Abstract
Gastroduodenal artery aneurysm is a disease with low incidence that manifests in a nonspecific form in the majority of cases, which hinders initial diagnosis. Symptomatic cases may present with abdominal pains or hemorrhage secondary to rupture. In cases in which the aneurysm ruptures, prognosis is poor and mortality can reach 40%. Steps should therefore be taken to ensure early diagnosis and treatment. Although open surgical treatment is an option, over recent years there has been a growing trend to use endovascular techniques. This report describes a rare case of a young patient with a gastroduodenal artery who was successfully treated with endovascular techniques.
Keywords:
aneurysm; endovascular procedures; vascular surgical procedures
Resumo
O aneurisma de artéria gastroduodenal é uma doença de baixa incidência que se manifesta de forma inespecífica na maioria das vezes, o que dificulta o diagnóstico inicial. Nos casos sintomáticos, pode ocorrer dor abdominal, além de hemorragia secundária à sua rotura. Nos casos de rotura aneurismática, o prognóstico é desfavorável, atingindo 40% de mortalidade. Assim, devem-se empregar os recursos necessários para o diagnóstico e intervenção terapêutica precoce. Embora o tratamento cirúrgico aberto seja uma opção, nos últimos anos, tem havido uma maior tendência ao tratamento endovascular. Relata-se um caso raro de paciente jovem portador de aneurisma de artéria gastroduodenal tratado com sucesso por meio da terapia endovascular.
Palavras-chave:
aneurisma; procedimentos endovasculares; procedimentos cirúrgicos vasculares
INTRODUCTION
Visceral aneurysms have low incidence (0.01 to 0.2% in the general population,11 Zuhaili B, Molnar RG, Malhotra NG. The endovascular management of a 3.5-cm gastroduodenal artery aneurysm presenting with gastritis and recurrent pancreatitis. Avicenna J Med. 2017;7(3):130-2. PMid:28791247. and gastroduodenal artery aneurysm is one of the least common (just 1.5% of all visceral aneurysms).22 Lu M, Weiss C, Fishman EK, Johnson PT, Verde F. Review of visceral aneurysms and pseudoaneurysms. J Comput Assist Tomogr. 2015;39(1):1-6. http://dx.doi.org/10.1097/RCT.0000000000000156. PMid:25319606.
http://dx.doi.org/10.1097/RCT.0000000000...
,33 Habib N, Hassan S, Abdou R, et al. Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review. Ann Surg Innov Res. 2013;7(1):4. http://dx.doi.org/10.1186/1750-1164-7-4. PMid:23587203.
http://dx.doi.org/10.1186/1750-1164-7-4...
In contrast to the majority of visceral aneurysms, gastroduodenal artery aneurysms tend to be symptomatic,11 Zuhaili B, Molnar RG, Malhotra NG. The endovascular management of a 3.5-cm gastroduodenal artery aneurysm presenting with gastritis and recurrent pancreatitis. Avicenna J Med. 2017;7(3):130-2. PMid:28791247. which may comprise minor symptoms such as nonspecific abdominal pains, or even major symptoms, such as hemodynamic instability, melena, and hematemesis (when an aneurysm ruptures into an organ of the digestive system).44 Shawky MS, Tan J, French R. Gastroduodenal artery aneurysm: a case report and concise review of literature. Ann Vasc Dis. 2015;8(4):331-3. http://dx.doi.org/10.3400/avd.cr.15-00086. PMid:26730262.
http://dx.doi.org/10.3400/avd.cr.15-0008...
The pathogenesis of gastroduodenal artery aneurysms is not fully understood. Trauma, arterial hypertension, and atherosclerosis have been identified as potential risk factors for these aneurysms. Other causes of development of gastroduodenal artery aneurysms are atherosclerosis, stenosis, or even congenital absence of the celiac trunk. The gastroduodenal and pancreaticoduodenal arteries are important routes of communication between the celiac trunk and the superior mesenteric artery. Increased blood flow through pancreaticoduodenal arteries, compensating for stenosis of the celiac trunk, may cause gastroduodenal artery aneurysms.33 Habib N, Hassan S, Abdou R, et al. Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review. Ann Surg Innov Res. 2013;7(1):4. http://dx.doi.org/10.1186/1750-1164-7-4. PMid:23587203.
http://dx.doi.org/10.1186/1750-1164-7-4...
