Abstract
Objective This was a retrospective observational study in patients submitted to intramedullary nail fixation after established or impeding pathological humerus-shaft tumoral fracture in the context of disseminated tumoral disease along 22 years of experience at the same institution.
Methods
Sample with 82 patients and 86 humeral fixations with unreamed rigid interlocking static intramedullary nail by the antegrade or retrograde approaches.
Results
The most prevalent primary tumors were breast carcinoma (30.49%), multiple myeloma (24.39%), lung adenocarcinoma (8.54%), and renal cell carcinoma (6.10%). The average surgical time was 90.16 ± 42.98 minutes (40-135 minutes). All of the patients reported improvement in arm pain and the mean Musculoskeletal Tumor Society (MSTS) score rose from 26% in the preoperative period to 72.6% in the evaluation performed in patients still alive 3 months after the surgery. The overall survival was 69.50% 3 months after the surgery, 56.10% at 6 months, 26.70% at 1 year, and 11.90% at 2 years. No death was related to the surgery or its complications. There were only 4 surgery-related complications, 1 intraoperative and 3 late, corresponding to a 4.65% complication risk.
Conclusion
Closed unreamed static interlocking intramedullary nailing (both in the antegrade or retrograde approaches) of the humerus is a fast, safe, effective, and low morbidity procedure to treat pathological fractures of the humerus shaft, assuring a stable arm fixation and consequently improving function and quality of life in these patients during their short life expectation.
Keywords:
humeral fractures; intramedullary fracture fixation/ instrumentation; intramedullary fracture fixation/ methods; spontaneous fractures/surgery; neoplasm metastasis
Resumo
Objetivo
Estudo retrospectivo observacional em pacientes submetidos à fixação com haste intramedular de fratura patológica tumoral consumada ou iminente da diáfise do úmero em contexto de doença tumoral disseminada ao longo de 22 anos na mesma instituição.
Métodos
Amostra com 82 pacientes e 86 fixações do úmero com haste intramedular rígida bloqueada estática não fresada anterógrada ou retrógrada.
Resultados
Os tumores primários mais prevalentes foram carcinoma da mama (30,49%), mieloma múltiplo (24,39%), adenocarcinoma do pulmão (8,54%) e carcinoma das células renais (6,10%). O tempo médio de intervenção cirúrgica para fixação com haste foi 90,16 ± 42,98 minutos (40-135). Todos os pacientes referiram melhoria das queixas álgicas no nível do braço e velicou-semelhoria do scoreMSTSmédio de 26% no pré-operatório para 72,6% na avaliação efetuada nos pacientes ainda vivos aos três meses de pós-operatório. A taxa de sobrevivência aos três meses após a cirurgia foi de 69,50%, 56,10% aos seis meses, 26,70% em um ano e 11,90% em dois anos. Nenhuma dasmortes decorreu da cirurgia ou de complicações dela. Apenas se registaramquatro complicações relacionadas com a cirurgia, uma intraoperatória e três tardias, corresponderam a risco de complicações de 4,65%.
Conclusão
O uso de haste intramedular não fresada estática bloqueada (anterógrado ou retrógrado) no úmero é um método rápido, seguro, eficaz e com baixa morbilidade no tratamento das fraturas patológicas da diáfise umeral, garante fixação estável do braço e consequentemente melhora a funcionalidade e a qualidade de vida desses pacientes durante a sua curta expectativa de vida.
Palavras-chave:
fraturas do húmero; fixação intramedular de fraturas/ instrumentação; fixação intramedular de fraturas/métodos; fraturas espontâneas/ cirurgia; metástase neoplásica
Introduction
The frequency of bone tumor conditions, especially of bone metastatic disease, increased markedly in recent years, and long bones are frequent sites of this type of lesion. The humerus is the second bone most affected by metastatic disease in the appendicular skeleton (ranging from 16 to 20% of the cases), followed by the femur.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 22 Ofluoglu O, Erol B, Ozgen Z, Yildiz M. Minimally invasive treatment of pathological fractures of the humeral shaft. Int Orthop2009;33(03):707-712 33 Dijkstra S, Stapert J, Boxma H,Wiggers T. Treatment of pathological fractures of the humeral shaft due to bone metastases: a comparison of intramedullary locking nail and plate osteosynthesis with adjunctive bone cement. Eur J Surg Oncol 1996;22(06):621-626 Metastatic humeral lesions are mostly lytic, and are associated with bone fragility and increased risk of fracture; however, only 8 to 10% of these lesions evolve to an established or impending fracture. Pathological humeral fractures account for 16 to 39% of all pathological fractures in long bones.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 44 Sarahrudi K,Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma 2009;66(03):789-794 55 Laitinen M, Nieminen J, Pakarinen TK. Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 2011;131(04):503-508 66 Gebhart M, Dequanter D, Vandeweyer E. Metastatic involvement of the humerus: a retrospective study of 51 cases. Acta Orthop Belg 2001;67(05):456-463 77 Redmond BJ, Biermann JS, Blasier RB. Interlocking intramedullary nailing of pathological fractures of the shaft of the humerus. J Bone Joint Surg Am 1996;78(06):891-896 As a general rule, the pathological humeral shaft fracture occurs late in the evolution of tumoral disease after minor or spontaneous trauma during activities, and it is an important negative prognostic and morbidity factor, causing pain, as well as loss of limb function and independent living; moreover, it often requires supportive care, including hygiene measures, which significantly reduces the quality of life of these patients in their supposed little time left (approximately 1 year after the appearance of bone metastases in disseminated tumor disease).11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 22 Ofluoglu O, Erol B, Ozgen Z, Yildiz M. Minimally invasive treatment of pathological fractures of the humeral shaft. Int Orthop2009;33(03):707-712 44 Sarahrudi K,Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma 2009;66(03):789-794 55 Laitinen M, Nieminen J, Pakarinen TK. Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 2011;131(04):503-508 88 Piccioli A, Maccauro G, Rossi B, Scaramuzzo L, Frenos F, Capanna R. Surgical treatment of pathologic fractures of humerus. Injury 2010;41(11):1112-1116 99 Atesok K, Liebergall M, Sucher E, Temper M, Mosheiff R, Peyser A. Treatment of pathological humeral shaft fractures with unreamed humeral nail. Ann Surg Oncol 2007;14(04):1493-1498 1010 Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218 1111 Flemming JE, Beals RK. Pathologic fracture of the humerus. Clin Orthop Relat Res 1986;(203):258-260 1212 Bauer HC,Wedin R. Survival after surgery for spinal and extremity metastases. Prognostication in 241 patients. Acta Orthop Scand 1995;66(02):143-146 The conservative treatment option with immobilization of the pathological humeral fractures had poor results, with insufficient pain reduction and little function improvement, mainly due to the reduced consolidation potential of these lesions because of the biological and mechanical effects of the tumor.33 Dijkstra S, Stapert J, Boxma H,Wiggers T. Treatment of pathological fractures of the humeral shaft due to bone metastases: a comparison of intramedullary locking nail and plate osteosynthesis with adjunctive bone cement. Eur J Surg Oncol 1996;22(06):621-626 44 Sarahrudi K,Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma 2009;66(03):789-794 55 Laitinen M, Nieminen J, Pakarinen TK. Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 2011;131(04):503-508 66 Gebhart M, Dequanter D, Vandeweyer E. Metastatic involvement of the humerus: a retrospective study of 51 cases. Acta Orthop Belg 2001;67(05):456-463 88 Piccioli A, Maccauro G, Rossi B, Scaramuzzo L, Frenos F, Capanna R. Surgical treatment of pathologic fractures of humerus. Injury 2010;41(11):1112-1116 1010 Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218 1111 Flemming JE, Beals RK. Pathologic fracture of the humerus. Clin Orthop Relat Res 1986;(203):258-260 As such, osteosynthesis is the current gold standard treatment for diaphyseal humeral fractures in patients with disseminated tumor disease who do not present with contraindications to the procedure.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 33 Dijkstra S, Stapert J, Boxma H,Wiggers T. Treatment of pathological fractures of the humeral shaft due to bone metastases: a comparison of intramedullary locking nail and plate osteosynthesis with adjunctive bone cement. Eur J Surg Oncol 1996;22(06):621-626 1010 Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218 1111 Flemming JE, Beals RK. Pathologic fracture of the humerus. Clin Orthop Relat Res 1986;(203):258-260 1313 Bauze AJ, Clayer MT. Treatment of pathological fractures of the humerus with a locked intramedullary nail. J Orthop Surg (Hong Kong) 2003;11(01):34-37 1414 Spencer SJ, Holt G, Clarke JV, Mohammed A, Leach WJ, Roberts JL. Locked intramedullary nailing of symptomatic metastases in the humerus. J Bone Joint Surg Br 2010;92(01):142-145 1515 Hunt KJ, Gollogly S, Randall RL. Surgical fixation of pathologic fractures: an evaluation of evolving treatment methods. BullHosp Jt Dis 2006;63(3-4):77-82 1616 Bickels J, Dadia S, Lidar Z. Surgical management of metastatic bone disease. J Bone Joint Surg Am 2009;91(06):1503-1516 1717 Capanna R, Campanacci DA. The treatment of metastases in the appendicular skeleton. J Bone Joint Surg Br 2001;83(04):471-481 This treatment is essentially palliative and aims at the immediate effective stabilization of the fracture (since one cannot expect or wait for consolidation), pain relief, and recovery of limb mobility, seeking to restore functional independence and quality of life as early as possible, preferably without further surgical intervention. The reduced invasiveness and minimal tissue aggression of the surgical technique, as well as good results in immediate stabilization, pain relief and rapid functional recovery, as well as the reduced rate of surgery-related complications, made the closed intramedullary humeral nailing the best option in established or impending diaphyseal fractures.