ABSTRACT
Objective: To map the strategies described in the literature that can be adopted by the nursing team to prevent pressure injuries in hospitalized older people.
Method: Structured scoping review according to the JBI methodology, performed on June 17, 2024. The search for documents was carried out in eight databases and in a library of theses and dissertations, with the help of the application Rayyan for selecting studies.
Results: Eleven studies were included in the review. Initial risk assessment, ongoing reassessment and monitoring, pressure redistribution, maintenance of skin integrity, treatment of pressure injuries, nutritional and fluid support, education and involvement of patients and families, training of the healthcare team, in addition to the implementation of standardized instruments and the use of technology, were identified as the main prevention strategies.
Conclusion: The identified prevention strategies allow the nursing team to act quickly, using integrated interventions optimized by professional training, as well as to use standardized instruments and advanced technologies.
DESCRIPTORS
Health of the Elderly; Aged; Pressure Ulcer; Nursing; Nursing Care
RESUMO
Objetivo: Mapear as estratégias descritas na literatura que podem ser adotadas pela equipe de enfermagem para a prevenção de lesões por pressão em pessoas idosas hospitalizadas.
Método: Revisão de escopo estruturada conforme a metodologia do JBI, realizada em 17 de junho de 2024. A busca dos documentos foi realizada em oito bases de dados e em uma biblioteca de teses e dissertações, com auxílio do aplicativo Rayyan para a seleção dos estudos.
Resultados: Foram incluídos 11 estudos na revisão. A avaliação inicial de risco, a reavaliação contínua e o monitoramento, a redistribuição da pressão, a manutenção da integridade da pele, o tratamento de lesões por pressão, o suporte nutricional e hídrico, a educação e o envolvimento de pacientes e familiares, a capacitação da equipe de saúde, além da implementação de instrumentos padronizados e do uso de tecnologia, foram identificados como as principais estratégias de prevenção.
Conclusão: As estratégias de prevenção identificadas permitem à equipe de enfermagem agir de forma rápida, utilizando intervenções integradas que são otimizadas pela capacitação dos profissionais, bem como pelo uso de instrumentos padronizados e tecnologias avançadas.
DESCRITORES
Saúde do Idoso; Idoso; Úlcera por Pressão; Enfermagem; Cuidados de Enfermagem
RESUMEN
Objetivo: Mapear las estrategias descritas en la literatura que pueden ser adoptadas por el equipo de enfermería para prevenir lesiones por presión en ancianos hospitalizados.
Método: Revisión de alcance estructurada según la metodología JBI, realizada el 17 de junio de 2024. La búsqueda de documentos se realizó en ocho bases de datos y en una biblioteca de tesis y disertaciones, con ayuda de la aplicación Rayyan para la selección de estudios.
Resultados: Se incluyeron once estudios en la revisión. La evaluación inicial del riesgo, la reevaluación continua y el seguimiento, la redistribución de la presión, el mantenimiento de la integridad de la piel, el tratamiento de las lesiones por presión, el soporte nutricional y de líquidos, la educación y la participación de los pacientes y las familias, la capacitación del equipo de atención médica, además de la implementación de instrumentos estandarizados y el uso de tecnología, se identificaron como las principales estrategias de prevención.
Conclusión: Las estrategias de prevención identificadas permiten al equipo de enfermería actuar con rapidez, utilizando intervenciones integradas y optimizadas por la formación profesional, así como el uso de instrumentos estandarizados y tecnologías avanzadas.
DESCRIPTORES
Salud del Anciano; Anciano; Úlcera por Presión; Enfermería; Atención de Enfermería
INTRODUCTION
A Pressure Ulcer (PU) is a localized damage to the skin or underlying tissues, usually over bony prominences or associated with medical devices, resulting from prolonged pressure alone or combined with shear, influenced by intrinsic and extrinsic factors that compromise tissue resistance(1). The overall prevalence is 12.8%, with stages I (43.5%) and II (28.0%) predominating, and the most affected sites are the sacrum (37.3%), heels (29.5%) and hip (7.8%)(2). Sustained pressure on these areas leads to ischemia and tissue necrosis; friction, shear, and moisture aggravate the process, favoring skin rupture(3).
The risk is greater in people with reduced mobility or sensitivity, such as bedridden or wheelchair-bound patients, especially in the older population, whose skin shows changes related to aging(4). The forecast of 2.1 billion people aged 60 and over by 2050 highlights the magnitude of this challenge and the need for effective preventive policies and practices(5,6,7). In the hospital environment, PU prevention is a shared responsibility, with emphasis on the role of nurses in direct care. However, knowledge and skills limitations still compromise preventive practice, reinforcing the need for professional development(8). Evidence-based practice is essential for safe and effective clinical decisions, but faces barriers such as training gaps and difficulties in incorporating recommendations(9).
Despite campaigns and technological advances, the incidence and impact of PUs in hospitalized older people remain alarming, with few significant advances in recent decades. This scenario highlights the urgent need to intensify efforts to raise awareness, prevent and treat these injuries, as well as greater investment in research and clinical practice to develop more effective strategies(10).
In Brazil, regulations such as the Nursing Professional Practice Law (Law No. 7,498/1986), COFEN Resolution No. 564/2017, and the National Patient Safety Program (PNSP), established by Ministry of Health Ordinance No. 529/2013, establish clear guidelines for the work of nurses in the prevention and treatment of PUs. These standards reinforce the importance of safe and qualified practices to ensure the safety and quality of care for hospitalized older people(11,12,13).
Despite these regulations and the mandatory Patient Safety Centers (NSP), Brazil faces significant challenges in preventing PU. Between 2014 and 2022, PUs accounted for 20.3% of adverse event notifications in the National Health Surveillance System (SNVS), totaling 223,378 cases. This number places PUs as the second most frequent type of adverse event in the country. During this period, 26,735 “never events” were reported, of which 72.21% were related to stage 3 PUs and 21.57% to stage 4 PUs, with 65 deaths directly attributed to these injuries(14).
These data show that, despite regulatory efforts, regional inequalities, insufficient resources and gaps in professional training persist. Many hospital services have inadequate infrastructure, including a lack of pressure redistribution mattresses and essential devices, which compromises preventive practices. Furthermore, socioeconomic disparities and increased demand for hospitalizations among older adults are straining the health system, hindering the implementation of evidence- based strategies(14).
