Abstract
Vaginismus is a poorly understood disorder, characterized by an involuntary muscular spasm of the pelvic floor muscles and outer third of the vagina during intercourse attempt, which results in aversion to penetration. It is reported to affect 1-7% of women worldwide. With this report the authors aim to describe the case of a young patient with vaginismus in whom techniques usually from the chronic pain domain were used as part of her multimodal therapeutic regimen.
Keywords
Vaginismus; Pulsed radiofrequency; Pudendal nerve; Trigger point; Chronic pain
Resumo
O vaginismo é uma doença pouco compreendida que se caracteriza por uma contração muscular involuntária dos músculos do pavimento pélvico e do terço externo da vagina durante as tentativas de intercurso sexual, o que resulta em aversão à penetração. Estima-se que possa afetar entre 1%-7% da população feminina mundial. Com este relato os autores pretendem apresentar o caso de uma paciente jovem com vaginismo na qual foram usadas técnicas habitualmente do domínio da medicina da dor crônica como parte do seu esquema terapêutico multimodal.
Palavras-chave
Vaginismo; Radiofrequência pulsada; Nervo pudendo; Ponto gatilho; Dor crônica
Introduction
Vaginismus is a disorder characterized by involuntary contraction of the pelvic floor and vaginal muscles, which makes sex intercourse difficult or impossible.11 Melnik T, Hawton K, McGuire H, et al. Interventions for vaginismus. Cochrane Database Syst Rev. 2012;12:CD001760. Although it was first described over 100 years ago, it remains poorly diagnosed and undertreated, a fact that becomes more relevant if one takes into account that compared to other sexual disorders, especially of desire and orgasm, it appears to be one whose treatment has the greatest potential for success.22 Pacik PT. Vaginismus: another ignored problem. Sex Culture. 2014;18:737-8. Several treatments have been used over the years, including sexual therapy, desensitization, hypnotherapy, vaginal dilators and injection of botulinum toxin, among others.22 Pacik PT. Vaginismus: another ignored problem. Sex Culture. 2014;18:737-8.,33 Pacik PT. Vaginismus: review of current concepts and treatment using botox injections, bupivacaine injections, and progressive dilation with the patient under anesthesia. Aesth Plast Surg. 2011;35:1160-4. Nevertheless, the optimal approach has not been determined, and both our clinical experience and current international literature point toward the pulsed radiofrequency (PRF) because its neuromodulatory properties are useful in the treatment of refractory pain.44 Rhame EE, Levey KA, Gharibo CG. Successful treatment of refractory pudendal neuralgia with pulsed radiofrequency. Pain Physician. 2009;12:633-8.
5 Cahana A, Van Zundert J, Macrea L, et al. Pulsed radiofrequency: current clinical and biological literature available. Pain Med. 2006;7:411-23.
6 Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.-77 Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008;12:37-41.
Clinical case
Female patient, 29 years old, nulliparous, ASA II due to diabetes mellitus (DM) type I since adolescence, taking insulin with good glycemic control in outpatient service, and with a history of repeated vaginal infections. The patient was referenced to the Pain Medicine Unit (PMU) of our institution due to complaints of vulvodynia and dyspareunia with two years of evolution. She had no history of aggression, trauma or accident; had surgical history of conization. At the time of referral, she was attending psychiatric and gynecologic consultations and in treatment with estazolam, escitalopram and topical dibucaine for use before sex intercourse. She described a self-limited and only temporary relief of pain symptoms with the latter drug.
At the physical examination, the patient had a marked sensitivity in the lower half of the vaginal introitus, disabling and limiting for clinical observation itself, and she tolerated with difficulty, for example, digital or compress vaginal examination. In this context, infiltration of the vaginal trigger points (TP) was proposed. The technique was performed under sedation in the outpatient unit (Fig. 1), and consisting of infiltration of the introitus at four, five, six, seven, and eight o'clock markers, with 0.2% ropivacaine (2 mg.mL-1) and clonidine (100 µg). No complications were recorded during this procedure. Four months after, the patient reported improvement of vulvodynia, but vaginismus was present at the physical examination. Thus, she was advised to undergo individual hypnotherapy sessions and bilateral PRF of the pudendal nerve, which she accepted.
