016.02.010
» http://dx.doi.org/10.11909/j.issn.1671-5411.2016.02.010 -
26Hsieh SD, Yoshinaga H, Muto T. Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes Relat Metab Disord. 2003;27(5):610-6, http://dx.doi.org/10.1038/sj.ijo.0802259
» http://dx.doi.org/10.1038/sj.ijo.0802259 -
27Ricardo DR, Araujo CG. Body mass index: a scientific evidence-based inquiry. Arq Bras Cardiol. 2002;79(1):61-78, http://dx.doi.org/10.1590/S0066-782X2002001000007
» http://dx.doi.org/10.1590/S0066-782X2002001000007 -
28Smalley KJ, Knerr AN, Kendrick ZV, Colliver JA, Owen OE. Reassessment of body mass indices. Am J Clin Nutr. 1990;52(3):405-8.
-
29Lee CM, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol. 2008;61(7):646-53, http://dx.doi.org/10.1016/j.jclinepi.2007.08.012
» http://dx.doi.org/10.1016/j.jclinepi.2007.08.012 -
30Coutinho T, Goel K, Corrêa de Sá D, Carter RE, Hodge DO, Kragelund C, et al. Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease: role of "normal weight central obesity". J Am Coll Cardiol. 2013;61(5):553-60, http://dx.doi.org/10.1016/j.jacc.2012.10.035
» http://dx.doi.org/10.1016/j.jacc.2012.10.035 -
31Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117(13):1658-67, http://dx.doi.org/10.1161/CIRCULATIONAHA.107.739714
» http://dx.doi.org/10.1161/CIRCULATIONAHA.107.739714 -
32Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13(3):275-86, http://dx.doi.org/10.1111/j.1467-789X.2011.00952.x
» http://dx.doi.org/10.1111/j.1467-789X.2011.00952.x
Publication Dates
-
Publication in this collection
Nov 2016
History
-
Received
7 Mar 2016 -
Reviewed
11 May 2016 -
Accepted
5 Aug 2016