Aneurysm rupture is linked with high mortality rates (up to 40%).22 Lu M, Weiss C, Fishman EK, Johnson PT, Verde F. Review of visceral aneurysms and pseudoaneurysms. J Comput Assist Tomogr. 2015;39(1):1-6. http://dx.doi.org/10.1097/RCT.0000000000000156. PMid:25319606.
http://dx.doi.org/10.1097/RCT.0000000000...
,33 Habib N, Hassan S, Abdou R, et al. Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review. Ann Surg Innov Res. 2013;7(1):4. http://dx.doi.org/10.1186/1750-1164-7-4. PMid:23587203.
http://dx.doi.org/10.1186/1750-1164-7-4...
When possible, early diagnosis of these aneurysms is the ideal way to avert unfavorable prognosis.22 Lu M, Weiss C, Fishman EK, Johnson PT, Verde F. Review of visceral aneurysms and pseudoaneurysms. J Comput Assist Tomogr. 2015;39(1):1-6. http://dx.doi.org/10.1097/RCT.0000000000000156. PMid:25319606.
http://dx.doi.org/10.1097/RCT.0000000000...
Many different resources can be used for diagnosis, such as magnetic resonance angiography and angiotomography, but angiography is considered the gold standard examination, because it has high sensitivity and offers the possibility of treatment during the same intervention.55 Babu A, Rattan A, Singhal M, Gupta A, Kumar S. Gastroduodenal artery aneurysm – A rare complication of traumatic pancreatic injury. Chin J Traumatol. 2016;19(6):368-70. http://dx.doi.org/10.1016/j.cjtee.2016.02.003. PMid:28088944.
http://dx.doi.org/10.1016/j.cjtee.2016.0...
,66 Navarro-Noguera E, Alberca-de-las-Parras F, Egea-Valenzuela J, et al. Gastroduodenal artery aneurysm presenting as a pancreatic mass. Rev Esp Enferm Dig. 2015;107(6):374. PMid:26031866.
The majority of guidelines recommend treatment of visceral aneurysms with a diameter of 2 cm or greater. However, gastroduodenal artery aneurysms justify intervention as soon as they are discovered,11 Zuhaili B, Molnar RG, Malhotra NG. The endovascular management of a 3.5-cm gastroduodenal artery aneurysm presenting with gastritis and recurrent pancreatitis. Avicenna J Med. 2017;7(3):130-2. PMid:28791247. as there have been reports of rupture of small aneurysms and there doesn’t appear to be any clear relationship with diameter.22 Lu M, Weiss C, Fishman EK, Johnson PT, Verde F. Review of visceral aneurysms and pseudoaneurysms. J Comput Assist Tomogr. 2015;39(1):1-6. http://dx.doi.org/10.1097/RCT.0000000000000156. PMid:25319606.
http://dx.doi.org/10.1097/RCT.0000000000...
Although open surgical treatment is effective, over recent years there has been an increasing tendency to employ endovascular treatment, because it is less invasive and response to treatment is good. Open surgery is reserved for cases with rupture and hemodynamic instability or cases with anatomy that is not favorable for endovascular repair.33 Habib N, Hassan S, Abdou R, et al. Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review. Ann Surg Innov Res. 2013;7(1):4. http://dx.doi.org/10.1186/1750-1164-7-4. PMid:23587203.
http://dx.doi.org/10.1186/1750-1164-7-4...
We describe the case of a young patient diagnosed with an aneurysm of the gastroduodenal artery and stenosis of the celiac trunk who was successfully treated using endovascular techniques.
CASE DESCRIPTION
The patient was a 20-year-old male with a history of chronic gastritis and a hiatus hernia. He had presented complaining of episodes of frequent abdominal pains, sometimes debilitating, associated with nausea and vomiting, with onset around 10 days prior to hospital admission.
