Abstracts
PURPOSE: To establish the frequency of genetic mutations related to sensorineural hearing loss (SNHL); to verify if there is association between the degree of SNHL and the presence of genetic alteration; and to verify if the Minimal Response Levels (MRL) with hearing aids vary according to the genetic alteration. METHODS: Thirty hearing aids users with ages between 8 and 111 months were evaluated. The evaluation procedures used were: pure-tone audiometry; the auditory steady state response (ASSR) on sound field, with and without hearing aids; and genetic study of the hearing loss. RESULTS: Three genetic mutations were diagnosed: 35delG, A1555G and A827G, and the children with these mutations showed higher degree of SNHL. There was no difference between the genetic patterns regarding the degree of SNHL, except for patients with A827G mitochondrial mutation, because all subjects with this mutation had profound SNHL. The difference between the MRL obtained with and without amplification, considering the presence of mutation and the degree of SNHL, was higher in children with moderate SNHL without genetic alterations, both in behavioral and electrophysiological evaluations. CONCLUSION: Genetic mutations were found in 36.7% of the sample, justifying the importance of genetic tracking in the hearing habilitation process. Children with genetic mutations showed higher degrees of hearing loss. The different mutation patterns do not directly determine the degree of hearing loss. The best thresholds with amplification were found in children with moderate hearing loss without genetic alterations.
Hearing loss; Evoked potentials, auditory; Hearing aids; Child; Genetics
OBJETIVO: Estabelecer a frequência de mutações genéticas relacionadas à deficiência auditiva neurossensorial (DANS); verificar se há associação entre grau da DANS e presença de alteração genética e verificar se os Níveis Mínimos de Resposta (NMR) com próteses auditivas variam em função da alteração genética. MÉTODOS: Foram avaliadas 30 crianças, com idades entre 8 e 111 meses, usuárias de próteses auditivas. Os procedimentos de avaliação utilizados foram: audiometria tonal e resposta auditiva de estado estável (RAEE) em campo livre, com e sem as próteses auditivas e estudo genético da DANS. RESULTADOS: Foram diagnosticadas três mutações genéticas: 35delG, A1555G e A827G, sendo que as crianças com tais mutações apresentaram maior grau de DANS. Não houve diferença entre os padrões genéticos em relação ao grau de DANS, com exceção dos pacientes com mutação mitocondrial A827G, pois todos com essa mutação eram portadores de DANS de grau profundo. A diferença entre os NMR obtidos sem e com o uso da amplificação, considerando a presença de mutação e grau de DANS, foi maior nas crianças portadoras de DANS de grau moderado sem alteração genética, tanto na avaliação comportamental quanto na eletrofisiológica. CONCLUSÃO: As mutações genéticas foram encontradas em 36,7% da amostra, o que justifica a importância do rastreamento genético no processo de habilitação auditiva. Crianças com mutações genéticas apresentam o maior grau de DANS. Os diferentes padrões de mutações não determinam diretamente o grau da DANS. Os melhores limiares com o uso da amplificação foram encontrados nas crianças com DANS moderada, sem alteração genética.
Perda auditiva; Potenciais evocados auditivos; Auxiliares de audição; Criança; Genética
ORIGINAL ARTICLE
Association between phenotype, performance with hearing aids, and genotype of childhood hearing loss in children with and without genetic alteration
Eliara Pinto Vieira BiaggioI; Marisa Frasson de AzevedoII; Maria Cecilia Martinelli IórioII; Maria Carolina Costa Melo SvidnickiIII; Edi Lúcia SatoratoIII
IDepartment of Speech-Language Pathology and Audiology, Universidade Federal de Santa Maria - UFSM - Santa Maria (RS), Brazil
IIDepartment of Speech-Language Pathology and Audiology, Universidade Federal de São Paulo - UNIFESP - São Paulo (SP), Brazil
IIIHuman Genetics Laboratory, Universidade Estadual de Campinas - UNICAMP - Campinas (SP), Brazil
Correspondence address Correspondence address: Eliara Pinto Vieira Biaggio R. Dr Bozano, 629/502, Bomfim, Santa Maria (RS), Brasil, CEP: 97015-001. E-mail: eliarapv@yahoo.com.br
ABSTRACT
PURPOSE: To establish the frequency of genetic mutations related to sensorineural hearing loss (SNHL); to verify if there is association between the degree of SNHL and the presence of genetic alteration; and to verify if the Minimal Response Levels (MRL) with hearing aids vary according to the genetic alteration.
METHODS: Thirty hearing aids users with ages between 8 and 111 months were evaluated. The evaluation procedures used were: pure-tone audiometry; the auditory steady state response (ASSR) on sound field, with and without hearing aids; and genetic study of the hearing loss.
