Abstracts
Elevated risk of fatal and non-fatal cardiovascular events is associated with high prevalence of peripheral arterial disease, with assessment through the ankle-brachial index (ABI). This study aimed to demonstrate that the ABI and the Edinburgh Claudication Questionnaire are tools to be used by nurses in prevention and/or treatment of CVD (cardiovascular disease). A cross-sectional study was carried out with patients from a cardiovascular clinic. The Edinburgh Claudication Questionnaire was applied and the ABI was measured with the formula (ABI= Blood Pressure Ankle/Blood Pressure Brachial). A total of 115 patients were included, most were females (57.4%), aged 60.6 ± 12.5 years. The most prevalent risk factors were hypertension (64.3%), physical inactivity (48.7%) and family history (58.3%). The study showed that abnormal ABI was frequently found and 42.6% of the patients with abnormal ABI showed intermittent claudication. The method to evaluate the ABI associated to the Edinburg Claudication Questionnaire, can be easily used by nurses in the clinical evaluation of asymptomatic and symptomatic CVD patients.
Peripheral arterial disease ; Ankle brachial index ; Intermittent claudication ; Risk factors ; Nursing care
El riesgo elevado de eventos cardiovasculares fatales y no fatales está asociado con la alta prevalencia de enfermedad arterial periférica, cuya evaluación puede realizarse por medio del índice tobillo-brazo (ITB). El objetivo de este estudio fue demostrar que el ITB y el Cuestionario de Claudicación de Edimburgo son herramientas que pueden ser utilizadas por las enfermeras en la prevención y tratamiento de enfermedades cardiovasculares (ECV). Se realizó un estudio transversal en pacientes de una clínica cardiovascular, aplicándose el Cuestionario de Claudicación de Edimburgo y realizándose la medición de cálculo del ITB (PAS tobillo/PAS braquial). Fueron incluidos 115 pacientes, la mayoría de sexo femenino (57,4%) con una edad media de 60,6 años ± 12,5 años. Los factores de riesgo más frecuentes fueron: la hipertensión arterial (64,3%), el sedentarismo (48,7%) y los antecedentes familiares (58,3%). El estudio demostró que el ITB alterado fue un hallazgo frecuente y el 42,6% con ITB anormal mostró claudicación intermitente. El método de evaluación del ITB asociado con el Cuestionario de Claudicación de Edimburgo, puede ser utilizado fácilmente por los enfermeros para la evaluación clínica de los pacientes sintomáticos y asintomáticos de ECV y para la prevención de eventos cardiovasculares.
Enfermedad arterial periférica ; Índice tobillo braquial ; Claudicación intermitente ; Factores de riesgo ; Atención de enfermería
O risco elevado de eventos cardiovasculares fatais e não fatais está associado à alta prevalência da doença arterial obstrutiva periférica, avaliada por meio do índice tornozelo-braquial (ITB). Objetivou-se demonstrar que o ITB e o Questionário de Claudicação de Edimburgo são ferramentas que podem ser utilizadas pelos enfermeiros na prevenção e no tratamento da doença cardiovascular (DCV). Realizou-se estudo transversal em pacientes de uma clínica cardiovascular. Aplicou-se o Questionário de Claudicação de Edimburgo e verificou-se a medida do ITB (PAS tornozelo/PAS braquial). Foram incluídos 115 pacientes, a maioria do sexo feminino (57,4%), com idade média de 60,6 ± 12,5 anos. Os fatores de risco mais prevalentes foram hipertensão arterial sistêmica (64,3%), sedentarismo (48,7%) e história familiar (58,3%). O ITB alterado foi um achado frequente e 42,6% dos pacientes com ITB anormal apresentaram claudicação intermitente. O método de avaliação do ITB, associado ao Questionário de Claudicação de Edimburgo, pode ser facilmente utilizado pelos enfermeiros para avaliação clínica de pacientes e prevenção de eventos cardiovasculares.
Doença arterial periférica ; Índice tornozelo-braço ; Claudicação intermitente ; Fatores de risco ; Cuidados de enfermagem
Introduction
Aging causes changes in the walls of blood vessels, affecting the transport of oxygen and nutrients to the tissues. These changes make vessels stiffen, resulting in increased peripheral resistance (11.Corrêa K, Ceolim MF. Qualidade do sono em pacientes idosos com patologias vasculares periféricas. Rev Esc Enferm USP. 2008;42(1):12-8).