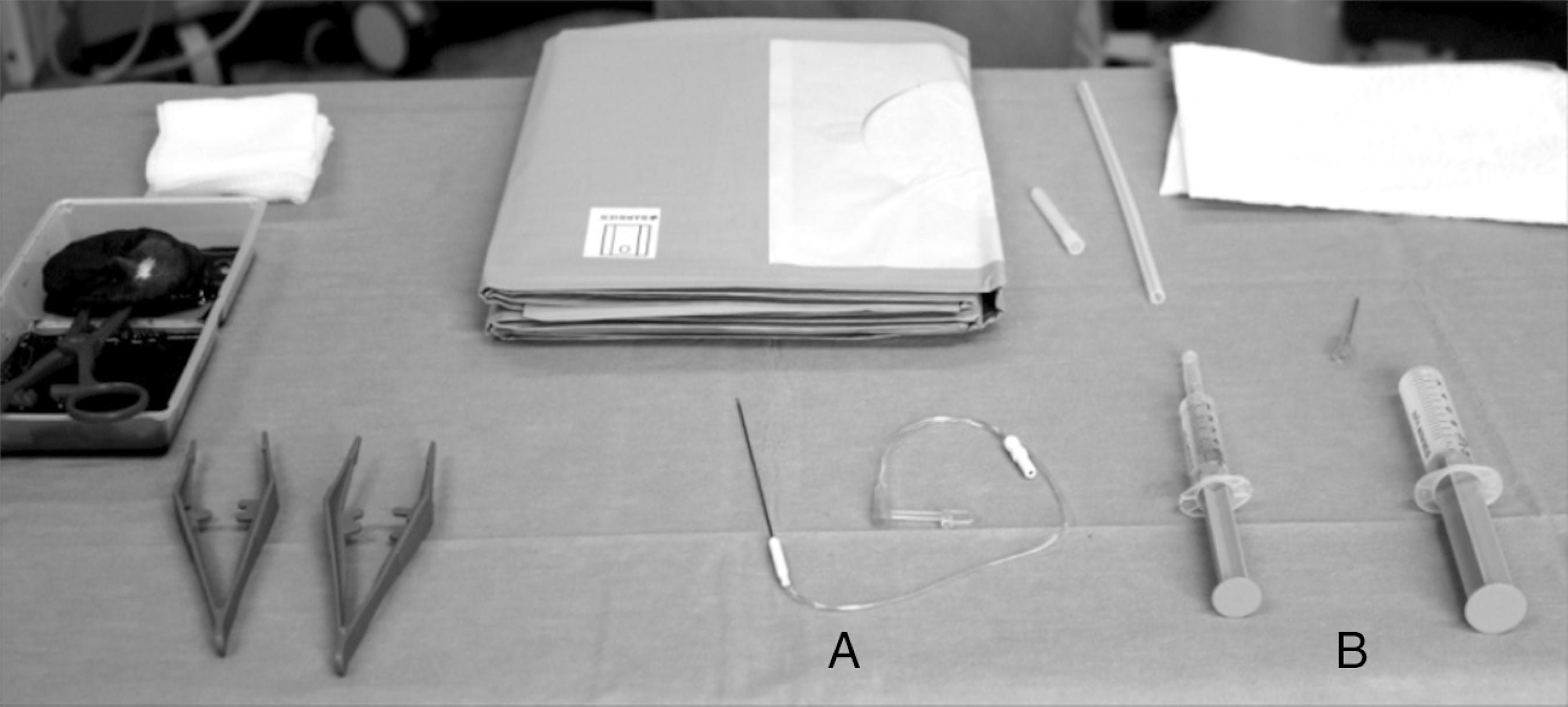
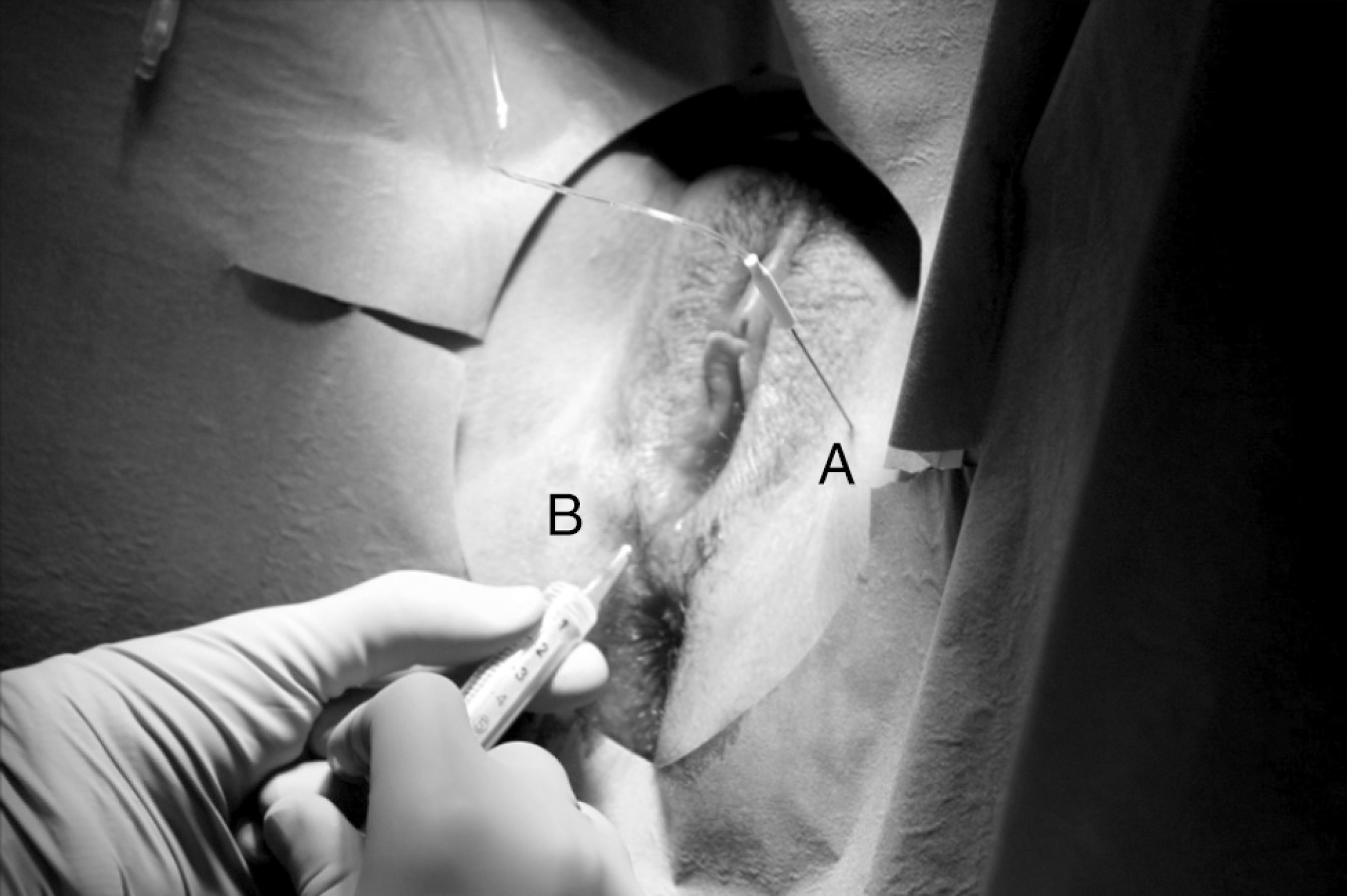
Patient at the outpatient unit, under deep sedation to trigger point infiltration. During the procedure, an American Society of Anesthesiologists standard monitoring was used.