RESULTS: Three genetic mutations were diagnosed: 35delG, A1555G and A827G, and the children with these mutations showed higher degree of SNHL. There was no difference between the genetic patterns regarding the degree of SNHL, except for patients with A827G mitochondrial mutation, because all subjects with this mutation had profound SNHL. The difference between the MRL obtained with and without amplification, considering the presence of mutation and the degree of SNHL, was higher in children with moderate SNHL without genetic alterations, both in behavioral and electrophysiological evaluations.
CONCLUSION: Genetic mutations were found in 36.7% of the sample, justifying the importance of genetic tracking in the hearing habilitation process. Children with genetic mutations showed higher degrees of hearing loss. The different mutation patterns do not directly determine the degree of hearing loss. The best thresholds with amplification were found in children with moderate hearing loss without genetic alterations.
Keywords: Hearing loss. Evoked potentials, auditory. Hearing aids. Child. Genetics
INTRODUCTION
In the past years improvements regarding hearing diagnosis practice and etiologic research of the hearing impairments (HI) in the pediatric population have been perceived, because precocious detection and intervention of hearing disorders are important to prevent alterations in children's development.
Regarding the etiology of children's hearing impairment, it can be classified as: acquired and genetic. The study about the genetic causes of HI advanced significantly and several genes related to this deficit have been identified(1,2). There has been increasing interest in studying non-syndromic recessive hearing impairment, mainly the GJB2gene, which codifies the Conexin 26 protein (Cx26), because it is responsible for most cases of hearing loss with genetic origin(3).
The tracking of genetic mutation should be included in the battery of tests to investigate hearing impairments, because it helps the etiology elucidation and it enables, in cases of positivity, the genetic counseling(2).
Moreover, the importance of knowing the diagnostic hypothesis of hearing impairments is directly related to the planning of hearing rehabilitation.
After the establishment of the auditory diagnosis, the focus of the speech-language therapy is the process of selection and adaptation of hearing aids, even if the etiologic hypothesis is not established.
Some studies aim at clarifying the relationship between the use of hearing aids (performance and benefit), language development and speech perception and the different manifestations of hereditary hearing impairments(4-6). Other authors(7-10) studied the performance of subjects with cochlear implantation, according to their hearing impairments, observing that children with genetic alterations present more benefits with cochlear implantation.
Several researchers studied the relationship between genotype of Conexin 26 mutations and auditory phenotype (configuration and degree of hearing loss), considering the results of tonal threshold audiometry, Transient Evoked Otoacoustic Emission (TEOAE) and of Brainstem Auditory Evoked Potential (BAEP)(11,12). However, there were no found studies which related the findings of the research of Auditory Steady State Response (ASSR) and the etiology of hearing impairments, especially genetic.
The ASSR is an important procedure of auditory evaluation, because it presents more facilities and efficiency to obtain responses, objectivity in the register analysis, selectivity in the responses frequency, and higher detection of hearing responses than other objective methods such as BAEP(13). Such findings justify the importance of the ASSR, because young children may not cooperate during the behavioral auditory evaluation and this procedure is useful to determine the auditory threshold, once there is close relationship between the electro physiological thresholds obtained through ASSR and behavioral thresholds(14).
Besides, the use of ASSR with sound field hearing aids has been emphasized, with the purpose of evaluating the audibility of weak sounds(15,16).
It is noticed increasing interest in the genetic investigation of hearing impairments and of the improvement of children's auditory evaluation procedures. In the same way, in the national scientific environment there are no clues about studies which relate the etiology of hearing impairments and results of ASSR with hearing aids in the pediatric population.
Thus, the purposes of this study were: (1) to establish the frequency of genetic mutations related to sensorineural hearing impairments in the sample; (2) to verify if there is association between degree of hearing loss and the presence of genetic alterations; and (3) to verify if the Minimum Response Levels (MRL) with auditory aids vary in relation to the variable genetic alteration.
METHODS
This research was a clinical cross-sectional study with children attended at the Integrated Assistance, Research and Teaching Nucleus on Hearing (NIAPEA), of the Universidade Federal de São Paulo, with the approval of the institution›s Research Ethics Committee (CEP 1828/09). Parents and/or caretakers who agreed with their children›s participation in the research signed the Informed Consent Form.
The following inclusion criteria were established for this study: children ranging in age from 6 months to 10 years old of both genders; with sensorineural bilateral symmetrical hearing loss from mild to profound(17); users of hearing aids with bilateral adaptation for, at least, three months; and being inserted in programs of auditory stimulation (speech therapy) in a certain moment of the auditory habilitation process. Children who presented evident neurological impairments and/or associated deficiency, conductive impairments, asymmetrical sensorineural hearing loss and carriers of the auditory neuropathy spectrum disorder were excluded of this research.
The sample selection was performed through research at the NIAPEA data basis, with 552 children who were born between 2000 and 2009, gender part of the data basis. From this total, 123 children presented complete auditory evaluation and, considering all eligibility criteria, 58 children were found. It is important to emphasize that 28 children did not conclude all steps of the present study and, so, the sample consisted of 30 children, male and female, with ages between eight to 111 months old.