Effective diagnostic measures of early intervention are needed to minimize the increase in cardiovascular morbidity and mortality(22.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al.; TASC II Working Goup Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg. 2007;33 Suppl 1:S1-75). A measure of great significance to evaluate the cardiovascular deficit is the Ankle-Brachial Index (ABI), an important marker of Peripheral Artery Disease (PAD) in its asymptomatic phase. Patients with PAD are five to seven times more likely to suffer acute myocardial infarction (AMI) and cerebrovascular accident (CVA), compared to a person who does not suffer from cardiovascular disease (CVD)(33.Giollo Junior LT, Martin JFV. Índice tornozelo-braquial no diagnóstico da doença aterosclerótica carotídea. Rev Bras Hipertens. 2010;17(2):117-8).
Measures of ABI between 0.90 and 1.30 are considered normal, and values above 1.30 or below 0.90 are strong predictors of atherosclerotic vascular disease due to calcification of the middle layer and therefore rigidity of vascular walls(44.Kawamura T. Índice Tornozelo-Braquial (ITB) determinado por esfigmomanômetros oscilométricos automáticos. Arq Bras Cardiol. 2008;90(5):322-6). The values of ABI and symptoms worsen with advancing age, as shown by a cohort study carried out in Rio de Janeiro, in which among 248 individuals (of the 407 surveyed with PAD), 89.9% had ABI below 0. 90(55.Panico MDB, Spichler ES, Neves MF, Pinto LW, Spichler D. Prevalência e fatores de risco da doença arterial periférica sintomática e assintomática em hospital terciário, Rio de Janeiro, Brasil. J Vasc Bras. 2009;8(2):125-32).
The risk factors for PAD are similar to CVD and include smoking, physical inactivity, diabetes mellitus, systemic arterial hypertension (SAH), obesity, advanced age and dyslipidemia(66.Savino Neto S, Nascimento JLM. Doença arterial obstrutiva periférica: novas perspectivas de fatores de risco. Rev Para Med. 2007;21(2):35-9). To assist in the early detection of PAD and hence CVD was created an assessment tool called The Edinburgh Claudication Questionnaire(77.Makdisse M, Nascimento Neto R, Chagas ACP, Brasil D, Borges JL, Borges JL, et al. Adaptação transcultural e validação do Questionário de Claudicação de Edimburgo. Arq Bras Cardiol. 2007;88(5):501-6), which aids in the differential diagnosis of peripheral vascular disease. The instrument investigates episodes of claudication, which are characterized by intense pain in areas with arterial blockage - usually the calf, thigh or buttock - because of ambulation(88.Turrini FJ, Ventura MM. Prevalência de doença arterial periférica em idosos atendidos no ambulatório de geriatria e sua correlação com fatores de risco cardiovascular. UNOPAR Cient Ciênc Biol Saúde. 2002;13(1):17-21).
In order to monitor changes in the ABI and of intermittent claudication (IC) in a general population over time, a study was carried out with 1,592 individuals followed for 12 years in the city of Edinburgh, Scotland. Among them, 695 had worsening of the ABI and IC. In addition to this worsening, another 179 new cases had IC. Subjects with abnormal ABI values in the beginning of the study were twice more likely to have fatal risks than those with normal ABI(99.Smith FB, Lee AJ, Price JF, van Wijk MC, Fowkes FG. Changes in ankle brachial index in symptomatic and asymptomatic subjects in the general population. J Vasc Surg. 2003;38(6):1323-30).
The recognition of PAD as a sensitive marker of systemic atherosclerosis and the increased risk of fatal and nonfatal cardiovascular events become decisive factors for the use of the ABI and the Edinburgh Claudication Questionnaire in clinical practice. Its results indicate the need to program changes in habits, adopting secondary prevention measures because of the high cardiovascular risk(1010.Burke GL, Arnold AM, Bild DE, Cushman M, Fried LP, Newman A, et al. Factors associated with health aging: the cardiovascular health study. J Am Geriatr Soc. 2001;49(3):254-62).
