ABSTRACT
Sepsis continues to be a leading public health burden in the United States and worldwide. With the increasing use of advanced laboratory technology, there is a renewed interest in the use of biomarkers in sepsis to aid in more precise and targeted decision-making. Natriuretic peptides have been increasingly recognized to play a role outside of heart failure. They are commonly elevated among critically ill patients in the setting of cardiopulmonary dysfunction and may play a role in identifying patients with sepsis and septic shock. There are limited data on the role of these biomarkers in the diagnosis, management, outcomes and prognosis of septic patients. This review seeks to describe the role of natriuretic peptides in fluid resuscitation, diagnosis of ventricular dysfunction and outcomes and the prognosis of patients with sepsis. B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP) have been noted to be associated with left ventricular systolic and diastolic and right ventricular dysfunction in patients with septic cardiomyopathy. BNP/NT-proBNP may predict fluid responsiveness, and trends of these peptides may play a role in fluid resuscitation. Despite suggestions of a correlation with mortality, the role of BNP in mortality outcomes and prognosis during sepsis needs further evaluation.
Keywords:
Sepsis; Shock, septic; Natriuretic peptides; Natriuretic peptide, brain; Ventricular dysfunction
RESUMO
A sepse persiste como importante sobrecarga à saúde pública nos Estados Unidos e em todo o mundo. Com o crescente uso de tecnologias laboratoriais, tem se renovado o interesse na utilização de biomarcadores na sepse, para auxiliar em um processo mais preciso e direcionado para tomadas de decisão. Os peptídeos natriuréticos vem sendo cada vez mais reconhecidos por seu papel que vai além da insuficiência cardíaca. Estes peptídeos estão comumente elevados em pacientes críticos que apresentam condições de disfunção cardiopulmonar e podem ter papel na identificação de pacientes com sepse e choque séptico. São poucos os dados disponíveis em relação ao papel destes biomarcadores no diagnóstico, no controle, nos desfechos e no prognóstico de pacientes sépticos. Esta revisão procura descrever o papel dos peptídeos natriuréticos na ressuscitação volêmica, no diagnóstico de disfunção ventricular, nos desfechos e no prognóstico de pacientes com sepse. Tem sido observado que o peptídeo natriurético tipo B (BNP) e o fragmento N-terminal do peptídeo natriurético tipo B (NT-proBNP) se associam com disfunção ventricular sistólica e diastólica, tanto esquerda quanto direita, em pacientes com cardiomiopatia séptica. O BNP e o NT-proBNP podem predizer a responsividade a volume, e as tendências de medidas seriadas destes peptídeos podem ser importantes na ressuscitação volêmica. A despeito da sugestão de correlação com mortalidade, o papel do BNP nos desfechos de mortalidade e prognóstico, durante a sepse, ainda necessita melhor avaliação.
Descritores:
Choque; Choque séptico; Peptídeos natriuréticos; Peptídeo natriurético encefálico; Disfunção ventricular
INTRODUCTION
Sepsis remains a major cause of morbidity and mortality, both within the intensive care unit (ICU) and outside, accounting for nearly US$17 billion of annual healthcare expenditures.(11 Cuthbertson BH, Elders A, Hall S, Taylor J, MacLennan G, Mackirdy F, Mackenzie SJ; Scottish Critical Care Trials Group; Scottish Intensive Care Society Audit Group. Mortality and quality of life in the five years after severe sepsis. Crit Care. 2013;17(2):R70.
2 Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis. Crit Care Med. 2014;42(3):625-31.
3 Jentzer JC, Vallabhajosyula S, Khanna AK, Chawla LS, Busse LW, Kashani KB. Management of refractory vasodilatory shock. Chest. 2018;154(2):416-26.
4 Kotecha AA, Vallabhajosyula S, Apala DR, Frazee E, Iyer VN. Clinical outcomes of weight-based norepinephrine dosing in underweight and morbidly obese patients: a propensity-matched analysis. J Intensive Care Med. 2018:885066618768180.-55 Vallabhajosyula S, Jentzer JC, Kotecha AA, Murphree DH Jr, Barreto EF, Khanna AK, et al. Development and performance of a novel vasopressor-driven mortality prediction model in septic shock. Ann Intensive Care. 2018;8(1):112.) Despite significant improvements in the diagnosis and management of sepsis, it remains a challenging clinical entity due to its varied etiology and presentation.(33 Jentzer JC, Vallabhajosyula S, Khanna AK, Chawla LS, Busse LW, Kashani KB. Management of refractory vasodilatory shock. Chest. 2018;154(2):416-26.,66 Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-10.
7 Vincent JL. The clinical challenge of sepsis identification and monitoring. PLoS Med. 2016;13(5):e1002022.
8 Haddad TM, Vallabhajosyula S, Nawaz MS, Vivekanandan R. Fatal Pneumocystis jirovecii pneumonia in a HIV-negative adult. BMJ Case Rep. 2015;2015. pii: bcr2015210117.
9 Mahfood Haddad T, Vallabhajosyula S, Sundaragiri PR, Vivekanandan R. Mycotic pseudoaneurysm by vancomycin-intermediate Staphylococcus aureus: a rare cause of persistent bacteraemia. BMJ Case Rep. 2015;2015. pii: bcr2014209003.
10 Rose SR, Vallabhajosyula S, Velez MG, Fedorko DP, VanRaden MJ, Gea-Banacloche JC, et al. The utility of bronchoalveolar lavage beta-D-glucan testing for the diagnosis of invasive fungal infections. J Infect. 2014;69(3):278-83.
11 Sundaragiri PR, Vallabhajosyula S, Haddad TM, Esterbrooks DJ. Tricuspid and mitral endocarditis due to methicillin-resistant Staphylococcus aureus exhibiting vancomycin-creep phenomenon. BMJ Case Rep. 2015;2015. pii: bcr2015211974.
12 Vallabhajosyula S, Varma MD, Vallabhajosyula S, Vallabhajosyula S. Association of hyponatremia with in-hospital outcomes in infective endocarditis: A 5-year review from an Indian Intensive Care Unit. Indian J Crit Care Med. 2016;20(10):597-600.
13 Vallabhajosyula S, Varma MD, Vallabhajosyula S, Vallabhajosyula S. Right-sided infective endocarditis in an Indian intensive care unit. J Glob Infect Dis. 2016;8(3):124-5.-1414 Varma MD, Vengalil S, Vallabhajosyula S, Krishnakumar PC, Vidyasagar S. Leptospirosis and dengue fever: a predictive model for early differentiation based on clinical and biochemical parameters. Trop Doct. 2014;44(2):100-2.) With the development of sensitive laboratory technology, there is a renewed interest in the use of biomarkers for the targeted treatment of sepsis. To date, 178 biomarkers have been studied in septic patients in recent years, with C-reactive protein and procalcitonin being the most commonly used tests in current clinical practice.(77 Vincent JL. The clinical challenge of sepsis identification and monitoring. PLoS Med. 2016;13(5):e1002022.) Although these biomarkers can aid in diagnosis, determination of the severity and prognosis of sepsis, their specificity, and their prognostic implications have been described with wide variability.(1515 Tang BM, Eslick GD, Craig JC, McLean AS. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systematic review and meta-analysis. Lancet Infect Dis. 2007;7(3):210-7.,1616 Wu CC, Lan HM, Han ST, Chaou CH, Yeh CF, Liu SH, et al. Comparison of diagnostic accuracy in sepsis between presepsin, procalcitonin, and C-reactive protein: a systematic review and meta-analysis. Ann Intensive Care. 2017;7(1):91.) Cardiac biomarkers have been evaluated previously in these patients to aid in prognosis and in the diagnosis of myocardial injury and/or dysfunction.(1717 Landesberg G, Jaffe AS, Gilon D, Levin PD, Goodman S, Abu-Baih A, et al. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit Care Med. 2014;42(4):790-800.
18 Vallabhajosyula S, Sakhuja A, Geske JB, Kumar M, Poterucha JT, Kashyap R, et al. Role of admission troponin-T and serial troponin-T testing in predicting outcomes in severe sepsis and septic shock. J Am Heart Assoc. 2017;6(9). pii: e005930.-1919 Vallabhajosyula S, Sakhuja A, Geske JB, Kumar M, Kashyap R, Kashani K, et al. Clinical profile and outcomes of acute cardiorenal syndrome type-5 in sepsis: An eight-year cohort study. PLoS One. 2018;13(1):e0190965.) Cardiac troponin-T and I have shown a strong correlation between sepsis severity and outcomes and prognosis.(1818 Vallabhajosyula S, Sakhuja A, Geske JB, Kumar M, Poterucha JT, Kashyap R, et al. Role of admission troponin-T and serial troponin-T testing in predicting outcomes in severe sepsis and septic shock. J Am Heart Assoc. 2017;6(9). pii: e005930.,2020 Bessière F, Khenifer S, Dubourg J, Durieu I, Lega JC. Prognostic value of troponins in sepsis: a meta-analysis. Intensive Care Med. 2013;39(7):1181-9.) However, the role of commonly used natriuretic peptides, namely, B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP), have not been thoroughly studied.(2121 Machado Rde L, David CM, Luiz RR, Amitrano Dde A, Salomão Cde S, Oliveira GM. Related prognostic factors in elderly patients with severe sepsis and septic shock. Rev Bras Ter Intensiva. 2009;21(1):9-17.)
This study sought to evaluate the existing literature on the role of BNP/NT-proBNP in the diagnosis and management of sepsis with or without concomitant septic cardiomyopathy. Prior reviews on this topic have focused on outcomes and prognosis in sepsis;(2222 Wang F, Wu Y, Tang L, Zhu W, Chen F, Xu T, et al. Brain natriuretic peptide for prediction of mortality in patients with sepsis: a systematic review and meta-analysis. Crit Care. 2012;16(3):R74.) however, there are limited summations of its correlation with ventricular function. Using a comprehensive literature search strategy, this review identified all pertinent studies evaluating the role of BNP and NT-proBNP in patients with sepsis. Specifically, adult human studies were reviewed and organized into a narrative style to describe the role of natriuretic peptides in septic cardiomyopathy, fluid resuscitation and outcomes and the prognosis of septic patients.
BIOCHEMISTRY AND PATHOPHYSIOLOGY
B-type natriuretic peptide was first isolated from the porcine brain but was subsequently noted to be secreted by human ventricular myocardial cells.(2323 Sudoh T, Kangawa K, Minamino N, Matsuo H. A new natriuretic peptide in porcine brain. Nature. 1988;332(6159):78-81.) The half-lives of BNP and NT-proBNP in plasma are 22 and 120 minutes, respectively.(2424 Hall C. Essential biochemistry and physiology of (NT-pro)BNP. Eur J Heart Fail. 2004;6(3):257-60.) These natriuretic peptides are predominantly released in response to volume overload and myocyte stretching.(2525 Vanderheyden M, Bartunek J, Goethals M. Brain and other natriuretic peptides: molecular aspects. Eur J Heart Fail. 2004;6(3):261-8.) B-type natriuretic peptide elimination occurs through several pathways, including natriuretic peptide receptor-C that clears natriuretic peptides from the circulation through receptor-mediated internalization and degradation and less so by neutral endopeptidases through the liver, lung, and kidney in its active form, whereas NT-proBNP is exclusively excreted by the kidneys.(2626 Mukoyama M, Nakao K, Hosoda K, Suga S, Saito Y, Ogawa Y, et al. Brain natriuretic peptide as a novel cardiac hormone in humans. Evidence for an exquisite dual natriuretic peptide system, atrial natriuretic peptide and brain natriuretic peptide. J Clin Invest. 1991;87(4):1402-12.
27 Smith MW, Espiner EA, Yandle TG, Charles CJ, Richards AM. Delayed metabolism of human brain natriuretic peptide reflects resistance to neutral endopeptidase. J Endocrinol. 2000;167(2):239-46.