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 33 Dijkstra S, Stapert J, Boxma H,Wiggers T. Treatment of pathological fractures of the humeral shaft due to bone metastases: a comparison of intramedullary locking nail and plate osteosynthesis with adjunctive bone cement. Eur J Surg Oncol 1996;22(06):621-626 44 Sarahrudi K,Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma 2009;66(03):789-794 55 Laitinen M, Nieminen J, Pakarinen TK. Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 2011;131(04):503-508 66 Gebhart M, Dequanter D, Vandeweyer E. Metastatic involvement of the humerus: a retrospective study of 51 cases. Acta Orthop Belg 2001;67(05):456-463 77 Redmond BJ, Biermann JS, Blasier RB. Interlocking intramedullary nailing of pathological fractures of the shaft of the humerus. J Bone Joint Surg Am 1996;78(06):891-896 1010 Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218 1313 Bauze AJ, Clayer MT. Treatment of pathological fractures of the humerus with a locked intramedullary nail. J Orthop Surg (Hong Kong) 2003;11(01):34-37 1414 Spencer SJ, Holt G, Clarke JV, Mohammed A, Leach WJ, Roberts JL. Locked intramedullary nailing of symptomatic metastases in the humerus. J Bone Joint Surg Br 2010;92(01):142-145 1515 Hunt KJ, Gollogly S, Randall RL. Surgical fixation of pathologic fractures: an evaluation of evolving treatment methods. BullHosp Jt Dis 2006;63(3-4):77-82 Although not an innovative treatment, researches on this specific osteosynthesis method in the context of pathological humeral fractures and its results are limited to small samples. The present study aimed to analyze a series of patients with pathological humeral diaphyseal fractures treated with closed unreamed static interlocking intramedullary nailing and their clinical-functional and radiographic results, focusing on postfixation survival time and surgery-related complications.
Material and Methods
This was a retrospective observational study with 101 consecutive patients submitted to palliative humeral stabilization with an unreamed static interlocking intramedullary nail after the diagnosis of established or imminent pathological fracture (the latter defined by a Mirels1818 Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 1989;(249):256-264 score > 8) of the humerus diaphysis in the context of tumor metastasis over 22 years at the same institution. A total of 19 patients were excluded from the sample because of data insufficiency, and the final sample consisted of 82 patients. The evaluation included demographics, primary neoplasm location and type, regional diaphyseal distribution of the humeral tumor lesion, surgical intervention time, nailing approach, nail dimensions, time of hospitalization, complications, and postoperative survival time.
A clinical and functional assessment of the upper limb was performed based on the Musculoskeletal Tumor Society (MSTS) scoring system.1919 Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993;(286):241-246 In addition, a radiographic evaluation of the humerus was also performed; consolidation was defined by the disappearance of pathological fracture hypolucency and the presence of a bone callus. All of the nailing procedures were closed, performed with unreamed devices, and the locking nail was static and associated with three or four proximal and distal bicortical screws. All of the patients were evaluated in an orthopedic visit at 6 weeks, 3 months and 6 months after the surgery or until the date of death. In addition, all of the patients received or continued to receive antineoplastic treatment with radiotherapy and/or chemotherapy. Some patients, particularly those with hypervascular tumors, such as renal cell and thyroid carcinomas and multiple myeloma, underwent an angioembolization of the humeral tumor lesion prior to the nailing. The date of death of the patients, if the death certificate was not available, was considered as the date of the first missed visit or scheduled treatment without rescheduling or a new attendance. Although it was not possible to recover all data from all of the patients, the total of cases without this information was always < 20%. In these situations, missing data were replaced by average values of the remaining ones. In calculating the mean time of the surgical intervention, 8 patients (9.76%) were excluded, since their nailing procedure was performed at the same time as other surgical interventions. Data was statistically treated using IBM SPSS Statistics for Windows, Version 23.0 (IBM Corp., Armonk, NY, USA). Values are presented in absolute number (n) and percentages (%), which are preferred as a central trend measure to the mean, whereas standard deviation (SD) (minimum value–maximum value) is preferred as a measure of dispersion. Survival curves were calculated using the Kaplan-Meier method. All of the patients or their families signed the informed consent form and the present study was approved by our institution.