This study aimed to demonstrate that the ABI and the Edinburgh Claudication Questionnaire are tools that can be used by nurses in the prevention of CVD.
Method
This is a cross-sectional study that was carried out between January and September/2012, in a clinic specialized in cardiovascular examinations. Adults aged ≥18 years with at least one risk factor for CVD, in use of medication or not, with or without claudication were included. The following patients were excluded: Two with cognitive impairment, three with amputation of lower limb (LL) or upper limb (UL), two obese that required appropriate cuffs and one in which there was contraindication of BP measurement at the ankles by the presence of painful inflammation and phlebitis.
The study variables were related to the sociodemographic profile, the score of the Edinburgh Claudication Questionnaire, the ABI and risk factors for CVD such as hypertension, sedentary lifestyle, smoking and diabetes mellitus.
The Edinburgh Claudication Questionnaire has been culturally adapted into Brazilian Portuguese and validated through analysis of sensitivity and specificity for IC(77.Makdisse M, Nascimento Neto R, Chagas ACP, Brasil D, Borges JL, Borges JL, et al. Adaptação transcultural e validação do Questionário de Claudicação de Edimburgo. Arq Bras Cardiol. 2007;88(5):501-6). It contains six questions about discomfort, intensity, onset and location of pain in the lower limbs. The responses offer positive and negative options or another option, characterizing the presence or absence of claudication.
The study was approved by the local Ethics Research Committee under no. CEP/IC-FUC UP 4703/12. All the study participants signed an Informed Consent Form (ICF).
Logistics of the study
After the participants accepted to participate in the study and signed the informed consent form, the clinic nurses applied a sociodemographic questionnaire and the Edinburgh Claudication Questionnaire in a private room. The average time to answer the questions was 15 minutes.
In a second step, for the analysis of ABI, patients remained seated or in orthostatic position, and the circumference of the arm was measured to determine the optimal cuff. Then they were placed in supine position to start pressure measurements. The brachial artery was located and the cuff was adjusted on the brachial pulse. The measures of the left and right brachial arteries were measured according to the VI Brazilian Guidelines on hypertension(1111.Sociedade Brasileira de Cardiologia; Sociedade Brasileira de Hipertensão; Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensão. Arq Bras Cardiol. 2010;95(1 Supl.1):1-51). The highest measurement of the pressure obtained by the method was used to calculate the ABI. The sound related to blood flow velocity was detected with the aid of a Doppler. The dorsalis pedis and tibial pulses were located in the ankle, and the pressure of blood and of both lower limbs were measured according to the standards recommended by the VI Brazilian Guidelines on hypertension.
The measurements of ABI were made by the nurses in accordance with the recommended protocol(55.Panico MDB, Spichler ES, Neves MF, Pinto LW, Spichler D. Prevalência e fatores de risco da doença arterial periférica sintomática e assintomática em hospital terciário, Rio de Janeiro, Brasil. J Vasc Bras. 2009;8(2):125-32,1212.Torres AGM, Machado EG, Lopes TS, Gentile PC, Vieira AC, Soares LG, et al. Prevalência de alterações do índice tornozelo-braço em indivíduos portadores assintomáticos de doença arterial obstrutiva periférica. Rev Bras Cardiol. 2012;25(2):87-93). The portable Vascular Doppler (DV 610 Med Mega) and the premium aneroid sphygmomanometer were used. Patients were kept at rest in the supine position and the systolic blood pressure (SBP) was measured in all four limbs; the right and left pedis arteries of the lower limbs, and the right and left brachial arteries of the upper limbs. The ABI was calculated based on the highest SBP recorded in the upper and lower limbs, whether right or left. The value was obtained by dividing the highest value of SBP obtained in each artery of the lower limbs by the highest SBP value obtained in the upper limbs, according to the formula: ABI= SBP Ankle/SBP Brachial(55.Panico MDB, Spichler ES, Neves MF, Pinto LW, Spichler D. Prevalência e fatores de risco da doença arterial periférica sintomática e assintomática em hospital terciário, Rio de Janeiro, Brasil. J Vasc Bras. 2009;8(2):125-32). The reference values were: abnormal ABI < 0.90 and >1.30; normal ABI between 0.91 and 1.29(55.Panico MDB, Spichler ES, Neves MF, Pinto LW, Spichler D. Prevalência e fatores de risco da doença arterial periférica sintomática e assintomática em hospital terciário, Rio de Janeiro, Brasil. J Vasc Bras. 2009;8(2):125-32).