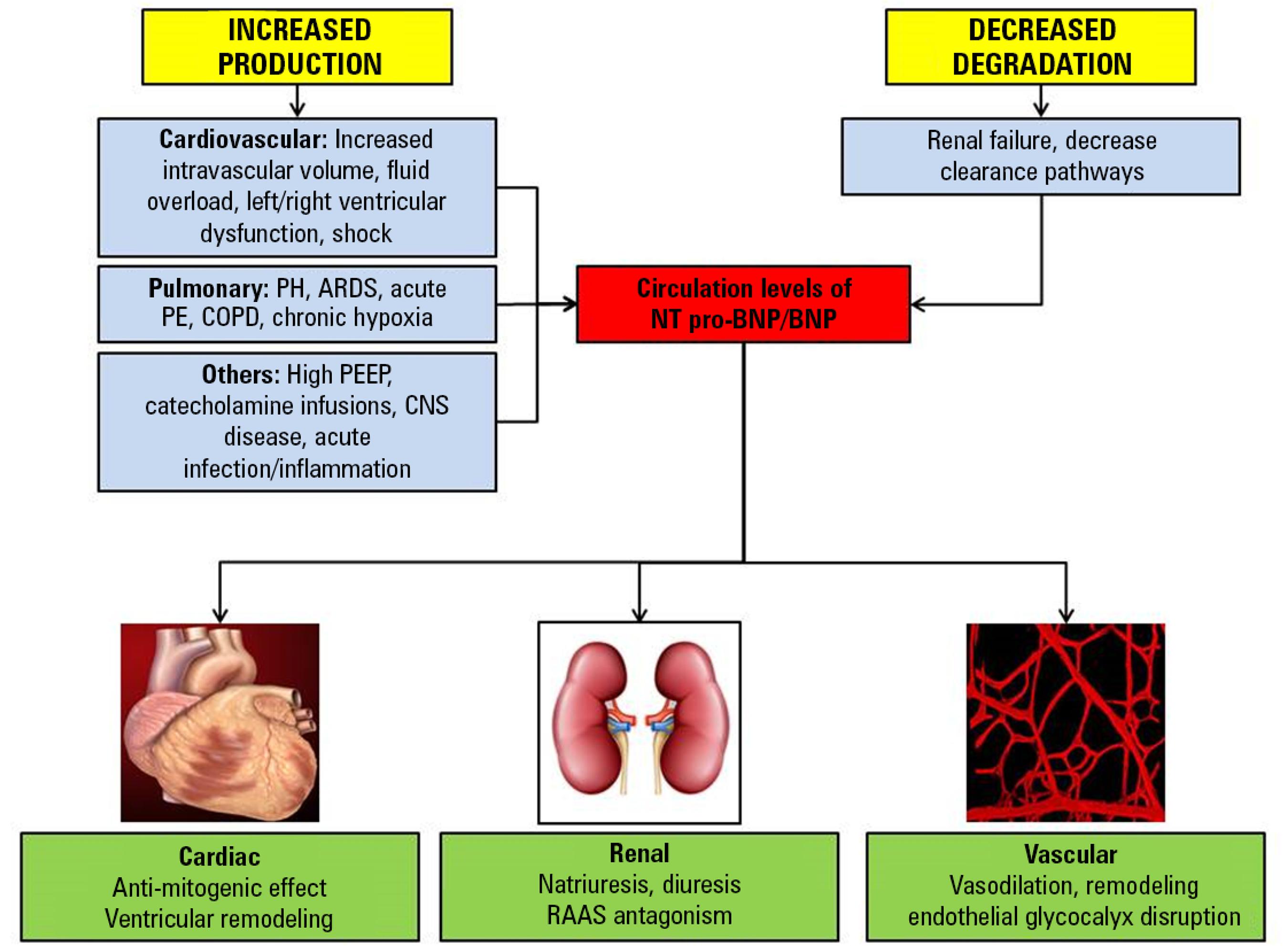
28 Valli N, Gobinet A, Bordenave L. Review of 10 years of the clinical use of brain natriuretic peptide in cardiology. J Lab Clin Med. 1999;134(5):437-44.-2929 Zakynthinos E, Kiropoulos T, Gourgoulianis K, Filippatos G. Diagnostic and prognostic impact of brain natriuretic peptide in cardiac and noncardiac diseases. Heart Lung. 2008;37(4):275-85.) The release of BNP and NT-pro BNP in sepsis is stimulated by multiple factors (Figure 1). Myocytic stretch with ventricular dysfunction and proinflammatory molecules, such as lipopolysaccharides, interleukin-1, C-reactive protein, and cardiotrophin-1, promote BNP gene expression and release in patients with sepsis.(3030 Charpentier J, Luyt CE, Fulla Y, Vinsonneau C, Cariou A, Grabar S, et al. Brain natriuretic peptide: A marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004;32(3):660-5.
31 Post F, Weilemann LS, Messow CM, Sinning C, Münzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36(11):3030-7.-3232 Shor R, Rozenman Y, Bolshinsky A, Harpaz D, Tilis Y, Matas Z, et al. BNP in septic patients without systolic myocardial dysfunction. Eur J Intern Med. 2006;17(8):536-40.) Additionally, concomitant renal failure and processes of care such as catecholamine infusions and volume resuscitation lead to an elevation of BNP/NT-proBNP levels.(3333 McLean AS, Huang SJ. Brain not processing: is finding a role for BNP in sepsis like fitting a square peg into a round hole? Crit Care. 2014;18(4):161.,3434 Kotecha A, Vallabhajosyula S, Coville HH, Kashani K. Cardiorenal syndrome in sepsis: A narrative review. J Crit Care.43:122-7.) In addition to the primary septic process, often pulmonary pathology and interventions such as acute respiratory distress syndrome, chronic obstructive pulmonary disease and mechanical ventilation influence the BNP levels in this population.(3333 McLean AS, Huang SJ. Brain not processing: is finding a role for BNP in sepsis like fitting a square peg into a round hole? Crit Care. 2014;18(4):161.,3535 Vallabhajosyula S, Haddad TM, Sundaragiri PR, Ahmed AA, Nawaz MS, Rayes HA, et al. Role of B-type natriuretic peptide in predicting in-hospital outcomes in acute exacerbation of chronic obstructive pulmonary disease with preserved left ventricular function: a 5-year retrospective analysis. J Intensive Care Med. 2018;33(11):635-44.) Along with increased production/secretion of BNP, sepsis alters the clearance of BNP due to renal failure and other mechanisms.(3434 Kotecha A, Vallabhajosyula S, Coville HH, Kashani K. Cardiorenal syndrome in sepsis: A narrative review. J Crit Care.43:122-7.,3636 Pirracchio R, Deye N, Lukaszewicz AC, Mebazaa A, Cholley B, Matéo J, et al. Impaired plasma B-type natriuretic peptide clearance in human septic shock. Crit Care Med. 2008;36(9):2542-6.)
Mechanisms of release and action of natriuretic peptides.
PH - pulmonary hypertension; ARDS - acute respiratory distress syndrome; PE - pulmonary embolism; COPD - chronic obstructive pulmonary disease; BNP - B-type natriuretic peptide; NT pro-BNP - N-terminal pro-B-type natriuretic peptide; PEEP - positive end-expiratory pressure; CNS - central nervous system; RAAS - renin-angiotensin-aldosterone system.
NATRIURETIC PEPTIDES AND SEPTIC CARDIOMYOPATHY
Left ventricular systolic dysfunction
Left ventricular (LV) dysfunction is noted variably in 20 - 50% of septic patients, which is likely due to differences in the timing of performing echocardiography and the severity of sepsis among these patients.(3737 Vallabhajosyula S, Jentzer JC, Geske JB, Kumar M, Sakhuja A, Singhal A, et al. New-onset heart failure and mortality in hospital survivors of sepsis-related left ventricular dysfunction. Shock. 2018;49(2):144-9.
38 Sevilla Berrios RA, O'Horo JC, Velagapudi V, Pulido JN. Correlation of left ventricular systolic dysfunction determined by low ejection fraction and 30-day mortality in patients with severe sepsis and septic shock: a systematic review and meta-analysis. J Crit Care. 2014;29(4):495-9.-3939 Vallabhajosyula S, Deshmukh AJ, Kashani K, Prasad A, Sakhuja A. Tako-tsubo cardiomyopathy in severe sepsis: Nationwide trends, predictors, and outcomes. J Am Heart Assoc. 2018;7(18):e009160.) Multiple studies have shown a reduced left ventricular ejection fraction (LVEF) in sepsis, although a recent meta-analysis did not demonstrate any correlation between LV systolic function and LV dimensions with mortality in this population.(4040 Huang SJ, Nalos M, McLean AS. Is early ventricular dysfunction or dilatation associated with lower mortality rate in adult severe sepsis and septic shock? A meta-analysis. Crit Care. 2013;17(3):R96.) Formal echocardiography requires expert acquisition and interpretation that limits its generalizability and so a biomarker to detect early LV dysfunction could, therefore, be valuable for evaluating cardiac dysfunction in sepsis.
Charpentier et al. first correlated BNP and LV dysfunction in septic patients, showing that patients with LV fractional area change < 50% and a higher end systolic LV diameter on day two had higher BNP levels than patients with a normal LV fractional area change.(3030 Charpentier J, Luyt CE, Fulla Y, Vinsonneau C, Cariou A, Grabar S, et al. Brain natriuretic peptide: A marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004;32(3):660-5.) Klouche et al. corroborated this finding at days three and four after admission, and patients with LV systolic dysfunction had significantly higher BNP values.(4141 Klouche K, Pommet S, Amigues L, Bargnoux AS, Dupuy AM, Machado S, et al. Plasma brain natriuretic peptide and troponin levels in severe sepsis and septic shock: relationships with systolic myocardial dysfunction and intensive care unit mortality. J Intensive Care Med. 2014;29(4):229-37.) In a cohort of cancer patients with sepsis, BNP on day two correlated with patients developing echocardiography-detected LV systolic dysfunction.(4242 Mokart D, Sannini A, Brun JP, Faucher M, Blaise D, Blache JL, et al. N-terminal pro-brain natriuretic peptide as an early prognostic factor in cancer patients developing septic shock. Crit Care. 2007;11(2):R37.) In contrast to these studies that evaluated single measurements, Post et al. assessed BNP trends, demonstrating an inverse correlation between BNP and LV systolic dysfunction in patients with septic shock.(3131 Post F, Weilemann LS, Messow CM, Sinning C, Münzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36(11):3030-7.) Despite these correlations, it is important to note that echocardiography derived LVEF in sepsis should be interpreted with caution since it is a function of preload, afterload, and myocardial contractility, all of which vary in septic patients.(4343 Repessè X, Charron C, Vieillard-Baron A. Evaluation of left ventricular systolic function revisited in septic shock. Crit Care. 2013;17(4):164.) Left ventricular stroke work index, a pulmonary artery catheter-derived parameter, may be a less load-dependent parameter of LV contractility and has been shown to be indicative of myocardial dysfunction in septic shock.(4444 Kumar A, Anel R, Bunnell E, Zanotti S, Habet K, Haery C, et al. Preload-independent mechanisms contribute to increased stroke volume following large volume saline infusion in normal volunteers: a prospective interventional study. Crit Care. 2004;8(3):R128-36.,4545 Vincent JL, Gris P, Coffernils M, Leon M, Pinsky M, Reuse C, et al. Myocardial depression characterizes the fatal course of septic shock. Surgery. 1992;111(6):660-7.) There are limited data in the current era due to decreased use of pulmonary artery catheters.(4646 Witthaut R, Busch C, Fraunberger P, Walli A, Seidel D, Pilz G, et al. Plasma atrial natriuretic peptide and brain natriuretic peptide are increased in septic shock: impact of interleukin-6 and sepsis-associated left ventricular dysfunction. Intensive Care Med. 2003;29(10):1696-702.,4747 Ueda S, Nishio K, Akai Y, Fukushima H, Ueyama T, Kawai Y, et al. Prognostic value of increased plasma levels of brain natriuretic peptide in patients with septic shock. Shock. 2006;26(2):134-9.)