On physical examination he was in good general health, with good color, hydrated, acyanotic, no sign of jaundice, free from fever, with normal blood pressure and peripheral pulses present. He had diffuse abdominal pains on palpation and attenuated bowel sounds.
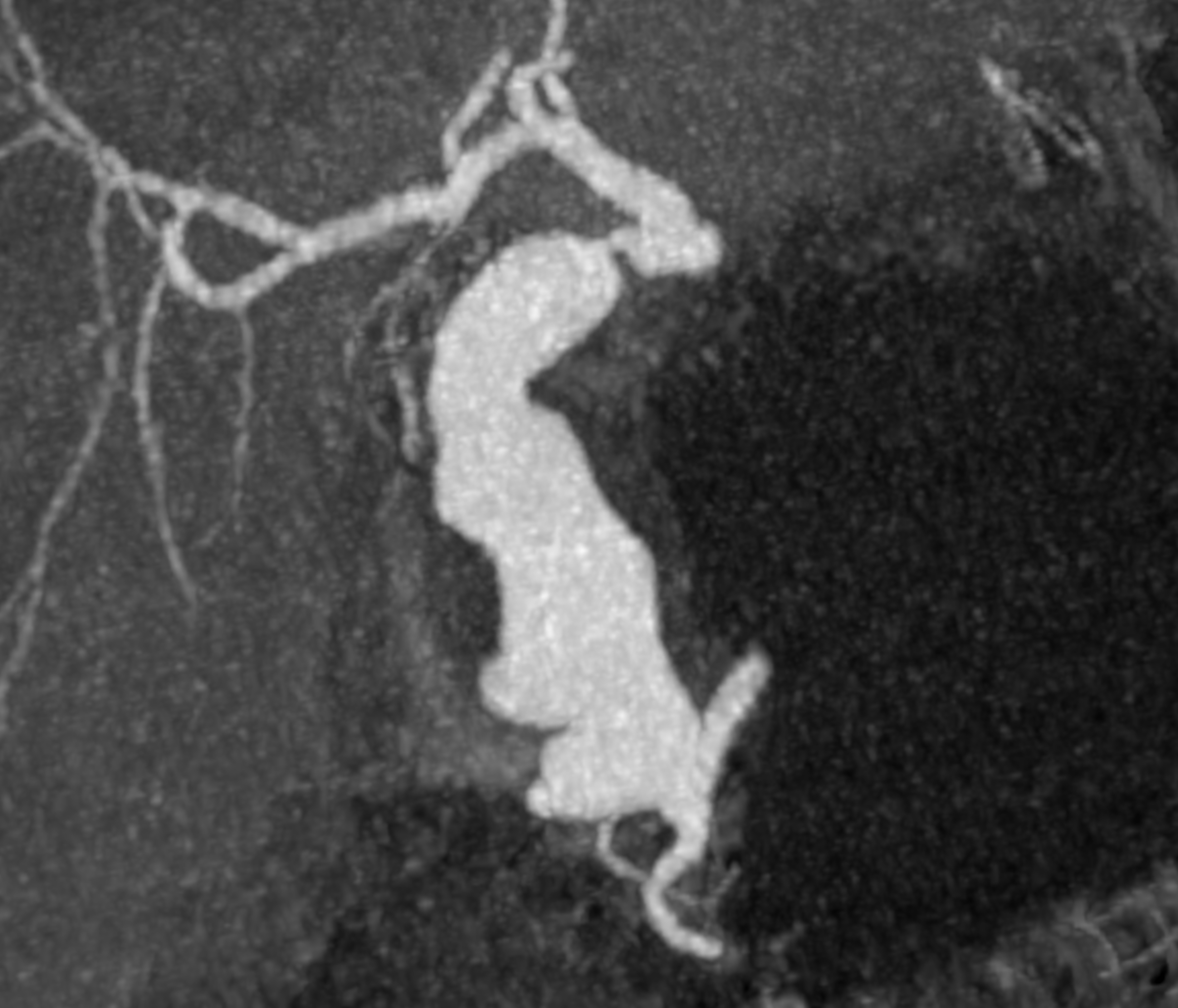
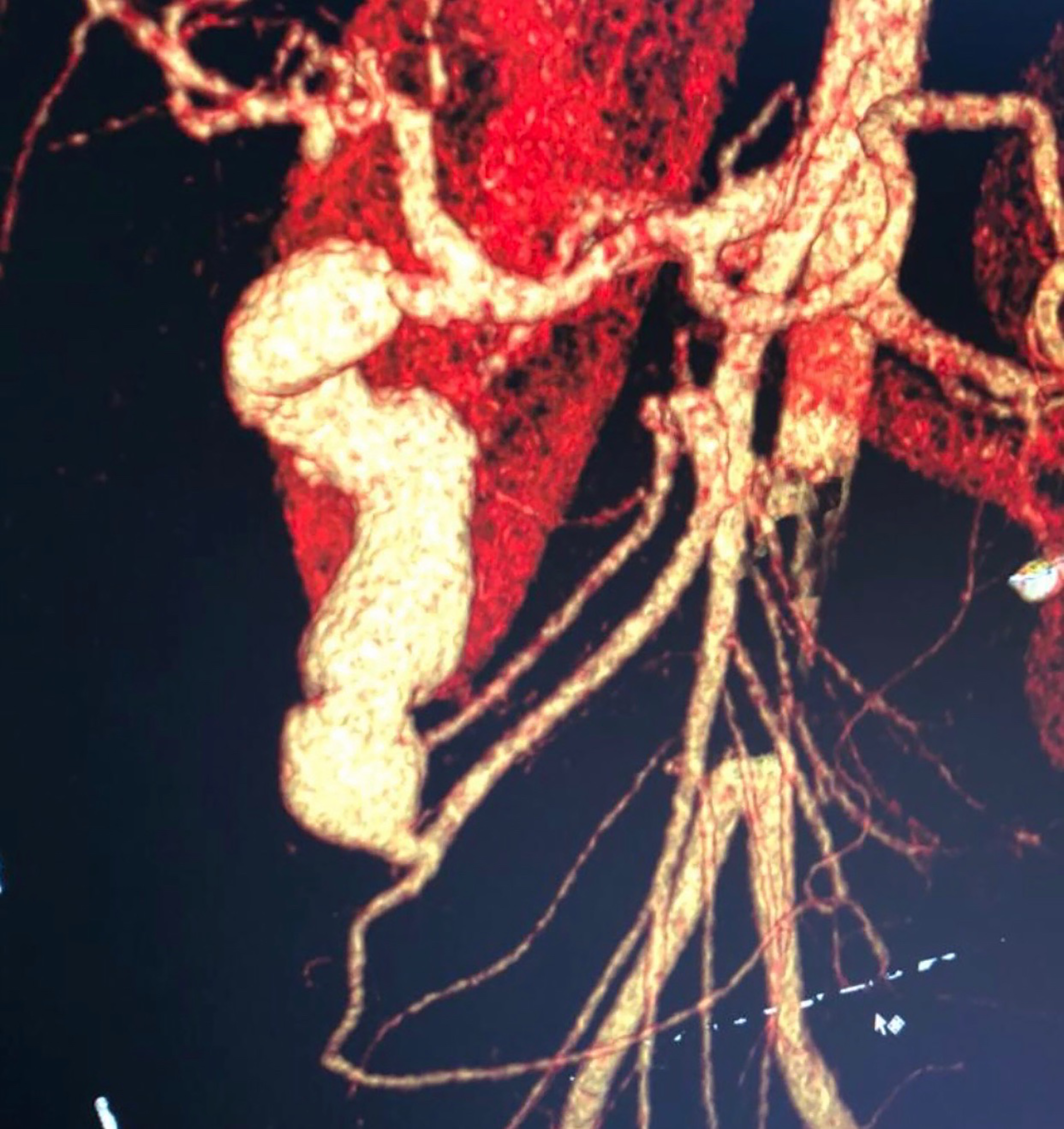
After assessment by the general surgery team, the patient underwent computed tomography of the abdomen, which showed a gastroduodenal artery aneurysm and significant stenosis of the celiac trunk (Figure 1). The vascular surgery team was called in and angiotomography was performed, showing the gastroduodenal artery aneurysm with a maximum diameter of 3.6 cm, length of 9.5 cm and no signs of rupture (Figures 2 and 3).