Statistical analysis
Data were entered in Excel for Windows and analyzed with the statistical software SPSS version 18.0. The categorical variables were expressed in percentage and absolute values; the continuous variables as mean ± standard deviation or median and interquartile range, in accordance with normal distribution or not. The Chi-squared test was used to analyze the association between the variables. For the sample size calculation it was considered the significance level of 5% and power of 80%. The association between claudication and ABI was based on a study by Torres et al.(1212.Torres AGM, Machado EG, Lopes TS, Gentile PC, Vieira AC, Soares LG, et al. Prevalência de alterações do índice tornozelo-braço em indivíduos portadores assintomáticos de doença arterial obstrutiva periférica. Rev Bras Cardiol. 2012;25(2):87-93), in which the percentage difference of claudication between patients with normal and abnormal ABI was 27.3% in a sample of 72 patients.
Results
A total of 115 patients were evaluated, among which 57.4% were females, with mean age of 60.6 ± 12.5 years. In the assessment of risk factors, hypertension (64.3%), sedentary lifestyle (48.7%) and family history (58.3%) stand out. An abnormal ABI was found (≤ 0.90 and ≥ 1.3) in 42.6% of the sample (Table 1).
Table 2 shows the association of risk factors for CVD and abnormal ABI. A sedentary lifestyle was significantly associated with abnormal ABI values (p=0.05). Other cardiovascular risk factors showed no association with abnormal ABI values.
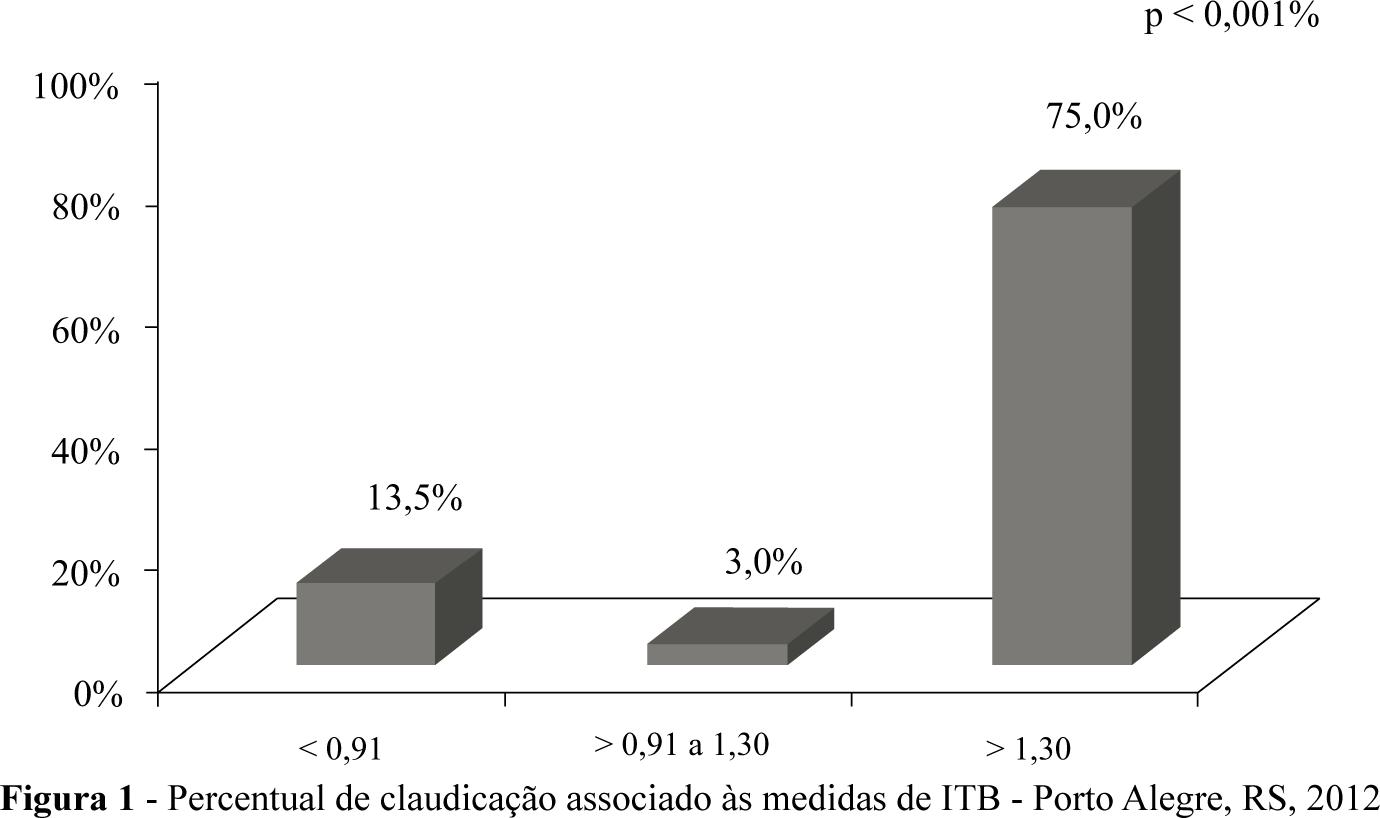
The data presented in Figure 1 show the percentage of claudication among patients according to ABI measurement. Among those with ABI>1.3 the percentage in the sample was 75% (p=0.001).
Discussion
This study demonstrated that the ABI and the Edinburgh Claudication Questionnaire are tools that provide important information on the risk for CVD, assisting in the early detection of asymptomatic cases. Moreover, they are instruments easy to use during clinical evaluation.
