Abstracts
OBJECTIVE:
the aim of this study was to assess the degree of exposure of the orthopedic surgical team to fluoroscopic ionizing radiation.
METHODS:
the ionizing radiation to which the orthopedic surgical team (R1, R2 and R3) was exposed was assayed using thermoluminescent dosimeters that were distributed in target anatomical regions (regions with and without protection using a lead apron). This was done during 45 hip osteosynthesis procedures to treat transtrochanteric fractures that were classified as 31-A2.1 (AO).
RESULTS:
the radioactive dose received by R3 was 6.33 mSv, R2 4.51 mSv and R3 1.99 mSv (p = 0.33). The thyroid region received 0.86 mSv of radiation, the thoracic region 1.24 mSv and the gonadal region 2.15 mSv (p = 0.25). There was no record of radiation at the dosimeters located below the biosafety protectors or on the team members' backs.
CONCLUSIONS:
the members of the surgical team who were located closest to the fluoroscope received greater radiation doses than those located further away. The anatomical regions located below the waistline were the ones that received most ionizing radiation. These results emphasize the importance of using biosafety devices, since these are effective in preventing radiation from reaching the vital organs of the medical team.
Ionizing radiation; Fluoroscopy; Orthopedic surgery
OBJETIVO:
avaliar o grau de exposição da equipe cirúrgica ortopédica à radiação ionizante fluoroscópica.
MÉTODOS:
foi dosada a radiação ionizante incidida sobre a equipe cirúrgica ortopédica (R1, R2 e R3) com dosímetros termoluminescentes, distribuídos em regiões anatômicas alvo, com e sem a proteção de avental de chumbo, durante 45 procedimentos de osteossíntese de quadril (DHS), por fraturas transtrocantéricas classificadas como 31-A2.1 (AO).
RESULTADOS:
a dose radioativa sobre o R3 foi de 6,33 mSv, de 4,51 mSv sobre o R2 e de 1,99 mSv sobre o R1 (p = 0,33). A região da tireoide recebeu 0,86 mSv de radiação, a região torácica 1,24 mSv e a região gonadal 2,15 mSv (p = 0,25). Não houve registro de radiação nas dosímetros localizados abaixo dos protetores de biossegurança ou nas costas dos membros da equipe.
CONCLUSÕES:
os membros da equipe cirúrgica que ficaram mais próximos do fluoroscópio receberam maiores doses de radiação do que os que ficaram mais remotamente. As regiões anatômicas abaixo da linha cintura foram as que mais receberam radiação ionizante. Os resultados ressaltam a importância do uso de dispositivos de biossegurança, os quais são efetivos em impedir que a radiação atinja órgãos vitais dos integrantes da equipe médica.
Radiação ionizante; Fluoroscopia; Cirurgia ortopédica
Introduction
Fluoroscopy is an important tool used during orthopedic surgery, which provides surgeons with better assessment of the anatomical structures operated and the synthesis materials implanted. It also considerably diminishes the duration of the operation and morbidity among patients. Although there are many advantages of using fluoroscopy devices, there is potential danger not only to the surgeon but also to all members of the surgical team: increased exposure to ionizing radiation.11. Giachino AA, Cheng M. Irradiation of the surgeon during pinning of femoral fractures. J Bone Joint Surg Br. 1980;62(2):227-9. and 22. Mehlman CT, DiPasquale TG. Radiation exposure to the orthopaedic surgical team during fluoroscopy: "how far away is far enough?". J Orthop Trauma. 1997;11(6):392-8.