Other authors have shown that BNP levels are elevated in severe sepsis and septic shock regardless of the presence or absence of LV dysfunction.(4848 McLean AS, Huang SJ, Hyams S, Poh G, Nalos M, Pandit R, et al. Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(4):1019-26.) Papanakolaou et al. demonstrated that LVEF was not an independent predictor of BNP elevation in sepsis patients; rather, the severity of the illness seemed to be the primary determinant of BNP elevation.(4949 Papanikolaou J, Makris D, Mpaka M, Palli E, Zygoulis P, Zakynthinos E. New insights into the mechanisms involved in B-type natriuretic peptide elevation and its prognostic value in septic patients. Crit Care. 2014;18(3):R94.) Several other authors also demonstrated elevated BNP levels in septic patients despite normal LV function.(3232 Shor R, Rozenman Y, Bolshinsky A, Harpaz D, Tilis Y, Matas Z, et al. BNP in septic patients without systolic myocardial dysfunction. Eur J Intern Med. 2006;17(8):536-40.,5050 Burjonroppa SC, Tong AT, Xiao LC, Johnson MM, Yusuf SW, Lenihan DJ. Cancer patients with markedly elevated B-type natriuretic peptide may not have volume overload. Am J Clin Oncol. 2007;30(3):287-93.)
In summary, BNP/NT-proBNP exhibits a strong correlation with LV function. However, the measurement of LV function in sepsis remains an ongoing debate,(5151 Vallabhajosyula S, Pruthi S, Shah S, Wiley BM, Mankad SV, Jentzer JC. Basic and advanced echocardiographic evaluation of myocardial dysfunction in sepsis and septic shock. Anaesth Intensive Care. 2018;46(1):13-24.,5252 Vallabhajosyula S, Rayes HA, Sakhuja A, Murad MH, Geske JB, Jentzer JC. Global longitudinal strain using speckle-tracking echocardiography as a mortality predictor in sepsis: A systematic review. J Intensive Care Med. 2019;34(2):87-93.) and thus the correlation ability of BNP is subject to variability. Use of advanced imaging modalities such as tissue Doppler imaging, global longitudinal strain, and speckle tracking echocardiography may be more useful to evaluate the role of myocardial stretching in these patients that results in BNP release.(3434 Kotecha A, Vallabhajosyula S, Coville HH, Kashani K. Cardiorenal syndrome in sepsis: A narrative review. J Crit Care.43:122-7.)
Left ventricular diastolic dysfunction
Left ventricular diastolic dysfunction is increasingly recognized in modern practice and is noted to have a 20 - 57% prevalence in septic patients.(5353 Sanfilippo F, Corredor C, Fletcher N, Landesberg G, Benedetto U, Foex P, et al. Diastolic dysfunction and mortality in septic patients: a systematic review and meta-analysis. Intensive Care Med. 2015;41(6):1004-13. Erratum in: Intensive Care Med. 2015;41(6):1178-9.) Diastolic dysfunction can potentially explain the etiology of troponin release in sepsis;(1717 Landesberg G, Jaffe AS, Gilon D, Levin PD, Goodman S, Abu-Baih A, et al. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit Care Med. 2014;42(4):790-800.) however, similar mechanistic studies about the role of BNP in sepsis are not readily available. Elevated filling pressures in LV diastolic dysfunction may induce BNP release, and the prior literature has demonstrated that natriuretic peptides are typically lower in patients with preserved LVEF.(5454 van Veldhuisen DJ, Linssen GC, Jaarsma T, van Gilst WH, Hoes AW, Tijssen JG, et al. B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction. J Am Coll Cardiol. 2013;61(14):1498-506.) Patients with LV diastolic dysfunction often have concomitant respiratory failure, necessitating the use of mechanical ventilation, which results in higher levels of BNP release.(1717 Landesberg G, Jaffe AS, Gilon D, Levin PD, Goodman S, Abu-Baih A, et al. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit Care Med. 2014;42(4):790-800.,3535 Vallabhajosyula S, Haddad TM, Sundaragiri PR, Ahmed AA, Nawaz MS, Rayes HA, et al. Role of B-type natriuretic peptide in predicting in-hospital outcomes in acute exacerbation of chronic obstructive pulmonary disease with preserved left ventricular function: a 5-year retrospective analysis. J Intensive Care Med. 2018;33(11):635-44.,5555 Vallabhajosyula S, Kumar M, Pandompatam G, Sakhuja A, Kashyap R, Kashani K, et al. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7(1):94.,5656 Vallabhajosyula S, Gillespie SM, Barbara DW, Anavekar NS, Pulido JN. Impact of new-onset left ventricular dysfunction on outcomes in mechanically ventilated patients with severe sepsis and septic shock. J Intensive Care Med. 2018;33(12):680-6.) Several studies have evaluated the correlation of BNP with diastolic dysfunction in septic patients, although they included small numbers of patients, and diastolic function was mainly reported as an ancillary outcome.(5757 Sturgess DJ, Pascoe RL, Scalia G, Venkatesh B. A comparison of transcutaneous Doppler corrected flow time, B-type natriuretic peptide and central venous pressure as predictors of fluid responsiveness in septic shock: a preliminary evaluation. Anaesth Intensive Care. 2010;38(2):336-41.,5858 Lin X, Jiang X, Cheng Q, Liu C, Zhang X. [Changes of left ventricular systolic and diastolic function and the diagnostic value of B-type natriuretic peptide in patients with sepsis]. Zhonghua Yi Xue Za Zhi. 2014;94(11):816-20. Chinese.) Sturgess et al. demonstrated diastolic dysfunction to be an independent predictor of BNP concentration in septic shock patients, and Lin et al. showed that BNP correlated with the severity of LV diastolic dysfunction in septic patients.(5757 Sturgess DJ, Pascoe RL, Scalia G, Venkatesh B. A comparison of transcutaneous Doppler corrected flow time, B-type natriuretic peptide and central venous pressure as predictors of fluid responsiveness in septic shock: a preliminary evaluation. Anaesth Intensive Care. 2010;38(2):336-41.,5858 Lin X, Jiang X, Cheng Q, Liu C, Zhang X. [Changes of left ventricular systolic and diastolic function and the diagnostic value of B-type natriuretic peptide in patients with sepsis]. Zhonghua Yi Xue Za Zhi. 2014;94(11):816-20. Chinese.) In contrast, in a study evaluating BNP trends in severe sepsis and septic shock patients, Mclean et al. revealed no apparent correlation between BNP and tissue Doppler velocities of diastolic function (p = 0.15).(4848 McLean AS, Huang SJ, Hyams S, Poh G, Nalos M, Pandit R, et al. Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(4):1019-26.) Based on the currently available data, it appears that BNP/NT-proBNP levels correlate with diastolic dysfunction. Further study of the BNP trends in diastolic dysfunction during sepsis is needed to evaluate its potential role in this increasingly recognized patient population since diastolic dysfunction has demonstrated strong correlations with clinical outcomes.(1717 Landesberg G, Jaffe AS, Gilon D, Levin PD, Goodman S, Abu-Baih A, et al. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit Care Med. 2014;42(4):790-800.,5353 Sanfilippo F, Corredor C, Fletcher N, Landesberg G, Benedetto U, Foex P, et al. Diastolic dysfunction and mortality in septic patients: a systematic review and meta-analysis. Intensive Care Med. 2015;41(6):1004-13. Erratum in: Intensive Care Med. 2015;41(6):1178-9.)
Right ventricular dysfunction
Right ventricular (RV) dysfunction in sepsis and septic shock occurs in 30 - 60% of the population and is associated with worse short and long-term outcomes including mortality.(1717 Landesberg G, Jaffe AS, Gilon D, Levin PD, Goodman S, Abu-Baih A, et al. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit Care Med. 2014;42(4):790-800.,5555 Vallabhajosyula S, Kumar M, Pandompatam G, Sakhuja A, Kashyap R, Kashani K, et al. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7(1):94.) In sepsis, in addition to direct myocardial toxicity, increased nitric oxide, acute respiratory distress syndrome, hypoxemic pulmonary vasoconstriction and pulmonary hypertension contribute to worsening RV function.(5555 Vallabhajosyula S, Kumar M, Pandompatam G, Sakhuja A, Kashyap R, Kashani K, et al. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7(1):94.,5959 Chandra NG, Vallabhajosyula S, Shastry BA, Vallabhajosyula S, Vallabhajosyula S, Saravu K. Use of corticosteroids in acute respiratory distress syndrome: Perspective from an Indian intensive care unit. Med J Armed Forces India. 2017;73(2):118-22.
60 Vallabhajosyula S, Geske JB, Kumar M, Kashyap R, Kashani K, Jentzer JC. Doppler-defined pulmonary hypertension in sepsis and septic shock. J Crit Care. 2019;50:201-6.-6161 Vallabhajosyula S, Trivedi V, Gajic O. Ventilation in acute respiratory distress syndrome: importance of low-tidal volume. Ann Transl Med. 2016;4(24):496.) BNP and NT-proBNP have been described in other disease states that can lead to acute RV failure, including acute respiratory distress syndrome, pulmonary embolism, and chronic obstructive pulmonary disease.(3535 Vallabhajosyula S, Haddad TM, Sundaragiri PR, Ahmed AA, Nawaz MS, Rayes HA, et al. Role of B-type natriuretic peptide in predicting in-hospital outcomes in acute exacerbation of chronic obstructive pulmonary disease with preserved left ventricular function: a 5-year retrospective analysis. J Intensive Care Med. 2018;33(11):635-44.,6262 Mitaka C, Hirata Y, Nagura T, Tsunoda Y, Itoh M, Amaha K. Increased plasma concentrations of brain natriuretic peptide in patients with acute lung injury. J Crit Care. 1997;12(2):66-71.,6363 Enea I, Ceparano G, Mazzarella G, Di Sarno R, Cangiano G, Busino CA. [Biohumoral markers and right ventricular dysfunction in acute pulmonary embolism: the answer to thrombolytic therapy]. Ital Heart J Suppl. 2004;5(1):29-35. Italian.) However, the specific role of BNP and NT-proBNP in sepsis-related RV dysfunction remains to be clarified.(4242 Mokart D, Sannini A, Brun JP, Faucher M, Blaise D, Blache JL, et al. N-terminal pro-brain natriuretic peptide as an early prognostic factor in cancer patients developing septic shock. Crit Care. 2007;11(2):R37.,4848 McLean AS, Huang SJ, Hyams S, Poh G, Nalos M, Pandit R, et al. Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(4):1019-26.,4949 Papanikolaou J, Makris D, Mpaka M, Palli E, Zygoulis P, Zakynthinos E. New insights into the mechanisms involved in B-type natriuretic peptide elevation and its prognostic value in septic patients. Crit Care. 2014;18(3):R94.) McLean et al. demonstrated that BNP elevations in patients with severe sepsis and septic shock correlated with RV systolic performance more closely than with LVEF or LV end-diastolic diameter (r = 0.24; p = 0.02).(4848 McLean AS, Huang SJ, Hyams S, Poh G, Nalos M, Pandit R, et al. Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(4):1019-26.) Papanikolaou et al. demonstrated that both RVEF and LVEF were significantly correlated with serial BNP values, showing the likely interdependent nature of both chambers in this population.(4949 Papanikolaou J, Makris D, Mpaka M, Palli E, Zygoulis P, Zakynthinos E. New insights into the mechanisms involved in B-type natriuretic peptide elevation and its prognostic value in septic patients. Crit Care. 2014;18(3):R94.,5555 Vallabhajosyula S, Kumar M, Pandompatam G, Sakhuja A, Kashyap R, Kashani K, et al. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7(1):94.) B-type natriuretic peptide may play a role in the diagnosis and management of RV dysfunction in sepsis during the acute phase, analogous to high-sensitivity troponin.(1717 Landesberg G, Jaffe AS, Gilon D, Levin PD, Goodman S, Abu-Baih A, et al. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit Care Med. 2014;42(4):790-800.) Importantly, RV dysfunction has shown stronger correlations with clinical outcomes at 6 months and one year, leading us to speculate on the role of long-term cardiopulmonary interactions.(5555 Vallabhajosyula S, Kumar M, Pandompatam G, Sakhuja A, Kashyap R, Kashani K, et al. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7(1):94.,6464 Orde SR, Pulido JN, Masaki M, Gillespie S, Spoon JN, Kane GC, et al. Outcome prediction in sepsis: speckle tracking echocardiography based assessment of myocardial function. Crit Care. 2014;18(4):R149.) There might be a role for serial BNP trending analogous to chronic heart failure, which remains an exciting new avenue for clinical and translational research.(6565 Shah MR, Califf RM, Nohria A, Bhapkar M, Bowers M, Mancini DM, et al. The STARBRITE trial: a randomized, pilot study of B-type natriuretic peptide-guided therapy in patients with advanced heart failure. J Card Fail. 2011;17(8):613-21.) However, the contemporary data are limited and inadequate to evaluate the correlation between RV dysfunction and natriuretic peptides.
