Abstract
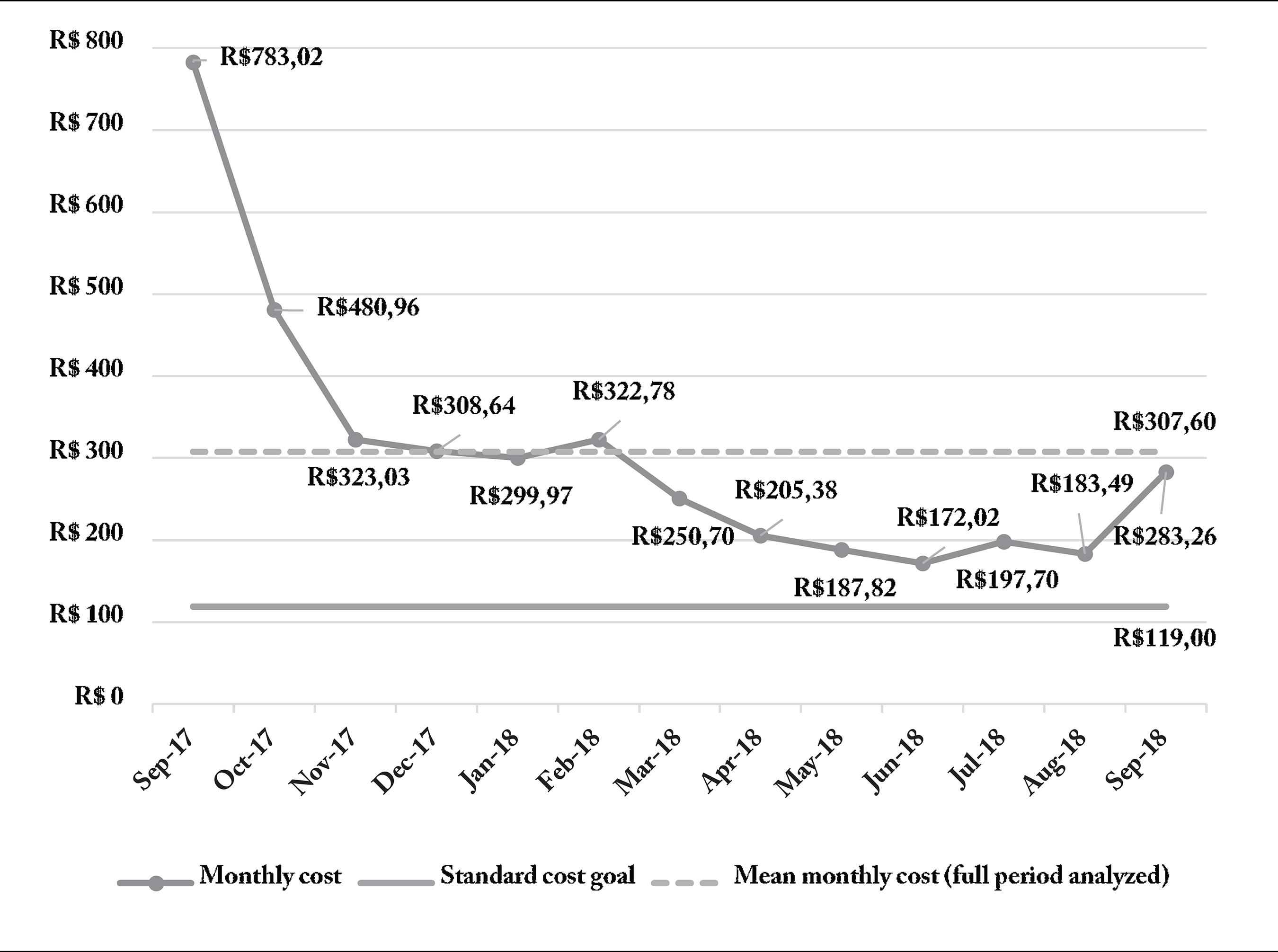
This study evaluated the cost of public telediagnostic service in ophthalmology. The time-driven activity-based costing method (TDABC) was adopted to examine the cost components related to teleophthalmology. This method allowed us to establish the standard unit cost of telediagnosis, given the installed capacity and utilization of professionals. We considered data from one year of telediagnoses and evaluated the cost per telediagnosis change throughout technology adaptation in the system. The standard cost calculated by distance ophthalmic diagnosis was approximately R$ 119, considering the issuance of 1,080 monthly ophthalmic telediagnostic reports. We identified an imbalance between activities, which suggests the TDABC method’s ability to guide management actions and improve resource allocation. The actual unit cost fell from R$ 783 to R$ 283 over one year – with room to approach the estimated standard cost. Partial economic evaluations contribute significantly to support the incorporation of new technologies. The TDABC method deserves prominence, as it enables us to retrieve more accurate information on the cost of technology, improving the scalability and management capacity of the healthcare system.
Key words
Health Technology Assessment; Telemedicine; Teleophthalmology
Resumo
Este estudo avaliou o custo de um serviço público de telediagnóstico em oftalmologia. O método de custeio baseado em atividades e tempo (TDABC) foi adotado para examinar os componentes de custos relacionados à teleoftalmologia. Com este método, também foi possível estabelecer o custo unitário padrão que o telediagnóstico deveria ter, dada a capacidade instalada e utilização de profissionais. Dados de um ano de telediagnósticos foram considerados, e avaliou-se a mudança do custo por telediagnóstico ao longo do período de adaptação da tecnologia no sistema. O custo padrão calculado por diagnóstico oftalmológico a distância foi de R$ 119, considerando a emissão de 1.080 laudos de telediagnóstico oftalmológico por mês. Foi identificado um desequilíbrio entre as atividades que sugere a capacidade do método TDABC orientar ações de gestão e melhoria na alocação dos recursos. Ao longo de um ano, o custo unitário real passou de R$ 783 para R$ 283, ainda havendo espaço para se aproximar do custo padrão estimado. Avaliações econômicas parciais possuem importante aporte para subsidiar a incorporação de novas tecnologias. O TDABC merece destaque nesse sentido, pois permite obter informações mais precisas sobre custo da tecnologia, melhorando a capacidade de dimensionamento e gerenciamento da organização de saúde.
Palavras-chave
Avaliação de Tecnologias em Saúde; Telemedicina; Teleoftalmologia
Introduction
Telemedicine can be defined as the use of information and communication technologies in healthcare, enabling the provision of services related to improving patient access to care11 Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med 2017; 377(16):1585-1592.. The emergence of new technological capacities and their integration in health care delivery systems provides us with opportunities to improve clinical care, especially in cases where distance is a critical factor11 Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med 2017; 377(16):1585-1592.,22 Maldonado JMSV, Marques AB, Cruz A. Telemedicina: desafios à sua difusão no Brasil. Cad Saude Publica 2016; 32(Supl. 2):e00155615.. In a reality in which health systems are under pressure to reduce costs and, at the same time, improve the quality, access, and equity of the service33 Halvorsen PA, Kristiansen IS. Radiology services for remote communities: cost minimisation study of telemedicine. BMJ 1996; 312(7042):1333-1336., one must explore tools that prove to be an alternative to this changing scenario.