On procedure day, upon arrival to the operating room, the patient was premedicated with intravenous (IV) fentanyl (0.05 mg) and midazolam (1 mg) and placed in gynecological position. Subsequently, she was anesthetized with propofol bolus, a total of 270 mg IV. After proper disinfection, the ischial spine (IS) and insertion point of the sacrospinous ligament were identified transvaginally. Medially to IS, a 23G radio frequency needle with 10 cm long and 0.5 cm active tip was introduced gradually, with 2 Hz motor stimulus until pudendal nerve identification, visually confirmed by the occurrence of contraction of the external anal sphincter muscle (Fig. 2). Subsequently, an alternating current was applied bilaterally to the pudendal nerves for 240 s (2 cycles of 120 s). It has been infiltrated also, for the second time, a TP at five and seven o'clock with 0.2% ropivacaine and methylprednisolone acetate (Depo-Medrol®) (Fig. 3). The procedure was well tolerated by the patient, and no complications were reported.
Radio frequency (RF) materials. In the image it is possible to see the RF needle (A), as well as the syringe with 0.2% ropivacaine and Depomedrol® (B) to infiltration of trigger points.
RF needle placed juxtaposed to the pudendal nerve during emission of alternating electric current (A). Infiltration of a trigger point (B) is also displayed.
In the first 12 months of follow-up, the patient reported significant clinical improvement and managed using progressive size dilators and attempted penetration. The pain complaints were limited to the vaginal vault. From the 13th month, the pain intensity increased, although to a lower threshold than when she was initially referred to the PMU. Given these circumstances, it was decided to repeat the PRF with the same protocol used in the first intervention. Five months later, the patient has not required a new differentiated intervention by the PMU.
Discussion
Currently, almost half the world's female population suffers from some kind of sexual dysfunction.55 Cahana A, Van Zundert J, Macrea L, et al. Pulsed radiofrequency: current clinical and biological literature available. Pain Med. 2006;7:411-23. Vaginismus is one of these disorders and is estimated to affect up to 7% of women, a figure that may represent an underestimation, as many of these patients tend to be quite reserved and not to share their health problem.33 Pacik PT. Vaginismus: review of current concepts and treatment using botox injections, bupivacaine injections, and progressive dilation with the patient under anesthesia. Aesth Plast Surg. 2011;35:1160-4.
Vaginismus tends to be a psychosomatic problem. That is, although in a high percentage of cases the etiology appears to be related to psychological problems the spasmodic reaction preventing penetration is physical.88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8. Psychologically, many of these women share a history of traumatic sexual intercourse, sexual aversion or family and/or religious negative constraints regarding sex, a history not described in our case.33 Pacik PT. Vaginismus: review of current concepts and treatment using botox injections, bupivacaine injections, and progressive dilation with the patient under anesthesia. Aesth Plast Surg. 2011;35:1160-4.,88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8.
However, the etiology may also be primarily physical. In fact, women with suspected diagnosis should be the subject of careful examination, as a basic assessment cannot find support for their complaints.88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8. Possible pain origins are malformations of the hymen, clitoris or labia; sexually transmitted diseases; endometriosis; pelvic inflammatory disease; cancer; insufficient lubrication; vaginal atrophy or abnormal wound healing.33 Pacik PT. Vaginismus: review of current concepts and treatment using botox injections, bupivacaine injections, and progressive dilation with the patient under anesthesia. Aesth Plast Surg. 2011;35:1160-4.,88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8. Furthermore, our patient has DM, an endocrinopathy with multiple microvascular complications, particularly neuropathy. In a meta-analysis published in 2013 by Nguyen et al., fibromyalgia and irritable bowel syndrome were significantly identified as comorbidities present in patients with history of vulvodynia.99 Nguyen RH, Veasley C, Smolenski D. Latent class analysis of comorbidity patterns among women with generalized and localized vulvodynia: preliminary findings. J Pain Res. 2013;6:303-9. This relationship was not found for DM, for not being sought, but, theoretically, there might be a relationship considering that both are chronic medical conditions difficult to treat, and the adjectives chosen to describe vulvar pain (excruciating, burning, tingling) refer to a neuropathic cause.1010 Kalra B, Kalra S, Bajaj S. Vulvodynia: an unrecognized diabetic neuropathic syndrome. Indian J Endocrinol Metab. 2013;17:787-9. Either by a direct or indirect mechanism, for example, the greater predisposition to recurrent vaginal/urinary infections reported by this patient, DM seems to be a cause of vulvodynia.33 Pacik PT. Vaginismus: review of current concepts and treatment using botox injections, bupivacaine injections, and progressive dilation with the patient under anesthesia. Aesth Plast Surg. 2011;35:1160-4.,88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8.,1010 Kalra B, Kalra S, Bajaj S. Vulvodynia: an unrecognized diabetic neuropathic syndrome. Indian J Endocrinol Metab. 2013;17:787-9.