Despite all the biosafety equipment available to medical teams, such as lead aprons, protective collars for the thyroid and goggles with lead film, the cumulative deleterious effects of radioactivity cannot be neglected. Fluoroscopes emit doses of approximately 5 rads per minute33. Hanel DP, Robson DB. The image intensifier as an operating table. J Hand Surg Am. 1987;12(2):322-3. and minifluoroscopes can cause serious and irreversible damage to health.22. Mehlman CT, DiPasquale TG. Radiation exposure to the orthopaedic surgical team during fluoroscopy: "how far away is far enough?". J Orthop Trauma. 1997;11(6):392-8. , 33. Hanel DP, Robson DB. The image intensifier as an operating table. J Hand Surg Am. 1987;12(2):322-3. , 44. Levin PE, Schoen Jr RW, Browner BD. Radiation exposure to the surgeon during closed interlocking intramedullary nailing. J Bone Joint Surg Am. 1987;69(5):761-6. , 55. Miller ME, Davis ML, MacClean CR, Davis JG, Smith BL, Humphries JR. Radiation exposure and associated risks to operating-room personnel during use of fluoroscopic guidance for selected orthopaedic surgical procedures. J Bone Joint Surg Am. 1983;65(1):1-4. and 66. Riley SA. Radiation exposure from fluoroscopy during orthopedic surgical procedures. Clin Orthop Relat Res. 1989;(248):257-60. It is known that doses of 1 rad, when applied systematically to a given region, can cause damage to deoxyribonucleic acid (DNA) and consequently cancer, at proportions of approximately 1:100,000.55. Miller ME, Davis ML, MacClean CR, Davis JG, Smith BL, Humphries JR. Radiation exposure and associated risks to operating-room personnel during use of fluoroscopic guidance for selected orthopaedic surgical procedures. J Bone Joint Surg Am. 1983;65(1):1-4. and 77. International Electrotechnical Commission 61267 (IEC 61267). Medical diagnostic X-ray equipment - radiation conditions for use in determination of characteristics. Geneva: International Electrotechnical Commission; 1994. It is important to emphasize that, in the human organism, ionizing radiation inhibits cell mitosis and irreparably breaks the DNA double chain. Nuclear structural modifications produce severe alterations to cells and increase the chances of potential genetic transmission of such errors. The hands, thyroid, eyes, abdomen and genitals are critical target areas that should receive proper care.
Ionizing radiation and its negative effects take on greater gravity when the indiscriminate use of fluoroscopes by medical residents within orthopedics is taken into consideration. They are subjected to high doses of radiation from the start of their training, mainly because of lack of operative practice and/or knowledge of its dire consequences.
Taking into consideration the large number of orthopedic surgical interventions performed with the aid of fluoroscopes and the severe sequelae relating to ionizing radiation, along with the scarcity of literature on this topic, particularly in the main Brazilian databases, the present study was proposed with the objective of evaluating the degree of exposure of orthopedic surgical teams to fluoroscopic ionizing radiation, with or without the associated use of bioprotection equipment.
Materials and methods
In conformity with resolution no. 1595/2000 of the Federal Medical Council, the authors declare that they did not have assistance of any kind for this study. Moreover, the researchers did not have any conflicts of interest in relation to the present study.
The study protocol was approved by the Ethics Committee for Research involving Human Beings, under no. 474/2012. All the patients or the adults legally responsible for them agreed to participate in the study and signed a free and informed consent statement after having been given detailed information about the content and shape of the study.
The sample size was determined at the start of the study, by means of specific statistical tests. The α risk (5%) and β risk (20%) were taken into consideration, along with the diversity of the variables, and the minimum number of surgical procedures was calculated as 45.
The ionizing radiation to which the orthopedic surgical team (R1, R2 and R3) was exposed during surgical procedures of hip osteosynthesis (Richard dynamic hip screw (DHS) or sliding screw and plate) due to transtrochanteric fractures classified as 31-A2.1 (AO), performed between February 2012 and August 2012, was assayed. The inclusion criteria were that the patients should have a minimum age of 18 years and have proximal femoral fractures of type 31-A2.1. All patients whose operations required intraoperative radiographs, those with fractures of tumor origin and those who refused to sign the consent form were excluded. Seven patients were excluded from this study: five who required intraoperative radiographs and two who, at the time of admission to our service, were unconscious and unaccompanied and thus unable to sign the consent statement. In this manner, 48 surgical procedures were included in this study.
