IMAGEM EM MEDICINA
Retroperitoneal sarcoma-like malakoplakia
Paulo Henrique G.F. DiasI; Luiz Edison SlongoII; Frederico R. RomeroIII; Guilherme R. PaquesIV; Regina Paula X. GomesV; Luiz Carlos de Almeida RochaVI
IUrology Intern, Hospital de Clínicas, Universidade Federal do Paraná (UFPR), Curitiba, PR, Brazil
IIPhD in Surgical Clinics; Full Professor of Urology, Hospital de Clínicas, UFPR, Curitiba, PR, Brazil
IIIPhD Student in Surgical Clinics; Substitute Professor of Urology, Hospital de Clínicas, UFPR, Curitiba, PR, Brazil
IVPathology Intern, Hospital de Clínicas, UFPR, Curitiba, PR, Brazil
VPhD in Pathology; Pathologist, Hospital de Clínicas, UFPR, Curitiba, PR, Brazil
VIPhD in Surgical Clinics; Full Professor and Chief of Urology, Hospital de Clínicas, UFPR, Curitiba, PR, Brazil
Correspondence Correspondence to: Frederico R. Romero Rua Emiliano Perneta, 653/41 Curitiba, PR, Brazil - CEP: 80420-080 frederico.romero@gmail.com
A variety of primary tumors originate in the retroperitoneum, and they may achieve large volumes before being diagnosed. The most common retroperitoneal tumors are sarcomas, lymphomas, carcinomas, germ cell tumors, undifferentiated malignant tumors, and benign tumors1,2. Malakoplakia is a chronic granulomatous benign disease that is frequently misdiagnosed as a malignant disease3,4. We illustrate an unusual case of extensive retroperitoneal malakoplakia mimicking retroperitoneal sarcoma.
A 20-year-old male was admitted in our institution with a 3-month history of back pain, hematuria, lower urinary tract symptoms, and weight loss of 12 kg. Past medical history was non-significant. On physical examination, he had a scaphoid abdomen with no palpable masses. DRE showed a normal prostate, with a large palpable mass with undefined limits above the prostate.
Laboratory tests revealed serum creatinine of 1.5 mg/dL, PSA of 0.3 mg/dL, negative HIV-ELISA test, positive urine culture for Escherichia coli, negative culture for acid-fast bacilli, and a negative PPD.
Ultrasound showed a retrovesical mass with increased blood flow on Doppler. CT scan demonstrated a solid heterogeneously enhancing mass topographically centered in the left seminal vesicle. The mass measured 4.5 x 6.0 x 5.5 cm, and it infiltrated the prostate gland, urinary bladder, and left distal ureter. There was severe hydroureteronephrosis with marked reduction of renal cortical thickness on the left, and mild right hydroureteronephrosis. MRI showed a large retrovesical mass infiltrating the bladder (Figure 1). At cystoscopy, the mass involved the base and the left wall of the bladder, including the left ureteral orifice.
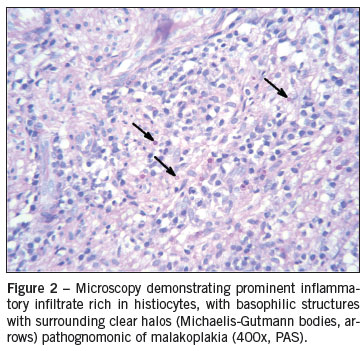
With diagnostic suspicion of retroperitoneal sarcoma, TRUS-guided biopsy was performed, which revealed chronic sclerotic xanthogranulomatous inflammation. Repeated transrectal biopsy showed only acute and chronic inflammatory process. Since malignancy was still suspected, requiring aggressive local resection pending pathological confirmation, the patient underwent transurethral resection of the lesion in an attempt to collect more tissue for pathologic analysis, and stenting of the right ureter to avoid further damage of renal function during investigation. Histhopathology with periodic acid-Schiff (PAS, Figure 2) identified basophilic structures with surrounding clear halos (Michaelis-Gutmann bodies), characteristic of malakoplakia.
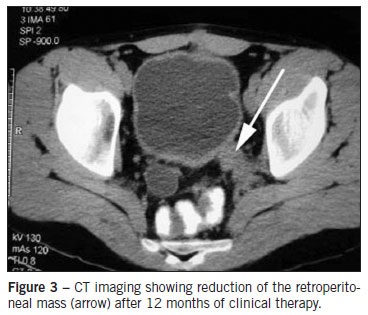
The patient was treated with fluoroquinolone, bethanechol, and vitamin C. Follow-up at 6 and 12 months (Figure 3) showed effective and progressive success of clinical therapy, with no need of further surgical intervention.
DISCUSSION
Malakoplakia is an unusual chronic inflammatory disease frequently associated with immunodeficiency and a defective phagolysosomal activity3-6. It was first described by Von Hansemann in 1902, and it is characterized by tumorlike lesions, single or multiple, which may affect any organ of the body3,4,7. It is frequently a diagnostic challenge, in which the main differential diagnosis is malignancy5.