Results
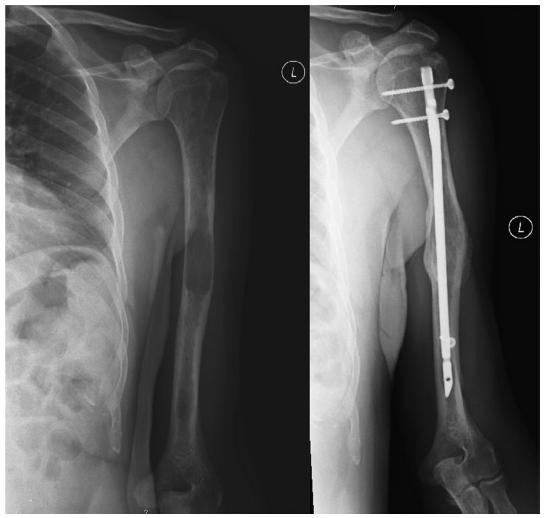
We present a sample of 82 patients submitted to 86 humeral fixations with intramedullary nail in the context of an established fracture (Fig. 1) or of an impending fracture (Fig. 2) due to a tumoral lesion. The mean age of the patients at the time of the diagnosis of the fracture was of 64.77 ± 13.78 years old (30–90 years old). The diagnosis in male patients occurred at an average age of 61.96 years old, approximately 4 years earlier than in female patients, in whom the average age at the time of diagnosis was of 66.23 years old. About 70% of the patients (n= 59) were in their 7th and 8th decades of life when the humeral pathological fracture was diagnosed. Most of the patients were female (69.51%; n= 57). Approximately 90% of the fractures were established, and only 8 impending fractures were treated. Most of the fractures occurred on the right side (48.84%; n= 42), and 4 patients had bilateral fractures, 3 of them simultaneously and 1 at different times, equivalent to 86 surgically treated fractures in 82 patients. The regional distribution of tumor lesions along the 3 thirds of the humeral shaft, in decreasing order (Fig. 3), was the following: medial diaphysis (44.19%; n= 38), proximal diaphysis (36.05%; n= 31), and distal diaphysis (19.77%, n= 17). A total of 12 patients (14.63%) had a previous history of pathological fractures in other anatomical sites, 8 in the dorsolumbar spine, and 4 in the femur. Primary tumors were located predominantly in the following anatomical areas, in descending order (Fig. 4): breast (30.49%; n= 25), blood (26.83%; n= 22), lung (10.98%; n= 9), kidney (8.54%; n= 7), prostate (4.88%; n= 4), thyroid (3.66%; n= 3), larynx (2.44%; n= 2) and brain (2.44%; n= 2). Here, multiple myeloma is considered a primary (hematopoietic) blood tumor. In two patients, the primary tumor remained unspecified. Tumor diseases that most frequently caused pathological fractures were metastatic bone disease and multiple myeloma. The most prevalent primary tumors were breast carcinoma (30.49%; n= 25), multiple myeloma (24.39%; n= 20), lung adenocarcinoma (8.54%; n= 7) and renal cells carcinoma (6.10%; n= 5). The most common primary tumor in women was breast carcinoma (present in 43.86% of the female patients), whereas, in men, the most frequent primary tumor was multiple myeloma (affecting 36% of the male patients).
Anatomical location of primary tumors. Note: Multiple myeloma was considered a primary blood (hematopoietic) tumor.
In most patients (86.59%), the humerus fracture occurred with a previously diagnosed underlying neoplasia. However, in 11 cases, the oncological diagnosis was only made after the pathological fracture, which was assumed as the 1st cancer manifestation and motivated an etiological screening. The mean time between the diagnosis of the primary neoplasm and the humeral pathological fracture was of 37.58 ± 2.40 months. The mean time of surgical nail fixation was of 90.16 ± 42.98 minutes (40–135 minutes), and the mean hospitalization time was of 8.23 ± 5.27 days (2–33 days). Most of the nailing procedures occurred via the antegrade approach (68.60%; n= 59), while the remainder were performed through the retrograde approach (31.40%; n= 27). The dimensions of the nails were customized in a case-per-case basis, considering the anatomical characteristics of the humerus from each patient. The most frequently used nails were 6.7 mm (66.28%; n= 57) and 7.5 mm (16.28; n= 14) in diameter and 250 mm in length (19.77%; n= 17, ranging from 205 to 360 mm). Three locking screws were most often used (86.05%; n= 74) and, in the remaining cases, the nail was locked with a total of 4 screws, with 2 proximal screws and 2 distal screws.
In clinical-functional terms, all of the patients reported improvement in arm pain, and the mean MSTS score increased from 26% to 72.6% in the evaluation performed in individuals still alive 3 months after the surgery. With the inclusion of only 57 patients with established fractures who survived for at least 3 months after the procedure, the radiographic consolidation rate in the operated humeri was of 77.19%.
The mean survival time after the surgery was of 309.29 ± 33.71 days, and the median time was of 196 days, with the highest number of deaths occurring during the 1st postoperative year. The survival rate at 90 days (3 months) after surgery was 69.50%, with 56.10% at 180 days (6 months), 26.70% at 365 days (1 year), and 11.90% at 730 days (2 years). There were no deaths in the immediate postoperative period, but 5 patients (6.10%) died during the 1st month after the surgery. Survival analysis of the sample is shown in Fig. 5 with a Kaplan-Meyer curve. No death was related with the surgery or with complications associated with it.
Kaplan-Meyer curve showing the accumulated survival rates, in days, of the sample after humeral nailing.
There were only 4 surgery-related complications, 1 in the early intraoperative period and 3 late complications, corresponding to a total complication risk of 4.65%. Complications included an iatrogenic fracture of the distal humerus in a retrograde procedure, requiring open reduction and fixation with plaque, screws and cerclage; a proximal nail migration due to loss of fixation of the proximal screws due to the growth of the tumor lesion, requiring the removal of the nails and of the screws; a pullout of one from two proximal locking screws, requiring its isolated extraction; and a subacromial impingement syndrome caused by the nail; these last three procedures were performed through the antegrade approach. When extracting the proximally migrating nail, it was found intraoperatively that the fracture was consolidated. There were no cases of neurovascular injury, embolism, infection, heterotopic ossification, refracture or other alterations. There was no significant difference in the MSTS functional score, postoperative survival time, and occurrence of complications according to age, gender, established or impending fracture and its distribution in the humeral shaft, primary tumor type, surgical approach, nail dimensions, and the number of locking bolts used.