Growing concerns about sustainability and the expected scarcity of resources arouse interest in exploring the potential of telemedicine to deal with many challenges faced by primary health care (PHC)44 Bashshur RL, Howell JD, Krupinski EA, Harms KM, Bashshur N, Doarn CR. The Empirical Foundations of Telemedicine Interventions in Primary Care. Telemed E-Health 2016; 22(5):342-375.. Among the values associated with the adoption of telemedicine services in PHC are collaboration, with the swift access of patients to high-complexity centers55 Lamminen H, Lamminen J, Ruohonen K, Uusitalo H. A cost study of teleconsultation for primary-care ophthalmology and dermatology. J Telemed Telecare 2001; 7(3):167-173., higher resolution at the baseline level and a reduced number of referrals to other municipalities for specialized care66 Hjelm NM. Benefits and drawbacks of telemedicine. J Telemed Telecare 2005; 11(2):60-70., besides being an ally for monitoring and controlling the quality of patient care delivery77 Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015; 9:CD002098..
Most telemedicine services that focus on diagnosis and clinical management are already routinely supplied in more developed countries. In this context, recent publications treat these services as effective in the management of patients with chronic diseases88 Grustam AS, Severens JL, van Nijnatten J, Koymans R, Vrijhoef HJM. Cost-effectiveness of telehealth interventions for chronic heart failure patients: a literature review. Int J Technol Assess Health Care 2014; 30(1):59-68., such as, for example, ECG reports99 Kotb A, Cameron C, Hsieh S, Wells G. Comparative Effectiveness of Different Forms of Telemedicine for Individuals with Heart Failure (HF): A Systematic Review and Network Meta-Analysis. PLoS One 2015; 10(2):e0118681., screening for diabetic retinopathy1010 Rachapelle S, Legood R, Alavi Y, Lindfield R, Sharma T, Kuper H, Polack S. The Cost-Utility of Telemedicine to Screen for Diabetic Retinopathy in India. Ophthalmology 2013; 120(3):566-573.,1111 Castillo-Riquelme MC, Lord J, Moseley MJ, Fielder AR, Haines L. Cost-effectiveness of digital photographic screening for retinopathy of prematurity in the United Kingdom. Int J Technol Assess Health Care 2004; 20(2):201-213. and glaucoma1212 Thomas S, Hodge W, Malvankar-Mehta M. The Cost-Effectiveness Analysis of Teleglaucoma Screening Device. PLoS One 2015; 10(9):e0137913., patient guidance through mobile apps1313 Rush KL, Hatt L, Janke R, Burton L, Ferrier M, Tetrault M. The efficacy of telehealth delivered educational approaches for patients with chronic diseases: A systematic review. Patient Educ Couns 2018; 101(8):1310-1321. and cardiac rehabilitation1414 Hamilton SJ, Mills B, Birch EM, Thompson SC. Smartphones in the secondary prevention of cardiovascular disease: a systematic review. BMC Cardiovasc Disord 2018; 18(1):25..
Brazil is a country with unique opportunities for the development and applications of telemedicine, given its geographical distribution and inability to meet the demand for face-to-face care22 Maldonado JMSV, Marques AB, Cruz A. Telemedicina: desafios à sua difusão no Brasil. Cad Saude Publica 2016; 32(Supl. 2):e00155615.,1515 Harzheim E, Gonçalves MR, Umpierre RN, Siqueira ACS, Katz N, Agostinho MR, Oliveira EB, Basso J, Roman R, Moro RG, Pilz C, Heinzelmann RS, Schmitz CAA, Hauser L, Mengue SS. Telehealth in Rio Grande do Sul, Brazil: Bridging the Gaps. Telemed E-Health 2016; 22(11):938-944.,1616 Gonçalves MR, Umpierre RN, D'Avila OP, Katz N, Mengue SS, Siqueira ACS, Carrard VC, Schmitz CAA, Molina-Bastos CG, Rados DV, Agostinho MR, Oliveira EB, Roman R, Basso J, Pfeil JN, Mendonça MVA, Moro RG, Frank T, Stürmer PL, Harzheim E. Expanding Primary Care Access: A Telehealth Success Story. Ann Fam Med 2017; 15(4):383.. Data from the management system of specialized outpatient appointments provided by the State Health Secretariat of Rio Grande do Sul reveal that, at the end of 2016, the number of people waiting for a specialized ophthalmology visit in the capital was about 10 times higher than the monthly offer of visits, translating into a maximum 19-month waiting period1717 Secretaria de Saúde Estadual. Gestão e Tecnologia em Saúde Sistema AGHOS. 2016 (não publicado).. Telemedicine technologies can be a significant advance in the provision of health care in this context and can play a strategic role in the consolidation of Health Care Networks and improved health of the population1818 Brasil. Ministério da Saúde (MS), Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Departamento de Ciência e Tecnologia. Guia Metodológico para Programas e Serviços em Telessaúde [documento na Internet]. Brasilia: MS; 2019 [acessado 2019 Set 4]. Disponível em: https://www.telessaude.unifesp.br/images/docs/Guia_Monitoramento_Telessaude_WEB.pdf.
Existing economic assessments of the subject are still recent and do not allow an assertive conclusion about the economic feasibility of the implementation in the Brazilian Health System1919 Lin M, Yuan W, Huang T, Zhang H, Mai J, Wang J. Clinical effectiveness of telemedicine for chronic heart failure: a systematic review and meta-analysis. J Investig Med 2017; 65(5):899-911.. It is known that the scientific and financial investments required to introduce these technologies into the system are high2020 Iribarren SJ, Cato K, Falzon L, Stone PW. What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS One 2017; 12(2):e0170581., enhancing the importance of conducting accurate economic analyses to guide decisions regarding the implementation of telemedicine services1616 Gonçalves MR, Umpierre RN, D'Avila OP, Katz N, Mengue SS, Siqueira ACS, Carrard VC, Schmitz CAA, Molina-Bastos CG, Rados DV, Agostinho MR, Oliveira EB, Roman R, Basso J, Pfeil JN, Mendonça MVA, Moro RG, Frank T, Stürmer PL, Harzheim E. Expanding Primary Care Access: A Telehealth Success Story. Ann Fam Med 2017; 15(4):383.,2020 Iribarren SJ, Cato K, Falzon L, Stone PW. What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS One 2017; 12(2):e0170581..