In the presence of one or more of the aforementioned predisposing factors, women may experience painful sensations. Subsequently, the fear of the painful sensation is fixed in sexual intercourse and develops an involuntary “flight or fight” reaction whenever there is a possibility of penetration.88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8. Furthermore, increased muscle tension secondary to persistent fear of pain, associated with the inability to relax, may be involved in the development of small areas of muscle contracture, the TP.1111 Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65:653-61.
The clinician should keep in mind that penetration not only includes the form that characterizes a sexual intercourse (penis × vagina).88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8. Indeed, according to the updated Diagnostic and Statistical Manual of Mental Disorders (DSM-5), any form of penetration, either using fingers, tampons, vaginal specula or extenders, can be particularly difficult.22 Pacik PT. Vaginismus: another ignored problem. Sex Culture. 2014;18:737-8.,33 Pacik PT. Vaginismus: review of current concepts and treatment using botox injections, bupivacaine injections, and progressive dilation with the patient under anesthesia. Aesth Plast Surg. 2011;35:1160-4.,1212 Araújo AC, Neto FL. A nova classificação americana para os transtornos mentais - o DSM-5. Rev Bras Ter Comp Cogn. 2014;XVI:67-82. This demanded adjustments in the patient assessment mode, at least in the initial phase of monitoring, all in order to foster a relationship of trust necessary for the progress of treatment.
The controlled studies published up to the present day are no consensus regarding the superiority of any technique for vaginismus treatment.11 Melnik T, Hawton K, McGuire H, et al. Interventions for vaginismus. Cochrane Database Syst Rev. 2012;12:CD001760.,1313 Pereira VM, Arias-Carrión O, Machado S, et al. Sex therapy for female sexual dysfunction. Int Arch Med. 2013;6:37.,1414 Harish T, Muliyala K, Murthy P. Successful management of vaginismus: an eclectic approach. Indian J Psychiatry. 2011;53:154-5. According to a review published by Cochrane, systematic desensitization—which may include relaxation techniques and use of progressively larger dilators—seems not to be more effective than cognitive therapy or pharmacological interventions.11 Melnik T, Hawton K, McGuire H, et al. Interventions for vaginismus. Cochrane Database Syst Rev. 2012;12:CD001760. These data, however, are obtained from heterogeneous studies with moderate to high risk of bias and a small number of patients and, therefore, should be carefully extrapolated into clinical practice.11 Melnik T, Hawton K, McGuire H, et al. Interventions for vaginismus. Cochrane Database Syst Rev. 2012;12:CD001760. Regardless of these limitations, the international literature is consistent in asserting that a vaginismus approach is more likely to be successful with an interdisciplinary approach.1313 Pereira VM, Arias-Carrión O, Machado S, et al. Sex therapy for female sexual dysfunction. Int Arch Med. 2013;6:37.,1414 Harish T, Muliyala K, Murthy P. Successful management of vaginismus: an eclectic approach. Indian J Psychiatry. 2011;53:154-5. Classically, the main treatment steps involves reflection and identification of the causes of the problem, relaxation therapy, and progressive deconditioning of involuntary muscle spasm.55 Cahana A, Van Zundert J, Macrea L, et al. Pulsed radiofrequency: current clinical and biological literature available. Pain Med. 2006;7:411-23. In our patient, the psychology and hypnotherapy consultations helped in achieving the first two goals, while TP infiltration associated with PRF and gradual use of dilators the key behind the desensitization process.