Malakoplakia involves the genitourinary tract in 80% of cases3,5. The bladder is the most commonly affected organ, followed by the upper urinary tract1,3. Other reported locations include the retroperitoneum, gastrointestinal tract, central nervous system, female genital tract, lungs, adrenal glands, spleen, pancreas, mensenteric nodes, thyroid, eyes, skin, and bones3,5,7.
Urinary malakoplakia is more common in females, while extraurinary malakoplakia is more frequently seen in men4-6. Age of diagnosis ranges from six weeks to 85 years, peaking in the fifth decade of life5, similar to primary sarcoma8. Immunodeficiency disorders and the use of immunosuppressive drugs are common9, and most cases are associated with urinary tract infection or other systemic infections6.
Malakoplakia results from a defective phagocytosis system with incomplete bacterial digestion by macrophages and histiocytes. Bacterial debris accumulates in the cytoplasm of these cells and usually becomes mineralized due to deposition of calcium and iron on bacterial glycolipid5-7. This basophilic - PAS positive - inclusion structures with surrounding clear halos may be visualized by microscopy as pathognomonic intracytoplasmic Michaelis-Gutmann bodies4,7, which have the appearance of concentric rings9.
Clinically, patients usually present abdominal pain, weight loss, diarrhea, hematuria and/or fever, with different symptoms according to the affected organ3. Involvement of the bladder is characterized by long-standing urinary symptoms and hematuria4. Most cases have positive urine cultures, usually with Gram-negative bacteria4,9. When the ureter is involved, obstruction may lead to loss of the ipsilateral renal parenchyma3,4.
Diagnosis of malakoplakia is difficult, and it cannot be made exclusively in clinical or imaging ground. Definitive diagnosis is based on the hystopathologic findings described above3. However, both false-negative and false-positive diagnosis may occur following biopsy8,9.
Malakoplakia located in the lower urinary tract can usually be managed non-surgically. Long-term antibiotics such as fluoroquinolones and thrimetoprim-sulfamethoxazole, both of which achieve high intracellular levels, have been shown efficient3,7. There is evidence that concomitant use of bethanechol may improve macrophage function6. Similarly, ascorbic acid may enhance the effect of bacteriolytic enzymes, compromised by associated immune deficiency9. Immunosuppressive drugs should be discontinued if possible. In contrast with isolated disease of lower urinary tract that usually presents good prognosis, extensive pelvic malakoplakia may be aggressive, invasive, and even lethal3,5. Surgical procedures are restricted to unresponsive clinical therapy3. Some cases respond to clinical and endoscopic treatment, as in the case reported herein, while others may require aggressive surgical intervention6. The prognosis of patients with malakoplakia is usually good4. Follow-up, however, must be careful because long-term recurrence may occur3.
Malakoplakia is a chronic benign process that may present as a tumoral lesion of the retroperitoneum invading the bladder and adjacent structures. It should always be kept in mind by surgeons and pathologists as a differential diagnosis of retroperitoneal sarcoma to avoid iatrogenesis, especially after multiple negative biopsies, in which pathognomonic Michaelis-Gutmann bodies should be carefully investigated.
Study conducted at Universidade Federal do Paraná (UFPR), Curitiba, PR, Brazil
©2011 Elsevier Editora Ltda. Todos os direitos reservados.
- 1. Arlen M, Marcove RC. Retroperitoneal sarcomas. In: Arlen M, Marcove RC, editors. Surgical management of soft tissue sarcomas. Philadelphia: W.B. Saunders; 1987. p. 220.
- 2. Pinson CW, ReMine SG, Fletcher WS, Braasch JW. Long-term results with primary retroperitoneal tumors. Arch Surg. 1989;124:1168-73.
- 3. Velasquez Lopez Juan G, Velez Hoyos A, Uribe Arcila JF. Malakoplasia in urology: six cases report and review of the literature. Actas Urol Esp. 2006;30:610-8.
- 4. Patnayak R, Reddy MK, Subramanian S, Jena A, Ravisankar G, Dandu RS. An unusual case of bilateral hydroureteronephrosis caused by uretero-vesical malakoplakia in a young male: a case report and review of the literature. Cases J. 2009;29:7527.
- 5. Oladipo A, Somaiya P, Kassab A, Liddicoat A, Mathew J. A rare cause of pelvic malakoplakia mimicking advanced cervical cancer infiltrating the bladder. J Obstet Gyenaecol. 2007;27:749-51.
- 6. Shah A, Chandran H. Malakoplakia of bladder in childhood. Pediatr Surg Int. 2005;21:113-5.
- 7. Wielenberg AJ, Demos TC, Rangachari B, Turk T. Malacoplakia presenting as a solitary renal mass. AJR Am J Roentgenol. 2004;183:1703-5.
- 8. Chew C, Reid R, O'Dwyer PJ. Value of biopsy in the assessment of a retroperitoneal mass. Surgeon. 2006;4:79-81.
- 9. Kobayashi A, Utsunomiya Y, Kono M, Ito Y, Yamamoto I, Osaka N, et al. Malakoplakia of the kidney. Am J Kidney Dis. 2008;51:326-30.
Correspondence to:
Publication Dates
-
Publication in this collection
12 Jan 2012 -
Date of issue
Dec 2011