The sample of 30 children presented 20 (66.7%) girls and 10 (33.3%) boys, with ages ranging between eight and 111 months old.
About the degree of sensorineural hearing loss (SNHL), the sample consisted of 12 children with severe SNHL (13.3%) and 14 with profound SNHL (46.7%).
The auditory evaluation was performed with and without hearing aid through behavioral and electro physiological evaluation, and also genetic study.
The evaluation consisted of pure-tone audiometry (PTA) and of Auditory Steady State Response (ASSR), both in sound field. First, both procedures were performed without the use of hearing aids.
The equipment used to accomplish the audiometry in sound field was an audiometer, Interacoustics®, model AC33. The stimuli were calibrated with proper equipment. Three different procedures were used to perform the free field tonal threshold audiometry, according to the chronological age, the development and the children's ability to respond sound stimuli: the Visual Reinforcement Audiometry (VRA); the ludic audiometry and the conventional audiometry.
Through these procedures, it was used the research of the Minimum Response Levels (MRL), minimal intensity in which children present responses for sound stimuli(18), in this moment without sound amplification. It is important to mention that, because this is a free field evaluation, it was obtained responses from the ear with better cochlear reserve.
The MRL research was accomplished with pure modulated tones in the frequency warble, in the frequencies of 500 Hz, 1, 2 and 4 kHz. The stimuli were initially presented in descending and after in ascending way. The sound stimuli were presented with maximal levels of 100 dBNA for all the frequencies. The protocol of this study was based on a previous one(19).
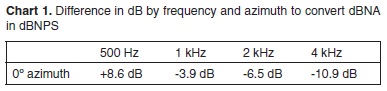
The MRLs were obtained in dBNA, but they were converted to dBNPS. Thus, the values measured from the difference between the dBNA in the audiometer dial and the dBNPS measured in the distance and positioning degree of the child in relation to the speaker were used. Chart 1 presents the values of correction obtained through frequency in different degrees and distances for the equipment which were used in this study.
The second auditory evaluation procedure was the ASSR, also performed in free field, with the equipment Smart EP by Intelligent Hearing System®, from a channel. The stimuli were calibrated in dBNPS, following the recommendations of the equipment manufacturer. The measurement of these stimuli was performed.
The evaluations were performed in acoustically treated rooms, with children positioned 70 cm from the speaker and 0° azimuth of it. All evaluations were achieved with children in natural sleep, regardless their age.
The evaluated ear was kept the same as the behavioral evaluation, because it was also a free field evaluation. The presentation way was ipsilateral. Besides, the same frequencies were evaluated, but the maximal intensity was 90 dBNPS (because of speakers' limitations).
The parameters adopted for such evaluation are displayed in Chart 2.
After the auditory evaluation, the MRLs were evaluated with the use of hearing aids. It means that the previous procedures were repeated (tonal audiometry and ASSR), but with children adapted with their hearing aids.
Before the beginning of the mentioned evaluation, it was verified the operation of the auditory aids and of the ear molds.
Finally, to investigate the possibility of non-syndromic genetic auditory loss, a genetic study was performed. The collected blood was binned into a test tube with EDTA as anticoagulant and it was sent to the Center of Molecular Biology and Genetic Engineering (CBMEG), Universidade Estadual de Campinas (UNICAMP).
The DNA was extracted and analyzed through adapted CBMEG methods. Initially, the mutation 35delG was tracked in the Conexin 16 protein gene through the method allele-specific PCR. Next, the deletions involving the Conexin 30 (GJB6), del (GJB6-D13S1830) and del (GJB6-D13S1854) were analyzed through multiplex PCR. According to the results, the complete sequencing of the GJB2 gene was accomplished.
The A1555G and A827G mitochondrial mutations were also analyzed in the 12S rRNA gene. The A1555G mutation was tracked through restriction analysis and the A827G mutation, through direct sequencing.
After the genetic study of the studied group, three mutations were found: 35deIG, A1555G and A827G. These mutations were diagnosed in 11 children (36.7% of the sample). After this evaluation, the sample was distributed in two groups, according to their genetic condition: with genetic alteration (n=11 children) and without genetic alteration (n=19 children).
Regarding the used statistical tests, to evaluate the correlation between the behavioral and electro physiological MRLs in free field, in both studied conditions (with and without auditory aids), it was used the Spearman's Correlation. Other statistical tests were used to analyze the data obtained in this research: Correlation test, Equality of Two Proportions, Wilcoxon's, Kruskal-Wallis', Mann-Whitney's Confidence Intervals for the average and p-value calculation. In each hypothesis test it was selected the significance level of 0.05. The significant values were checked with an asterisk. All confidence intervals which were built along the study were created with 95% of statistical confidence.