Discussion
Although life expectancy increased in the last decades, most patients suffering from a pathological humeral fracture secondary to disseminated tumor disease have an estimated short survival time of ∼ 1 year, as demonstrated by the present study, in which the mean postoperative survival time was of 309.29 ± 33.71 days, with a median time of 196 days. As such, it is imperative that the chosen treatment focus on immediate pain control and early function restitution to minimize associated morbidity and provide a better quality of life in patients whose general condition is compromised.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 22 Ofluoglu O, Erol B, Ozgen Z, Yildiz M. Minimally invasive treatment of pathological fractures of the humeral shaft. Int Orthop2009;33(03):707-712 44 Sarahrudi K,Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma 2009;66(03):789-794 55 Laitinen M, Nieminen J, Pakarinen TK. Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 2011;131(04):503-508 66 Gebhart M, Dequanter D, Vandeweyer E. Metastatic involvement of the humerus: a retrospective study of 51 cases. Acta Orthop Belg 2001;67(05):456-463 88 Piccioli A, Maccauro G, Rossi B, Scaramuzzo L, Frenos F, Capanna R. Surgical treatment of pathologic fractures of humerus. Injury 2010;41(11):1112-1116 99 Atesok K, Liebergall M, Sucher E, Temper M, Mosheiff R, Peyser A. Treatment of pathological humeral shaft fractures with unreamed humeral nail. Ann Surg Oncol 2007;14(04):1493-1498 1010 Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218 1111 Flemming JE, Beals RK. Pathologic fracture of the humerus. Clin Orthop Relat Res 1986;(203):258-260 1212 Bauer HC,Wedin R. Survival after surgery for spinal and extremity metastases. Prognostication in 241 patients. Acta Orthop Scand 1995;66(02):143-146 2020 Hansen BH, Keller J, Laitinen M, Berg P, Skjeldal S, Trovik C, et al. The Scandinavian Sarcoma Group Skeletal Metastasis Register. Survival after surgery for bone metastases in the pelvis and extremities. Acta Orthop Scand Suppl 2004;75(311):11-15 2121 Harrington KD. Orthopedic surgical management of skeletal complications of malignancy. Cancer 1997;80(8, Suppl): 1614-1627 2222 Harrington KD, Sim FH, Enis JE, Johnston JO, Diok HM, Gristina AG. Methylmethacrylate as an adjunct in internal fixation of pathological fractures. Experiencewith three hundred and seventy-five cases. J Bone Joint Surg Am 1976;58(08):1047-1055 The current gold standard approach for pathological fractures of the humeral shaft is fixation with proximal and distal static interlocking rigid intramedullary nails.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 33 Dijkstra S, Stapert J, Boxma H,Wiggers T. Treatment of pathological fractures of the humeral shaft due to bone metastases: a comparison of intramedullary locking nail and plate osteosynthesis with adjunctive bone cement. Eur J Surg Oncol 1996;22(06):621-626 44 Sarahrudi K,Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma 2009;66(03):789-794 55 Laitinen M, Nieminen J, Pakarinen TK. Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 2011;131(04):503-508 66 Gebhart M, Dequanter D, Vandeweyer E. Metastatic involvement of the humerus: a retrospective study of 51 cases. Acta Orthop Belg 2001;67(05):456-463 77 Redmond BJ, Biermann JS, Blasier RB. Interlocking intramedullary nailing of pathological fractures of the shaft of the humerus. J Bone Joint Surg Am 1996;78(06):891-896 1010 Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218 1313 Bauze AJ, Clayer MT. Treatment of pathological fractures of the humerus with a locked intramedullary nail. J Orthop Surg (Hong Kong) 2003;11(01):34-37 1414 Spencer SJ, Holt G, Clarke JV, Mohammed A, Leach WJ, Roberts JL. Locked intramedullary nailing of symptomatic metastases in the humerus. J Bone Joint Surg Br 2010;92(01):142-145 1515 Hunt KJ, Gollogly S, Randall RL. Surgical fixation of pathologic fractures: an evaluation of evolving treatment methods. BullHosp Jt Dis 2006;63(3-4):77-82 As far as we know, the present study has the largest sample in terms of humeral diaphyseal fractures treatment with rigid intramedullary nails in the literature in the English language. As shown in the present series, whose results are confirmed by similar studies, static interlocking rigid nails are a safe and biomechanically effective implant, allowing a stable fixation against angulation, rotation, distraction and compression forces to stabilize the humerus in the context of diaphyseal pathological fractures; moreover, this is a relatively fast intervention with a short hospital stay that assures fixation of the arm and consequently provides pain control and function restauration, tolerating immediate limb mobilization and improving the quality of life. In addition, the nail allows a bypass to the diaphyseal tumor lesion and, as a result, the implant is stably fixed in the healthy proximal and distal bone, reducing the risk of fixation failure. It also ensures prophylactic protection of a long humeral segment against new fractures and, consequently, further surgery due to eventual disease progression or new metastasis. Since this is a closed reduction technique (with no opening of the fracture site), there is reduced blood loss, faster healing, and a lower risk of infection, as well as the possibility of adjuvant radiotherapy immediately after surgery with no significant risk of impaired healing, decreasing the risk of tumor progression and, consequently, reducing symptoms and/or fixation failures that require surgical revision.