To ensure the originality of this review, a search was carried out in the scientific literature, covering several databases. Although there are global guidelines and systematic reviews on PU prevention, these recommendations are broad and aimed at multidisciplinary teams or long-term care facilities. However, there are no reviews focused exclusively on nursing performance in the hospital context.
Therefore, this review seeks to map the strategies adopted by nursing and identify the most relevant preventive practices for this scenario. The selection of a scoping review allows for a comprehensive view, highlighting not only the consolidated evidence, but also the gaps in the literature on nursing’s role in preventing PU in hospitalized older people.
The relevance of this study lies in the systematization of preventive strategies for hospitalized older people, a particularly vulnerable group, with the potential to improve clinical practices and ensure more effective care. Furthermore, by mapping the studies carried out by nursing, the role of this profession in the production of knowledge and the implementation of preventive interventions is reinforced. As a protagonist in the continuum of care, nursing can use this evidence to foster training, influence institutional policies, and strengthen its autonomy in preventing PU. Therefore, this scoping review aims at mapping the strategies described in the literature that can be adopted by the nursing team to prevent pressure ulcers in hospitalized older people.
METHOD
Design of the Study
This is a scoping review conducted according to the JBI methodology for this type of study(15), following the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 (PRISMA 2020)(16). The review protocol was registered in the Open Science Framework (OSF) under the Digital Object Identifier (DOI): 10.17605/OSF.IO/WRVZ5. All methodological modifications made during the development of the protocol were documented in this version.
Review Research Question
To formulate the research question, the PCC (Population, Concept and Context) strategy was used: Population (hospitalized older people), Concept (PU prevention strategies) and Context (nursing care for hospitalized older people). Thus, the question was formulated as follows: “What strategies described in the literature can be adopted by the nursing team to prevent PUs in hospitalized older people?”
Eligibility Criteria
The inclusion and exclusion criteria were established based on the PCC method (Population, Concept and Context)(15). The target population included hospitalized older people, excluding studies that addressed other age groups. The concept focused on PU prevention strategies, while studies that did not address this topic in elderly people were excluded. The context considered nursing care for hospitalized older people. Various sources of evidence were included, without restrictions on language, time frame or country of origin, including articles, dissertations and theses. Methodological studies for translation or validation of instruments, theoretical essays, and editorials were excluded.
Research Strategy
To develop the search strategy for this scoping review, a preliminary search was carried out in the PubMed® and Web of Science™ databases, using Medline medical subject headings (MeSH), Health Sciences descriptors (DeCS), and the Emtree thesaurus. Reading the titles and abstracts of the texts found in this preliminary research allowed the identification of other keywords and synonymous terms, with the aim of expanding the search results and obtaining a more sensitive strategy for the second phase of data selection.
Thus, the databases included: PubMed® (National Library of Medicine, NLM); Web of Science™ Core Collection (Clarivate Analytics); Scopus® (Elsevier); and Embase® (Elsevier). The databases Nursing Database (BDENF), Latin American and Caribbean Literature on Health Sciences Information (LILACS) and Bibliographical Index Spanish in Health Sciences (IBECS) were accessed through the Virtual Health Library (VHL). To include gray literature studies, the Brazilian Digital Library of Theses and Dissertations (BDTD) of the Coordination for the Improvement of Higher Education Personnel (CAPES) was also used.
The terms related to the PCC acronym were adapted for each data platform, taking into account the variations and Boolean operators (AND and OR) to develop the final strategies, presented in Chart 1.
Construction syntax, descriptors/keywords and Boolean operators used in databases – Teresina, PI, Brazil, 2024.
The searches were carried out on June 17, 2024, using remote access to databases through the journal portal of the Coordination for the Improvement of Higher Education Personnel (CAPES), accessed via the Federated Academic Community (CAFe) with the login of the Universidade Federal do Piauí (UFPI).
Evidence Source Selection
The selection of material related to the theme took place with the help of the reference management system Rayyan CQRI Systems(17). Initially, files containing the literature found in each information source were exported to the system. Two reviewers independently excluded duplicate material. They then proceeded to read the summaries of the remaining texts, assigning acceptance or rejection concepts according to the established inclusion and exclusion criteria. The process was conducted blindly, using the resource blind on made available by the system, and any discrepancies between reviewers were resolved by a third reviewer.
After this stage, the selected texts were read in full and evaluated according to the inclusion and exclusion criteria. The accepted texts were used for data extraction. The results of this process were organized in a diagram that presents the phases of identification, screening, inclusion, and selection of texts for review.
Data Extraction
Data extraction for inclusion in this review was performed based on the list of references generated in Rayyan, which was exported to a Microsoft Excel spreadsheet. Subsequently, the three reviewers completed the spreadsheet independently, following a form designed specifically for this stage, with the aim of meeting the purpose and question of the review. During the protocol phase, a draft table was developed and tested to record the main information. This draft was refined throughout the review phase and resulted in the final version, which included the following data extracted from each source: source of information, author(s), title, type, method, country, language, descriptors/keywords, and PU prevention strategies in older adults implemented by the nursing team.
Presentation of Results
The findings were summarized using the data reduction method, through critical reading and classification of the results into conceptual categories(18). The results were presented in figures and charts. The first chart detailed the descriptive information of the studies, including the source of information, author(s), title, type, method, country, language and descriptors/keywords. The second chart summarized the PU prevention strategies in hospitalized older people that can be applied by the nursing team.