From the children who presented the studied genetic mutations, 45% of them presented the 35deIG mutation, 22% the A1555G mutation and 33% the A827G mutation.
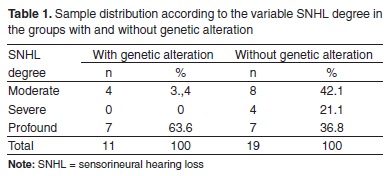
The HI degree in both groups, with and without genetic alteration, is presented in Table 1.
It was noticed that in the sample group, with genetic alteration, the SNHL degree which was the most prevalent was the profound degree, 63.6% (7/11), with significant difference.
It was accomplished an analysis of the group of children with genetic alterations, considering the distribution of SNHL degree for the three main studied genetic mutations: 35deIG, A1555G and A827G. There was no significant difference between the heterozygote (p=0.248) and homozygote (p=0.157) patterns of the 35delG mutation in relation to the SNHL degree.
There was also no significant difference between the SNHL degrees for the patients with A1555G mitochondrial mutation. There was significant difference among the SNHL degrees for the patients with A827G mitochondrial mutation, and all the patients with this mutation were carriers of profound degree SHNLs.
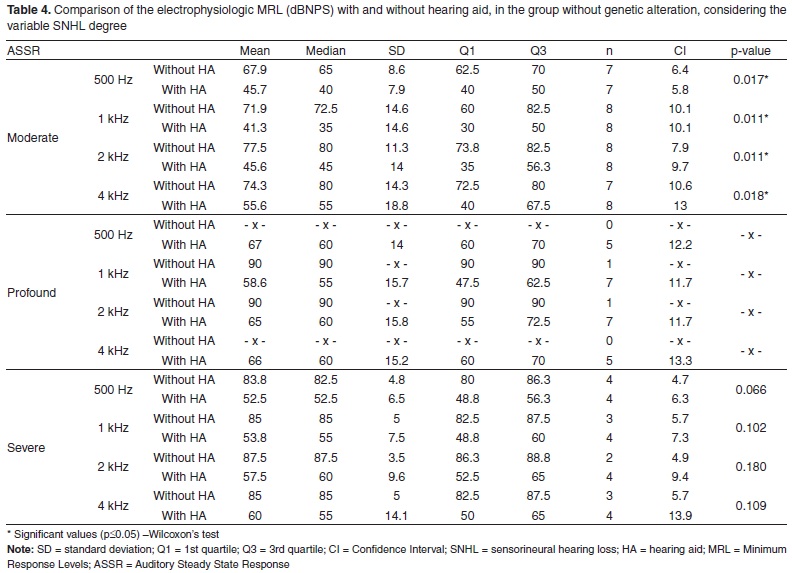
After that, the MRLs obtained on both procedures with and without the use of amplification were evaluated, considering the following variables: group and degree of loss (Tables 2, 3, 4 and 5).
As great part of the sample is profound degree SNHL carrier, there were many absent MRLs in both procedures (behavioral and electro physiological evaluations). In these cases, as it was not obtained information, it was not possible to perform the analysis. To show this MRL absence, the symbol "-x-" was inserted.
DISCUSSION
The sample consisted of 30 children with sensorineural hearing loss, moderate and profound level, with ages ranging between 8 months and 9 years old, users of hearing aids, treated at NIAPEA.
The children's distribution, according to the variable degree of auditory deficiency, evidenced that the highest degree of occurrence was the profound, followed by the moderate and the severe. Some authors(20) who elaborated a study with the purpose of describing the auditory characteristics of children seen by a Hearing Health Program, similar to the NIAPEA, observed that 46% of the children presented profound hearing loss, very similar to the present study.
It was accomplished genetic tracking to investigate the main recessive non-syndromic genetic mutations. The mutations 35delG, A1555G and A827G were diagnosed. From a total of 30 children, 19 (63.3%) did not present any genetic mutation and 11 (36.7%) presented some type of genetic mutation
In the group formed by children with genetic alteration, it is emphasized the presence of two siblings, who presented the same genetic mutation (35delG in heterozygosis). This is a frequently data related by literature, because in these cases the authors consider the family, not the individual. These siblings present the same genetic information, but the two subjects were considered, because one of the concerns of this study was relating genotype and phenotype. It is important to mention that they presented different performances regarding the use of hearing aids.
The focus of the genetic tracking was the study of recessive mutations, because among the heredity, the autosomal recessive is the most frequent(21). Another important aspect is the 35delG mutation, because it is the most frequent SNHL cause(1). Summarizing, the HI physiopathological extract caused as a consequence of the 35ddelG is related to alterations in the functioning of the gap junctions and in the maintenance of high concentrations of intracellular potassium, which damage the mechanism of fast response by the ciliated cells to the new sound stimuli and, so, it results in hearing impairments(22,23).