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 22 Ofluoglu O, Erol B, Ozgen Z, Yildiz M. Minimally invasive treatment of pathological fractures of the humeral shaft. Int Orthop2009;33(03):707-712 33 Dijkstra S, Stapert J, Boxma H,Wiggers T. Treatment of pathological fractures of the humeral shaft due to bone metastases: a comparison of intramedullary locking nail and plate osteosynthesis with adjunctive bone cement. Eur J Surg Oncol 1996;22(06):621-626 44 Sarahrudi K,Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma 2009;66(03):789-794 55 Laitinen M, Nieminen J, Pakarinen TK. Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 2011;131(04):503-508 66 Gebhart M, Dequanter D, Vandeweyer E. Metastatic involvement of the humerus: a retrospective study of 51 cases. Acta Orthop Belg 2001;67(05):456-463 77 Redmond BJ, Biermann JS, Blasier RB. Interlocking intramedullary nailing of pathological fractures of the shaft of the humerus. J Bone Joint Surg Am 1996;78(06):891-896 88 Piccioli A, Maccauro G, Rossi B, Scaramuzzo L, Frenos F, Capanna R. Surgical treatment of pathologic fractures of humerus. Injury 2010;41(11):1112-1116 99 Atesok K, Liebergall M, Sucher E, Temper M, Mosheiff R, Peyser A. Treatment of pathological humeral shaft fractures with unreamed humeral nail. Ann Surg Oncol 2007;14(04):1493-1498 1010 Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218 1313 Bauze AJ, Clayer MT. Treatment of pathological fractures of the humerus with a locked intramedullary nail. J Orthop Surg (Hong Kong) 2003;11(01):34-37 1414 Spencer SJ, Holt G, Clarke JV, Mohammed A, Leach WJ, Roberts JL. Locked intramedullary nailing of symptomatic metastases in the humerus. J Bone Joint Surg Br 2010;92(01):142-145 1515 Hunt KJ, Gollogly S, Randall RL. Surgical fixation of pathologic fractures: an evaluation of evolving treatment methods. BullHosp Jt Dis 2006;63(3-4):77-82 1616 Bickels J, Dadia S, Lidar Z. Surgical management of metastatic bone disease. J Bone Joint Surg Am 2009;91(06):1503-1516 1717 Capanna R, Campanacci DA. The treatment of metastases in the appendicular skeleton. J Bone Joint Surg Br 2001;83(04):471-481 2323 TownsendPW, Rosenthal HG, Smalley SR, Cozad SC, Hassanein RE. Impact of postoperative radiation therapy and other perioperative factors on outcome after orthopedic stabilization of impending or pathologic fractures due to metastatic disease. J Clin Oncol 1994;12(11):2345-2350 2424 Damron TA, Rock MG, Choudhury SN, Grabowski JJ, An KN. Biomechanical analysis of prophylactic fixation for middle third humeral impending pathologic fractures. Clin Orthop Relat Res 1999;(363):240-248 Although these patients are frequently more concerned with pain relief than with limb function, we consider that the functional improvement obtained from the mean MSTS score from 26% to 72.6% is quite satisfactory. Despite the previously mentioned reduced potential for the consolidation of pathological fractures, the stable fixation provided by the nail combined with the antineoplastic radiotherapy and chemotherapy probably allowed the consolidation indexes observed in the present sample (evaluated only in those who survived > 3 months after the surgery), which were deemed very satisfactory (77.19%). These rates were similar to the ones observed by Pretell et al11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 (80%) and by Atesok et al99 Atesok K, Liebergall M, Sucher E, Temper M, Mosheiff R, Peyser A. Treatment of pathological humeral shaft fractures with unreamed humeral nail. Ann Surg Oncol 2007;14(04):1493-1498 (88%), with an incidence of complications due to fixation failure limited to 1 case.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 22 Ofluoglu O, Erol B, Ozgen Z, Yildiz M. Minimally invasive treatment of pathological fractures of the humeral shaft. Int Orthop2009;33(03):707-712 99 Atesok K, Liebergall M, Sucher E, Temper M, Mosheiff R, Peyser A. Treatment of pathological humeral shaft fractures with unreamed humeral nail. Ann Surg Oncol 2007;14(04):1493-1498 1111 Flemming JE, Beals RK. Pathologic fracture of the humerus. Clin Orthop Relat Res 1986;(203):258-260