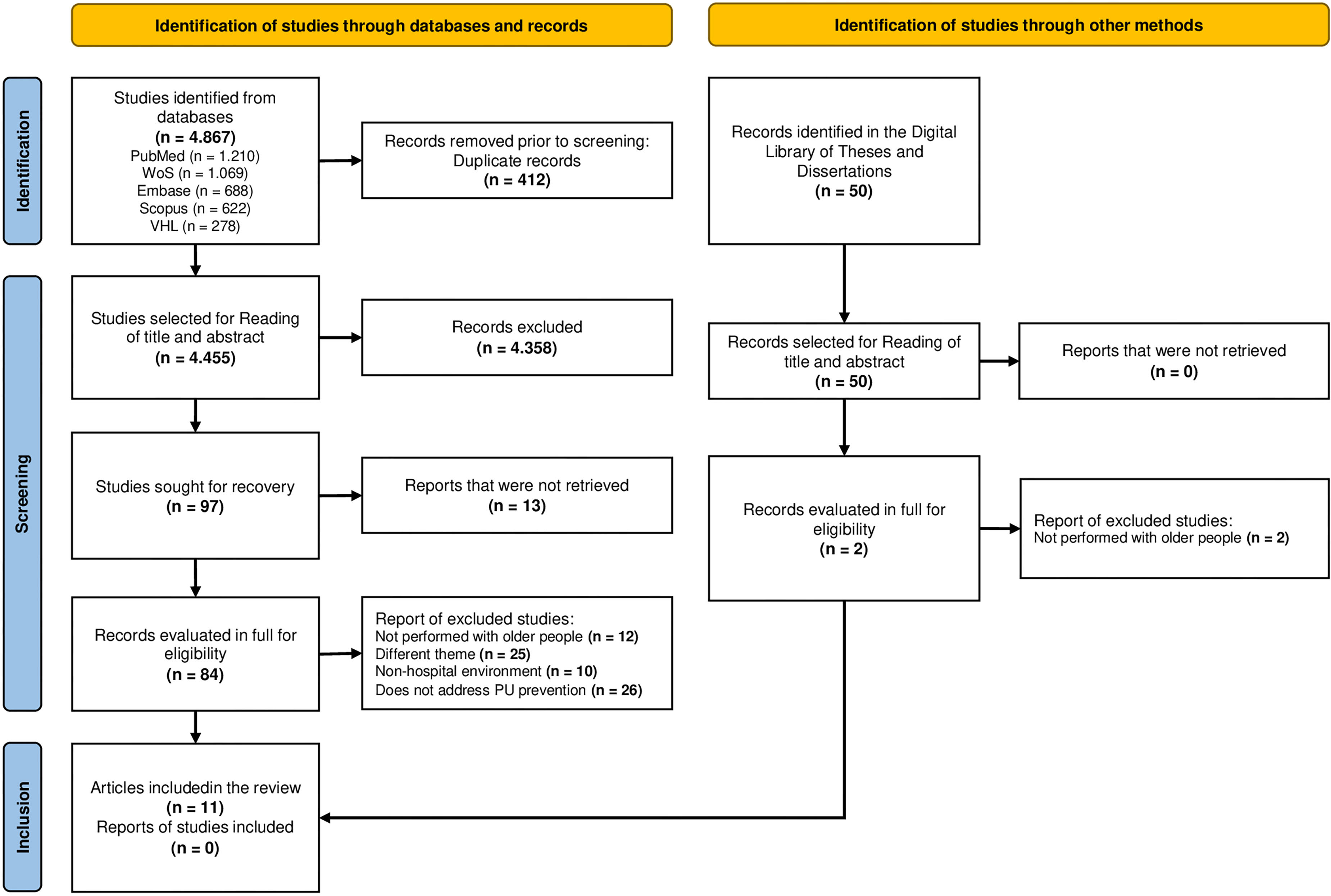
Figure 1 presents the process of identifying, screening, and including articles. Figure 2, a circular diagram, organizes the PU prevention strategies in hospitalized older adults identified in the review. Unlike a hierarchy, the diagram displays strategies interdependently, with interventions positioned in segments that highlight their complementarity and equal relevance. This format favors an integrated visualization of actions, highlighting the contribution of each strategy to the effective prevention of PU in the context of hospitalized older people.
Flowchart of the process of identification, screening, and inclusion of articles – Teresina, PI, Brazil, 2024.
Circular diagram of pressure injury prevention strategies in older people carried out by the nursing team – Teresina, PI, Brazil, 2024.
The discussion was based on selected literature and other scientific studies related to the topic. Furthermore, documents from entities that promote the creation and dissemination of evidence-based guidelines were used, with the aim of educating and training health professionals, in addition to developing policies aimed at improving the prevention and treatment of PUs.
Ethical Aspects
As this was a scoping review without the direct involvement of human participants, there was no need for submission to the Research Ethics Committee, as per JBI guidelines. All stages were conducted in accordance with the ethical principles applicable to research, ensuring transparency, methodological rigor, and scientific integrity. Copyright and correct citation of sources were respected, ensuring the reproducibility and reliability of the findings.
RESULTS
The search strategies identified a total of 4,867 publications. After removing 412 duplicates, 4,455 studies remained for screening titles and abstracts. Of these, 97 were selected for full reading. During this phase, 13 studies could not be retrieved, resulting in 84 articles that were read in full. After a thorough analysis, 73 articles were excluded, and 11 studies remained to compose this review. All reasons for exclusion were documented to create a report of those excluded for later presentation. It is important to highlight that it was not possible to identify additional studies using other methods, thus not adding further evidence to the present review (Figure 1).
From the analysis of the 11 studies included, it was found that the journal with the largest number of publications on the topic was International Wound Journal, with two publications (18.18%). Furthermore, the studies were carried out by 36 different authors. The years with the highest number of publications were 2021, 2019 and 2015, each with two publications (18.18%), while the other years recorded one publication (9.09%) each. Regarding typology, it was found that all the studies analyzed were scientific articles, nine of which were field studies (81.82%). The most used method was the quasi-experimental method, present in three studies (27.27%). Furthermore, China was the most representative country of origin, with three studies (27.27%).
Regarding language, most texts were available in English (72.73%). Finally, the keywords highlighted strategies for preventing and treating PU in older adults, emphasizing the importance of continuous nursing care, nutritional therapy, and the use of technology for real-time feedback. This information is detailed in Chart 2.
The analysis of strategies for preventing PU in hospitalized older people revealed 10 important approaches that can be carried out by the nursing team: initial risk assessment; continuous reassessment and monitoring; pressure redistribution; maintenance of skin integrity; PU treatment, nutritional and fluid support; education and involvement of patients and families; training of the health team, implementation of standardized instruments and use of technology (Chart 3).
Strategies for preventing pressure ulcers in older adults that can be performed by the nursing team – Teresina, PI, Brazil, 2024.
To facilitate understanding of PU prevention strategies in hospitalized older adults, interventions were organized into a circular model presenting four interrelated areas, each representing fundamental aspects of the care required (Figure 2).