Considering the results of different studies performed in Brazil, it is observed great variation in relation to the proportion of the 35delG mutation, ranging from 5.3%(2) to 45% of the sample which presents the mutations (present study). This finding may be justified by the significant miscegenation in Brazil. The Brazilian population presents interaction of different races and ethnics, mainly the genetic integration of Europeans, especially from Italy, Spain and Portugal. Another researched genetic alteration was the A1555G, because it is the most frequent deoxyribonucleic acid (DNA) mutation, associated with higher sensibility to ototoxic drugs, especially the use of amino glycosides(24). In the group of children with genetic alterations, two of them were carriers of this type of mutation, what represents 22% of the sample.
As the mitochondrial mutation A1555G, the mutation A827G, in the 12S rRNA gene, was initially associated with hearing loss susceptibility induced by amino glycosides(25). Also, 33% of the children from the group with genetic alterations presented this mitochondrial mutation. However, the effect of this alteration is still controversial. Some authors believe that this mutation is simple polymorphism, not justified by the hearing loss in individuals who present this alteration.
It was also studied the children's degree of SNHL, considering the distribution of the sample in two groups: with and without genetic alteration (Table 1). The results evidenced that in the group of children with genetic alteration there was predomination of profound degree SNHL (63.6%). In the group of children without genetic alteration there was no significant difference among the three SNHLs degrees (moderate, severe and profound).
Several studies describe the auditory characteristics related to SNHLs with recessive genetic origin, that, in most cases, are characterized by severe and profound degree auditory deficiency, but in some cases the degree of hearing loss may be moderate(4,24,26), as it was observed in the present study.
Then, it was analyzed the group of children with genetic alteration, considering the distribution of the SNHL degree for the three main studied genetic mutations: 35deIG, A1555G and A827G.
In the children with the 35delG mutation, there was no significant difference between the heterozygote and homozygote patterns of the 35delG mutation in relation to the degree of SNHL. The issue heterozygote and homozygote if often studied by researchers(1,9). The authors refer that it is necessary that the individual inherits two mutated alleles, one from the father and another from the mother, to express the auditory deficiency (homozygosis). Thus, it is impossible to the Conexin 26 to be codified by the altered GJB2 gene, what would cause the SHNL. When the child presents the 35delG mutation in heterozygosis, it means that there is mutation in only one of the alleles, and it is possible that the other allele codifies the protein. It would imply in a lower number of codified Conexin 26. So, the 35delG mutation in heterozygosis does not diagnosis cause of deafness. It only proves that the patient is carrier of this mutation.
There was no significant difference among the SNHL degrees for the patients with A1555G mitochondrial mutation. An author(27) refers that the auditory phenotype, in subjects who are carriers of the A1555G mitochondrial mutation, may vary even among members of the same family, and the degree of the SNHL may be moderate and profound.
There was significant difference among the degrees of SNHL for the patients with the A827G mitochondrial mutation, and all patients with this mutation were carriers of profound degree SNHL. However, other authors(25) mention that the degree of the hearing deficiency may be from mild to profound. According to the same authors, aggravating factors for the deficiency would be the time of use of amino glycosides, the associated use of this drug, the age of children when they use amino glycosides, etc.
The MRLs obtained in the procedures with and without the use of amplification were also evaluated, considering the following variables: group and HI degree (Tables 2, 3, 4 and 5). In these analysis, the data which deserves more relevance is the fact that only the children with severe degree of SNHL, without genetic alteration, as in the behavioral as in the electro physical evaluation, presented significant difference between the evaluations with and without hearing aids.
Some authors studied the relationship among the use of auditory aids (performance and benefit), language development and speech perception with different manifestations of HI with genetic origin(4-6). The results of the three mentioned studies converge to a similar finding, that the genetic mutations do not determine directly the benefit with sound amplification. Nevertheless, the highest incidence of more severe SNHLs in children with genetic mutations, leads to a negative impact about the benefits of hearing aids for these children. The authors emphasized that the linguistic and hearing performance would be correlated with the SNHL severity, age of diagnosis and intervention, quality of the speech-language therapy, etc.
The findings of the present study, in children without genetic alteration, agree with the previously mentioned authors, because the children who presented significant MRL difference, with and without sound amplification, are carriers of moderate degree SNHL. However, the children with genetic alteration, even with moderate HI, do not present significant differences, only a tendency of it that could perhaps be significant if the sample was higher. The greatest benefit with the hearing aids would be related to the lowest cochlear impairments.
Another possible hypothesis for this finding is the MRL absence, mainly in the condition without hearing aids, once the children with severe and profound SNHL present high index of absent responses in the maximum level of the sound pressure which was evaluated. The maximum level in which the electro physical MRL was researched was 90 dBNPS, because of a limitation of loudspeakers. Maybe if it was higher and if it was obtained higher number of present MRL, a more conclusive analysis could be achieved.