FLUID THERAPY AND NATRIURETIC PEPTIDES
Early appropriate fluid resuscitation leads to better outcomes in sepsis, and this often requires a delicate balance between under-resuscitation and volume overload.(6666 Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304-77.,6767 Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011;39(2):259-65.) Only approximately 50% of unstable septic patients respond to a fluid challenge and identifying fluid responsive patients remains a significant challenge for clinicians.(6868 Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med. 2013;41(7):1774-81.) Dynamic measures such as respiratory variation of the inferior vena cava and changes in stroke volume after passive leg raising are more accurate in identifying patients who will increase their cardiac output in response to a fluid bolus.(6969 Pinsky MR. Heart lung interactions during mechanical ventilation. Curr Opin Crit Care. 2012;18(3):256-60.)
B-type natriuretic peptide and NT-proBNP have been investigated as markers of volume status and fluid responsiveness. In patients with heart failure, BNP has been shown to be a useful marker of volume status, preload, estimated LV filling pressure, pulmonary artery occlusion pressure, and end-diastolic volume.(7070 Maeda K, Tsutamoto T, Wada A, Hisanaga T, Kinoshita M. Plasma brain natriuretic peptide as a biochemical marker of high left ventricular end-diastolic pressure in patients with symptomatic left ventricular dysfunction. Am Heart J. 1998;135(5 Pt 1):825-32.
71 Dokainish H, Zoghbi WA, Lakkis NM, Al-Bakshy F, Dhir M, Quinones MA, et al. Optimal noninvasive assessment of left ventricular filling pressures: a comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation. 2004;109(20):2432-9.-7272 Kazanegra R, Cheng V, Garcia A, Krishnaswamy P, Gardetto N, Clopton P, et al. A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompensated heart failure: a pilot study. J Card Fail. 2001;7(1):21-9.) However, these data have not been reliably replicated in patients with undifferentiated shock or sepsis (Table 1).(4141 Klouche K, Pommet S, Amigues L, Bargnoux AS, Dupuy AM, Machado S, et al. Plasma brain natriuretic peptide and troponin levels in severe sepsis and septic shock: relationships with systolic myocardial dysfunction and intensive care unit mortality. J Intensive Care Med. 2014;29(4):229-37.,4646 Witthaut R, Busch C, Fraunberger P, Walli A, Seidel D, Pilz G, et al. Plasma atrial natriuretic peptide and brain natriuretic peptide are increased in septic shock: impact of interleukin-6 and sepsis-associated left ventricular dysfunction. Intensive Care Med. 2003;29(10):1696-702.,4747 Ueda S, Nishio K, Akai Y, Fukushima H, Ueyama T, Kawai Y, et al. Prognostic value of increased plasma levels of brain natriuretic peptide in patients with septic shock. Shock. 2006;26(2):134-9.,4949 Papanikolaou J, Makris D, Mpaka M, Palli E, Zygoulis P, Zakynthinos E. New insights into the mechanisms involved in B-type natriuretic peptide elevation and its prognostic value in septic patients. Crit Care. 2014;18(3):R94.,7373 Tung RH, Garcia C, Morss AM, Pino RM, Fifer MA, Thompson BT, et al. Utility of B-type natriuretic peptide for the evaluation of intensive care unit shock. Crit Care Med. 2004;32(8):1643-7.
74 Jefic D, Lee JW, Jefic D, Savoy-Moore RT, Rosman HS. Utility of B-type natriuretic peptide and N-terminal pro B-type natriuretic peptide in evaluation of respiratory failure in critically ill patients. Chest. 2005;128(1):288-95.
75 Forfia PR, Watkins SP, Rame JE, Stewart KJ, Shapiro EP. Relationship between B-type natriuretic peptides and pulmonary capillary wedge pressure in the intensive care unit. J Am Coll Cardiol. 2005;45(10):1667-71.
76 Turner KL, Moore LJ, Todd SR, Sucher JF, Jones SA, McKinley BA, et al. Identification of cardiac dysfunction in sepsis with B-typenatriuretic peptide. J Am Coll Surg. 2011;213(1):139-46; discussion 146-7.
77 Rivers EP, McCord J, Otero R, Jacobsen G, Loomba M. Clinical utility of B-type natriuretic peptide in early severe sepsis and septic shock. J Intensive Care Med. 2007;22(6):363-73.-7878 Varpula M, Pulkki K, Karlsson S, Ruokonen E, Pettilä V; FINNSEPSIS Study Group. Predictive value of N-terminal pro-brain natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(5):1277-83.) Hartemink et al. showed that a NT-proBNP cutoff of 3467pg/mL in septic patients predicted fluid responsiveness with a sensitivity of 90% and a specificity of 71%.(7979 Hartemink KJ, Twisk JW, Groeneveld AB. High circulating N-terminal pro-B-type natriuretic peptide is associated with greater systolic cardiac dysfunction and nonresponsiveness to fluids in septic vs nonseptic critically ill patients. J Crit Care. 2011;26(1):108.e1-8.) Similarly, Zhang et al. demonstrated a correlation between delta BNP over three days and fluid balance in septic patients (r = 0.63, p < 0.01).(8080 Zhang Z, Zhang Z, Xue Y, Xu X, Ni H. Prognostic value of B-type natriuretic peptide (BNP) and its potential role in guiding fluid therapy in critically ill septic patients. Scand J Trauma Resusc Emerg Med. 2012;20:86.) In contrast, several authors showed no correlation between BNP and various parameters of volume status. Among surgical ICU patients, in which 42% had severe sepsis and septic shock, BNP did not correlate with circulating blood volume as measured by radioisotope dilution (coefficient of determination of 0.09; p = 0.45).(8181 Takahashi EA, Moran SE, Hayashi MS, Inouye DS, Takanishi DM Jr, Yu M. Brain-type natriuretic peptide and right ventricular end-diastolic volume index measurements are imprecise estimates of circulating blood volume in critically ill subjects. J Trauma Acute Care Surg. 2013;75(5):813-8.) Pirracchio et al. demonstrated that despite BNP > 1000pg/mL, 9 out of 11 patients with septic shock were still fluid responsive.(3636 Pirracchio R, Deye N, Lukaszewicz AC, Mebazaa A, Cholley B, Matéo J, et al. Impaired plasma B-type natriuretic peptide clearance in human septic shock. Crit Care Med. 2008;36(9):2542-6.) Sturgess et al. showed a weak correlation between BNP and changes in stroke volume in septic shock patients (r = −0.3, p = 0.40).(8282 Sturgess DJ, Marwick TH, Joyce C, Jenkins C, Jones M, Masci P, et al. Prediction of hospital outcome in septic shock: a prospective comparison of tissue Doppler and cardiac biomarkers. Crit Care. 2010;14(2):R44.) From the existing limited data, BNP does not appear to be a reliable marker of fluid status or responsiveness in septic patients. B-type natriuretic peptide represents a static variable and is unlikely to correctly estimate RV or LV preload conditions that undergo dynamic adaptation in sepsis. Studies incorporating a BNP-directed fluid management protocol may help elaborate on the role of BNP in fluid status determination in sepsis patients.(8080 Zhang Z, Zhang Z, Xue Y, Xu X, Ni H. Prognostic value of B-type natriuretic peptide (BNP) and its potential role in guiding fluid therapy in critically ill septic patients. Scand J Trauma Resusc Emerg Med. 2012;20:86.)
Studies demonstrating correlations between natriuretic peptides and cardiac filling pressures in critically ill patients
NATRIURETIC PEPTIDES AND MORTALITY
B-type natriuretic peptide and NT-proBNP have shown a varied correlation with short-term mortality (Tables 2 and 3).(3030 Charpentier J, Luyt CE, Fulla Y, Vinsonneau C, Cariou A, Grabar S, et al. Brain natriuretic peptide: A marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004;32(3):660-5.,3131 Post F, Weilemann LS, Messow CM, Sinning C, Münzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36(11):3030-7.,4141 Klouche K, Pommet S, Amigues L, Bargnoux AS, Dupuy AM, Machado S, et al. Plasma brain natriuretic peptide and troponin levels in severe sepsis and septic shock: relationships with systolic myocardial dysfunction and intensive care unit mortality. J Intensive Care Med. 2014;29(4):229-37.,4242 Mokart D, Sannini A, Brun JP, Faucher M, Blaise D, Blache JL, et al. N-terminal pro-brain natriuretic peptide as an early prognostic factor in cancer patients developing septic shock. Crit Care. 2007;11(2):R37.,4747 Ueda S, Nishio K, Akai Y, Fukushima H, Ueyama T, Kawai Y, et al. Prognostic value of increased plasma levels of brain natriuretic peptide in patients with septic shock. Shock. 2006;26(2):134-9.,4949 Papanikolaou J, Makris D, Mpaka M, Palli E, Zygoulis P, Zakynthinos E. New insights into the mechanisms involved in B-type natriuretic peptide elevation and its prognostic value in septic patients. Crit Care. 2014;18(3):R94.,5757 Sturgess DJ, Pascoe RL, Scalia G, Venkatesh B. A comparison of transcutaneous Doppler corrected flow time, B-type natriuretic peptide and central venous pressure as predictors of fluid responsiveness in septic shock: a preliminary evaluation. Anaesth Intensive Care. 2010;38(2):336-41.,7878 Varpula M, Pulkki K, Karlsson S, Ruokonen E, Pettilä V; FINNSEPSIS Study Group. Predictive value of N-terminal pro-brain natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(5):1277-83.,8282 Sturgess DJ, Marwick TH, Joyce C, Jenkins C, Jones M, Masci P, et al. Prediction of hospital outcome in septic shock: a prospective comparison of tissue Doppler and cardiac biomarkers. Crit Care. 2010;14(2):R44.
83 Brueckmann M, Huhle G, Lang S, Haase KK, Bertsch T, Weiss C, et al. Prognostic value of plasma N-terminal pro-brain natriuretic peptide in patients with severe sepsis. Circulation. 2005;112(4):527-34.
84 Roch A, Allardet-Servent J, Michelet P, Oddoze C, Forel JM, Barrau K, et al. NH2 terminal pro-brain natriuretic peptide plasma level as an early marker of prognosis and cardiac dysfunction in septic shock patients. Crit Care Med. 2005;33(5):1001-7.
85 Guaricci AI, Santoro F, Paoletti Perini A, Ioffredo L, Trivedi C, Pontone G, et al. Correlations between NT-proBNP, outcome and haemodynamics in patients with septic shock. Acta Cardiol. 2015;70(5):545-52.
86 Zhao HY, An YZ, Liu F. [Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2009 May;21(5):293-5. Chinese.
87 Khoury J, Arow M, Elias A, Makhoul BF, Berger G, Kaplan M, et al. The prognostic value of brain natriuretic peptide (BNP) in non-cardiac patients with sepsis, ultra-long follow-up. J Crit Care. 2017;42:117-22.
88 Perman SM, Chang AM, Hollander JE, Gaieski DF, Trzeciak S, Birkhahn R, et al. Relationship between B-type natriuretic peptide and adverse outcome in patients with clinical evidence of sepsis presenting to the emergency department. Acad Emerg Med. 2011;18(2):219-22.