Our series had just four complications, and only one of them was intraoperative, consisting in an iatrogenic humeral fracture during the insertion of the nail; most of the sample obtained a stable humeral fixation throughout the remaining life time. Although some studies have reported important levels of complications with the nailing of pathological humeral fractures, in particular nerve lesions during the placement of locking screws, iatrogenic fractures during nail insertion, and failure in the fixation of the locking screws, most studies agree with our findings and also refer to a minimal incidence of surgical complications.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 22 Ofluoglu O, Erol B, Ozgen Z, Yildiz M. Minimally invasive treatment of pathological fractures of the humeral shaft. Int Orthop2009;33(03):707-712 44 Sarahrudi K,Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma 2009;66(03):789-794 55 Laitinen M, Nieminen J, Pakarinen TK. Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 2011;131(04):503-508 66 Gebhart M, Dequanter D, Vandeweyer E. Metastatic involvement of the humerus: a retrospective study of 51 cases. Acta Orthop Belg 2001;67(05):456-463 77 Redmond BJ, Biermann JS, Blasier RB. Interlocking intramedullary nailing of pathological fractures of the shaft of the humerus. J Bone Joint Surg Am 1996;78(06):891-896 88 Piccioli A, Maccauro G, Rossi B, Scaramuzzo L, Frenos F, Capanna R. Surgical treatment of pathologic fractures of humerus. Injury 2010;41(11):1112-1116 99 Atesok K, Liebergall M, Sucher E, Temper M, Mosheiff R, Peyser A. Treatment of pathological humeral shaft fractures with unreamed humeral nail. Ann Surg Oncol 2007;14(04):1493-1498 1010 Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218 1313 Bauze AJ, Clayer MT. Treatment of pathological fractures of the humerus with a locked intramedullary nail. J Orthop Surg (Hong Kong) 2003;11(01):34-37 1414 Spencer SJ, Holt G, Clarke JV, Mohammed A, Leach WJ, Roberts JL. Locked intramedullary nailing of symptomatic metastases in the humerus. J Bone Joint Surg Br 2010;92(01):142-145 2525 Noger M, Berli MC, Fasel JH, Hoffmeyer PJ. The risk of injury to neurovascular structures from distal locking screws of the Unreamed Humeral Nail (UHN): a cadaveric study. Injury 2007; 38(08):954-957 The antegrade approach has been more associated with shoulder pain and stiffness due to iatrogenic rotator cuff injury, whereas the retrograde approach is most associated with iatrogenic humeral fractures during the insertion of the nails.11 Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563 22 Ofluoglu O, Erol B, Ozgen Z, Yildiz M. Minimally invasive treatment of pathological fractures of the humeral shaft. Int Orthop2009;33(03):707-712 1010 Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218 1313 Bauze AJ, Clayer MT. Treatment of pathological fractures of the humerus with a locked intramedullary nail. J Orthop Surg (Hong Kong) 2003;11(01):34-37 Nevertheless, only one of each of these complications was observed during the present study; we attribute this to the nailing technique used and to the experience of the surgical team. Moreover, we believe that most operative complications reported in the literature may not occur if the surgical technique is the correct one. The reduced rate of shoulder problems due to the antegrade nail entry point in our sample could be explained by the single deltoid and cuff incisions with cold blade and its adequate closure to protect these structures during nail insertion, as well as the care not to displace the nail. However, we should also consider that the lower functional expectations and greater pain tolerance of terminal cancer patients probably have some impact on the reduced prevalence of shoulder pain after antegrade humeral nailing procedures.99 Atesok K, Liebergall M, Sucher E, Temper M, Mosheiff R, Peyser A. Treatment of pathological humeral shaft fractures with unreamed humeral nail. Ann Surg Oncol 2007;14(04):1493-1498 We have also considered that the adequate choice of the nail diameter was relevant to prevent intraoperative iatrogenic fractures and to increase the stability of osteosynthesis. It is important to fill most of the humeral medullary cavity to decrease the likelihood of fixation failures by instability. In turn, we also consider that the absence of pulmonary embolism in the sample warrants the use of unreamed nails in cancer patients with an increased risk of this complication.22 Ofluoglu O, Erol B, Ozgen Z, Yildiz M. Minimally invasive treatment of pathological fractures of the humeral shaft. Int Orthop2009;33(03):707-712 2626 Johnson JA, Berkshire A, Leighton RK, Gross M, Chess DG, Petrie D. Some basic biomechanical characteristics of medullary pressure generation during reaming of the femur. Injury 1995;26(07): 451-454 The limitations of the present study include its retrospective nature, the lack of data from some patients, and the loss of some individuals at follow-up due to the reduced life expectancy in metastatic cancer patients.
Conclusion
The use of unreamed rigid interlocking static intramedullary nail by the antegrade or retrograde approach is a treatment method that meets the requirements of a patient with short life expectancy and symptomatic pathological humeral fracture, since it is a fast, effective, safe, low morbidity technique that ensures stable and immediate bone fixation, resulting in pain relief, functional improvement, and increased quality of life.