Understanding cost information is challenging in the assessment of technologies in the Brazilian public sector, and, while counterintuitive, the practice of measuring costs is not adequately disseminated among health centers2121 Souza RJSP, Mattedi AP, Rezende ML, Corrêa MP, Duarte EM. Estimativa do custo do tratamento de câncer de pele tipo melanoma no Estado de São Paulo - Brasil. An Bras Dermatol 2009 ;84(3):237-343.. One reason is the use of different costing methods, the lack of definition of standards, and a computerized cost system in public institutions, which hinders comparability between different health services2222 Etges APBS, Cruz LN, Notti RK, Neyeloff JL, Schlatter RP, Astigarraga CC, Falavigna M, Polanczyk CA. An 8-step framework for implementing time-driven activity-based costing in healthcare studies. Eur J Health Econ 2019; 20(8):1133-1145.. The lack of a detailed understanding of the actual cost of providing care to the patient is commonly the central problem of scalability in health expenditures2323 Martin JA, Mayhew CR, Morris AJ, Bader AM, Tsai MH, Urman RD. Using Time-Driven Activity-Based Costing as a Key Component of the Value Platform: A Pilot Analysis of Colonoscopy, Aortic Valve Replacement and Carpal Tunnel Release Procedures. J Clin Med Res 2018; 10(4):314-320.. In this sense, micro-costing estimates are the gold standard for cost valuation as they provide a high degree of detail, especially for more complex services or where human resources are of higher weight2424 Brasil. Ministério da Saúde (MS), Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Departamento de Ciência e Tecnologia. Diretrizes metodológicas?: Diretriz de Avaliação Econômica. Brasília: MS; 2014., as is the case with telemedicine services.
Some micro-costing methods used in the health area since the 1980s are the absorption costing method and Activity-Based Costing (ABC), whose primary assumption is to correct some deficiencies in traditional methods, such as proportional apportionments2525 Kaplan RS, Cooper R. Custo e desempenho: administre seus custos para ser mais competitivo. São Paulo: Futura; 1998.. However, the implementation of the traditional ABC model is challenging for many organizations due to the high implementation costs in interviewing people for the initial ABC method survey2626 Kaplan RS, Anderson SR. The Innovation of Time-Driven Activity-Based Costing. J Cost Manag 2007; 21(2):5-15..
To overcome these limitations, Kaplan and Anderson developed the Time-Driven Activity-Based Costing (TDABC) method2626 Kaplan RS, Anderson SR. The Innovation of Time-Driven Activity-Based Costing. J Cost Manag 2007; 21(2):5-15.. The TDABC aims to measure the cost of services from their actual consumption of resources. Since its initial proposal in 2007, it has been used in several health studies2222 Etges APBS, Cruz LN, Notti RK, Neyeloff JL, Schlatter RP, Astigarraga CC, Falavigna M, Polanczyk CA. An 8-step framework for implementing time-driven activity-based costing in healthcare studies. Eur J Health Econ 2019; 20(8):1133-1145.,2727 Keel G, Savage C, Rafiq M, Mazzocato P. Time-driven activity-based costing in health care: A systematic review of the literature. Health Policy 2017; 121(7):755-763.,2828 Erhun F, Mistry B, Platchek T, Milstein A, Narayanan VG, Kaplan RS. Time-driven activity-based costing of multivessel coronary artery bypass grafting across national boundaries to identify improvement opportunities: study protocol. BMJ 2015; 5(8):e008765.. This method allows identifying individual taxpayers and accounting for the indirect costs necessary to support patient care2929 Chapko MK, Liu C-F, Perkins M, Li Y-F, Fortney JC, Maciejewski ML. Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ 2009; 18(10):1188-1201.. The fundamental principle of this method is that it transforms the cost drivers into equations of time that represent the time required to perform a given activity3030 Heaton HA, Nestler DM, Barry WJ, Helmers RA, Sir MY, Goyal DG, Haas DA, Kaplan RS, Sadosty AT. A Time-Driven Activity-Based Costing Analysis of Emergency Department Scribes. Mayo Clin Proc Innov Qual Outcomes 2019; 3(1):30-34.. Another advantage of using this method when it comes to implementing technologies is that it allows the identification of the standard cost, that is, the cost at the unit level of the service within the anticipated efficiency conditions, also acting as a metric for comparing productivity3131 Martins E. Contabilidade de custos. São Paulo: Atlas; 2008..
This study aims to assess the cost of a telemedicine service (TelessaúdeRS-UFRGS) using the scope of telediagnosis in ophthalmology and, specifically, to assess the cost of learning related to the implementation of the service in PHC.
Methods
As it is a partial economic evaluation, providing information on cost without referring to effectiveness or comparison between alternatives, the organization of the study description was made following the conformities recommended by the Consolidated Health Economic Evaluation Reporting Standards (CHEERS)3232 Husereau D, Drummond M, Petrou S. Consolidated health economic evaluation reporting standards (CHEERS) - Explanation and elaboration: A report of the ISPOR health economic evaluations publication guidelines good reporting practices task force. Value Health 2013; 16(2):231-250..
The study followed the eight-step structure suggested by Etges et al.2222 Etges APBS, Cruz LN, Notti RK, Neyeloff JL, Schlatter RP, Astigarraga CC, Falavigna M, Polanczyk CA. An 8-step framework for implementing time-driven activity-based costing in healthcare studies. Eur J Health Econ 2019; 20(8):1133-1145. to implement costing based on activities in health services: (i) selecting the technology to be evaluated; (ii) mapping the telemedicine service process; (iii) identifying the primary resources used throughout the process; (iv) estimating total cost of each group of resources; (v) estimating the capacity of each resource and calculate the unit capacity cost rate (UCR – R$/h); (vi) analyzing time estimates for each resource used in an activity; (vii) calculating the total cost of patient care; (viii) analyzing cost data.
Selection of the technology to be evaluated
The Telehealth Center of the Federal University of Rio Grande do Sul (TelessaúdeRS-UFRGS) was selected as the telemedicine’s study object1515 Harzheim E, Gonçalves MR, Umpierre RN, Siqueira ACS, Katz N, Agostinho MR, Oliveira EB, Basso J, Roman R, Moro RG, Pilz C, Heinzelmann RS, Schmitz CAA, Hauser L, Mengue SS. Telehealth in Rio Grande do Sul, Brazil: Bridging the Gaps. Telemed E-Health 2016; 22(11):938-944.,1616 Gonçalves MR, Umpierre RN, D'Avila OP, Katz N, Mengue SS, Siqueira ACS, Carrard VC, Schmitz CAA, Molina-Bastos CG, Rados DV, Agostinho MR, Oliveira EB, Roman R, Basso J, Pfeil JN, Mendonça MVA, Moro RG, Frank T, Stürmer PL, Harzheim E. Expanding Primary Care Access: A Telehealth Success Story. Ann Fam Med 2017; 15(4):383., because combating eye diseases is a priority for the World Health Organization (WHO)3333 Dua HS, Singh AD. Global estimates of visual impairment: 2010. Br J Ophthalmol 2012; 96(5):614-618. and because it demands greater interest among managers in knowing the real cost of the procedure. TeleOftalmo is a telemedicine research and service offering project that has been underway since July 2017 in the state of Rio Grande do Sul (RS), Brazil, which receives primary funding from the Ministry of Health, through the Program to Support the Institutional Development of the Unified Health System (PROADI-SUS). It has a command center at the headquarters of TelessaúdeRS-UFRGS and eight remote test rooms distributed in the state of Rio Grande do Sul State. Doctors working in PHC can request the service from their patients. The ophthalmologist issues a telediagnostic report to the requesting physician after evaluating the patient in the remote test room. The latter will then conduct the patient’s case with the help of the information received in the report.
The study horizon used the project data from September 2017, which allowed us to conduct the analysis throughout its implementation and observe the impact of the learning factor on cost. The teleophthalmology command center, where ophthalmologists work, and two remote test rooms in the municipalities of Porto Alegre and Santa Rosa were evaluated. The two rooms studied were the first implemented, and were the only ones in operation at the time of the beginning of this study.