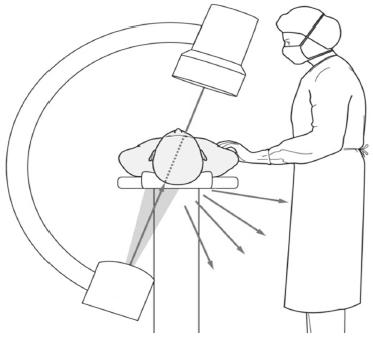
After arrival at the emergency service, the patients underwent the advanced trauma life support (ATLS) protocol and initial radiographs were produced, from which fractures in the proximal region of the femur were identified and classified. The patients were quickly thereafter taken to the surgical center to undergo osteosynthesis procedures, always performed by the same medical team (R1: technologist; R2: first surgeon; and R3: second surgeon) and using the same protocols and procedural times. All the surgical procedures were monitored in loco by the same preceptor, who was a specialist in hip surgery. The fluoroscopy device (Philips(r) BV Endura) ( Fig. 1), which was calibrated within the specific technical standards,88. International Organization for Standardization. ISO 4037-1:1996. X and gamma reference radiation for calibrating dosemeters and doserate meters for determining their response as a function of photon energy - Part 1: Radiation characteristics and production methods; 2013. Disponível em: http://www.iso.org/iso/catalogue detail.htm?csnumber=20781 (acessado em 20 de maio de 2013).
Disponível em: http://www.iso.org/iso/ca...
and 99. Hynes DE, Conere T, Mee MB, Cashman WF. Ionising radiation and the orthopaedic surgeon. J Bone Joint Surg Br. 1992;74(3):332-4. was always operated by the same professional and under the same technical parameters.
Protective lead aprons of thickness 5 mm (Konex(r)) were used by the surgical team as personal protection equipment. Throughout the time of the surgical procedure, the medical team used 21 thermoluminescent radiation dosimeters, distributed in different anatomical regions (Fig. 2 and Table 1), above and below the biosafety equipment, which had the function of measuring the ionizing radiation that was emitted by the fluoroscopy device and received by the orthopedic team.
Anterior and posterior locations of the dosimeters on the team members (above and below the lead protector).
The dosimeters were kept packed in a lead box, from which they were removed by the surgical team only just before they performed their asepsis and antisepsis procedures. After the end of the operative procedure, the surgical team immediately placed the dosimeters back into the same container. Three dosimeters (controls) were kept permanently inside lead wrappings, protected from any external radiation that could compromise the results.
Information such as the length of time for which the fluoroscope was used and the quantity of kV and mSv emitted by the device were provided automatically by the computer of the device and were subsequently tabulated in an electronic spreadsheet. At the end of the study, the dosimeters were sent to the Department of Nuclear Physics of the Physics Institute, University of São Paulo, which analyzed the individual doses of radiation received by each dosimeter, without knowing the original anatomical location (blinding process).
Statistical methodology
The variables of duration of the surgery, individual dose of radiation and location where received, for each of the members of the surgical team, were analyzed by means of parametric and nonparametric descriptive statistical tests, in a fully randomized model, using the SigmaStat(r) software, version 3.5 (Systat Software Inc., 2006), and the Minitab(r) software, version 15 (Minitab Inc., 2007). For all the calculations, a significance level of 5% was used (p < 0.05).
The means, standard deviations, medians, frequencies, percentages and 95% confidence intervals (95% CI) were calculated (α = 5%).
Results
The total time for which the fluoroscope was used was 2 h and 55 min, and the mean length of use was 3 min and 53 s (±1 min 22 s) (minimum: 1 min 44 s; maximum: 6 min 45 s; 95% CI: 3 min 29 s to 4 min 18 s).
The effective radiation dose received by R3 was 6.33 mSv, by R2 4.51 mSv and by R1 1.99 mSv (p = 0.33) ( Fig. 3). There were no statistical differences in total individual dose received between R3 and R2 (p = 0.58), R2 and R1 (p = 0.32) or R3 and R1 (p = 0.13).