Currently, there are diagnostic measures of early intervention that are effective in preventing cardiovascular morbidity and mortality. The ABI is one of them, which is used in the early detection of PAD and hence, CVD(1111.Sociedade Brasileira de Cardiologia; Sociedade Brasileira de Hipertensão; Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensão. Arq Bras Cardiol. 2010;95(1 Supl.1):1-51,1313.Baena-Díez JM, Alzamora MT, Forés R, Pera G, Torán P, Sorribes M; ARTPER Study. Ankle-brachial index improves the classification of cardiovascular risk: PERART/ARTPER Study. Rev Esp Cardiol. 2011;64(3):186-92). New technologies have emerged in recent years and a range of new drugs and effective procedures for the treatment of atherosclerotic diseases have been developed. The preventive care is encouraged by acting in the control of risk factors, since the numerous complications of CVD have a major impact on the health of individuals and also generate significant public cost increases(66.Savino Neto S, Nascimento JLM. Doença arterial obstrutiva periférica: novas perspectivas de fatores de risco. Rev Para Med. 2007;21(2):35-9).
The Edinburgh Claudication Questionnaire assisted in the detection of peripheral artery disease. It guided the definition of the presence or absence of IC in patients, along with clinical assessment. The IC can be a manifestation of PAD, characterized by pain, burning and stinging in the calf region and buttocks after physical activity(1414.Silva RCG, Consolim-Colombo FM. Aspectos relevantes para identificação da claudicação intermitente. Acta Paul Enferm. 2011;24(3):426-9). Among patients with claudication, in 28.6% (p= 0.001) the ABI was abnormal. Thus, the ABI showed to be valuable for detecting abnormality in both symptomatic as in asymptomatic individuals(1515.Nunes FGF, Leão GCS, Exel AL, Diniz MCC. Índice tornozelo-braquial em pacientes de alto risco cardiovascular. Rev Bras Cadiol. 2012;25(2):94-101). Foremost, it proved to be an important strategy to help tracking the patients with CI, which was confirmed through the questionnaire applied by nurses(1414.Silva RCG, Consolim-Colombo FM. Aspectos relevantes para identificação da claudicação intermitente. Acta Paul Enferm. 2011;24(3):426-9).