Measuring the actual costs of health technologies is a crucial step to identify their efficiency and subsequent guidance for decision-making3434 Lima SGG, Brito C, Andrade CJC. Health technology assessment in Brazil - an international perspective. Cien Saude Colet 2019; 24(5):1709-1722.. Thus, the analysis was carried out from the perspective of the health system.
Mapping the teleophthalmology service process
The care delivery mapping details the patient’s path within the service offered, in which a starting and ending point must be defined for each patient. The main activities that are part of the treatment flow and the routine activities of the patient are identified, illustrating the current state of a complex system2828 Erhun F, Mistry B, Platchek T, Milstein A, Narayanan VG, Kaplan RS. Time-driven activity-based costing of multivessel coronary artery bypass grafting across national boundaries to identify improvement opportunities: study protocol. BMJ 2015; 5(8):e008765.,3535 Golini R, Kalchschmidt M, Landoni P. Adoption of project management practices: The impact on international development projects of non-governmental organizations. Int J Proj Manag 2015; 33(3):650-663.. This division is essential for the subsequent development of cost and resource allocation equations.
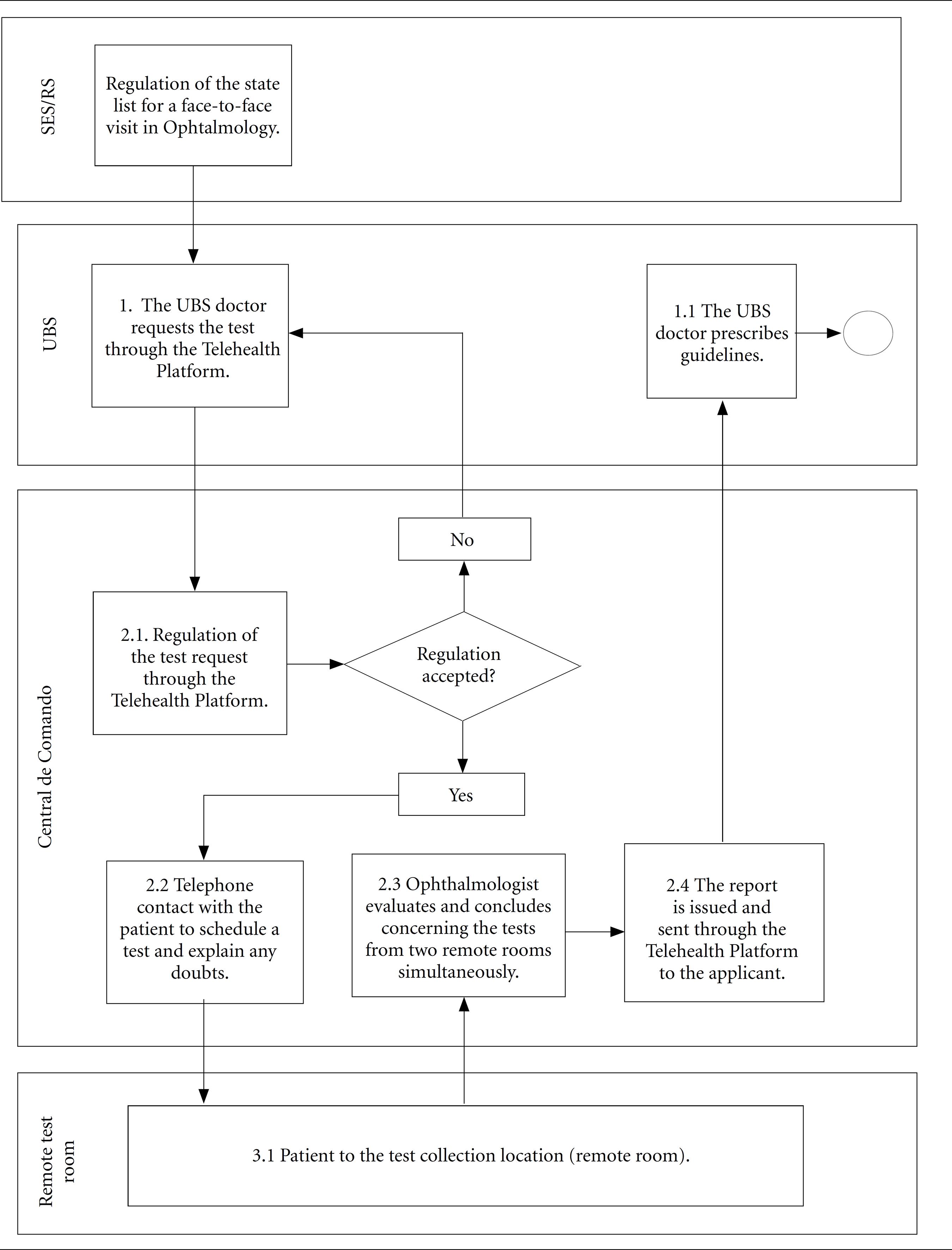
This stage involved interviews with the coordinator and the ophthalmologist plus observations from the service in operation. The map was presented to the professionals involved in the teleophthalmology service for validation. Four macro activities were defined to support the cost evaluation: regulation of the request, telephone contact for scheduling, evaluation of the ophthalmologist, and collection of tests (telediagnosis).
Identification of the primary resources used throughout the process
The resources necessary for its performance were listed for each activity from the details of the teleophthalmology service operation process. The resources were classified as the structure of the remote test room and structure of the teleophthalmology command center, and these consisted of fixed costs and a class of professionals (students, doctors, and nursing technicians).
Estimated total cost for each resource group
All cost items associated with each resource group must be estimated by the financial department of the TelessaúdeRS-UFRGS project.
The physical structure resource of the teleophthalmology command center was valued based on the structuring of the distribution of the fixed costs of the TelessaúdeRS-UFRGS project, which besides the teleophthalmology service has three other telediagnostic services, as well as teleconsulting and regulation. Besides the services, the project is also equipped with support and management departments. To distribute to fixed accounts student compensation, energy salaries, depreciation, rent, and maintenance, we considered, at first, the number of professionals of any class allocated to each department as an apportionment criterion. Subsequently, the costs attributed to the support and management departments were distributed to the departments that carry out some telediagnosis, teleconsulting, or regulation services considering the composition of the workload attributed to each service department as a cost driver. The sum of the direct cost attributed to the command center with that absorbed by the support and management departments represents the cost of the teleophthalmology center structure.
The remote test room structure resource was calculated from the survey of materials, professionals, and the cost of the physical structure of the state health secretariat, where the service takes place in each of the municipalities analyzed.
Estimating the capacity of each resource and calculating the unit capacity cost rate (UCR – R$/h)
The capacities were calculated as per the availability of the workload of professionals who carry out the activities and consume the resources of professionals and the structure, as they all demand human interaction. The macro activities of regulation and telephone contact are carried out by students in the structure of the telediagnosis center; ophthalmologists evaluate the command center, and the nursing technician collects tests in the remote test room.