The “Risk Assessment and Identification” area represents the foundation of preventive interventions. It includes initial risk assessment, which is essential for identifying vulnerable patients, and ongoing reassessment, which allows monitoring the patient’s condition over time.
Next, the “Direct Practical Interventions” area encompasses specific actions, such as pressure redistribution, maintaining skin integrity and treating existing lesions. These practices aim to prevent the emergence of new lesions and minimize damage to the existing ones.
The “Additional Support and Training” area highlights the importance of providing nutritional and water support, promoting education and involvement of patients and families, and training the healthcare team. These measures increase the effectiveness of preventive interventions and strengthen collaborative care.
Finally, the “Instruments and Technology” area brings together the most advanced elements of care, including the implementation of standardized instruments and the use of technologies to improve the efficiency and accuracy of preventive interventions.
DISCUSSION
The findings of this study allowed grouping the PU prevention strategies adopted by the nursing team in hospitalized older people into ten categories. These recommendations are aligned with international guidelines of Prevention and Treatment of Pressure Ulcers/Injuries: Quick Reference Guide 2019, which, although general, guide the adaptation of preventive practices to the hospital context and the older population(30).
Systematic skin assessment is an essential measure for prevention. The literature recommends a holistic inspection, from head to toe, with special attention to bony prominences and areas under devices, to identify early signs of injury. This assessment should be periodic and consider support surfaces, skin integrity, mobility, comfort and activity level, to support appropriate interventions(31).
Evidence indicates that predictive nursing interventions are more effective than conventional approaches in preventing PU in older people bedridden for long periods, increasing patient satisfaction and presenting high viability(19). The Braden (1987) and Norton (1962) scales are widely used tools to stratify the risk of PU, by analyzing factors such as mobility, moisture, sensitivity, nutrition and friction, favoring the implementation of targeted preventive measures(32,33).
Periodic reassessment and continuous monitoring enhance these results. One of the included studies showed that the use of a boot with a heel suspension device in patients over 70 years of age reduced the incidence of PU when the risk was assessed from pre-hospital care to discharge, ensuring continuity of care(27).
Thus, the initial assessment, reassessment and monitoring strategies, included in the “Risk Assessment and Identification” category, are low-cost, widely applicable and highly effective for the early identification of risk factors and the timely triggering of preventive interventions.
Pressure redistribution, through changing position and using support surfaces, is an essential strategy for preventing PU. A systematic review, however, points to a lack of consensus regarding the ideal repositioning intervals, varying between 2, 3, 4 and 6 hours(34). Thus, the guidelines of the Wound Ostomy & Continence Nurses Society recommend adjusting the frequency of repositioning to clinical conditions and individual needs, setting this care as standard(35).
Support surfaces help relieve pressure on vulnerable areas and can be classified as systemic and local. The former include high-specification mattresses, reactive or alternating pressure air mattresses, and other advanced devices, widely used to protect areas such as the sacrococcygeal region, which are more susceptible to developing PU. Local surfaces, such as gel or air cushions, are adapted to anatomical specificities. Older devices such as water mattresses and pads are not recommended due to their limited effectiveness and the risks associated with improper use(30,36).
Although older studies already highlighted the importance of pressure redistribution(29), current guidelines reinforce updated practices, such as the 30° lateral position and the use of heel suspension devices, combined with individualized plans that balance risk, comfort and advanced technologies(29,30).
Maintaining skin integrity is another central component. In environments with a high prevalence of cutaneous xerosis, incontinence-associated dermatitis, lacerations, and intertrigo, frequent inspections and maintenance of dry skin are essential measures. Evidence shows that structured care programs, including gentle cleansers and products, leave-on, are effective in preventing harm, especially in older people and pediatric patients(37).
In one of the studies analyzed, the use of specific diagnoses and care plans for older adults contributed to prevention and improved quality of care, with interventions focused on hygiene, incontinence management, skin and nutrition monitoring, positioning and monitoring of pressure on vulnerable areas(21).
Although the focus is on prevention, treatment of PU is an integral part of care. It includes proper cleaning, use of dressings and therapeutic techniques to speed healing and prevent complications. Debridement — surgical, autolytic, enzymatic, or mechanical — is essential for removing necrotic tissue, and infection control requires the use of topical or systemic antimicrobials, keeping the wound clean and covered to reduce risks and promote healing(38).
A study showed that continuous nursing care reduced complications and increased satisfaction among hospitalized elderly patients, integrating prevention, treatment, and physical and psychological support, with the active participation of patients and family members(20).
In the circular diagram, strategies for redistributing pressure, maintaining skin integrity, and treating PUs make up the “Direct Practical Interventions” area, which are essential for preventing new injuries and promoting the recovery of existing ones through specialized care.
Within the scope of the “Additional Support and Training” area, adequate nutrition and hydration are essential components for PU prevention and healing. The nursing team must monitor nutritional status and encourage water intake, as malnutrition and dehydration increase morbidity and mortality and compromise healing. Unplanned weight loss and low fluid intake are risk factors that require early identification and timely management(39).
Current guidelines recommend a multidisciplinary approach to PUs management(30). Nutritionists and dietitians adjust the diet and recommend protein supplements according to individual needs, optimizing nutritional status and promoting prevention and healing(40). However, evidence regarding the effectiveness of specific nutritional compositions is still scarce(41). A cross-sectional, multicenter study with patients ≥70 years old at risk of PU showed that the nutritional care provided falls short of what is recommended: nutritional screening, referral to a nutritionist, and protein supplementation are infrequent practices in routine care(23).
Involving patients and family members in the care plan is another pillar of this area, including guidance on warning signs and preventive measures. This strategy, however, is rarely implemented due to the lack of adequate educational materials; when available, they are often incomplete, neglecting guidelines for caregivers and visual aids(42). One of the studies analyzed reinforces the importance of integrating PU prevention into the overall care of hospitalized older individuals, highlighting the role of interdisciplinary geriatric assessment teams(28).
Staff training is crucial for patient education and quality of care. Continuing education programs, whether in-person or distance learning, must be structured, supervised, and use active methodologies, such as simulation and online teaching. Evidence indicates that training lasting between 45 minutes and two hours, even in e-learning format, is effective in improving early risk identification and the implementation of preventive measures(43,44,45).