In relation to the anatomical regions, the thyroid region received a mean radiation dose of 0.86 mSv (±0.3), the thoracic region 1.24 mSv (±0.8) and the gonadal region 2.15 mSv (±1.2) (p = 0.25) ( Fig. 4).
The individual dose of radiation received by R3 in the thyroid region was 1.24 mSv, by R2 0.81 mSv and by R1 0.55 mSv (p = 0.87) ( Fig. 5). There were no statistical differences in the doses received in the thyroid region between R3 and R2 (p = 0.76), R2 and R1 (p = 0.82) or R3 and R1 (p = 0.6).
The individual dose of radiation received by R3 in the thoracic region was 2.14 mSv, by R2 0.9 mSv and by R1 0.70 mSv (p = 0.61) ( Fig. 6). There were no statistical differences in the doses received in the thoracic region between R3 and R2 (p = 0.47), R2 and R1 (p = 0.87) or R3 and R1 (p = 0.4).
The individual dose of radiation received by R3 in the gonadal region was 2.94 mSv, by R2 2.8 mSv and by R1 0.73 mSv (p = 0.5) ( Fig. 7). There were no statistical differences in the doses received in the gonadal region between R3 and R2 (p = 0.95), R2 and R1 (p = 0.27) or R3 and R1 (p = 0.24).
The radiation levels detected in the control dosimeters, which were placed below the biosafety protectors (lead aprons) and on the backs of the team members, were less than 0.1 mSv. They were therefore considered to be zero.
Discussion
Studies conducted in the United States by the Department of Radiological Health and the Department of Health, Education and Wellbeing have indicated that the use of medical equipment that emits X-rays is the biggest source of exposure of the population to ionizing radiation of non-natural origin.1010. Kwong LM, Johanson PH, Zinar DM, Lenihan MR, Herman MW. Shielding of the patient's gonads during intramedullary interlocking femoral nailing. J Bone Joint Surg Am. 1990;72(10):1523-6. , 1111. Giordano BD, Ryder S, Baumhauer JF, DiGiovanni BF. Exposure to direct and scatter radiation with use of mini-c-arm fluoroscopy. J Bone Joint Surg Am. 2007;89(5):948-52. and 1212. Franciscatto PC [dissertação] Caracterização das qualidades de radiação X segundo as recomendações da norma IEC 61267 no Laboratório de Calibração do Ipem São Paulo. São Paulo: Universidade de São Paulo; 2009. In Brazil, the National Nuclear Energy Commission (CNEN) has recommended that the effective dose for individuals who are occupationally exposed to radiation should not exceed the mean limit of 20 mSv per year.1313. Giordano BD, Baumhauer JF, Morgan TL, Rechtine GR. Patient and surgeon radiation exposure: comparison of standard and mini-C-arm fluoroscopy. J Bone Joint Surg Am. 2009;91(2):297-304. The results from the present study demonstrate that, over a period of only six months, the residents in a medical residency program within orthopedics and traumatology received, on average, a quarter of the maximum permitted annual dose while only performing medium-complexity hip surgery, monitored by a specialist within the field. It can therefore be hypothesized that, if all the surgical procedures performed by these residents during their training were taken into consideration, the annual limit for the dose would certainly be exceeded.
Like other authors,1414. Mahaisavariya B, Songcharoen P, Riansuwan K. Radiation scattering to the primary surgeon during closed locked femoral nailing. J Med Assoc Thai. 2005;88(2):252-5. , 1515. Tremains MR, Georgiadis GM, Dennis MJ. Radiation exposure with use of the inverted-c-arm technique in upper-extremity surgery. J Bone Joint Surg Am. 2001;83-A(5):674-8. and 1616. Quimby EH, Shafiro G, Stickley EE. Radiation protection for medical and allied health personnel: recommendations of the National Council on Radiation Protection and Measurements. Bethesda (MD): National Council on Radiation Protection and Measurements (US) Council's Scientific Committee 49 on Radiation Protection Guidance for Paramedical Personnel; 1976 [NCRP. Report, 48]. we found that fluoroscopes generate large doses of ionizing radiation that affects the lower abdominal area, particularly the gonads (Fig. 4 and Fig. 7). Reflected radiation, also known as scattered radiation, which is disseminated after it encounters the object of study, is one of the main agents responsible for increasing the incidence of radiation in these regions (Fig. 8). Reflected radiation also explains why the position of the fluoroscope should not be inverted when its radiation emission source is placed above the object of study.