Subsequently, the remuneration values for the students involved, salaries of salaried professionals, and other bills paid monthly were collected from the financial controller of Telessaúde, which were organized considering the classification made previously concerning the work activities of the professionals.
With the information on capacity and the monthly cost of the resources involved, the time unit contribution rates (UCR) were calculated in R$/h for each activity. Applying equation11 Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med 2017; 377(16):1585-1592., the UCR of each activity was calculated, in which the denominator considers the costs of professionals and the structure consumed by each activity and the capacity and workload of professionals who perform each activity.
Analysis of time estimates for each resource used in an activity
The times required for each activity were estimated from observation and collection of times and movements. These studies can resort to on-site observations plus review by an expert to analyze the real-time during which different resources are devoted to each activity3636 Kaplan RS, Witkowski ML, Hohman JA. Children's Hospital Boston: measuring patient costs. C. R. Math 2012; 3(1):e28..
To this end, the production volume of each activity per hour was observed over two weeks during the working hours of TeleOftalmo and in alternating shifts, converging to an average of the unit time required for an activity unit.
Calculation of the total cost of patient care
The cost and time equations were structured, and the cost per service was calculated. The individual costs were estimated at standard target cost and the actual cost over the months of service operation. Concerning the calculation of the cost per standard service target, a modeling of the service volumes that should be carried out per month in each macro activity was made, based on the available hourly capacity. To get closer to the installed capacity of the service reality, we considered that a portion of 20% of the capacity of each activity is destined for other activities or expected idleness. The 20% share was defined in conjunction with the coordination of the service, which understands that this fraction of time should be dedicated to research activities by professionals. The actual costs were calculated considering the actual volume of attendance per activity performed over a year of follow-up.
Cost data analysis
With the actual and standard costs evaluated, an assessment was made of the capacity balance between activities, identifying opportunities for better distribution of professionals, and the consequent reduction in unit costs. Finally, the impact of the service in the state in which it is inserted was discussed, comparing the volume of attendances made by the teleophthalmology service with the demand for visits in the regions where the service is in operation. This analysis allows us to measure the effects of the scale of use on the costs of this technology, given the high fixed costs necessary to introduce the strategy in the system.
Values are expressed in Brazilian currency (Real – R$), and data from one year of service was monitored from September 2017 to September 2018, expressed as unadjusted values collected per month. For reference purposes, the mean price of international dollars by the Purchasing Power Parity rate in 2017 was 2.0133737 Sistema Gerenciador de Séries Temporais (SGS) [página na Internet]. [acessado 2019 Set 4]. Disponível em: https://www3.bcb.gov.br/sgspub/consultarvalores /consultarValoresSeries.do?method=consultarValores
https://www3.bcb.gov.br/sgspub/consultar...
.
Results
Mapping the process
The process was mapped from interviews with coordinators and implementers of the “TeleOftalmo Project – Olhar Gaúcho”, which sought to understand the flow of activities performed, professionals and location involved, and the need to use specific resources. Figure 1 illustrates the mapped activities.
Mapping of the teleophthalmology process within the primary care system.
SES/RS = State Health Secretariat of Rio Grande do Sul; UBS = Basic Health Unit.
Structuring financial cost data by resources
When conducting the cost distribution, the teleophthalmology command center consolidated a total monthly cost of R$85,000, of which R$10,570 (12%) were for students, R$43,980 (52%) for salaried professionals, R$3,900 (5%) other fixed costs, and R$26,550 (31%) were absorbed from the support and management areas of the TelessaúdeRS-UFRGS center. This result is essential for the calculation of the unit cost rates that will be used in the time measurement equations of a telediagnosis cost. The remote test room cost was consolidated at R$20,600 per month.
Then, the monthly hourly capacity of the professionals who perform each activity was collected to calculate the UCRs. Table 1 describes the costing results for the stages of the teleophthalmology service flow.
Calculation of the cost of telediagnosis and analysis of service balancing
The identified times are shown in Table 2, which, together with the UCRs adjusted to R$/min, allow us to measure the estimated standard cost.
Table 2 indicates that the cost value that should be considered for telediagnosis is R$119. We identified that the system must operate 6,720 regulations, 1,824 calls, 1,080 assessments, and 422 telediagnoses per month in each of the offices, observing the existing capacity levels, to achieve this value and considering the capacity of professionals.
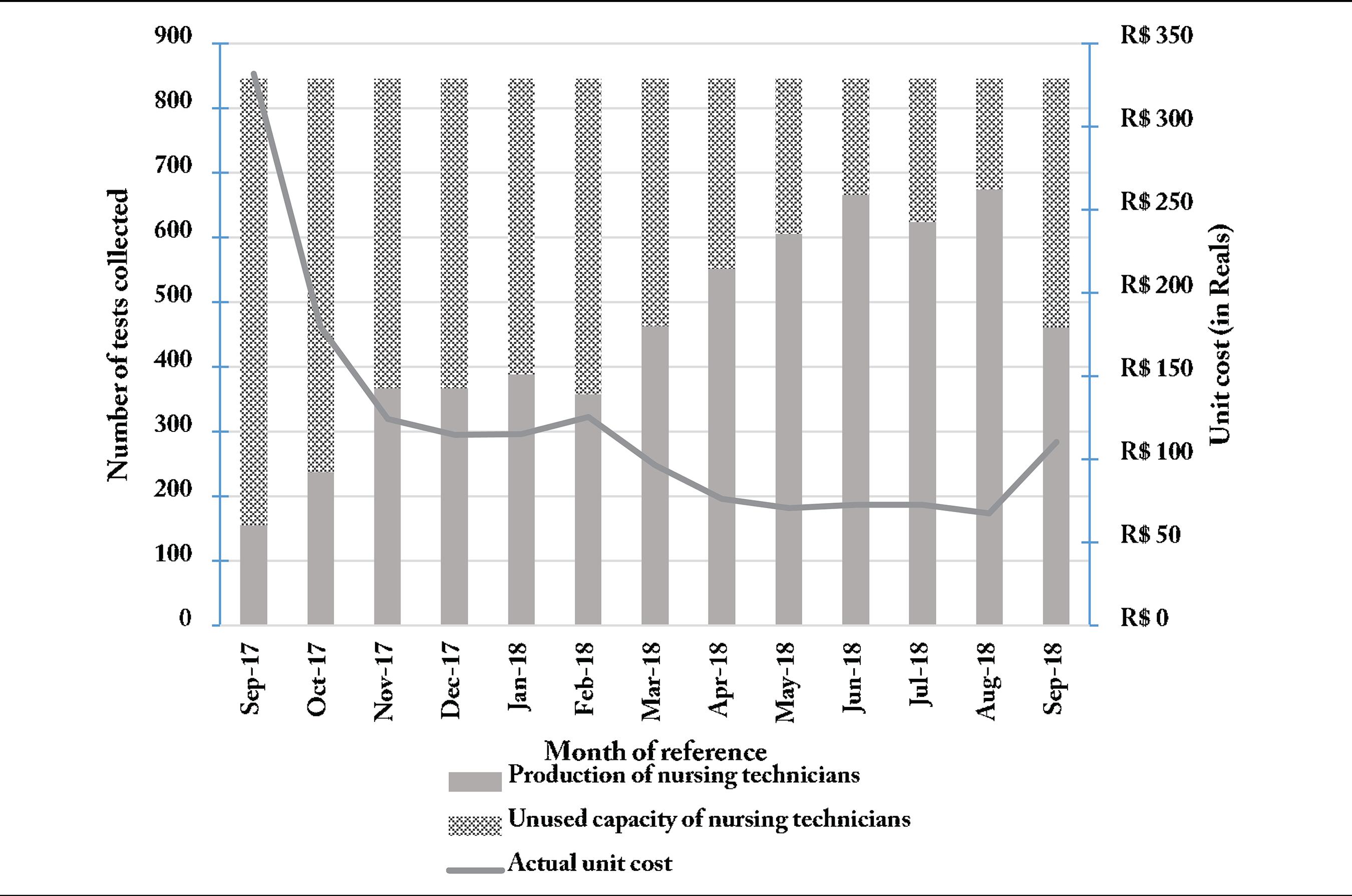
No month has recorded this level of production during the year of operation of the service. Figures 2, 3, and 4 show the professional production ratio and installed capacity not used by them over the months and the trend of the unit cost of each activity.