89 Chen Y, Li C. Prognostic significance of brain natriuretic peptide obtained in the ED in patients with SIRS or sepsis. Am J Emerg Med. 2009;27(6):701-6.-9090 Yucel T, Memis D, Karamanlioglu B, Süt N, Yuksel M. The prognostic value of atrial and brain natriuretic peptides, troponin I and C-reactive protein in patients with sepsis. Exp Clin Cardiol. 2008;13(4):183-8.) In patients with sepsis and septic shock, Charpentier et al. first showed that a BNP of > 190pg/mL on day two of admission was associated with a 5.7-fold increased risk of death (95% confidence interval [95%CI] 1.8 - 27.5; p = 0.14).(3030 Charpentier J, Luyt CE, Fulla Y, Vinsonneau C, Cariou A, Grabar S, et al. Brain natriuretic peptide: A marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004;32(3):660-5.) Brueckmann et al. evaluated NT-proBNP, also on day two of ICU admission, and noted a NT-proBNP of > 1400pg/mL was associated with a 3.9 times higher risk of mortality (95%CI, 1.6 - 9.7).(8383 Brueckmann M, Huhle G, Lang S, Haase KK, Bertsch T, Weiss C, et al. Prognostic value of plasma N-terminal pro-brain natriuretic peptide in patients with severe sepsis. Circulation. 2005;112(4):527-34.) Since these initial studies, many other investigators have evaluated the correlation of BNP and NT-proBNP with mortality in sepsis in various clinical settings (Tables 2 and 3). More recently, Khoury et al. demonstrated BNP at admission was strongly correlated with in-hospital, 90-day and 60-month mortality.(8787 Khoury J, Arow M, Elias A, Makhoul BF, Berger G, Kaplan M, et al. The prognostic value of brain natriuretic peptide (BNP) in non-cardiac patients with sepsis, ultra-long follow-up. J Crit Care. 2017;42:117-22.) Using predetermined cut-offs, they demonstrated serial increases in BNP to be associated with worse short-term mortality.(8787 Khoury J, Arow M, Elias A, Makhoul BF, Berger G, Kaplan M, et al. The prognostic value of brain natriuretic peptide (BNP) in non-cardiac patients with sepsis, ultra-long follow-up. J Crit Care. 2017;42:117-22.) Similar data have been noted in patients with acute exacerbations of chronic obstructive pulmonary disease, leading to the hypothesis that BNP should be used as a continuous outcome predictor in these patients.(3535 Vallabhajosyula S, Haddad TM, Sundaragiri PR, Ahmed AA, Nawaz MS, Rayes HA, et al. Role of B-type natriuretic peptide in predicting in-hospital outcomes in acute exacerbation of chronic obstructive pulmonary disease with preserved left ventricular function: a 5-year retrospective analysis. J Intensive Care Med. 2018;33(11):635-44.) Studies in the emergency room have shown higher natriuretic peptide levels to be associated with higher mortality.(8888 Perman SM, Chang AM, Hollander JE, Gaieski DF, Trzeciak S, Birkhahn R, et al. Relationship between B-type natriuretic peptide and adverse outcome in patients with clinical evidence of sepsis presenting to the emergency department. Acad Emerg Med. 2011;18(2):219-22.,8989 Chen Y, Li C. Prognostic significance of brain natriuretic peptide obtained in the ED in patients with SIRS or sepsis. Am J Emerg Med. 2009;27(6):701-6.) There have been variable cut-offs stated in the literature-Perman et al. demonstrated a BNP > 49pg/mL to be associated with increased mortality while Chen et al. used a cutoff of > 113pg/mL.(8888 Perman SM, Chang AM, Hollander JE, Gaieski DF, Trzeciak S, Birkhahn R, et al. Relationship between B-type natriuretic peptide and adverse outcome in patients with clinical evidence of sepsis presenting to the emergency department. Acad Emerg Med. 2011;18(2):219-22.,8989 Chen Y, Li C. Prognostic significance of brain natriuretic peptide obtained in the ED in patients with SIRS or sepsis. Am J Emerg Med. 2009;27(6):701-6.) The majority of studies focused on ICU patients, several of which evaluated mechanically ventilated patients. In mechanically ventilated septic patients, primary cardiac dysfunction often complicates the pulmonary process, leading to elevation of BNP via multiple mechanisms as highlighted in figure 1.(3434 Kotecha A, Vallabhajosyula S, Coville HH, Kashani K. Cardiorenal syndrome in sepsis: A narrative review. J Crit Care.43:122-7.,3535 Vallabhajosyula S, Haddad TM, Sundaragiri PR, Ahmed AA, Nawaz MS, Rayes HA, et al. Role of B-type natriuretic peptide in predicting in-hospital outcomes in acute exacerbation of chronic obstructive pulmonary disease with preserved left ventricular function: a 5-year retrospective analysis. J Intensive Care Med. 2018;33(11):635-44.,5555 Vallabhajosyula S, Kumar M, Pandompatam G, Sakhuja A, Kashyap R, Kashani K, et al. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7(1):94.) In mechanically ventilated patients, both BNP and NT-proBNP have been demonstrated to have a good correlation with mortality with areas under the receiver operating characteristic curve (AUROC) of 0.99 and 0.8, respectively.(8484 Roch A, Allardet-Servent J, Michelet P, Oddoze C, Forel JM, Barrau K, et al. NH2 terminal pro-brain natriuretic peptide plasma level as an early marker of prognosis and cardiac dysfunction in septic shock patients. Crit Care Med. 2005;33(5):1001-7.,9090 Yucel T, Memis D, Karamanlioglu B, Süt N, Yuksel M. The prognostic value of atrial and brain natriuretic peptides, troponin I and C-reactive protein in patients with sepsis. Exp Clin Cardiol. 2008;13(4):183-8.) In cancer patients who develop sepsis, NT-proBNP levels of > 6,624pg/mL predicted ICU mortality (AUROC 0.87; 95%CI 0.77 - 0.97; p < 0.001) on day two of ICU admission.(4242 Mokart D, Sannini A, Brun JP, Faucher M, Blaise D, Blache JL, et al. N-terminal pro-brain natriuretic peptide as an early prognostic factor in cancer patients developing septic shock. Crit Care. 2007;11(2):R37.) Several other studies also reported BNP correlations with mortality at various time points during hospital and ICU stays.(4141 Klouche K, Pommet S, Amigues L, Bargnoux AS, Dupuy AM, Machado S, et al. Plasma brain natriuretic peptide and troponin levels in severe sepsis and septic shock: relationships with systolic myocardial dysfunction and intensive care unit mortality. J Intensive Care Med. 2014;29(4):229-37.,4747 Ueda S, Nishio K, Akai Y, Fukushima H, Ueyama T, Kawai Y, et al. Prognostic value of increased plasma levels of brain natriuretic peptide in patients with septic shock. Shock. 2006;26(2):134-9.,7777 Rivers EP, McCord J, Otero R, Jacobsen G, Loomba M. Clinical utility of B-type natriuretic peptide in early severe sepsis and septic shock. J Intensive Care Med. 2007;22(6):363-73.,7878 Varpula M, Pulkki K, Karlsson S, Ruokonen E, Pettilä V; FINNSEPSIS Study Group. Predictive value of N-terminal pro-brain natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(5):1277-83.,8585 Guaricci AI, Santoro F, Paoletti Perini A, Ioffredo L, Trivedi C, Pontone G, et al. Correlations between NT-proBNP, outcome and haemodynamics in patients with septic shock. Acta Cardiol. 2015;70(5):545-52.,8989 Chen Y, Li C. Prognostic significance of brain natriuretic peptide obtained in the ED in patients with SIRS or sepsis. Am J Emerg Med. 2009;27(6):701-6.
90 Yucel T, Memis D, Karamanlioglu B, Süt N, Yuksel M. The prognostic value of atrial and brain natriuretic peptides, troponin I and C-reactive protein in patients with sepsis. Exp Clin Cardiol. 2008;13(4):183-8.-9191 Singh H, Ramai D, Patel H, Iskandir M, Sachdev S, Rai R, et al. B-type natriuretic peptide: a predictor for mortality, intensive care unit length of stay, and hospital length of stay in patients with resolving sepsis. Cardiol Res. 2017;8(6):271-5.) Most studies included patients already diagnosed with a sepsis syndrome before inclusion, and therefore limited data are currently available for the association of BNP and outcomes prior to the onset of sepsis. One study evaluated patients who developed sepsis during their ICU stay (evolving sepsis) and demonstrated that BNP measured on day five was correlated with 30-day mortality in these patients.(3131 Post F, Weilemann LS, Messow CM, Sinning C, Münzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36(11):3030-7.)
Some studies have shown no correlation between BNP and mortality in sepsis patients. Among forty patients with sepsis and septic shock, Mclean et al. reported that BNP did not predict in-hospital mortality (odds ratio 1.0, 95%CI 0.99 - 1.0).(4848 McLean AS, Huang SJ, Hyams S, Poh G, Nalos M, Pandit R, et al. Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(4):1019-26.) Other authors have also corroborated these findings, including in subsets of severe sepsis and septic shock.(7474 Jefic D, Lee JW, Jefic D, Savoy-Moore RT, Rosman HS. Utility of B-type natriuretic peptide and N-terminal pro B-type natriuretic peptide in evaluation of respiratory failure in critically ill patients. Chest. 2005;128(1):288-95.,8282 Sturgess DJ, Marwick TH, Joyce C, Jenkins C, Jones M, Masci P, et al. Prediction of hospital outcome in septic shock: a prospective comparison of tissue Doppler and cardiac biomarkers. Crit Care. 2010;14(2):R44.,9292 Rudiger A, Gasser S, Fischler M, Hornemann T, von Eckardstein A, Maggiorini M. Comparable increase of B-type natriuretic peptide and amino-terminal pro-B-type natriuretic peptide levels in patients with severe sepsis, septic shock, and acute heart failure. Crit Care Med. 2006;34(8):2140-4.,9393 Cuthbertson BH, Patel RR, Croal BL, Barclay J, Hillis GS. B-type natriuretic peptide and the prediction of outcome in patients admitted to intensive care. Anaesthesia. 2005;60(1):16-21.) These discrepant results may be partly due to the heterogeneity of sepsis, differences in timing of BNP measurement and types of assays used, small sample sizes and lack of controls for septic cardiomyopathy.(3333 McLean AS, Huang SJ. Brain not processing: is finding a role for BNP in sepsis like fitting a square peg into a round hole? Crit Care. 2014;18(4):161.,5151 Vallabhajosyula S, Pruthi S, Shah S, Wiley BM, Mankad SV, Jentzer JC. Basic and advanced echocardiographic evaluation of myocardial dysfunction in sepsis and septic shock. Anaesth Intensive Care. 2018;46(1):13-24.,5555 Vallabhajosyula S, Kumar M, Pandompatam G, Sakhuja A, Kashyap R, Kashani K, et al. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7(1):94.) The optimal timing for measurement of BNP still remains to be ascertained. In the reported literature, BNP and NT-proBNP were measured anytime between admission and day five.(2222 Wang F, Wu Y, Tang L, Zhu W, Chen F, Xu T, et al. Brain natriuretic peptide for prediction of mortality in patients with sepsis: a systematic review and meta-analysis. Crit Care. 2012;16(3):R74.) Although a recent meta-analysis demonstrated BNP to be a predictor of mortality in septic patients with pooled sensitivity and specificity of 79% and 60%, there was significant heterogeneity (I2 = 64%) among the evaluated studies.(2222 Wang F, Wu Y, Tang L, Zhu W, Chen F, Xu T, et al. Brain natriuretic peptide for prediction of mortality in patients with sepsis: a systematic review and meta-analysis. Crit Care. 2012;16(3):R74.) In this systematic analysis, BNP assays, clinical endpoints, and vasopressor use varied markedly among the enrolled studies.(2222 Wang F, Wu Y, Tang L, Zhu W, Chen F, Xu T, et al. Brain natriuretic peptide for prediction of mortality in patients with sepsis: a systematic review and meta-analysis. Crit Care. 2012;16(3):R74.) Additionally, exclusion of pre-existing conditions known to elevate BNP and NT-proBNP differed among studies, with five of the 12 studies including cases with a combination of either pre-existing kidney and/or cardiac disease. Furthermore, two of the largest included studies were performed in the emergency room, representing sepsis patients at a markedly different time of resuscitation than later in their hospital course.(8888 Perman SM, Chang AM, Hollander JE, Gaieski DF, Trzeciak S, Birkhahn R, et al. Relationship between B-type natriuretic peptide and adverse outcome in patients with clinical evidence of sepsis presenting to the emergency department. Acad Emerg Med. 2011;18(2):219-22.,8989 Chen Y, Li C. Prognostic significance of brain natriuretic peptide obtained in the ED in patients with SIRS or sepsis. Am J Emerg Med. 2009;27(6):701-6.)