According to our survey conducted in PubMed, the use TP infiltration and PRF of pudendal nerve has never been previously described as part of multimodal therapeutic strategy for vaginismus, which reinforces the importance of this report.
TP are in the origin of myofascial syndromes and defined as limited areas of hyperirritability, with firm consistency, inside the striated muscles, tendons or fascia.1111 Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65:653-61. Although more often described in the scapular, lumbar and gluteal areas, they may be present in any anatomical region, particularly perineal, and develop secondary to acute trauma or repeated microtrauma,1111 Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65:653-61. particularly increased muscle tension.
Although the caused pain may be constant, it often arises only when there is muscle activity, such as during sex intercourse or when these tiny nodule formation are palpated, as in the gynecological examination.1111 Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65:653-61. The pain may be local or referred areas and is associated with a slight contraction,1010 Kalra B, Kalra S, Bajaj S. Vulvodynia: an unrecognized diabetic neuropathic syndrome. Indian J Endocrinol Metab. 2013;17:787-9. findings that were seen in our patient on the initial physical examination.
In this patient, the TP management decision depended not only on team experience, but also on its very nature. Indeed, although the long-term benefits of different therapeutic techniques are questionable, the chronicity of the patient's TP led the team to opt for infiltration with local anesthetic and steroid, a technique reported as providing a greater pain relief.1111 Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65:653-61. In fact, physiotherapy and manual therapy are more suitable for acute situations, patients with fear of needles, or TP in not easily accessible muscle bundles, not present in our the case.1111 Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65:653-61.
The radio frequency technique (RF) is a relatively new treatment modality based on administration of a high frequency alternating current in the vicinity of a nerve or ganglion structure.55 Cahana A, Van Zundert J, Macrea L, et al. Pulsed radiofrequency: current clinical and biological literature available. Pain Med. 2006;7:411-23.
6 Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.-77 Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008;12:37-41. Although its mechanism of action is not fully understood, it seems to be based on the principle of neuromodulation; that is, change in signal transduction and transmission along the pain pathways.66 Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.
This current can be administered in two major and distinct forms. In continuous RF, the current is administered to produce a thermal lesion on the target tissue, block the conduction of nociceptive signal and provide pain relief while nerve terminals do not regenerate.66 Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.,77 Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008;12:37-41. In pulsed RF, the current is intermittent, there is heat dissipation, and no development of neural coagulation The cellular morphology of the tissue is maintained. However, it causes molecular alterations in the expression of some transcription factors that culminate in change in pain signal transduction.66 Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.
RF techniques are currently used as a therapeutic tool in many chronic pain syndromes and, despite the paucity of randomized controlled trials, numerous reports of RF applied to peripheral nerve structures prove its effectiveness.44 Rhame EE, Levey KA, Gharibo CG. Successful treatment of refractory pudendal neuralgia with pulsed radiofrequency. Pain Physician. 2009;12:633-8.
5 Cahana A, Van Zundert J, Macrea L, et al. Pulsed radiofrequency: current clinical and biological literature available. Pain Med. 2006;7:411-23.-66 Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.
The pudendal nerve, consisting of the posterior branches of the sacred roots S2, S3 and S4, is responsible for motor innervation of the perineal muscles and sensory innervation of the lower portion of the vagina, vulva, and perineum.44 Rhame EE, Levey KA, Gharibo CG. Successful treatment of refractory pudendal neuralgia with pulsed radiofrequency. Pain Physician. 2009;12:633-8. Because these were the anatomic regions of our patient's complaints, the choice of this nerve for our therapeutic approach is warranted.
We opted for a pulsed technique given that it is more innocuous and not associated with risk of motor damage, complications reported with continuous RF. The occurrence of a motor damage would have devastating effects on the patient's already poor quality of life, as its clinical translation could include, among other findings, sphincter incontinence.66 Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.