Relationship between the production of scholarship professionals with the unused capacity for regulation and connection activities and the trend of the unit cost of combined activities.
Relationship between doctors’ production and unused capacity for ophthalmologist care activities and the trend of the unit cost of the activity.
Relationship between nursing technicians’ production and unused capacity for test collection activities and the trend of the unit cost of the activity.
The analysis of one year of service stratified by activity allows identifying that the activity with the most significant imbalance and idle capacity is exercised by the scholars and represents, on average, 3% of the total cost. Medical professionals show an activity that gathers 57% of the costs and, although they are approaching the target cost over time, they still have the opportunity to issue more reports. Technical nursing professionals are the ones closest to operating at the maximum level of available capacity. These results suggest that there is an imbalance between the capacities of each activity, for example, the ability to collect tests should coincide with the ability to issue reports, and we were able to measure through this method that this does not occur in the sizing of the service.
The four activities were then consolidated into an individual cost of the teleophthalmology service to evaluate the unit component, and the following behavior of variation of unit costs over time was found (Figure 5). Over a year, the unit cost had a maximum amplitude in the period of R$611, mostly with a trend of nearing the fixed target standard cost.
Discussion
The applied method allowed detailing the costs associated with the adoption of a telemedicine service technology and to review the effectiveness of its implementation process. The standard measured cost for telediagnosis was R$119. A decreasing trend in the telediagnosis unit cost was observed during the evaluation period, which went from R$783 to R$283.30, characterizing the learning curve for the implementation of new technologies.
It is estimated that waiting for an appointment to receive a prescription for corrective lenses is more than one year in southern Brazil1616 Gonçalves MR, Umpierre RN, D'Avila OP, Katz N, Mengue SS, Siqueira ACS, Carrard VC, Schmitz CAA, Molina-Bastos CG, Rados DV, Agostinho MR, Oliveira EB, Roman R, Basso J, Pfeil JN, Mendonça MVA, Moro RG, Frank T, Stürmer PL, Harzheim E. Expanding Primary Care Access: A Telehealth Success Story. Ann Fam Med 2017; 15(4):383.. The lack of rational criteria in the ophthalmological appointment scheduling protocol, which causes an excessive delay in providing medical services, has the most severe consequence of irreparable loss of vision, in cases of glaucoma, diabetic retinopathy, among other pathologies. For another significant portion of patients diagnosed with cataracts and refraction, the delay will result in years of substantial loss of quality of life due to reduced visual acuity3838 Tahhan N, Papas E, Fricke TR, Frick KD, Holden BA. Utility and Uncorrected Refractive Error. Ophthalmology 2013; 120(9):1736-1744.
39 Cypel MC, Salomão SR, Dantas PEC, Lottenberg CL, Kasahara N, Ramos LR, Belfort Junior R. Vision status, ophthalmic assessment, and quality of life in the very old. Arq Bras Oftalmol 2017; 80(3):159-164.-4040 GBD 2017 DALYs HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392(10159):1859-1922.. The advent of telemedicine has the potential to qualify health and improve access. A better resolution in primary care can reduce referrals to secondary and tertiary care services77 Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015; 9:CD002098.,3838 Tahhan N, Papas E, Fricke TR, Frick KD, Holden BA. Utility and Uncorrected Refractive Error. Ophthalmology 2013; 120(9):1736-1744..
The cost behavior found in this study can be understood as the effect of learning on service provision. The maturity that can be acquired during the service’s learning period contributes to a better alignment of availability of professionals by activity, making the service more balanced. The balance of the service allows guiding the restructuring of the hourly availability of health professionals who perform the service, allowing a reduction in expenses by telediagnosis and better use of each allocated resource4141 McLaughlin N, Garrett MC, Emami L, Foss SK, Klohn JL, Martin NA. Integrating risk management data in quality improvement initiatives within an academic neurosurgery department. J Neurosurg 2016; 124(1):199-206.
42 French KE, Albright HW, Frenzel JC, Incalcaterra JR, Rubio AC, Jones JF, Feeley TW. Measuring the value of process improvement initiatives in a preoperative assessment center using time-driven activity-based costing. Healthc (Amst) 2013; 1(3-4):136-142.-4343 Koehler DM, Balakrishnan R, Lawler EA, Shah AS. Endoscopic Versus Open Carpal Tunnel Release: A Detailed Analysis Using Time-Driven Activity-Based Costing at an Academic Medical Center. J Hand Surg 2019; 44(1):62.e1-62.e9..
Economic assessments, starting with accurate cost measurement, are great allies to guide policymakers and funders to determine whether the evidence supports a broader adoption of mobile health interventions and to understand the ideal conditions under which they should be implemented2424 Brasil. Ministério da Saúde (MS), Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Departamento de Ciência e Tecnologia. Diretrizes metodológicas?: Diretriz de Avaliação Econômica. Brasília: MS; 2014.,4444 Le Goff-Pronost M, Sicotte C. The added value of thorough economic evaluation of telemedicine networks. Eur J Health Econ 2010; 11(1):45-55.. Technology must be continuously analyzed and improved so that its adoption occurs in a sustainable, transparent manner, and that favors its consolidation in the Brazilian public health system3434 Lima SGG, Brito C, Andrade CJC. Health technology assessment in Brazil - an international perspective. Cien Saude Colet 2019; 24(5):1709-1722. to be subjected to evaluation. In this study, the evaluation included observation of the behavior curve of the implementation of the provision of such a service. Therefore, the need for compatibility and data integration becomes clear, thus allowing a continuous process of learning and improving information about the use of the health service.