After careful consideration of the case and the patient’s general status, endovascular treatment of the aneurysm was proposed. The right common femoral artery was catheterized, a 5 French introducer was inserted and a 5 French Cobra catheter was positioned within the superior mesenteric artery (access to the aneurysm via the celiac trunk was ruled out because of the stenosis). A Rebar® microcatheter was then inserted and advanced along the path of the pancreaticoduodenal artery to access the gastroduodenal artery. Embolization was performed using a total of 19 Concerto® coils of varying sizes (6/20 mm, 8/30 mm, 9/30 mm, and 10/30 mm) and also Onyx® embolizing agent (Figure 4) and angiographic results after the procedure were satisfactory (Figure 5).
There was significant remission of the patient’s pain after the procedure and he was discharged 2 days after surgery in a satisfactory general condition. Six months after the procedure, the patient underwent angiotomography once more, which showed complete exclusion of the aneurysm and no complications related to the procedure (Figure 6). The celiac trunk stenosis was not treated because around 12 months after the procedure the patient was still stable and asymptomatic.
DISCUSSION
Although considered rare,66 Navarro-Noguera E, Alberca-de-las-Parras F, Egea-Valenzuela J, et al. Gastroduodenal artery aneurysm presenting as a pancreatic mass. Rev Esp Enferm Dig. 2015;107(6):374. PMid:26031866. visceral aneurysms are sometimes associated with fatal outcomes, primarily caused by ruptures, which have mortality rates in the range of 20 to 70%, depending on the site. Since diagnostic imaging methods are now widely available, these aneurysms are very often discovered early, while still in an asymptomatic phase (as incidental findings), in time to perform elective surgery.77 Dorigo W, Pulli R, Azas L, et al. Early and intermediate results of elective endovascular treatment of true visceral artery aneurysms. Ann Vasc Surg. 2016;30:211-8. http://dx.doi.org/10.1016/j.avsg.2015.06.097. PMid:26381325.
http://dx.doi.org/10.1016/j.avsg.2015.06...
Stenosis of the celiac trunk, very often provoked by the arched ligament of the diaphragm (median arcuate ligament syndrome), can be the cause of formation of aneurysms, primarily because of increased retrograde collateral flow through the gastroduodenal artery and other adjacent vessels.88 Arazińska A, Polguj M, Wojciechowski A, Trębiński Ł, Stefańczyk L. Median arcuate ligament syndrome: predictor of ischemic complications? Clin Anat. 2016;29(8):1025-30. http://dx.doi.org/10.1002/ca.22773. PMid:27560288.
http://dx.doi.org/10.1002/ca.22773...
They can be associated with acute or chronic pancreatitis, cholangitis, trauma, stenosis of the celiac trunk or iatrogenic causes.99 Zaafouri H, Hasnaoui A, Essghaeir S, et al. Ascending Cholangitis secondary to migrated embolization coil of gastroduodenal artery pseudo-aneurysm a case report. BMC Surg. 2017;17(1):30. http://dx.doi.org/10.1186/s12893-017-0227-9. PMid:28330448.
http://dx.doi.org/10.1186/s12893-017-022...
In those related to pancreatitis, activity of inflammatory mediators and proteolytic pancreatic enzymes provokes destruction of the walls of vessels in the region, leading to formation of pseudoaneurysms in the majority of cases.33 Habib N, Hassan S, Abdou R, et al. Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review. Ann Surg Innov Res. 2013;7(1):4. http://dx.doi.org/10.1186/1750-1164-7-4. PMid:23587203.
http://dx.doi.org/10.1186/1750-1164-7-4...