The results also showed that, although there were no significant differences between R3, R2 and R1, there was a strong tendency toward diminished radioactive impact on the surgical team members, as their distance from the fluoroscope increased. In fact, several authors have recommended that the team should remain at a safe distance from the device, of at least one meter.1111. Giordano BD, Ryder S, Baumhauer JF, DiGiovanni BF. Exposure to direct and scatter radiation with use of mini-c-arm fluoroscopy. J Bone Joint Surg Am. 2007;89(5):948-52. , 1212. Franciscatto PC [dissertação] Caracterização das qualidades de radiação X segundo as recomendações da norma IEC 61267 no Laboratório de Calibração do Ipem São Paulo. São Paulo: Universidade de São Paulo; 2009. , 1313. Giordano BD, Baumhauer JF, Morgan TL, Rechtine GR. Patient and surgeon radiation exposure: comparison of standard and mini-C-arm fluoroscopy. J Bone Joint Surg Am. 2009;91(2):297-304. , 1414. Mahaisavariya B, Songcharoen P, Riansuwan K. Radiation scattering to the primary surgeon during closed locked femoral nailing. J Med Assoc Thai. 2005;88(2):252-5. and 1515. Tremains MR, Georgiadis GM, Dennis MJ. Radiation exposure with use of the inverted-c-arm technique in upper-extremity surgery. J Bone Joint Surg Am. 2001;83-A(5):674-8. It is also important to note that use of personal protection equipment (lead aprons, goggles, etc.) is essential for professionals who come into contact with this type of radiation.16 16. Quimby EH, Shafiro G, Stickley EE. Radiation protection for medical and allied health personnel: recommendations of the National Council on Radiation Protection and Measurements. Bethesda (MD): National Council on Radiation Protection and Measurements (US) Council's Scientific Committee 49 on Radiation Protection Guidance for Paramedical Personnel; 1976 [NCRP. Report, 48]. and 1717. Theocharopoulos N, Perisinakis K, Damilakis J, Papadokostakis G, Hadjipavlou A, Gourtsoyiannis N. Occupational exposure from common fluoroscopic projections used in orthopaedic surgery. J Bone Joint Surg Am. 2003;85-A(9):1698-703. In the present study, the dosimeters placed below the lead apron remained without registering any radiation, which proves the effectiveness of this protection for preserving the medical team. However, it needs to be emphasized that although the protection equipment is effective, the unprotected regions of the body, particularly the upper limbs, remain at risk of neoplasia development.
Orthopedic teams, whether composed of residents or trained orthopedic surgeons, should use fluoroscopes cautiously during their operative procedures. The time for which the devices are used should be kept as short as possible, the team members should remain at a distance from the ionizing source and, obviously, adequate protective equipment should be used. These are effective measures for preventing serious health problems among the team members.
Conclusions
Under the conditions of the present study, the members of the surgical team who remained closest to the fluoroscope (R3 and R2) received higher doses of radiation, particularly in anatomical regions below the waistline. The biosafety equipment (lead apron) was effective in preventing radiation from reaching the vital organs of the medical team members.
REFERENCES
-
1Giachino AA, Cheng M. Irradiation of the surgeon during pinning of femoral fractures. J Bone Joint Surg Br. 1980;62(2):227-9.
-
2Mehlman CT, DiPasquale TG. Radiation exposure to the orthopaedic surgical team during fluoroscopy: "how far away is far enough?". J Orthop Trauma. 1997;11(6):392-8.
-
3Hanel DP, Robson DB. The image intensifier as an operating table. J Hand Surg Am. 1987;12(2):322-3.
-
4Levin PE, Schoen Jr RW, Browner BD. Radiation exposure to the surgeon during closed interlocking intramedullary nailing. J Bone Joint Surg Am. 1987;69(5):761-6.