The search for papers in the literature shows that the number of studies aimed at evaluating the cost of telemedicine services has increased in the last decade. The origin of costs is mostly secondary, originating from national tables, estimated prices, and averages. There was no detailed calculation of the amount invested for the installation or continuity of the telemedicine program. In the area of teleophthalmology, it was not uncommon for the authors to claim that gauging and detailing costs is necessary to attribute the indirect benefit of telemedicine in the health system1010 Rachapelle S, Legood R, Alavi Y, Lindfield R, Sharma T, Kuper H, Polack S. The Cost-Utility of Telemedicine to Screen for Diabetic Retinopathy in India. Ophthalmology 2013; 120(3):566-573.,1111 Castillo-Riquelme MC, Lord J, Moseley MJ, Fielder AR, Haines L. Cost-effectiveness of digital photographic screening for retinopathy of prematurity in the United Kingdom. Int J Technol Assess Health Care 2004; 20(2):201-213.,4545 Nguyen HV, Tan GSW, Tapp RJ, Mital S, Ting DSW, Wong HT, Tan CS, Laude A, Tai ES, Tan NC, Finkelstein EA, Wong TY, Lamoureux EL. Cost-effectiveness of a National Telemedicine Diabetic Retinopathy Screening Program in Singapore. Ophthalmology 2016; 123(12):2571-2580.. However, only two of them made use of micro-costing methods in the variable of costs, both specific for screening for diabetic retinopathy. In the Brazilian scenario4646 Andrade MV, Maia AC, Cardoso CS, Alkmim MB, Ribeiro ALP. Custo-Benefício do Serviço de Telecardiologia no Estado de Minas Gerais: Projeto Minas Telecardio. Custo-benefício da telecardiologia 2011; 97:307-316., studies on the implementation and cost-effectiveness of telemedicine in the field of cardiology have already been carried out, and likewise consider implementation costs separate from the others, given the period of adaptation of the technology and personnel involved. However, due to differences in methods, time of publication, and data collection, comparisons between results are limited and should be made with caution.
Among the limitations, we can mention the failure to carry out a complete economic evaluation, considering that insufficient outcome metrics were not included in the study to carry out a cost-effectiveness or cost-utility evaluation. It is also noteworthy that the use of these results for purposes of comparison with other States and services must consider that labour costs of Telehealth service is composed of scholarships and employment relations and, thus, can operate at a lower cost through telediagnosis.
This result is relevant for planning the provision of health services in the country, as it shows that the implementation of teleophthalmology systems is feasible and has excellent potential to qualify the eye care waiting list in PHC. With scale gain, telemedicine will be essential to overcome the bottleneck of the waiting lists for highly complex procedures because it allows the risk classification, thus qualifying access to the specialty and the user’s care4747 Maeyama MA, Calvo MCM. A Integração do Telessaúde nas Centrais de Regulação: a Teleconsultoria como Mediadora entre a Atenção Básica e a Atenção Especializada. Rev Bras Educ Médica 2018; 42(2):63-72..
Conclusions
This study is unprecedented in Brazil when evaluating the real costs of a telemedicine service, and it is believed that the multiplication of partial economic evaluation studies of these services is essential to support incorporation decisions. The use of TDABC is noteworthy to facilitate this and scalability, as it allows to obtain more accurate information on technology cost, improving the management capacity of the health organization. The case studied allowed us to identify how the implementation of new technology in the health system needs time to mature to measure the standard cost to be used to guide the decision on incorporating the technology. Applying methodologies that better enable the measurement and analysis of financial information becomes essential for strategic health management and subsequent guidance for decision-making. Future cost-effectiveness studies will be carried out as a continuation of this economic assessment.
Acknowledgments
Financial support was provided by the Ministry of Health, through the SUS Institutional Development Support Program (PROADI-SUS), the State Health Secretariat of Rio Grande do Sul and the National Institute of Science and Technology for health Technology Assessment (IATS) – CNPq/Brazil.
Referências
-
1Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med 2017; 377(16):1585-1592.
-
2Maldonado JMSV, Marques AB, Cruz A. Telemedicina: desafios à sua difusão no Brasil. Cad Saude Publica 2016; 32(Supl. 2):e00155615.
-
3Halvorsen PA, Kristiansen IS. Radiology services for remote communities: cost minimisation study of telemedicine. BMJ 1996; 312(7042):1333-1336.
-
4Bashshur RL, Howell JD, Krupinski EA, Harms KM, Bashshur N, Doarn CR. The Empirical Foundations of Telemedicine Interventions in Primary Care. Telemed E-Health 2016; 22(5):342-375.
-
5Lamminen H, Lamminen J, Ruohonen K, Uusitalo H. A cost study of teleconsultation for primary-care ophthalmology and dermatology. J Telemed Telecare 2001; 7(3):167-173.
-
6Hjelm NM. Benefits and drawbacks of telemedicine. J Telemed Telecare 2005; 11(2):60-70.
-
7Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015; 9:CD002098.
-
8Grustam AS, Severens JL, van Nijnatten J, Koymans R, Vrijhoef HJM. Cost-effectiveness of telehealth interventions for chronic heart failure patients: a literature review. Int J Technol Assess Health Care 2014; 30(1):59-68.
-
9Kotb A, Cameron C, Hsieh S, Wells G. Comparative Effectiveness of Different Forms of Telemedicine for Individuals with Heart Failure (HF): A Systematic Review and Network Meta-Analysis. PLoS One 2015; 10(2):e0118681.
-
10Rachapelle S, Legood R, Alavi Y, Lindfield R, Sharma T, Kuper H, Polack S. The Cost-Utility of Telemedicine to Screen for Diabetic Retinopathy in India. Ophthalmology 2013; 120(3):566-573.
-
11Castillo-Riquelme MC, Lord J, Moseley MJ, Fielder AR, Haines L. Cost-effectiveness of digital photographic screening for retinopathy of prematurity in the United Kingdom. Int J Technol Assess Health Care 2004; 20(2):201-213.
-
12Thomas S, Hodge W, Malvankar-Mehta M. The Cost-Effectiveness Analysis of Teleglaucoma Screening Device. PLoS One 2015; 10(9):e0137913.
-
13Rush KL, Hatt L, Janke R, Burton L, Ferrier M, Tetrault M. The efficacy of telehealth delivered educational approaches for patients with chronic diseases: A systematic review. Patient Educ Couns 2018; 101(8):1310-1321.
-
14Hamilton SJ, Mills B, Birch EM, Thompson SC. Smartphones in the secondary prevention of cardiovascular disease: a systematic review. BMC Cardiovasc Disord 2018; 18(1):25.
-
15Harzheim E, Gonçalves MR, Umpierre RN, Siqueira ACS, Katz N, Agostinho MR, Oliveira EB, Basso J, Roman R, Moro RG, Pilz C, Heinzelmann RS, Schmitz CAA, Hauser L, Mengue SS. Telehealth in Rio Grande do Sul, Brazil: Bridging the Gaps. Telemed E-Health 2016; 22(11):938-944.
-
16Gonçalves MR, Umpierre RN, D'Avila OP, Katz N, Mengue SS, Siqueira ACS, Carrard VC, Schmitz CAA, Molina-Bastos CG, Rados DV, Agostinho MR, Oliveira EB, Roman R, Basso J, Pfeil JN, Mendonça MVA, Moro RG, Frank T, Stürmer PL, Harzheim E. Expanding Primary Care Access: A Telehealth Success Story. Ann Fam Med 2017; 15(4):383.
-
17Secretaria de Saúde Estadual. Gestão e Tecnologia em Saúde Sistema AGHOS 2016 (não publicado).