Alcohol abuse, prior cholecystectomy, congenital variants, Marfan Syndrome, polyarteritis nodosa, fibromuscular dysplasias, and hepatic cirrhosis have all also been described as associated factors.55 Babu A, Rattan A, Singhal M, Gupta A, Kumar S. Gastroduodenal artery aneurysm – A rare complication of traumatic pancreatic injury. Chin J Traumatol. 2016;19(6):368-70. http://dx.doi.org/10.1016/j.cjtee.2016.02.003. PMid:28088944.
http://dx.doi.org/10.1016/j.cjtee.2016.0...
In contrast with the majority of visceral aneurysms, gastroduodenal artery aneurysms are generally symptomatic and can manifest with nonspecific abdominal pains (present in 46% of cases) and nausea and vomiting, or even shock, in cases in which the aneurysm ruptures.44 Shawky MS, Tan J, French R. Gastroduodenal artery aneurysm: a case report and concise review of literature. Ann Vasc Dis. 2015;8(4):331-3. http://dx.doi.org/10.3400/avd.cr.15-00086. PMid:26730262.
http://dx.doi.org/10.3400/avd.cr.15-0008...
,66 Navarro-Noguera E, Alberca-de-las-Parras F, Egea-Valenzuela J, et al. Gastroduodenal artery aneurysm presenting as a pancreatic mass. Rev Esp Enferm Dig. 2015;107(6):374. PMid:26031866. However, since they do not have characteristic clinical status, early diagnosis is very often difficult. Notwithstanding, in many cases, using magnetic resonance angiography and angiotomography will result in diagnosis. Angiography is considered the gold standard, not only because of its high diagnostic sensitivity, but also because it offers the opportunity to treat during the same intervention.55 Babu A, Rattan A, Singhal M, Gupta A, Kumar S. Gastroduodenal artery aneurysm – A rare complication of traumatic pancreatic injury. Chin J Traumatol. 2016;19(6):368-70. http://dx.doi.org/10.1016/j.cjtee.2016.02.003. PMid:28088944.
http://dx.doi.org/10.1016/j.cjtee.2016.0...
,66 Navarro-Noguera E, Alberca-de-las-Parras F, Egea-Valenzuela J, et al. Gastroduodenal artery aneurysm presenting as a pancreatic mass. Rev Esp Enferm Dig. 2015;107(6):374. PMid:26031866.
When available, endovascular techniques are preferable because of their success rates (78 to 97%)11 Zuhaili B, Molnar RG, Malhotra NG. The endovascular management of a 3.5-cm gastroduodenal artery aneurysm presenting with gastritis and recurrent pancreatitis. Avicenna J Med. 2017;7(3):130-2. PMid:28791247. and the low rates of complications and reoperation.77 Dorigo W, Pulli R, Azas L, et al. Early and intermediate results of elective endovascular treatment of true visceral artery aneurysms. Ann Vasc Surg. 2016;30:211-8. http://dx.doi.org/10.1016/j.avsg.2015.06.097. PMid:26381325.
http://dx.doi.org/10.1016/j.avsg.2015.06...
Generally, embolization materials are employed (coils). Open surgery is reserved for cases of rupture with hemodynamic instability or cases with anatomy that is unfavorable for endovascular repair.33 Habib N, Hassan S, Abdou R, et al. Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review. Ann Surg Innov Res. 2013;7(1):4. http://dx.doi.org/10.1186/1750-1164-7-4. PMid:23587203.
http://dx.doi.org/10.1186/1750-1164-7-4...
The need to treat stenosis of the celiac trunk, when present, is still uncertain. Revascularization in this territory is performed with the intention of preventing gastrointestinal ischemia and emergence of additional aneurysms in adjacent vessels. However, because these complications have low incidence, repair of the gastroduodenal artery aneurysm only is considered sufficient.1010 Boll JM, Sharp KW, Garrard CL, Naslund TC, Curci JA, Valentine RJ. Does management of true aneurysms of peripancreatic arteries require repair of associated celiac artery stenosis? J Am Coll Surg. 2017;224(2):199-203. http://dx.doi.org/10.1016/j.jamcollsurg.2016.10.030. PMid:27773774.
http://dx.doi.org/10.1016/j.jamcollsurg....