Despite suggestions of a correlation with mortality, the role of BNP in mortality outcomes and prognosis during sepsis needs further evaluation in larger prospective studies. A single marker known to be elevated in a wide range of pathophysiologic states is unlikely to be a perfect fit as a prognostic marker in sepsis.(3333 McLean AS, Huang SJ. Brain not processing: is finding a role for BNP in sepsis like fitting a square peg into a round hole? Crit Care. 2014;18(4):161.)
Scoring systems, optimal cut-offs and serial testing
In recent years, some authors have used natriuretic peptides to develop novel scoring systems or demonstrate more accurate prognostic capacities than pre-existing scoring systems.(8787 Khoury J, Arow M, Elias A, Makhoul BF, Berger G, Kaplan M, et al. The prognostic value of brain natriuretic peptide (BNP) in non-cardiac patients with sepsis, ultra-long follow-up. J Crit Care. 2017;42:117-22.,9494 Liu Z, Chen J, Liu Y, Si X, Jiang Z, Zhang X, et al. A simple bioscore improves diagnostic accuracy of sepsis after surgery. J Surg Res. 2016;200(1):290-7.) Khoury et al. demonstrated that BNP at admission was more predictive of short-term mortality than the Sequential Organ Failure Assessment (SOFA) score.(8787 Khoury J, Arow M, Elias A, Makhoul BF, Berger G, Kaplan M, et al. The prognostic value of brain natriuretic peptide (BNP) in non-cardiac patients with sepsis, ultra-long follow-up. J Crit Care. 2017;42:117-22.) In contrast, Ryoo et al. demonstrated a combination of BNP with the SOFA score resulted in better outcomes and prognosis in septic patients who either method independently.(9595 Ryoo SM, Kim WY, Huh JW, Hong SB, Lim CM, Koh Y, et al. Prognostic value of B-type natriuretic peptide with the sequential organ failure assessment score in septic shock. Am J Med Sci. 2015;349(4):287-91.) In surgically critically ill patients, the use of a bioscore combining BNP with lymphocyte percentage and procalcitonin showed a strong prediction for sepsis onset in this population.(9494 Liu Z, Chen J, Liu Y, Si X, Jiang Z, Zhang X, et al. A simple bioscore improves diagnostic accuracy of sepsis after surgery. J Surg Res. 2016;200(1):290-7.)
The optimal cutoff of BNP and NT-proBNP to predict mortality in sepsis remains uncertain and varies between 32 to 681pg/mL for BNP and 400 to 13,600pg/mL for NT-proBNP. A recent meta-analysis was unable to determine optimal cutoffs for mortality outcomes and prognosis in patients with sepsis.(2222 Wang F, Wu Y, Tang L, Zhu W, Chen F, Xu T, et al. Brain natriuretic peptide for prediction of mortality in patients with sepsis: a systematic review and meta-analysis. Crit Care. 2012;16(3):R74.) In the evaluation of patients with dyspnea, a BNP level of < 100pg/mL has been used as a sensitive and specific value for ruling out heart failure. A level of > 400pg/mL suggests that heart failure is potentially a contributor to the patient's symptoms with 90% specificity.(9696 Maisel A, Mueller C, Adams K Jr, Anker SD, Aspromonte N, Cleland JG, et al. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail. 2008;10(9):824-39.) For NT-proBNP, a cutoff of 300pg/mL is used to rule out heart failure, whereas optimal 'rule-in' cutoffs vary, depending on age (450pg/mL for < 50 years, 900pg/mL for 50 - 75 years, and 1800pg/mL for > 75 years).(9696 Maisel A, Mueller C, Adams K Jr, Anker SD, Aspromonte N, Cleland JG, et al. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail. 2008;10(9):824-39.
97 Kim HN, Januzzi JL Jr. Natriuretic peptide testing in heart failure. Circulation. 2011;123(18):2015-9.-9898 Chow SL, Maisel AS, Anand I, de Boer RA, Felker GM, Fonarow GC, Greenberg B, Januzzi JL Jr, Kiernan MS, Liu PP, Wang TJ, Yancy CW, Zile MR; American Heart Association Clinical Pharmacology Committee of the Council on Clinical Cardiology; Council on Basic Cardiovascular Sciences; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Epidemiology and Prevention; Council on Functional Genomics and Translational Biology; and Council on Quality of Care and Outcomes Research. Role of biomarkers for the prevention, assessment, and management of heart failure: a scientific statement from the American Heart Association. Circulation. 2017;135(22):e1054-e1091. Erratum in: Circulation. 2017;136(19):e345.)
Akin to acute heart failure, there may be utility in trending natriuretic peptides in patients with sepsis.(6565 Shah MR, Califf RM, Nohria A, Bhapkar M, Bowers M, Mancini DM, et al. The STARBRITE trial: a randomized, pilot study of B-type natriuretic peptide-guided therapy in patients with advanced heart failure. J Card Fail. 2011;17(8):613-21.) Serial BNP testing may have greater clinical utility in outcomes and prognosis for patients with sepsis rather than as a one-time measure. Papanikolaou et al. recently demonstrated that persistently elevated BNP > 500pg/mL was a better predictor of 28-day mortality than isolated BNP values.(4949 Papanikolaou J, Makris D, Mpaka M, Palli E, Zygoulis P, Zakynthinos E. New insights into the mechanisms involved in B-type natriuretic peptide elevation and its prognostic value in septic patients. Crit Care. 2014;18(3):R94.) Inability to reduce BNP to < 500pg/mL predicted 28-day mortality with AUROC 0.74 (95%CI 0.55 - 0.93; p = 0.03).(4949 Papanikolaou J, Makris D, Mpaka M, Palli E, Zygoulis P, Zakynthinos E. New insights into the mechanisms involved in B-type natriuretic peptide elevation and its prognostic value in septic patients. Crit Care. 2014;18(3):R94.) Similarly, several other authors showed that improvements in BNP in serial measurements conducted over their ICU stay were associated with better survival, and variation between baseline BNP compared to 72 hours was significantly associated with 28-day mortality.(4141 Klouche K, Pommet S, Amigues L, Bargnoux AS, Dupuy AM, Machado S, et al. Plasma brain natriuretic peptide and troponin levels in severe sepsis and septic shock: relationships with systolic myocardial dysfunction and intensive care unit mortality. J Intensive Care Med. 2014;29(4):229-37.,8585 Guaricci AI, Santoro F, Paoletti Perini A, Ioffredo L, Trivedi C, Pontone G, et al. Correlations between NT-proBNP, outcome and haemodynamics in patients with septic shock. Acta Cardiol. 2015;70(5):545-52.) 'Delta BNP' is a promising dynamic marker used to assess cardiovascular function and the outcomes of sepsis.
SPECIAL CONSIDERATIONS
Impact of renal failure, age, and sex
Kidney dysfunction is a well-known cause of elevated natriuretic peptide levels and often confounds assessment in sepsis where AKI is seen in nearly 50 - 65% of patients.(3434 Kotecha A, Vallabhajosyula S, Coville HH, Kashani K. Cardiorenal syndrome in sepsis: A narrative review. J Crit Care.43:122-7.,9999 Mueller C, Laule-Kilian K, Scholer A, Nusbaumer C, Zeller T, Staub D, et al. B-type natriuretic peptide for acute dyspnea in patients with kidney disease: insights from a randomized comparison. Kidney Int. 2005;67(1):278-84.) An inverse correlation has been shown between BNP and kidney dysfunction in critically ill patients. However, optimal cutoffs are yet to be defined in the septic population.(2222 Wang F, Wu Y, Tang L, Zhu W, Chen F, Xu T, et al. Brain natriuretic peptide for prediction of mortality in patients with sepsis: a systematic review and meta-analysis. Crit Care. 2012;16(3):R74.,7474 Jefic D, Lee JW, Jefic D, Savoy-Moore RT, Rosman HS. Utility of B-type natriuretic peptide and N-terminal pro B-type natriuretic peptide in evaluation of respiratory failure in critically ill patients. Chest. 2005;128(1):288-95.,7575 Forfia PR, Watkins SP, Rame JE, Stewart KJ, Shapiro EP. Relationship between B-type natriuretic peptides and pulmonary capillary wedge pressure in the intensive care unit. J Am Coll Cardiol. 2005;45(10):1667-71.) Several studies have shown elevated BNP levels in kidney dysfunction compared to patients with normal renal function despite similar cardiac function and hemodynamics.(3636 Pirracchio R, Deye N, Lukaszewicz AC, Mebazaa A, Cholley B, Matéo J, et al. Impaired plasma B-type natriuretic peptide clearance in human septic shock. Crit Care Med. 2008;36(9):2542-6.,100100 McLean AS, Huang SJ, Nalos M, Tang B, Stewart DE. The confounding effects of age, gender, serum creatinine, and electrolyte concentrations on plasma B-type natriuretic peptide concentrations in critically ill patients. Crit Care Med. 2003;31(11):2611-8.) Abnormalities in kidney function in sepsis remain a major confounder in studies evaluating the prognostic value of BNP in sepsis, as current studies variably exclude pre-existing chronic kidney disease and inconsistently adjust for acute kidney injury in the analysis.(2222 Wang F, Wu Y, Tang L, Zhu W, Chen F, Xu T, et al. Brain natriuretic peptide for prediction of mortality in patients with sepsis: a systematic review and meta-analysis. Crit Care. 2012;16(3):R74.) In septic patients, studies have shown conflicting results regarding correlations between BNP and serum creatinine; Roch et al.(8484 Roch A, Allardet-Servent J, Michelet P, Oddoze C, Forel JM, Barrau K, et al. NH2 terminal pro-brain natriuretic peptide plasma level as an early marker of prognosis and cardiac dysfunction in septic shock patients. Crit Care Med. 2005;33(5):1001-7.) showed a weak correlation (r = 0.2, p = 0.03), whereas Ueda et al.(4747 Ueda S, Nishio K, Akai Y, Fukushima H, Ueyama T, Kawai Y, et al. Prognostic value of increased plasma levels of brain natriuretic peptide in patients with septic shock. Shock. 2006;26(2):134-9.) showed no correlation. In addition to renal function, age and sex influence natriuretic peptide levels. Increasing age is known to cause elevated BNP and NT pro-BNP levels, although the mechanisms remain under investigation.(100100 McLean AS, Huang SJ, Nalos M, Tang B, Stewart DE. The confounding effects of age, gender, serum creatinine, and electrolyte concentrations on plasma B-type natriuretic peptide concentrations in critically ill patients. Crit Care Med. 2003;31(11):2611-8.,101101 Redfield MM, Rodeheffer RJ, Jacobsen SJ, Mahoney DW, Bailey KR, Burnett JC Jr. Plasma brain natriuretic peptide concentration: impact of age and gender. J Am Coll Cardiol. 2002;40(5):976-82.) Women generally have higher levels of BNP and NT pro-BNP due to higher estrogen levels.(101101 Redfield MM, Rodeheffer RJ, Jacobsen SJ, Mahoney DW, Bailey KR, Burnett JC Jr. Plasma brain natriuretic peptide concentration: impact of age and gender. J Am Coll Cardiol. 2002;40(5):976-82.) Cutoffs based on age and sex have been suggested in primary care patients and heart failure populations but have not been validated in sepsis populations at the current time.(102102 Keyzer JM, Hoffmann JJ, Ringoir L, Nabbe KC, Widdershoven JW, Pop VJ. Age- and gender-specific brain natriuretic peptide (BNP) reference ranges in primary care. Clin Chem Lab Med. 2014;52(9):1341-6.)
CONCLUSIONS
Natriuretic peptides are commonly elevated in patients with sepsis. Despite suggestions that their elevation can predict mortality and other clinically meaningful outcomes, studies are conflicting, and the role of these biomarkers remains unclear. The role of BNP and NT-proBNP in evaluating acute and chronic cardiovascular morbidity in sepsis and septic shock remains an exciting new avenue, and further research is warranted. Trends rather than isolated values may be more useful, and their use in conjunction with other clinical data may define a clearer role for BNP and NT-proBNP in sepsis.
REFERÊNCIAS
-
1Cuthbertson BH, Elders A, Hall S, Taylor J, MacLennan G, Mackirdy F, Mackenzie SJ; Scottish Critical Care Trials Group; Scottish Intensive Care Society Audit Group. Mortality and quality of life in the five years after severe sepsis. Crit Care. 2013;17(2):R70.