In a retrospective study conducted at the Second Affiliated Hospital of Wenzhou Medical University, 103 hospitalized older individuals were assisted by newly trained nurses on the causes, prevention, and treatment of PU. Comprehensive care significantly reduced the risk of PU, improved patients’ psychological status and quality of life, and increased comfort during hospitalization(22).
In the circular model, nutritional and water support strategies, associated with the education and engagement of patients and families, make up the “Additional Support and Training” area. These measures are essential for preventing PU in hospitalized older individuals, a population especially susceptible to malnutrition and dehydration, and require comprehensive, interdisciplinary, and continuous care.
In the “Instruments and Technology” area of the circular diagram, the implementation of structured protocols is a central axis for the prevention of PU. Strict adherence to well-defined protocols improves the quality of care and significantly reduces the incidence of these injuries. Specific programs enhance their effectiveness by ensuring comprehensive and continuous patient care(46). In this process, nursing plays a central role in applying, monitoring and adjusting measures, adapting them to individual needs(47).
The review identified essential tools for PU prevention. THE SSKIN Care Bundle is a comprehensive approach based on five pillars: adequate support surfaces, regular skin monitoring, moisture management, nutrition, and patient movement. The Malnutrition Universal Screening Tool (MUST) assesses the risk of malnutrition through factors such as Body mass index (BMI), recent weight loss, and impact of disease on nutritional status. The Safety Cross or Safety Calendar is a visual strategy used in healthcare facilities to monitor adverse events and promote a safer care environment(26).
Advanced technologies have proven effective as prevention strategies. Machine learning methods for predictive models, posture recognition and image analysis contribute to early detection and continuous monitoring(48). Wearable sensors aid in adherence to repositioning protocols, reducing the incidence of PU(49). Other technologies, such as ultrasound, thermography, subepidermal moisture measurement, and laser Doppler spectroscopy, overcome the limitations of traditional visual inspection, enabling a more accurate and proactive approach(50).
Despite these advances, technological implementation in hospitals, especially in developing countries, faces challenges: lack of infrastructure, high costs, the need for ongoing training, budgetary impact, unequal access, and dependence on imported equipment. Such factors reinforce the importance of strategies adapted to local reality, seeking accessibility and sustainability(51).
One study included in this review evaluated the use of Continuous Bedside Pressure Mapping (CBPM) in an orthopedic rehabilitation unit in Uppsala, Sweden, with patients over 65 years of age. CBPM uses a mat with pressure sensors connected to a monitor, which indicates areas of highest pressure in red. This real-time visualization provided feedback to staff and patients, encouraging positional change and promoting self-care. After the intervention, there was an improvement in patients’ knowledge about risk factors and PU prevention, with greater engagement in preventive measures(24).
In the circular model, the implementation of standardized instruments and the use of technologies make up the “Instruments and Technology” area. These strategies require more resources and involve more complex interventions than direct management actions, but they structure and qualify care practices, providing support to other areas, strengthening secondary and tertiary prevention, and contributing to reducing harm to hospitalized older people.
Despite evidence of the effectiveness of targeted interventions, the global prevalence of pressure injuries remains high. This paradox stems from structural and organizational barriers, such as a shortage of human and material resources, low adherence to guidelines, knowledge and skills gaps, a lack of a consolidated safety culture, and practical difficulties in incorporating recommendations into routine care. Even in hospitals with structured systems, a recent study shows that the implementation of guidelines is hampered by these factors, reinforcing that isolated measures are insufficient without institutional changes and consistent policies(52).
A limitation of this review is the lack of formal assessment of the methodological quality of the studies included, which may affect the robustness of the conclusions. This limitation was mitigated by a comprehensive analysis of the scientific literature and by consulting recommendations from specialized bodies. Although scoping reviews do not usually perform a critical evaluation of studies, we sought to base the strategies presented on the specificities of hospitalization of older people, with recommendations more applicable to the clinical context.
This study contributes to nursing practice by identifying evidence that guides the implementation of systematized strategies for the prevention of PU. The need for continuous training of the team is emphasized, as well as the rational use of technologies for risk monitoring and evaluation of interventions, promoting greater safety and quality of care. In the hospital context, these strategies must be adapted to the available resources and infrastructure, especially in scenarios with technological and professional training limitations. Therefore, integrating these actions into institutional protocols, investing in continuing education, and using emerging technologies judiciously are essential measures to consolidate PU prevention as a safe and effective care standard.
Finally, the findings of this review are in line with the international literature, which emphasizes the need to expand nursing research on PU prevention, reinforcing the importance of evidence-based practices to adequately serve this vulnerable population(53).
CONCLUSION
The PU prevention strategies mapped in the review were organized into four areas: risk assessment and identification, direct practical interventions, additional support and training, and tools and technology. These strategies allow the nursing team to act quickly and efficiently, employing integrated interventions, optimized by professional training and the use of standardized instruments and advanced technologies.
These approaches have direct implications for care of older people. Early assessment identifies risks and enables immediate action. Practical interventions, such as pressure redistribution and skin care, prevent the development of lesions. Additional support, including nutrition, education, and staff training, enhances the quality of care. The use of standardized instruments and advanced technologies facilitates both the implementation and monitoring of preventive practices. When applied in an integrated manner, these strategies ensure quality care, reduce the risk of PU, and promote comprehensive and specific care for hospitalized older individuals.
Intervention studies exploring different strategies are recommended, with a special focus on implementing advanced technologies and rigorous protocols. These studies can strengthen the effectiveness of preventive practices and promote improvements in the quality of care provided to this vulnerable population.
DATA AVAILABILITY
The entire dataset that supports the findings of this study was published within the article itself.
REFERENCES
-
1. Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised national pressure ulcer advisory panel pressure injury staging system: revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585–97. doi: http://doi.org/10.1097/WON.0000000000000281. PubMed PMID: 27749790.
» https://doi.org/10.1097/WON.0000000000000281 -
2. Li Z, Lin F, Thalib L, Chaboyer W. Global prevalence and incidence of pressure injuries in hospitalised adult patients: a systematic review and meta-analysis. Int J Nurs Stud. 2020;105:103546. doi: http://doi.org/10.1016/j.ijnurstu.2020.103546. PubMed PMID: 32113142.