The Idea of relating the genetic HI manifestations with the auditory performance with the use of cochlear implant (CI) is also a concern of many researchers(7-10). Different from the findings with hearing aids, the children with genetic mutations present, in general, higher benefits with the CI when compared with the children without such mutations. It would happen because the SNHL caused by the Cx26 mutations cause alteration which do not affect cells of the spiral ganglion, which are the neural elements stimulated by the implant, leading to better results. So, in implanted patients the genetic etiology would be a positive indicator of success in the linguistic and auditory performance.
CONCLUSION
The data analysis allowed the conclusion that the genetic mutations were found in 11 children (36.7%) of the sample. They presented three diagnosed mutations: 35delG, A1555G and A827G. In addition, the children with the studied genetic alterations presented higher degree of SNHL. It is also concluded that the behavioral and electro physical MRLs of children with moderate degree SNHL, without genetic alteration were lower than the MRLs of children with genetic alteration, also carriers of moderate degree SNHL, what means better performance with aids by children without genetic alteration
REFERENCES
1. Wilcox SA, Saunders K, Osborn AH, Arnold A, Wunderlich J, Kelly T, et al. High frequency hearing loss correlated with mutations in the GJB2 gene. Hum Genet. 2000;106(4):399-405.
2. Pfeilsticker LN, Stole G, Sartorato EL, Delfino D, Guerra AT. A investigação genética na surdez hereditária não-sindrômica. Rev Bras Otorrinolaringol. 2004;70:182-6.
3. Guilford P, Ben Arab S, Blanchard S, Levilliers J, Weissenbach J, Belkahia A, et al. A non-syndromic form of neurosensory, recessive deafness maps to the pericentromeric region of chromosome 13q. Nat Genet. 1994;6(1):24-8.
4. Mesolella M, Tranchino G, Nardone M, Motta S, Galli V. Connexin 26 mutations in nonsyndromic autosomal recessive hearing loss: speech and hearing rehabilitation. Int J Pediatr Otorhinolaryngol. 2004;68(8):995-1005.
5. Dahl HH, Wake M, Sarant J, Poulakis Z, Siemering K, Blamey P. Language and speech perception outcomes in hearing-impaired children with and without connexin 26 mutations. Audiol Neurootol. 2003;8(5):263-8.
6. Matsunaga T, Hirota E, Bito S, Niimi S, Usami S. Clinical course of hearing and language development in GJB2 and non-GJB2 deafness following habilitation with hearing aids. Audiol Neurootol. 2006;11(1):59-68.
7. Green GE, Scott DA, McDonald JM, Teagle HF, Tomblin BJ, Spencer LJ et al. Performance of cochlear implant recipients with GJB2-related deafness. Am J Med Genet. 2002;109(3):167-70
8. Sinnathuray AR, Toner JG, Clarke-Lyttle J, Geddis A, Patterson CC, Hughes AE. Connexin 26 (GJB2) gen-related deafness and speech intelligibility after cochlear implantation. Otol Neurotol 2004;25(4):935- 42.
9. Bernades R, Bortoncello S, Christiani TV, Sartorato EL, César e Silva R, Porto PR. Estudo molecular em crianças candidatas e submetidas ao implante coclear. Rev Bras Otorrinolaringol. 2006;72(3):333-6.
10. Wu CC, Lee YC, Chen PJ, Hsu CJ Predominance of genetic diagnosis and imaging results as predictors in determining the speech perception performance outcome after cochlear implantation in children. Arch Pediatr Adolesc Med. 2008;162(3):269-76.
11. Batissoco AC, Abreu-Silva RS, Braga MC, Lezirovitz K, Della-Rosa Vet al. Prevalence of GJB2 (connexin-26) and GJB6 (connexin-30) mutations in a cohort of 300 Brazilian hearing-impaired individuals: implications for diagnosis and genetic counseling. Ear Hear. 2009 Feb;30(1):1-7.
12. Cordeiro-Silva Mde F, Barbosa A, Santiago M, Provetti M, Rabbi-Bortolini E. Prevalence of 35delG/GJB2 and del (GJB6-D13S1830) mutations in patients with non-syndromic deafness from a population of Espírito Santo - Brazil. Braz J Otorhinolaryngol. 2010;76(4):428-32.
13. Dimitrijevic A, John MS, Picton TW. Auditory steady-state responses and word recognition in normal-hearing and hearing-impaired adults. Ear Hear. 2004;25(1):68-84.
14. Ferraz OB, Freitas SV, Marchiori LL. Análise das respostas obtidas por potenciais evocados auditivos de estado estável em indíviduos normais Rev Bras Otorrinolaringol. 2002;68(4):480-6.