-
How to cite: Casas ALF, Camargo MPF, Moisés CB, Trad HS, Joviliano EE. Endovascular treatment of gastroduodenal artery aneurysm: case report. J Vasc Bras. 2019;18:e20190019. https://doi.org/10.1590/1677-5449.190019
-
Financial support: None.
-
The study was carried out at Universidade de Franca (UNIFRAN), Franca, SP, Brazil.
REFERÊNCIAS
-
1Zuhaili B, Molnar RG, Malhotra NG. The endovascular management of a 3.5-cm gastroduodenal artery aneurysm presenting with gastritis and recurrent pancreatitis. Avicenna J Med. 2017;7(3):130-2. PMid:28791247.
-
2Lu M, Weiss C, Fishman EK, Johnson PT, Verde F. Review of visceral aneurysms and pseudoaneurysms. J Comput Assist Tomogr. 2015;39(1):1-6. http://dx.doi.org/10.1097/RCT.0000000000000156 PMid:25319606.
» http://dx.doi.org/10.1097/RCT.0000000000000156 -
3Habib N, Hassan S, Abdou R, et al. Gastroduodenal artery aneurysm, diagnosis, clinical presentation and management: a concise review. Ann Surg Innov Res. 2013;7(1):4. http://dx.doi.org/10.1186/1750-1164-7-4 PMid:23587203.
» http://dx.doi.org/10.1186/1750-1164-7-4 -
4Shawky MS, Tan J, French R. Gastroduodenal artery aneurysm: a case report and concise review of literature. Ann Vasc Dis. 2015;8(4):331-3. http://dx.doi.org/10.3400/avd.cr.15-00086 PMid:26730262.
» http://dx.doi.org/10.3400/avd.cr.15-00086 -
5Babu A, Rattan A, Singhal M, Gupta A, Kumar S. Gastroduodenal artery aneurysm – A rare complication of traumatic pancreatic injury. Chin J Traumatol. 2016;19(6):368-70. http://dx.doi.org/10.1016/j.cjtee.2016.02.003 PMid:28088944.
» http://dx.doi.org/10.1016/j.cjtee.2016.02.003 -
6Navarro-Noguera E, Alberca-de-las-Parras F, Egea-Valenzuela J, et al. Gastroduodenal artery aneurysm presenting as a pancreatic mass. Rev Esp Enferm Dig. 2015;107(6):374. PMid:26031866.
-
7Dorigo W, Pulli R, Azas L, et al. Early and intermediate results of elective endovascular treatment of true visceral artery aneurysms. Ann Vasc Surg. 2016;30:211-8. http://dx.doi.org/10.1016/j.avsg.2015.06.097 PMid:26381325.
» http://dx.doi.org/10.1016/j.avsg.2015.06.097 -
8Arazińska A, Polguj M, Wojciechowski A, Trębiński Ł, Stefańczyk L. Median arcuate ligament syndrome: predictor of ischemic complications? Clin Anat. 2016;29(8):1025-30. http://dx.doi.org/10.1002/ca.22773 PMid:27560288.
» http://dx.doi.org/10.1002/ca.22773 -
9Zaafouri H, Hasnaoui A, Essghaeir S, et al. Ascending Cholangitis secondary to migrated embolization coil of gastroduodenal artery pseudo-aneurysm a case report. BMC Surg. 2017;17(1):30. http://dx.doi.org/10.1186/s12893-017-0227-9 PMid:28330448.
» http://dx.doi.org/10.1186/s12893-017-0227-9 -
10Boll JM, Sharp KW, Garrard CL, Naslund TC, Curci JA, Valentine RJ. Does management of true aneurysms of peripancreatic arteries require repair of associated celiac artery stenosis? J Am Coll Surg. 2017;224(2):199-203. http://dx.doi.org/10.1016/j.jamcollsurg.2016.10.030 PMid:27773774.
» http://dx.doi.org/10.1016/j.jamcollsurg.2016.10.030
Publication Dates
-
Publication in this collection
25 Nov 2019 -
Date of issue
2019
History
-
Received
08 Apr 2019 -
Accepted
17 Sept 2019