-
2Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis. Crit Care Med. 2014;42(3):625-31.
-
3Jentzer JC, Vallabhajosyula S, Khanna AK, Chawla LS, Busse LW, Kashani KB. Management of refractory vasodilatory shock. Chest. 2018;154(2):416-26.
-
4Kotecha AA, Vallabhajosyula S, Apala DR, Frazee E, Iyer VN. Clinical outcomes of weight-based norepinephrine dosing in underweight and morbidly obese patients: a propensity-matched analysis. J Intensive Care Med. 2018:885066618768180.
-
5Vallabhajosyula S, Jentzer JC, Kotecha AA, Murphree DH Jr, Barreto EF, Khanna AK, et al. Development and performance of a novel vasopressor-driven mortality prediction model in septic shock. Ann Intensive Care. 2018;8(1):112.
-
6Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-10.
-
7Vincent JL. The clinical challenge of sepsis identification and monitoring. PLoS Med. 2016;13(5):e1002022.
-
8Haddad TM, Vallabhajosyula S, Nawaz MS, Vivekanandan R. Fatal Pneumocystis jirovecii pneumonia in a HIV-negative adult. BMJ Case Rep. 2015;2015. pii: bcr2015210117.
-
9Mahfood Haddad T, Vallabhajosyula S, Sundaragiri PR, Vivekanandan R. Mycotic pseudoaneurysm by vancomycin-intermediate Staphylococcus aureus: a rare cause of persistent bacteraemia. BMJ Case Rep. 2015;2015. pii: bcr2014209003.
-
10Rose SR, Vallabhajosyula S, Velez MG, Fedorko DP, VanRaden MJ, Gea-Banacloche JC, et al. The utility of bronchoalveolar lavage beta-D-glucan testing for the diagnosis of invasive fungal infections. J Infect. 2014;69(3):278-83.
-
11Sundaragiri PR, Vallabhajosyula S, Haddad TM, Esterbrooks DJ. Tricuspid and mitral endocarditis due to methicillin-resistant Staphylococcus aureus exhibiting vancomycin-creep phenomenon. BMJ Case Rep. 2015;2015. pii: bcr2015211974.
-
12Vallabhajosyula S, Varma MD, Vallabhajosyula S, Vallabhajosyula S. Association of hyponatremia with in-hospital outcomes in infective endocarditis: A 5-year review from an Indian Intensive Care Unit. Indian J Crit Care Med. 2016;20(10):597-600.
-
13Vallabhajosyula S, Varma MD, Vallabhajosyula S, Vallabhajosyula S. Right-sided infective endocarditis in an Indian intensive care unit. J Glob Infect Dis. 2016;8(3):124-5.
-
14Varma MD, Vengalil S, Vallabhajosyula S, Krishnakumar PC, Vidyasagar S. Leptospirosis and dengue fever: a predictive model for early differentiation based on clinical and biochemical parameters. Trop Doct. 2014;44(2):100-2.
-
15Tang BM, Eslick GD, Craig JC, McLean AS. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systematic review and meta-analysis. Lancet Infect Dis. 2007;7(3):210-7.
-
16Wu CC, Lan HM, Han ST, Chaou CH, Yeh CF, Liu SH, et al. Comparison of diagnostic accuracy in sepsis between presepsin, procalcitonin, and C-reactive protein: a systematic review and meta-analysis. Ann Intensive Care. 2017;7(1):91.
-
17Landesberg G, Jaffe AS, Gilon D, Levin PD, Goodman S, Abu-Baih A, et al. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit Care Med. 2014;42(4):790-800.
-
18Vallabhajosyula S, Sakhuja A, Geske JB, Kumar M, Poterucha JT, Kashyap R, et al. Role of admission troponin-T and serial troponin-T testing in predicting outcomes in severe sepsis and septic shock. J Am Heart Assoc. 2017;6(9). pii: e005930.
-
19Vallabhajosyula S, Sakhuja A, Geske JB, Kumar M, Kashyap R, Kashani K, et al. Clinical profile and outcomes of acute cardiorenal syndrome type-5 in sepsis: An eight-year cohort study. PLoS One. 2018;13(1):e0190965.
-
20Bessière F, Khenifer S, Dubourg J, Durieu I, Lega JC. Prognostic value of troponins in sepsis: a meta-analysis. Intensive Care Med. 2013;39(7):1181-9.
-
21Machado Rde L, David CM, Luiz RR, Amitrano Dde A, Salomão Cde S, Oliveira GM. Related prognostic factors in elderly patients with severe sepsis and septic shock. Rev Bras Ter Intensiva. 2009;21(1):9-17.
-
22Wang F, Wu Y, Tang L, Zhu W, Chen F, Xu T, et al. Brain natriuretic peptide for prediction of mortality in patients with sepsis: a systematic review and meta-analysis. Crit Care. 2012;16(3):R74.
-
23Sudoh T, Kangawa K, Minamino N, Matsuo H. A new natriuretic peptide in porcine brain. Nature. 1988;332(6159):78-81.
-
24Hall C. Essential biochemistry and physiology of (NT-pro)BNP. Eur J Heart Fail. 2004;6(3):257-60.
-
25Vanderheyden M, Bartunek J, Goethals M. Brain and other natriuretic peptides: molecular aspects. Eur J Heart Fail. 2004;6(3):261-8.
-
26Mukoyama M, Nakao K, Hosoda K, Suga S, Saito Y, Ogawa Y, et al. Brain natriuretic peptide as a novel cardiac hormone in humans. Evidence for an exquisite dual natriuretic peptide system, atrial natriuretic peptide and brain natriuretic peptide. J Clin Invest. 1991;87(4):1402-12.
-
27Smith MW, Espiner EA, Yandle TG, Charles CJ, Richards AM. Delayed metabolism of human brain natriuretic peptide reflects resistance to neutral endopeptidase. J Endocrinol. 2000;167(2):239-46.
-
28Valli N, Gobinet A, Bordenave L. Review of 10 years of the clinical use of brain natriuretic peptide in cardiology. J Lab Clin Med. 1999;134(5):437-44.
-
29Zakynthinos E, Kiropoulos T, Gourgoulianis K, Filippatos G. Diagnostic and prognostic impact of brain natriuretic peptide in cardiac and noncardiac diseases. Heart Lung. 2008;37(4):275-85.
-
30Charpentier J, Luyt CE, Fulla Y, Vinsonneau C, Cariou A, Grabar S, et al. Brain natriuretic peptide: A marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004;32(3):660-5.
-
31Post F, Weilemann LS, Messow CM, Sinning C, Münzel T. B-type natriuretic peptide as a marker for sepsis-induced myocardial depression in intensive care patients. Crit Care Med. 2008;36(11):3030-7.
-
32Shor R, Rozenman Y, Bolshinsky A, Harpaz D, Tilis Y, Matas Z, et al. BNP in septic patients without systolic myocardial dysfunction. Eur J Intern Med. 2006;17(8):536-40.
-
33McLean AS, Huang SJ. Brain not processing: is finding a role for BNP in sepsis like fitting a square peg into a round hole? Crit Care. 2014;18(4):161.
-
34Kotecha A, Vallabhajosyula S, Coville HH, Kashani K. Cardiorenal syndrome in sepsis: A narrative review. J Crit Care.43:122-7.
-
35Vallabhajosyula S, Haddad TM, Sundaragiri PR, Ahmed AA, Nawaz MS, Rayes HA, et al. Role of B-type natriuretic peptide in predicting in-hospital outcomes in acute exacerbation of chronic obstructive pulmonary disease with preserved left ventricular function: a 5-year retrospective analysis. J Intensive Care Med. 2018;33(11):635-44.
-
36Pirracchio R, Deye N, Lukaszewicz AC, Mebazaa A, Cholley B, Matéo J, et al. Impaired plasma B-type natriuretic peptide clearance in human septic shock. Crit Care Med. 2008;36(9):2542-6.
-
37Vallabhajosyula S, Jentzer JC, Geske JB, Kumar M, Sakhuja A, Singhal A, et al. New-onset heart failure and mortality in hospital survivors of sepsis-related left ventricular dysfunction. Shock. 2018;49(2):144-9.
-
38Sevilla Berrios RA, O'Horo JC, Velagapudi V, Pulido JN. Correlation of left ventricular systolic dysfunction determined by low ejection fraction and 30-day mortality in patients with severe sepsis and septic shock: a systematic review and meta-analysis. J Crit Care. 2014;29(4):495-9.
-
39Vallabhajosyula S, Deshmukh AJ, Kashani K, Prasad A, Sakhuja A. Tako-tsubo cardiomyopathy in severe sepsis: Nationwide trends, predictors, and outcomes. J Am Heart Assoc. 2018;7(18):e009160.
-
40Huang SJ, Nalos M, McLean AS. Is early ventricular dysfunction or dilatation associated with lower mortality rate in adult severe sepsis and septic shock? A meta-analysis. Crit Care. 2013;17(3):R96.
-
41Klouche K, Pommet S, Amigues L, Bargnoux AS, Dupuy AM, Machado S, et al. Plasma brain natriuretic peptide and troponin levels in severe sepsis and septic shock: relationships with systolic myocardial dysfunction and intensive care unit mortality. J Intensive Care Med. 2014;29(4):229-37.
-
42Mokart D, Sannini A, Brun JP, Faucher M, Blaise D, Blache JL, et al. N-terminal pro-brain natriuretic peptide as an early prognostic factor in cancer patients developing septic shock. Crit Care. 2007;11(2):R37.
-
43Repessè X, Charron C, Vieillard-Baron A. Evaluation of left ventricular systolic function revisited in septic shock. Crit Care. 2013;17(4):164.
-
44Kumar A, Anel R, Bunnell E, Zanotti S, Habet K, Haery C, et al. Preload-independent mechanisms contribute to increased stroke volume following large volume saline infusion in normal volunteers: a prospective interventional study. Crit Care. 2004;8(3):R128-36.
-
45Vincent JL, Gris P, Coffernils M, Leon M, Pinsky M, Reuse C, et al. Myocardial depression characterizes the fatal course of septic shock. Surgery. 1992;111(6):660-7.
-
46Witthaut R, Busch C, Fraunberger P, Walli A, Seidel D, Pilz G, et al. Plasma atrial natriuretic peptide and brain natriuretic peptide are increased in septic shock: impact of interleukin-6 and sepsis-associated left ventricular dysfunction. Intensive Care Med. 2003;29(10):1696-702.
-
47Ueda S, Nishio K, Akai Y, Fukushima H, Ueyama T, Kawai Y, et al. Prognostic value of increased plasma levels of brain natriuretic peptide in patients with septic shock. Shock. 2006;26(2):134-9.
-
48McLean AS, Huang SJ, Hyams S, Poh G, Nalos M, Pandit R, et al. Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(4):1019-26.
-
49Papanikolaou J, Makris D, Mpaka M, Palli E, Zygoulis P, Zakynthinos E. New insights into the mechanisms involved in B-type natriuretic peptide elevation and its prognostic value in septic patients. Crit Care. 2014;18(3):R94.
-
50Burjonroppa SC, Tong AT, Xiao LC, Johnson MM, Yusuf SW, Lenihan DJ. Cancer patients with markedly elevated B-type natriuretic peptide may not have volume overload. Am J Clin Oncol. 2007;30(3):287-93.
-
51Vallabhajosyula S, Pruthi S, Shah S, Wiley BM, Mankad SV, Jentzer JC. Basic and advanced echocardiographic evaluation of myocardial dysfunction in sepsis and septic shock. Anaesth Intensive Care. 2018;46(1):13-24.
-
52Vallabhajosyula S, Rayes HA, Sakhuja A, Murad MH, Geske JB, Jentzer JC. Global longitudinal strain using speckle-tracking echocardiography as a mortality predictor in sepsis: A systematic review. J Intensive Care Med. 2019;34(2):87-93.
-
53Sanfilippo F, Corredor C, Fletcher N, Landesberg G, Benedetto U, Foex P, et al. Diastolic dysfunction and mortality in septic patients: a systematic review and meta-analysis. Intensive Care Med. 2015;41(6):1004-13. Erratum in: Intensive Care Med. 2015;41(6):1178-9.