» https://doi.org/10.1016/j.ijnurstu.2020.103546 -
3. Mervis JS, Phillips TJ. Pressure ulcers: Pathophysiology, epidemiology, risk factors, and presentation. J Am Acad Dermatol. 2019;81(4): 881–90. doi: http://doi.org/10.1016/j.jaad.2018.12.069. PubMed PMID: 30664905.
» https://doi.org/10.1016/j.jaad.2018.12.069 - 4. Mondragon N, Zito PM. Pressure injury. Treasure Island: StatPearls Publishing; 2024. PubMed PMID: 32491791.
-
5. Jiang Q, Chen K, Liu Y, Zhou J, Bai Y, Zhao J, et al. Relationship between dry skin and pressure injury in older patients: A multicentre cross-sectional survey in China. Int Wound J. 2023;20(5):1402–17. doi: http://doi.org/10.1111/iwj.13993. PubMed PMID: 36307094.
» https://doi.org/10.1111/iwj.13993 -
6. Roussou E, Fasoi G, Stavropoulou A, Kelesi M, Vasilopoulos G, Gerogianni G, et al. Quality of life of patients with pressure ulcers: a systematic review. Med Pharm Rep. 2023;96(2):123–30. doi: http://doi.org/10.15386/mpr-2531. PubMed PMID: 37197280.
» https://doi.org/10.15386/mpr-2531 -
7. Rudnicka E, Napierała P, Podfigurna A, Męczekalski B, Smolarczyk R, Grymowicz M. The World Health Organization (WHO) approach to healthy ageing. Maturitas. 2020;139:6–11. doi: http://doi.org/10.1016/j.maturitas.2020.05.018. PubMed PMID: 32747042.
» https://doi.org/10.1016/j.maturitas.2020.05.018 -
8. Awoke N, Tekalign T, Arba A, Lenjebo TL. Pressure injury prevention practice and associated factors among nurses at Wolaita Sodo University Teaching and Referral Hospital, South Ethiopia: a cross-sectional study. BMJ Open. 2022;12(3):e047687. doi: http://doi.org/10.1136/bmjopen-2020-047687. PubMed PMID: 35288379.
» https://doi.org/10.1136/bmjopen-2020-047687 -
9. Mohamed RA, Alhujaily M, Ahmed FA, Nouh WG, Almowafy AA. Nurses’ experiences and perspectives regarding evidence-based practice implementation in healthcare context: a qualitative study. Nurs Open. 2024;11(1):e2080. doi: http://doi.org/10.1002/nop2.2080. PubMed PMID: 38268296.
» https://doi.org/10.1002/nop2.2080 - 10. Siotos C, Bonett AM, Damoulakis G, Becerra AZ, Kokosis G, Hood K, et al. Burden of pressure injuries: findings from the global burden of disease study. Eplasty. 2022;22:e19. PubMed PMID: 35873067.
-
11. Brasil. Lei nº 7.498, de 25 de junho de 1986. Dispõe sobre a regulamentação do exercício da enfermagem e dá outras providências [Internet]. Diário Oficial da União; Brasília; 26 jun 1986 [cited 2024 Aug 8]. Available from: http://www.planalto.gov.br/ccivil_03/leis/l7498.htm
» http://www.planalto.gov.br/ccivil_03/leis/l7498.htm -
12. Brasil, Conselho Federal de Enfermagem – COFEN. Resolução COFEN nº 564, de 6 de novembro de 2017. Atualiza e estabelece parâmetros para o dimensionamento do quadro de profissionais de enfermagem nas instituições de saúde e assemelhados [Internet]. Diário Oficial da União; Brasília; 8 nov 2017 [cited 2024 Aug 8]. Available from: http://www.cofen.gov.br/resolucao-cofen-no-5642017_56459.html
» http://www.cofen.gov.br/resolucao-cofen-no-5642017_56459.html -
13. Brasil. Portaria GM/MS nº 529, de 1º de abril de 2013. Institui o Programa Nacional de Segurança do Paciente (PNSP) [Internet]. Diário Oficial da União; Brasília; 2 abr 2013 [cited 2024 Aug 8]. Available from: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt0529_01_04_2013.html
» https://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt0529_01_04_2013.html -
14. Brasil, Agência Nacional de Vigilância Sanitária – ANVISA. Nota Técnica GVIMS/GGTES/Anvisa nº 05/2023. Práticas de segurança do paciente em serviços de saúde: prevenção de lesão por pressão [Internet]. Brasília: ANVISA; 2023 [cited 2024 Aug 8]. Available from: https://www.gov.br/anvisa/pt-br/centraisdeconteudo/publicacoes/servicosdesaude/notas-tecnicas/notas-tecnicas-vigentes/nota-tecnica-gvims-ggtes-anvisa-no-05-2023-praticas-de-seguranca-do-paciente-em-servicos-de-saude-prevencao-de-lesao-por-pressao/view
» https://www.gov.br/anvisa/pt-br/centraisdeconteudo/publicacoes/servicosdesaude/notas-tecnicas/notas-tecnicas-vigentes/nota-tecnica-gvims-ggtes-anvisa-no-05-2023-praticas-de-seguranca-do-paciente-em-servicos-de-saude-prevencao-de-lesao-por-pressao/view -
15. Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Scoping reviews (2020). In: Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z, editores. JBI manual for evidence synthesis. Adelaide: JBI; 2024. doi: http://doi.org/10.46658/JBIMES-24-09.
» https://doi.org/10.46658/JBIMES-24-09 - 16. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. PubMed PMID: 33782057.
-
17. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan: a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: http://doi.org/10.1186/s13643-016-0384-4. PubMed PMID: 27919275.
» https://doi.org/10.1186/s13643-016-0384-4 -
18. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53. doi: http://doi.org/10.1111/j.1365-2648.2005.03621.x. PubMed PMID: 16268861.
» https://doi.org/10.1111/j.1365-2648.2005.03621.x -
19. Deng GL, Lei YL, Tan H, Geng BC, Liu Z. Effects of predictive nursing interventions on pressure ulcer in elderly bedridden patients. Int Wound J. 2024;21(3):e14690. doi: http://doi.org/10.1111/iwj.14690. PubMed PMID: 38453139.