15. Donini TS. A utilização do potencial evocado auditivo de estado estável no processo de indicação do aparelho de amplificação sonora individual em crianças com deficiência auditiva [Dissertação de Mestrado]. São Paulo: Pontifícia Universidade Católica de São Paulo; 2007. 16. Rodrigues GR, Lewis DR. Potenciais evocados auditivos de estado estável em crianças com perdas auditivas cocleares. Pro Fono. 2010;22(1):37-42.
17. Organização Mundial da Saúde (World Health Organization). Prevention of blindeness and deafness: grades of hearing impairment. 1997. [internet]. http://www.who.int/pbd/deafness/hearing_impairment_grades/en/. Acesso em: 15/11/2010.
18. American Speech Language Hearing Association. Guidelines for the audiologic assessment of children from the birth through 36 months of age. ASHA. 1991;33(5):37-43.
19. Azevedo MF. Avaliação subjetiva da audição no primeiro ano de vida. Temas desenvolv. 1991;1(3):11-4.
20. Lanzetta BP, Frota S, Goldfeld M. Acompanhamento da adaptação de próteses auditivas em crianças surdas. Rev. CEFAC [online]. 2010;12(3):360-70.
21. Bitner-Glindzicz M. Hereditary deafness and phenotyping in humans. Br Med Bull. 2002;63:73-94.
22. Mueller R. Connexin 26 (GJB2) deafness homepage. In: Martini A, Mazzoli M, Stephens D, Read A. Definitions, Protocols and Guidelines in Genetic Hearing Impairment. London: Whurr Publishers Ltd; 2001. p. 176-80.
23. Shibata Y, Kumai M, Nishi K, Nakamura K. Diversity and molecular anatomy of gap junctions. Med Electron Microsc. 2001;34(3):153-9.
24. Cryns K, Van Camp, G. Deafness genes and their diagnostic applications. Audiol Neurootol. 2004;9(1):2-22.
25. Li R, Greinwald JH Jr, Yang L, Choo DI, Wenstrup RJ, Guan MX. Molecular analysis of the mitochondrial 12SrRNA and tRNASer (UNC) genes in pediatric subjects with non-syndromic hearing loss. J Med Genet. 2004;41(8):615-20. 26. Hismi BO, Yilmaz ST, Incesulu A, Tekin M. Effects of GJB2 genotypes on the audiological phenotype: variability is present for all genotypes. Int J Pediatr Otorhinolaryngol. 2006;70(10):1687-94.
27. Del Castillo FJ, Rodriguez-Ballesteros M, Martin Y, Arellano B, Gallo-Teran J, Morales-Angulo C, et al. Heteroplasmy for the 1555AG mutation in the mitochondrial 12S rRNA gene in six Spanish families with non-syndromic hearing loss. J Med Genet. 2003;40(8):632-6.
Conflict of interests: None
Received: 9/27/2011
Accepted: 6/12/2012
Study accomplished at the Integrated Assistance, Research and Teaching Nucleus on Hearing (NIAPEA), Department of Speech-Language Pathology and Audiology, Universidade Federal de São Paulo - UNIFESP - São Paulo (SP), Brazil.
- 1. Wilcox SA, Saunders K, Osborn AH, Arnold A, Wunderlich J, Kelly T, et al. High frequency hearing loss correlated with mutations in the GJB2 gene. Hum Genet. 2000;106(4):399-405.
- 2. Pfeilsticker LN, Stole G, Sartorato EL, Delfino D, Guerra AT. A investigação genética na surdez hereditária não-sindrômica. Rev Bras Otorrinolaringol. 2004;70:182-6.
- 3. Guilford P, Ben Arab S, Blanchard S, Levilliers J, Weissenbach J, Belkahia A, et al. A non-syndromic form of neurosensory, recessive deafness maps to the pericentromeric region of chromosome 13q. Nat Genet. 1994;6(1):24-8.
- 4. Mesolella M, Tranchino G, Nardone M, Motta S, Galli V. Connexin 26 mutations in nonsyndromic autosomal recessive hearing loss: speech and hearing rehabilitation. Int J Pediatr Otorhinolaryngol. 2004;68(8):995-1005.
- 5. Dahl HH, Wake M, Sarant J, Poulakis Z, Siemering K, Blamey P. Language and speech perception outcomes in hearing-impaired children with and without connexin 26 mutations. Audiol Neurootol. 2003;8(5):263-8.
- 6. Matsunaga T, Hirota E, Bito S, Niimi S, Usami S. Clinical course of hearing and language development in GJB2 and non-GJB2 deafness following habilitation with hearing aids. Audiol Neurootol. 2006;11(1):59-68.
- 7. Green GE, Scott DA, McDonald JM, Teagle HF, Tomblin BJ, Spencer LJ et al. Performance of cochlear implant recipients with GJB2-related deafness. Am J Med Genet. 2002;109(3):167-70
- 8. Sinnathuray AR, Toner JG, Clarke-Lyttle J, Geddis A, Patterson CC, Hughes AE. Connexin 26 (GJB2) gen-related deafness and speech intelligibility after cochlear implantation. Otol Neurotol 2004;25(4):935- 42.