Other advantages that influenced the choice of pulsed RF are related to the fact that it is a minimally invasive technique, safe and well tolerated, which can be repeated if there is recurrence of complaints.44 Rhame EE, Levey KA, Gharibo CG. Successful treatment of refractory pudendal neuralgia with pulsed radiofrequency. Pain Physician. 2009;12:633-8.
5 Cahana A, Van Zundert J, Macrea L, et al. Pulsed radiofrequency: current clinical and biological literature available. Pain Med. 2006;7:411-23.
6 Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.-77 Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008;12:37-41. This latter characteristic was used in this case. One potential drawback associated with this blockade is its technical difficulty, which may lead to a significant failure rate when performed by inexperienced teams.66 Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.
The pain complaints improvement reflected in other personal aspects of the patient's life. Thus, not only it was possible to advance in the pharmacological desensitization strategy and suspend the benzodiazepines taken by the patient, but an improvement of her self-esteem and self-assurance was also observed. Indeed, it is important that the medical team do not neglect the emotional charge entailed by this syndrome. Patients often present with a diminished image of themselves associated with feelings of shame.88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8.
It is also essential that the partners are included at all stages of treatment, as we try to do,88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8. either by the simple coexistence or by positive feedback mechanisms. As the patient's sexuality develops and grows, more safe, happy, and fulfilled will be the couple.88 Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8.
In summary, we can say that although this is a single report, TP infiltration and PRF of pudendal nerve seem to be a potential adjuvant therapeutic tool in the management of vaginismus. In our case, it provided to the patient a pain relief superior to any other experienced technique.
In order that the therapeutic effectiveness of these cases increases and minimizes the physical and psychological sequelae developed by these women in the medium and long term, it is essential also to improve the diagnostic ability of health professionals. Thus, as described by Pacik, it is necessary that during the years of training, pre- and post-graduation, professionals are able to recognize and treat this syndrome in the shortest possible time.22 Pacik PT. Vaginismus: another ignored problem. Sex Culture. 2014;18:737-8.
References
-
1Melnik T, Hawton K, McGuire H, et al. Interventions for vaginismus. Cochrane Database Syst Rev. 2012;12:CD001760.
-
2Pacik PT. Vaginismus: another ignored problem. Sex Culture. 2014;18:737-8.
-
3Pacik PT. Vaginismus: review of current concepts and treatment using botox injections, bupivacaine injections, and progressive dilation with the patient under anesthesia. Aesth Plast Surg. 2011;35:1160-4.
-
4Rhame EE, Levey KA, Gharibo CG. Successful treatment of refractory pudendal neuralgia with pulsed radiofrequency. Pain Physician. 2009;12:633-8.
-
5Cahana A, Van Zundert J, Macrea L, et al. Pulsed radiofrequency: current clinical and biological literature available. Pain Med. 2006;7:411-23.
-
6Rea W, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011;11:35-8.
-
7Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008;12:37-41.
-
8Silva MCA. Vaginismo/dispareunia. Rev Soc Bras Estud Sex Hum. 2009;20:143-8.
-
9Nguyen RH, Veasley C, Smolenski D. Latent class analysis of comorbidity patterns among women with generalized and localized vulvodynia: preliminary findings. J Pain Res. 2013;6:303-9.
-
10Kalra B, Kalra S, Bajaj S. Vulvodynia: an unrecognized diabetic neuropathic syndrome. Indian J Endocrinol Metab. 2013;17:787-9.
-
11Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65:653-61.
-
12Araújo AC, Neto FL. A nova classificação americana para os transtornos mentais - o DSM-5. Rev Bras Ter Comp Cogn. 2014;XVI:67-82.
-
13Pereira VM, Arias-Carrión O, Machado S, et al. Sex therapy for female sexual dysfunction. Int Arch Med. 2013;6:37.
-
14Harish T, Muliyala K, Murthy P. Successful management of vaginismus: an eclectic approach. Indian J Psychiatry. 2011;53:154-5.
Publication Dates
-
Publication in this collection
Nov-Dec 2017
History
-
Received
7 July 2014 -
Accepted
2 Oct 2014