-
18Brasil. Ministério da Saúde (MS), Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Departamento de Ciência e Tecnologia. Guia Metodológico para Programas e Serviços em Telessaúde [documento na Internet]. Brasilia: MS; 2019 [acessado 2019 Set 4]. Disponível em: https://www.telessaude.unifesp.br/images/docs/Guia_Monitoramento_Telessaude_WEB.pdf
-
19Lin M, Yuan W, Huang T, Zhang H, Mai J, Wang J. Clinical effectiveness of telemedicine for chronic heart failure: a systematic review and meta-analysis. J Investig Med 2017; 65(5):899-911.
-
20Iribarren SJ, Cato K, Falzon L, Stone PW. What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS One 2017; 12(2):e0170581.
-
21Souza RJSP, Mattedi AP, Rezende ML, Corrêa MP, Duarte EM. Estimativa do custo do tratamento de câncer de pele tipo melanoma no Estado de São Paulo - Brasil. An Bras Dermatol 2009 ;84(3):237-343.
-
22Etges APBS, Cruz LN, Notti RK, Neyeloff JL, Schlatter RP, Astigarraga CC, Falavigna M, Polanczyk CA. An 8-step framework for implementing time-driven activity-based costing in healthcare studies. Eur J Health Econ 2019; 20(8):1133-1145.
-
23Martin JA, Mayhew CR, Morris AJ, Bader AM, Tsai MH, Urman RD. Using Time-Driven Activity-Based Costing as a Key Component of the Value Platform: A Pilot Analysis of Colonoscopy, Aortic Valve Replacement and Carpal Tunnel Release Procedures. J Clin Med Res 2018; 10(4):314-320.
-
24Brasil. Ministério da Saúde (MS), Secretaria de Ciência, Tecnologia e Insumos Estratégicos, Departamento de Ciência e Tecnologia. Diretrizes metodológicas?: Diretriz de Avaliação Econômica Brasília: MS; 2014.
-
25Kaplan RS, Cooper R. Custo e desempenho: administre seus custos para ser mais competitivo São Paulo: Futura; 1998.
-
26Kaplan RS, Anderson SR. The Innovation of Time-Driven Activity-Based Costing. J Cost Manag 2007; 21(2):5-15.
-
27Keel G, Savage C, Rafiq M, Mazzocato P. Time-driven activity-based costing in health care: A systematic review of the literature. Health Policy 2017; 121(7):755-763.
-
28Erhun F, Mistry B, Platchek T, Milstein A, Narayanan VG, Kaplan RS. Time-driven activity-based costing of multivessel coronary artery bypass grafting across national boundaries to identify improvement opportunities: study protocol. BMJ 2015; 5(8):e008765.
-
29Chapko MK, Liu C-F, Perkins M, Li Y-F, Fortney JC, Maciejewski ML. Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ 2009; 18(10):1188-1201.
-
30Heaton HA, Nestler DM, Barry WJ, Helmers RA, Sir MY, Goyal DG, Haas DA, Kaplan RS, Sadosty AT. A Time-Driven Activity-Based Costing Analysis of Emergency Department Scribes. Mayo Clin Proc Innov Qual Outcomes 2019; 3(1):30-34.
-
31Martins E. Contabilidade de custos São Paulo: Atlas; 2008.
-
32Husereau D, Drummond M, Petrou S. Consolidated health economic evaluation reporting standards (CHEERS) - Explanation and elaboration: A report of the ISPOR health economic evaluations publication guidelines good reporting practices task force. Value Health 2013; 16(2):231-250.
-
33Dua HS, Singh AD. Global estimates of visual impairment: 2010. Br J Ophthalmol 2012; 96(5):614-618.
-
34Lima SGG, Brito C, Andrade CJC. Health technology assessment in Brazil - an international perspective. Cien Saude Colet 2019; 24(5):1709-1722.
-
35Golini R, Kalchschmidt M, Landoni P. Adoption of project management practices: The impact on international development projects of non-governmental organizations. Int J Proj Manag 2015; 33(3):650-663.
-
36Kaplan RS, Witkowski ML, Hohman JA. Children's Hospital Boston: measuring patient costs. C. R. Math 2012; 3(1):e28.
-
37Sistema Gerenciador de Séries Temporais (SGS) [página na Internet]. [acessado 2019 Set 4]. Disponível em: https://www3.bcb.gov.br/sgspub/consultarvalores /consultarValoresSeries.do?method=consultarValores
» https://www3.bcb.gov.br/sgspub/consultarvalores /consultarValoresSeries.do?method=consultarValores -
38Tahhan N, Papas E, Fricke TR, Frick KD, Holden BA. Utility and Uncorrected Refractive Error. Ophthalmology 2013; 120(9):1736-1744.
-
39Cypel MC, Salomão SR, Dantas PEC, Lottenberg CL, Kasahara N, Ramos LR, Belfort Junior R. Vision status, ophthalmic assessment, and quality of life in the very old. Arq Bras Oftalmol 2017; 80(3):159-164.
-
40GBD 2017 DALYs HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392(10159):1859-1922.
-
41McLaughlin N, Garrett MC, Emami L, Foss SK, Klohn JL, Martin NA. Integrating risk management data in quality improvement initiatives within an academic neurosurgery department. J Neurosurg 2016; 124(1):199-206.
-
42French KE, Albright HW, Frenzel JC, Incalcaterra JR, Rubio AC, Jones JF, Feeley TW. Measuring the value of process improvement initiatives in a preoperative assessment center using time-driven activity-based costing. Healthc (Amst) 2013; 1(3-4):136-142.
-
43Koehler DM, Balakrishnan R, Lawler EA, Shah AS. Endoscopic Versus Open Carpal Tunnel Release: A Detailed Analysis Using Time-Driven Activity-Based Costing at an Academic Medical Center. J Hand Surg 2019; 44(1):62.e1-62.e9.
-
44Le Goff-Pronost M, Sicotte C. The added value of thorough economic evaluation of telemedicine networks. Eur J Health Econ 2010; 11(1):45-55.
-
45Nguyen HV, Tan GSW, Tapp RJ, Mital S, Ting DSW, Wong HT, Tan CS, Laude A, Tai ES, Tan NC, Finkelstein EA, Wong TY, Lamoureux EL. Cost-effectiveness of a National Telemedicine Diabetic Retinopathy Screening Program in Singapore. Ophthalmology 2016; 123(12):2571-2580.
-
46Andrade MV, Maia AC, Cardoso CS, Alkmim MB, Ribeiro ALP. Custo-Benefício do Serviço de Telecardiologia no Estado de Minas Gerais: Projeto Minas Telecardio. Custo-benefício da telecardiologia 2011; 97:307-316.
-
47Maeyama MA, Calvo MCM. A Integração do Telessaúde nas Centrais de Regulação: a Teleconsultoria como Mediadora entre a Atenção Básica e a Atenção Especializada. Rev Bras Educ Médica 2018; 42(2):63-72.
Publication Dates
-
Publication in this collection
06 Apr 2020 -
Date of issue
Mar 2020
History
-
Received
03 Oct 2019 -
Accepted
21 Oct 2019 -
Published
23 Oct 2019