In this investigation, the results are similar to those of other studies that indicate a relationship of ABI with PAD and greater frequency in females(1111.Sociedade Brasileira de Cardiologia; Sociedade Brasileira de Hipertensão; Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensão. Arq Bras Cardiol. 2010;95(1 Supl.1):1-51-1212.Torres AGM, Machado EG, Lopes TS, Gentile PC, Vieira AC, Soares LG, et al. Prevalência de alterações do índice tornozelo-braço em indivíduos portadores assintomáticos de doença arterial obstrutiva periférica. Rev Bras Cardiol. 2012;25(2):87-93,1414.Silva RCG, Consolim-Colombo FM. Aspectos relevantes para identificação da claudicação intermitente. Acta Paul Enferm. 2011;24(3):426-9-1515.Nunes FGF, Leão GCS, Exel AL, Diniz MCC. Índice tornozelo-braquial em pacientes de alto risco cardiovascular. Rev Bras Cadiol. 2012;25(2):94-101). A study with 407 patients, which aimed at detecting the prevalence of asymptomatic and symptomatic peripheral artery disease through the ABI<0.90 with PAD and between 0.90 – 1.3 without PAD, associated with risk factors, also showed a predominance of females (54%) and older age (70.1±10.2 years)(55.Panico MDB, Spichler ES, Neves MF, Pinto LW, Spichler D. Prevalência e fatores de risco da doença arterial periférica sintomática e assintomática em hospital terciário, Rio de Janeiro, Brasil. J Vasc Bras. 2009;8(2):125-32).
Another important aspect was the presence of a sedentary lifestyle in 59.2% of patients with abnormal ABI (p= 0.05). In an observational study on the presence of risk factors in the general population, physical inactivity appeared at the top of the most significant risk factors(1515.Nunes FGF, Leão GCS, Exel AL, Diniz MCC. Índice tornozelo-braquial em pacientes de alto risco cardiovascular. Rev Bras Cadiol. 2012;25(2):94-101). This reinforces the importance of encouraging physical activity at all ages and organizing activities of greater impact for this population.
Smoking was also present in the sample, however, with no statistical significance in relation to abnormal ITB. A study that also used the ABI and investigated its relation with coronary artery disease in 107 individuals, with the aim of analyzing the presence of PAD in patients undergoing cardiac catheterization, showed a 64% prevalence of smoking in patients with abnormal ABI. Therefore, it confirmed that smoking is an important predictor for PAD(1515.Nunes FGF, Leão GCS, Exel AL, Diniz MCC. Índice tornozelo-braquial em pacientes de alto risco cardiovascular. Rev Bras Cadiol. 2012;25(2):94-101). The presence of elevated total cholesterol, even when associated with ABI, did not show statistical significance, in spite of atheromatosis being related to aging(1616.Cunha ALS, Resende ES. Estudo comparativo dos fatores de risco para aterosclerose e atividade inflamatória em diferentes faixas etárias. Horiz Cient. 2007:1(1):1-9). The average age of the sample was 60.6 ± 12.5 years, with the use of hypolipidemic without compromising peripheral circulation.
The ABI is also associated with hypertension since patients with ABI <0.90 are 52% more likely to develop hypertension. This fact shows the importance of the care to hypertensive individuals, avoiding aggravations that may result in the development of arterial disease in a shorter time(66.Savino Neto S, Nascimento JLM. Doença arterial obstrutiva periférica: novas perspectivas de fatores de risco. Rev Para Med. 2007;21(2):35-9). However, in this study, no statistically significant difference was found when hypertension was analyzed separately and compared with abnormal ABI.
The alteration of ABI values and the presence of CVD risk factors in the vascular clinic proved the existence of a relation between symptomatic and asymptomatic patients. However, when analyzing the prevalence of abnormal ABI values in Figure 1, it was found that the value>1.3 was significant (p=0.001) when compared to other values.
In a cohort of The Strong Heart Study (SHS), the authors followed for 10 years (1989-1999) a population of 4,549 patients to verify whether there were differences among all the causes of mortality from CVD in the group with normal ABI values (≥ 0.9 – 1.3) and abnormal (< 0.9 or > 1.3). Abnormal ABI values were present in older patients, diabetics, hypertensive, with elevated cholesterol and microalbuminuria, plus a percentage 3-5 times higher in those with death from CVD(1717.Resnick HE, Lindsay RS, McDermott MM, Devereux RB, Jones KL, Fabsitz RR, et al. Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: the Strong Heart Study. Circulation. 2004;109(6):733-9).