- 9. Bernades R, Bortoncello S, Christiani TV, Sartorato EL, César e Silva R, Porto PR. Estudo molecular em crianças candidatas e submetidas ao implante coclear. Rev Bras Otorrinolaringol. 2006;72(3):333-6.
- 10. Wu CC, Lee YC, Chen PJ, Hsu CJ Predominance of genetic diagnosis and imaging results as predictors in determining the speech perception performance outcome after cochlear implantation in children. Arch Pediatr Adolesc Med. 2008;162(3):269-76.
- 11. Batissoco AC, Abreu-Silva RS, Braga MC, Lezirovitz K, Della-Rosa Vet al. Prevalence of GJB2 (connexin-26) and GJB6 (connexin-30) mutations in a cohort of 300 Brazilian hearing-impaired individuals: implications for diagnosis and genetic counseling. Ear Hear. 2009 Feb;30(1):1-7.
- 12. Cordeiro-Silva Mde F, Barbosa A, Santiago M, Provetti M, Rabbi-Bortolini E. Prevalence of 35delG/GJB2 and del (GJB6-D13S1830) mutations in patients with non-syndromic deafness from a population of Espírito Santo - Brazil. Braz J Otorhinolaryngol. 2010;76(4):428-32.
- 13. Dimitrijevic A, John MS, Picton TW. Auditory steady-state responses and word recognition in normal-hearing and hearing-impaired adults. Ear Hear. 2004;25(1):68-84.
- 14. Ferraz OB, Freitas SV, Marchiori LL. Análise das respostas obtidas por potenciais evocados auditivos de estado estável em indíviduos normais Rev Bras Otorrinolaringol. 2002;68(4):480-6.
- 15. Donini TS. A utilização do potencial evocado auditivo de estado estável no processo de indicação do aparelho de amplificação sonora individual em crianças com deficiência auditiva [Dissertação de Mestrado]. São Paulo: Pontifícia Universidade Católica de São Paulo; 2007.
- 16. Rodrigues GR, Lewis DR. Potenciais evocados auditivos de estado estável em crianças com perdas auditivas cocleares. Pro Fono. 2010;22(1):37-42.
-
17Organização Mundial da Saúde (World Health Organization). Prevention of blindeness and deafness: grades of hearing impairment. 1997. [internet]. http://www.who.int/pbd/deafness/hearing_impairment_grades/en/ Acesso em: 15/11/2010.
- 18. American Speech Language Hearing Association. Guidelines for the audiologic assessment of children from the birth through 36 months of age. ASHA. 1991;33(5):37-43.
- 19. Azevedo MF. Avaliação subjetiva da audição no primeiro ano de vida. Temas desenvolv. 1991;1(3):11-4.
- 20. Lanzetta BP, Frota S, Goldfeld M. Acompanhamento da adaptação de próteses auditivas em crianças surdas. Rev. CEFAC [online]. 2010;12(3):360-70.
- 21. Bitner-Glindzicz M. Hereditary deafness and phenotyping in humans. Br Med Bull. 2002;63:73-94.
- 22. Mueller R. Connexin 26 (GJB2) deafness homepage. In: Martini A, Mazzoli M, Stephens D, Read A. Definitions, Protocols and Guidelines in Genetic Hearing Impairment. London: Whurr Publishers Ltd; 2001. p. 176-80.
- 23. Shibata Y, Kumai M, Nishi K, Nakamura K. Diversity and molecular anatomy of gap junctions. Med Electron Microsc. 2001;34(3):153-9.
- 24. Cryns K, Van Camp, G. Deafness genes and their diagnostic applications. Audiol Neurootol. 2004;9(1):2-22.
- 25. Li R, Greinwald JH Jr, Yang L, Choo DI, Wenstrup RJ, Guan MX. Molecular analysis of the mitochondrial 12SrRNA and tRNASer (UNC) genes in pediatric subjects with non-syndromic hearing loss. J Med Genet. 2004;41(8):615-20.
- 26. Hismi BO, Yilmaz ST, Incesulu A, Tekin M. Effects of GJB2 genotypes on the audiological phenotype: variability is present for all genotypes. Int J Pediatr Otorhinolaryngol. 2006;70(10):1687-94.
- 27. Del Castillo FJ, Rodriguez-Ballesteros M, Martin Y, Arellano B, Gallo-Teran J, Morales-Angulo C, et al. Heteroplasmy for the 1555AG mutation in the mitochondrial 12S rRNA gene in six Spanish families with non-syndromic hearing loss. J Med Genet. 2003;40(8):632-6.
Publication Dates
-
Publication in this collection
07 Jan 2013 -
Date of issue
2012
History
-
Received
27 Sept 2011 -
Accepted
12 June 2012