» https://doi.org/10.1111/iwj.14690 - 20. Xiao F, Peng H, Li Y. The preventive effect of seamless nursing care on pressure ulcer and related complications in elderly inpatients. Am J Transl Res. 2021;13(4):3515–21. PubMed PMID: 34017530.
-
21. Morrudo Garcia EQ, Tarouco da Silva B, Gautério Abreu DP, Roque TDS, Dos Santos Sousa JI, Ilha S. Nursing diagnosis in older adults at risk for pressure injury. Rev Esc Enferm USP. 2021;55:e20200549. doi: http://doi.org/10.1590/1980-220x-reeusp-2020-0549. PubMed PMID: 34423807.
» https://doi.org/10.1590/1980-220x-reeusp-2020-0549 - 22. Yu Y, Chen J, Sha F. Analysis of the effect of comprehensive nursing on pressure ulcers risk and psychological state in severe elderly patients. Int J Clin Exp Med. 2020;13(11):9065-72.
-
23. Eglseer D, Hödl M, Lohrmann C. Nutritional management of older hospitalised patients with pressure injuries. Int Wound J. 2019;16(1):226–32. doi: http://doi.org/10.1111/iwj.13016. PubMed PMID: 30440105.
» https://doi.org/10.1111/iwj.13016 -
24. Hultin L, Karlsson AC, Öhrvall M, Gunningberg L. Information and communication technology can increase patient participation in pressure injury prevention: a qualitative study in older orthopedic patients. J Wound Ostomy Continence Nurs. 2019;46(5):383–9. doi: http://doi.org/10.1097/WON.0000000000000568. PubMed PMID: 31348431.
» https://doi.org/10.1097/WON.0000000000000568 -
25. Bååth C, Engström M, Gunningberg L, Athlin ÅM. Prevention of heel pressure ulcers among older patients--from ambulance care to hospital discharge: a multi-centre randomized controlled trial. Appl Nurs Res. 2016;30:170–5. doi: http://doi.org/10.1016/j.apnr.2015.10.003. PubMed PMID: 27091274.
» https://doi.org/10.1016/j.apnr.2015.10.003 -
26. Barry M, Nugent L. Pressure ulcer prevention in frail older people. Nurs Stand. 2015;30(16):50–8, quiz 60. doi: http://doi.org/10.7748/ns.30.16.50.s46. PubMed PMID: 26669407.
» https://doi.org/10.7748/ns.30.16.50.s46 -
27. Sousa JERB, Silva GRF, Luz MHBA, Pereira MLL. Concepciones teóricas de Neuman asociadas con la prevención de las úlceras por presión: un estudio de caso. Index Enferm. 2015;24(4):222–6. doi: http://doi.org/10.4321/S1132-12962015000300007.
» https://doi.org/10.4321/S1132-12962015000300007 -
28. Stotts NA, Wu HS. Hospital recovery is facilitated by prevention of pressure ulcers in older adults. Crit Care Nurs Clin North Am. 2007;19(3): 269–75, vi. doi: http://doi.org/10.1016/j.ccell.2007.05.005. PubMed PMID: 17697948.
» https://doi.org/10.1016/j.ccell.2007.05.005 -
29. Maklebust J. Pressure ulcers: decreasing the risk for older adults. Geriatr Nurs. 1997;18(6):250–4. doi: http://doi.org/10.1016/S0197-4572(97)90356-6. PubMed PMID: 9469056.
» https://doi.org/10.1016/S0197-4572(97)90356-6 -
30. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel, Pan Pacific Pressure Injury Alliance. Prevention and treatment of pressure ulcers/injuries: quick reference guide [Internet]. London: EPUAP/NPIAP/PPPIA; 2019 [cited 2024 Aug 8]. Available from: https://static1.squarespace.com/static/6479484083027f25a6246fcb/t/647dc6c178b260694b5c9365/1685964483662/Quick_Reference_Guide-10Mar2019.pdf
» https://static1.squarespace.com/static/6479484083027f25a6246fcb/t/647dc6c178b260694b5c9365/1685964483662/Quick_Reference_Guide-10Mar2019.pdf -
31. Alderden JG, Shibily F, Cowan L. Best practice in pressure injury prevention among critical care patients. Crit Care Nurs Clin North Am. 2020;32(4):489–500. doi: http://doi.org/10.1016/j.cnc.2020.08.001. PubMed PMID: 33129409.
» https://doi.org/10.1016/j.cnc.2020.08.001 -
32. Braden B, Bergstrom N. A conceptual schema for the study of the etiology of pressure sores. Rehabil Nurs. 1987;12(1):8–12. doi: http://doi.org/10.1002/j.2048-7940.1987.tb00541.x. PubMed PMID: 3643620.
» https://doi.org/10.1002/j.2048-7940.1987.tb00541.x - 33. Norton D, McLaren R, Exton-Smith AN. An investigation of geriatric nursing problems in hospital. London: National Corporation for the Care of Old People; 1962.
-
34. Asiri S. Turning and repositioning frequency to prevent hospital-acquired pressure injuries among adult patients: systematic review. Inquiry. 2023;60:469580231215209. doi: http://doi.org/10.1177/00469580231215209. PubMed PMID: 38050921.
» https://doi.org/10.1177/00469580231215209 -
35. Wound, Ostomy and Continence Nurses Society, Wound Guidelines Task Force. WOCN 2016 guideline for prevention and management of pressure injuries (ulcers): an executive summary. J Wound Ostomy Continence Nurs. 2017;44(3):241–6. doi: http://doi.org/10.1097/WON.0000000000000321. PubMed PMID: 28472816.
» https://doi.org/10.1097/WON.0000000000000321 -
36. Huang L, Yan Y, Huang Y, Liao Y, Li W, Gu C, et al. Summary of best evidence for prevention and control of pressure ulcer on support surfaces. Int Wound J. 2023;20(6):2276–85. doi: http://doi.org/10.1111/iwj.14109. PubMed PMID: 36891753.
» https://doi.org/10.1111/iwj.14109 -
37. Fastner A, Hauss A, Kottner J. Skin assessments and interventions for maintaining skin integrity in nursing practice: an umbrella review. Int J Nurs Stud. 2023;143:104495. doi: http://doi.org/10.1016/j.ijnurstu.2023.104495. PubMed PMID: 37099847.