References
-
1Pretell J, Rodriguez J, Blanco D, Zafra A, Resines C. Treatment of pathological humeral shaft fractures with intramedullary nailing. A retrospective study. Int Orthop 2010;34(04):559-563
-
2Ofluoglu O, Erol B, Ozgen Z, Yildiz M. Minimally invasive treatment of pathological fractures of the humeral shaft. Int Orthop2009;33(03):707-712
-
3Dijkstra S, Stapert J, Boxma H,Wiggers T. Treatment of pathological fractures of the humeral shaft due to bone metastases: a comparison of intramedullary locking nail and plate osteosynthesis with adjunctive bone cement. Eur J Surg Oncol 1996;22(06):621-626
-
4Sarahrudi K,Wolf H, Funovics P, Pajenda G, Hausmann JT, Vécsei V. Surgical treatment of pathological fractures of the shaft of the humerus. J Trauma 2009;66(03):789-794
-
5Laitinen M, Nieminen J, Pakarinen TK. Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 2011;131(04):503-508
-
6Gebhart M, Dequanter D, Vandeweyer E. Metastatic involvement of the humerus: a retrospective study of 51 cases. Acta Orthop Belg 2001;67(05):456-463
-
7Redmond BJ, Biermann JS, Blasier RB. Interlocking intramedullary nailing of pathological fractures of the shaft of the humerus. J Bone Joint Surg Am 1996;78(06):891-896
-
8Piccioli A, Maccauro G, Rossi B, Scaramuzzo L, Frenos F, Capanna R. Surgical treatment of pathologic fractures of humerus. Injury 2010;41(11):1112-1116
-
9Atesok K, Liebergall M, Sucher E, Temper M, Mosheiff R, Peyser A. Treatment of pathological humeral shaft fractures with unreamed humeral nail. Ann Surg Oncol 2007;14(04):1493-1498
-
10Frassica FJ, Frassica DA. Evaluation and treatment of metastases to the humerus. Clin Orthop Relat Res 2003(415, Suppl):S212-S218
-
11Flemming JE, Beals RK. Pathologic fracture of the humerus. Clin Orthop Relat Res 1986;(203):258-260
-
12Bauer HC,Wedin R. Survival after surgery for spinal and extremity metastases. Prognostication in 241 patients. Acta Orthop Scand 1995;66(02):143-146
-
13Bauze AJ, Clayer MT. Treatment of pathological fractures of the humerus with a locked intramedullary nail. J Orthop Surg (Hong Kong) 2003;11(01):34-37
-
14Spencer SJ, Holt G, Clarke JV, Mohammed A, Leach WJ, Roberts JL. Locked intramedullary nailing of symptomatic metastases in the humerus. J Bone Joint Surg Br 2010;92(01):142-145
-
15Hunt KJ, Gollogly S, Randall RL. Surgical fixation of pathologic fractures: an evaluation of evolving treatment methods. BullHosp Jt Dis 2006;63(3-4):77-82
-
16Bickels J, Dadia S, Lidar Z. Surgical management of metastatic bone disease. J Bone Joint Surg Am 2009;91(06):1503-1516
-
17Capanna R, Campanacci DA. The treatment of metastases in the appendicular skeleton. J Bone Joint Surg Br 2001;83(04):471-481
-
18Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 1989;(249):256-264
-
19Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993;(286):241-246
-
20Hansen BH, Keller J, Laitinen M, Berg P, Skjeldal S, Trovik C, et al. The Scandinavian Sarcoma Group Skeletal Metastasis Register. Survival after surgery for bone metastases in the pelvis and extremities. Acta Orthop Scand Suppl 2004;75(311):11-15
-
21Harrington KD. Orthopedic surgical management of skeletal complications of malignancy. Cancer 1997;80(8, Suppl): 1614-1627
-
22Harrington KD, Sim FH, Enis JE, Johnston JO, Diok HM, Gristina AG. Methylmethacrylate as an adjunct in internal fixation of pathological fractures. Experiencewith three hundred and seventy-five cases. J Bone Joint Surg Am 1976;58(08):1047-1055
-
23TownsendPW, Rosenthal HG, Smalley SR, Cozad SC, Hassanein RE. Impact of postoperative radiation therapy and other perioperative factors on outcome after orthopedic stabilization of impending or pathologic fractures due to metastatic disease. J Clin Oncol 1994;12(11):2345-2350
-
24Damron TA, Rock MG, Choudhury SN, Grabowski JJ, An KN. Biomechanical analysis of prophylactic fixation for middle third humeral impending pathologic fractures. Clin Orthop Relat Res 1999;(363):240-248
-
25Noger M, Berli MC, Fasel JH, Hoffmeyer PJ. The risk of injury to neurovascular structures from distal locking screws of the Unreamed Humeral Nail (UHN): a cadaveric study. Injury 2007; 38(08):954-957
-
26Johnson JA, Berkshire A, Leighton RK, Gross M, Chess DG, Petrie D. Some basic biomechanical characteristics of medullary pressure generation during reaming of the femur. Injury 1995;26(07): 451-454
-
*
Work developed at the Serviço de Ortopedia e Traumatologia, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal.
Publication Dates
-
Publication in this collection
03 June 2019 -
Date of issue
Mar-Apr 2019
History
-
Received
10 Aug 2017 -
Accepted
31 Oct 2017 -
Published
25 Mar 2019