-
5Miller ME, Davis ML, MacClean CR, Davis JG, Smith BL, Humphries JR. Radiation exposure and associated risks to operating-room personnel during use of fluoroscopic guidance for selected orthopaedic surgical procedures. J Bone Joint Surg Am. 1983;65(1):1-4.
-
6Riley SA. Radiation exposure from fluoroscopy during orthopedic surgical procedures. Clin Orthop Relat Res. 1989;(248):257-60.
-
7International Electrotechnical Commission 61267 (IEC 61267). Medical diagnostic X-ray equipment - radiation conditions for use in determination of characteristics. Geneva: International Electrotechnical Commission; 1994.
-
8International Organization for Standardization. ISO 4037-1:1996. X and gamma reference radiation for calibrating dosemeters and doserate meters for determining their response as a function of photon energy - Part 1: Radiation characteristics and production methods; 2013. Disponível em: http://www.iso.org/iso/catalogue detail.htm?csnumber=20781 (acessado em 20 de maio de 2013).
» Disponível em: http://www.iso.org/iso/catalogue detail.htm?csnumber=20781 -
9Hynes DE, Conere T, Mee MB, Cashman WF. Ionising radiation and the orthopaedic surgeon. J Bone Joint Surg Br. 1992;74(3):332-4.
-
10Kwong LM, Johanson PH, Zinar DM, Lenihan MR, Herman MW. Shielding of the patient's gonads during intramedullary interlocking femoral nailing. J Bone Joint Surg Am. 1990;72(10):1523-6.
-
11Giordano BD, Ryder S, Baumhauer JF, DiGiovanni BF. Exposure to direct and scatter radiation with use of mini-c-arm fluoroscopy. J Bone Joint Surg Am. 2007;89(5):948-52.
-
12Franciscatto PC [dissertação] Caracterização das qualidades de radiação X segundo as recomendações da norma IEC 61267 no Laboratório de Calibração do Ipem São Paulo. São Paulo: Universidade de São Paulo; 2009.
-
13Giordano BD, Baumhauer JF, Morgan TL, Rechtine GR. Patient and surgeon radiation exposure: comparison of standard and mini-C-arm fluoroscopy. J Bone Joint Surg Am. 2009;91(2):297-304.
-
14Mahaisavariya B, Songcharoen P, Riansuwan K. Radiation scattering to the primary surgeon during closed locked femoral nailing. J Med Assoc Thai. 2005;88(2):252-5.
-
15Tremains MR, Georgiadis GM, Dennis MJ. Radiation exposure with use of the inverted-c-arm technique in upper-extremity surgery. J Bone Joint Surg Am. 2001;83-A(5):674-8.
-
16Quimby EH, Shafiro G, Stickley EE. Radiation protection for medical and allied health personnel: recommendations of the National Council on Radiation Protection and Measurements. Bethesda (MD): National Council on Radiation Protection and Measurements (US) Council's Scientific Committee 49 on Radiation Protection Guidance for Paramedical Personnel; 1976 [NCRP. Report, 48].
-
17Theocharopoulos N, Perisinakis K, Damilakis J, Papadokostakis G, Hadjipavlou A, Gourtsoyiannis N. Occupational exposure from common fluoroscopic projections used in orthopaedic surgery. J Bone Joint Surg Am. 2003;85-A(9):1698-703.
-
☆
Please cite this article as: Palácio EP, Ribeiro AA, Gavassi BM, Di Stasi GG, Galbiatti JA, Junior AD, et al. Exposição da equipe cirúrgica à radiação ionizante durante procedimentos cirúrgicos ortopédicos. Rev Bras Ortop. 2014;49:227-232.
-
☆☆
Work performed in the Department of Orthopedics and Traumatology, Faculdade de Medicina de Marília (FAMEMA), Marília, SP, Brazil.
Publication Dates
-
Publication in this collection
May-June 2014
History
-
Received
16 Aug 2013 -
Accepted
23 Aug 2013