» https://doi.org/10.1016/j.ijnurstu.2023.104495 - 38. Al Aboud AM, Manna B. Wound pressure injury management. Treasure Island: StatPearls Publishing; 2024. PubMed PMID: 30422492.
-
39. Mahmoodpoor A, Shadvar K, Saghaleini S, Dehghan K, Ostadi Z. Pressure ulcer and nutrition. Indian J Crit Care Med. 2018;22(4):283–9. doi: http://doi.org/10.4103/ijccm.IJCCM_277_17. PubMed PMID: 29743767.
» https://doi.org/10.4103/ijccm.IJCCM_277_17 -
40. Munoz N, Posthauer ME. Nutrition strategies for pressure injury management: Implementing the 2019 International Clinical Practice Guideline. Nutr Clin Pract. 2022;37(3):567–82. doi: http://doi.org/10.1002/ncp.10762. PubMed PMID: 34462964.
» https://doi.org/10.1002/ncp.10762 - 41. Langer G, Wan CS, Fink A, Schwingshackl L, Schoberer D. Nutritional interventions for preventing and treating pressure ulcers. Cochrane Database Syst Rev. 2024;2(2):CD003216. PubMed PMID: 38345088.
-
42. Team V, Bouguettaya A, Richards C, Turnour L, Jones A, Teede H, et al. Patient education materials on pressure injury prevention in hospitals and health services in Victoria, Australia: availability and content analysis. Int Wound J. 2020;17(2):370–9. doi: http://doi.org/10.1111/iwj.13281. PubMed PMID: 31850664.
» https://doi.org/10.1111/iwj.13281 -
43. Tudor Car L, Soong A, Kyaw BM, Chua KL, Low-Beer N, Majeed A. Health professions digital education on clinical practice guidelines: a systematic review by Digital Health Education collaboration. BMC Med. 2019;17(1):139. doi: http://doi.org/10.1186/s12916-019-1370-1. PubMed PMID: 31315642.
» https://doi.org/10.1186/s12916-019-1370-1 -
44. Baracho VDS, Chaves MEA, Lucas TC. Application of the educational method of realistic simulation in the treatment of pressure injuries. Rev Lat Am Enfermagem. 2020;28:e3357. doi: http://doi.org/10.1590/1518-8345.3946.3357. PubMed PMID: 32901770.
» https://doi.org/10.1590/1518-8345.3946.3357 -
45. Ding Y, Qian J, Zhou Y, Zhang Y. Effect of e-learning program for improving nurse knowledge and practice towards managing pressure injuries: a systematic review and meta-analysis. Nurs Open. 2024;11(1):e2039. doi: http://doi.org/10.1002/nop2.2039. PubMed PMID: 38268243.
» https://doi.org/10.1002/nop2.2039 -
46. Lin F, Wu Z, Song B, Coyer F, Chaboyer W. The effectiveness of multicomponent pressure injury prevention programs in adult intensive care patients: a systematic review. Int J Nurs Stud. 2020;102:103483. doi: http://doi.org/10.1016/j.ijnurstu.2019.103483. PubMed PMID: 31835122.
» https://doi.org/10.1016/j.ijnurstu.2019.103483 -
47. Yilmazer T, Tuzer H. Effectiveness of a pressure injury prevention care bundle; prospective interventional study in intensive care units. J Wound Ostomy Continence Nurs. 2022;49(3):226–32. doi: http://doi.org/10.1097/WON.0000000000000875. PubMed PMID: 35523237.
» https://doi.org/10.1097/WON.0000000000000875 -
48. Jiang M, Ma Y, Guo S, Jin L, Lv L, Han L, et al. Using machine learning technologies in pressure injury management: systematic review. JMIR Med Inform. 2021;9(3):e25704. doi: http://doi.org/10.2196/25704. PubMed PMID: 33688846.
» https://doi.org/10.2196/25704 -
49. Crotty A, Killian JM, Miller A, Chilson S, Wright R. Using wearable technology to prevent pressure injuries: an integrative review. Worldviews Evid Based Nurs. 2023;20(4):351–60. doi: http://doi.org/10.1111/wvn.12638. PubMed PMID: 36938828.
» https://doi.org/10.1111/wvn.12638 -
50. Scafide KN, Narayan MC, Arundel L. Bedside technologies to enhance the early detection of pressure injuries: a systematic review. J Wound Ostomy Continence Nurs. 2020;47(2):128–36. doi: http://doi.org/10.1097/WON.0000000000000626. PubMed PMID: 32068647.
» https://doi.org/10.1097/WON.0000000000000626 -
51. Silva HP, Elias FTS. Incorporação de tecnologias nos sistemas de saúde do Canadá e do Brasil: perspectivas para avanços nos processos de avaliação. Cad Saude Publica. 2019;35(Suppl 2):e00071518. doi: http://doi.org/10.1590/0102-311x00071518. PubMed PMID: 31432894.
» https://doi.org/10.1590/0102-311x00071518 -
52. Wan CS, Musgrave-Takeda MM, Gillespie B, Tobiano G, McInnes E. Barriers and facilitators to implementing pressure injury guidelines for nutrition assessment and alternating pressure air mattress allocation: a qualitative study. J Adv Nurs. 2025;81(10):6767. doi: http://doi.org/10.1111/jan.16820. PubMed PMID: 39936558.
» https://doi.org/10.1111/jan.16820 -
53. Azizoğlu F, Terzi B. Research topics on pressure injury prevention and measurement tools from 1997 to 2023: a bibliometric analysis using VOSviewer. Intensive Crit Care Nurs. 2024;80:103557. doi: http://doi.org/10.1016/j.iccn.2023.103557. PubMed PMID: 37804817.
» https://doi.org/10.1016/j.iccn.2023.103557
Publication Dates
-
Publication in this collection
21 Nov 2025 -
Date of issue
2025
History
-
Received
30 Oct 2024 -
Accepted
18 Sept 2025

 Strategies adopted by the nursing team for the prevention of pressure ulcers in hospitalized older people: a scoping review
Strategies adopted by the nursing team for the prevention of pressure ulcers in hospitalized older people: a scoping review


 Source: Adapted from Page et al. (2021)(
Source: Adapted from Page et al. (2021)(