-
54van Veldhuisen DJ, Linssen GC, Jaarsma T, van Gilst WH, Hoes AW, Tijssen JG, et al. B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction. J Am Coll Cardiol. 2013;61(14):1498-506.
-
55Vallabhajosyula S, Kumar M, Pandompatam G, Sakhuja A, Kashyap R, Kashani K, et al. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7(1):94.
-
56Vallabhajosyula S, Gillespie SM, Barbara DW, Anavekar NS, Pulido JN. Impact of new-onset left ventricular dysfunction on outcomes in mechanically ventilated patients with severe sepsis and septic shock. J Intensive Care Med. 2018;33(12):680-6.
-
57Sturgess DJ, Pascoe RL, Scalia G, Venkatesh B. A comparison of transcutaneous Doppler corrected flow time, B-type natriuretic peptide and central venous pressure as predictors of fluid responsiveness in septic shock: a preliminary evaluation. Anaesth Intensive Care. 2010;38(2):336-41.
-
58Lin X, Jiang X, Cheng Q, Liu C, Zhang X. [Changes of left ventricular systolic and diastolic function and the diagnostic value of B-type natriuretic peptide in patients with sepsis]. Zhonghua Yi Xue Za Zhi. 2014;94(11):816-20. Chinese.
-
59Chandra NG, Vallabhajosyula S, Shastry BA, Vallabhajosyula S, Vallabhajosyula S, Saravu K. Use of corticosteroids in acute respiratory distress syndrome: Perspective from an Indian intensive care unit. Med J Armed Forces India. 2017;73(2):118-22.
-
60Vallabhajosyula S, Geske JB, Kumar M, Kashyap R, Kashani K, Jentzer JC. Doppler-defined pulmonary hypertension in sepsis and septic shock. J Crit Care. 2019;50:201-6.
-
61Vallabhajosyula S, Trivedi V, Gajic O. Ventilation in acute respiratory distress syndrome: importance of low-tidal volume. Ann Transl Med. 2016;4(24):496.
-
62Mitaka C, Hirata Y, Nagura T, Tsunoda Y, Itoh M, Amaha K. Increased plasma concentrations of brain natriuretic peptide in patients with acute lung injury. J Crit Care. 1997;12(2):66-71.
-
63Enea I, Ceparano G, Mazzarella G, Di Sarno R, Cangiano G, Busino CA. [Biohumoral markers and right ventricular dysfunction in acute pulmonary embolism: the answer to thrombolytic therapy]. Ital Heart J Suppl. 2004;5(1):29-35. Italian.
-
64Orde SR, Pulido JN, Masaki M, Gillespie S, Spoon JN, Kane GC, et al. Outcome prediction in sepsis: speckle tracking echocardiography based assessment of myocardial function. Crit Care. 2014;18(4):R149.
-
65Shah MR, Califf RM, Nohria A, Bhapkar M, Bowers M, Mancini DM, et al. The STARBRITE trial: a randomized, pilot study of B-type natriuretic peptide-guided therapy in patients with advanced heart failure. J Card Fail. 2011;17(8):613-21.
-
66Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304-77.
-
67Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011;39(2):259-65.
-
68Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med. 2013;41(7):1774-81.
-
69Pinsky MR. Heart lung interactions during mechanical ventilation. Curr Opin Crit Care. 2012;18(3):256-60.
-
70Maeda K, Tsutamoto T, Wada A, Hisanaga T, Kinoshita M. Plasma brain natriuretic peptide as a biochemical marker of high left ventricular end-diastolic pressure in patients with symptomatic left ventricular dysfunction. Am Heart J. 1998;135(5 Pt 1):825-32.
-
71Dokainish H, Zoghbi WA, Lakkis NM, Al-Bakshy F, Dhir M, Quinones MA, et al. Optimal noninvasive assessment of left ventricular filling pressures: a comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation. 2004;109(20):2432-9.
-
72Kazanegra R, Cheng V, Garcia A, Krishnaswamy P, Gardetto N, Clopton P, et al. A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompensated heart failure: a pilot study. J Card Fail. 2001;7(1):21-9.
-
73Tung RH, Garcia C, Morss AM, Pino RM, Fifer MA, Thompson BT, et al. Utility of B-type natriuretic peptide for the evaluation of intensive care unit shock. Crit Care Med. 2004;32(8):1643-7.
-
74Jefic D, Lee JW, Jefic D, Savoy-Moore RT, Rosman HS. Utility of B-type natriuretic peptide and N-terminal pro B-type natriuretic peptide in evaluation of respiratory failure in critically ill patients. Chest. 2005;128(1):288-95.
-
75Forfia PR, Watkins SP, Rame JE, Stewart KJ, Shapiro EP. Relationship between B-type natriuretic peptides and pulmonary capillary wedge pressure in the intensive care unit. J Am Coll Cardiol. 2005;45(10):1667-71.
-
76Turner KL, Moore LJ, Todd SR, Sucher JF, Jones SA, McKinley BA, et al. Identification of cardiac dysfunction in sepsis with B-typenatriuretic peptide. J Am Coll Surg. 2011;213(1):139-46; discussion 146-7.
-
77Rivers EP, McCord J, Otero R, Jacobsen G, Loomba M. Clinical utility of B-type natriuretic peptide in early severe sepsis and septic shock. J Intensive Care Med. 2007;22(6):363-73.
-
78Varpula M, Pulkki K, Karlsson S, Ruokonen E, Pettilä V; FINNSEPSIS Study Group. Predictive value of N-terminal pro-brain natriuretic peptide in severe sepsis and septic shock. Crit Care Med. 2007;35(5):1277-83.
-
79Hartemink KJ, Twisk JW, Groeneveld AB. High circulating N-terminal pro-B-type natriuretic peptide is associated with greater systolic cardiac dysfunction and nonresponsiveness to fluids in septic vs nonseptic critically ill patients. J Crit Care. 2011;26(1):108.e1-8.
-
80Zhang Z, Zhang Z, Xue Y, Xu X, Ni H. Prognostic value of B-type natriuretic peptide (BNP) and its potential role in guiding fluid therapy in critically ill septic patients. Scand J Trauma Resusc Emerg Med. 2012;20:86.
-
81Takahashi EA, Moran SE, Hayashi MS, Inouye DS, Takanishi DM Jr, Yu M. Brain-type natriuretic peptide and right ventricular end-diastolic volume index measurements are imprecise estimates of circulating blood volume in critically ill subjects. J Trauma Acute Care Surg. 2013;75(5):813-8.
-
82Sturgess DJ, Marwick TH, Joyce C, Jenkins C, Jones M, Masci P, et al. Prediction of hospital outcome in septic shock: a prospective comparison of tissue Doppler and cardiac biomarkers. Crit Care. 2010;14(2):R44.
-
83Brueckmann M, Huhle G, Lang S, Haase KK, Bertsch T, Weiss C, et al. Prognostic value of plasma N-terminal pro-brain natriuretic peptide in patients with severe sepsis. Circulation. 2005;112(4):527-34.
-
84Roch A, Allardet-Servent J, Michelet P, Oddoze C, Forel JM, Barrau K, et al. NH2 terminal pro-brain natriuretic peptide plasma level as an early marker of prognosis and cardiac dysfunction in septic shock patients. Crit Care Med. 2005;33(5):1001-7.
-
85Guaricci AI, Santoro F, Paoletti Perini A, Ioffredo L, Trivedi C, Pontone G, et al. Correlations between NT-proBNP, outcome and haemodynamics in patients with septic shock. Acta Cardiol. 2015;70(5):545-52.
-
86Zhao HY, An YZ, Liu F. [Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2009 May;21(5):293-5. Chinese.
-
87Khoury J, Arow M, Elias A, Makhoul BF, Berger G, Kaplan M, et al. The prognostic value of brain natriuretic peptide (BNP) in non-cardiac patients with sepsis, ultra-long follow-up. J Crit Care. 2017;42:117-22.
-
88Perman SM, Chang AM, Hollander JE, Gaieski DF, Trzeciak S, Birkhahn R, et al. Relationship between B-type natriuretic peptide and adverse outcome in patients with clinical evidence of sepsis presenting to the emergency department. Acad Emerg Med. 2011;18(2):219-22.
-
89Chen Y, Li C. Prognostic significance of brain natriuretic peptide obtained in the ED in patients with SIRS or sepsis. Am J Emerg Med. 2009;27(6):701-6.
-
90Yucel T, Memis D, Karamanlioglu B, Süt N, Yuksel M. The prognostic value of atrial and brain natriuretic peptides, troponin I and C-reactive protein in patients with sepsis. Exp Clin Cardiol. 2008;13(4):183-8.
-
91Singh H, Ramai D, Patel H, Iskandir M, Sachdev S, Rai R, et al. B-type natriuretic peptide: a predictor for mortality, intensive care unit length of stay, and hospital length of stay in patients with resolving sepsis. Cardiol Res. 2017;8(6):271-5.
-
92Rudiger A, Gasser S, Fischler M, Hornemann T, von Eckardstein A, Maggiorini M. Comparable increase of B-type natriuretic peptide and amino-terminal pro-B-type natriuretic peptide levels in patients with severe sepsis, septic shock, and acute heart failure. Crit Care Med. 2006;34(8):2140-4.
-
93Cuthbertson BH, Patel RR, Croal BL, Barclay J, Hillis GS. B-type natriuretic peptide and the prediction of outcome in patients admitted to intensive care. Anaesthesia. 2005;60(1):16-21.
-
94Liu Z, Chen J, Liu Y, Si X, Jiang Z, Zhang X, et al. A simple bioscore improves diagnostic accuracy of sepsis after surgery. J Surg Res. 2016;200(1):290-7.
-
95Ryoo SM, Kim WY, Huh JW, Hong SB, Lim CM, Koh Y, et al. Prognostic value of B-type natriuretic peptide with the sequential organ failure assessment score in septic shock. Am J Med Sci. 2015;349(4):287-91.
-
96Maisel A, Mueller C, Adams K Jr, Anker SD, Aspromonte N, Cleland JG, et al. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail. 2008;10(9):824-39.
-
97Kim HN, Januzzi JL Jr. Natriuretic peptide testing in heart failure. Circulation. 2011;123(18):2015-9.
-
98Chow SL, Maisel AS, Anand I, de Boer RA, Felker GM, Fonarow GC, Greenberg B, Januzzi JL Jr, Kiernan MS, Liu PP, Wang TJ, Yancy CW, Zile MR; American Heart Association Clinical Pharmacology Committee of the Council on Clinical Cardiology; Council on Basic Cardiovascular Sciences; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Epidemiology and Prevention; Council on Functional Genomics and Translational Biology; and Council on Quality of Care and Outcomes Research. Role of biomarkers for the prevention, assessment, and management of heart failure: a scientific statement from the American Heart Association. Circulation. 2017;135(22):e1054-e1091. Erratum in: Circulation. 2017;136(19):e345.
-
99Mueller C, Laule-Kilian K, Scholer A, Nusbaumer C, Zeller T, Staub D, et al. B-type natriuretic peptide for acute dyspnea in patients with kidney disease: insights from a randomized comparison. Kidney Int. 2005;67(1):278-84.
-
100McLean AS, Huang SJ, Nalos M, Tang B, Stewart DE. The confounding effects of age, gender, serum creatinine, and electrolyte concentrations on plasma B-type natriuretic peptide concentrations in critically ill patients. Crit Care Med. 2003;31(11):2611-8.
-
101Redfield MM, Rodeheffer RJ, Jacobsen SJ, Mahoney DW, Bailey KR, Burnett JC Jr. Plasma brain natriuretic peptide concentration: impact of age and gender. J Am Coll Cardiol. 2002;40(5):976-82.
-
102Keyzer JM, Hoffmann JJ, Ringoir L, Nabbe KC, Widdershoven JW, Pop VJ. Age- and gender-specific brain natriuretic peptide (BNP) reference ranges in primary care. Clin Chem Lab Med. 2014;52(9):1341-6.
Edited by
Publication Dates
-
Publication in this collection
14 Oct 2019 -
Date of issue
Jul-Sep 2019
History
-
Received
03 Mar 2019 -
Accepted
25 May 2019