A limitation of this study was the high age of the sample. Vascular greater impairment in this age group should be considered, since the patients who had claudication also had altered ABI.
Conclusion
This study demonstrated that the ABI associated with the result of the Edinburgh Claudication Questionnaire is correlated with the risk factors investigated, which qualifies it as a very important tool for clinical practice. Information regarding subclinical atherosclerotic disease, predictors of cardiovascular events, should be considered for use. It is a noninvasive method, easy to use by nurses, which should be encouraged given its low cost and potential for prevention of cardiovascular events.
References
-
1Corrêa K, Ceolim MF. Qualidade do sono em pacientes idosos com patologias vasculares periféricas. Rev Esc Enferm USP. 2008;42(1):12-8
-
2Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al.; TASC II Working Goup Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg. 2007;33 Suppl 1:S1-75
-
3Giollo Junior LT, Martin JFV. Índice tornozelo-braquial no diagnóstico da doença aterosclerótica carotídea. Rev Bras Hipertens. 2010;17(2):117-8
-
4Kawamura T. Índice Tornozelo-Braquial (ITB) determinado por esfigmomanômetros oscilométricos automáticos. Arq Bras Cardiol. 2008;90(5):322-6
-
5Panico MDB, Spichler ES, Neves MF, Pinto LW, Spichler D. Prevalência e fatores de risco da doença arterial periférica sintomática e assintomática em hospital terciário, Rio de Janeiro, Brasil. J Vasc Bras. 2009;8(2):125-32
-
6Savino Neto S, Nascimento JLM. Doença arterial obstrutiva periférica: novas perspectivas de fatores de risco. Rev Para Med. 2007;21(2):35-9
-
7Makdisse M, Nascimento Neto R, Chagas ACP, Brasil D, Borges JL, Borges JL, et al. Adaptação transcultural e validação do Questionário de Claudicação de Edimburgo. Arq Bras Cardiol. 2007;88(5):501-6
-
8Turrini FJ, Ventura MM. Prevalência de doença arterial periférica em idosos atendidos no ambulatório de geriatria e sua correlação com fatores de risco cardiovascular. UNOPAR Cient Ciênc Biol Saúde. 2002;13(1):17-21
-
9Smith FB, Lee AJ, Price JF, van Wijk MC, Fowkes FG. Changes in ankle brachial index in symptomatic and asymptomatic subjects in the general population. J Vasc Surg. 2003;38(6):1323-30
-
10Burke GL, Arnold AM, Bild DE, Cushman M, Fried LP, Newman A, et al. Factors associated with health aging: the cardiovascular health study. J Am Geriatr Soc. 2001;49(3):254-62
-
11Sociedade Brasileira de Cardiologia; Sociedade Brasileira de Hipertensão; Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensão. Arq Bras Cardiol. 2010;95(1 Supl.1):1-51
-
12Torres AGM, Machado EG, Lopes TS, Gentile PC, Vieira AC, Soares LG, et al. Prevalência de alterações do índice tornozelo-braço em indivíduos portadores assintomáticos de doença arterial obstrutiva periférica. Rev Bras Cardiol. 2012;25(2):87-93
-
13Baena-Díez JM, Alzamora MT, Forés R, Pera G, Torán P, Sorribes M; ARTPER Study. Ankle-brachial index improves the classification of cardiovascular risk: PERART/ARTPER Study. Rev Esp Cardiol. 2011;64(3):186-92
-
14Silva RCG, Consolim-Colombo FM. Aspectos relevantes para identificação da claudicação intermitente. Acta Paul Enferm. 2011;24(3):426-9
-
15Nunes FGF, Leão GCS, Exel AL, Diniz MCC. Índice tornozelo-braquial em pacientes de alto risco cardiovascular. Rev Bras Cadiol. 2012;25(2):94-101
-
16Cunha ALS, Resende ES. Estudo comparativo dos fatores de risco para aterosclerose e atividade inflamatória em diferentes faixas etárias. Horiz Cient. 2007:1(1):1-9
-
17Resnick HE, Lindsay RS, McDermott MM, Devereux RB, Jones KL, Fabsitz RR, et al. Relationship of high and low ankle brachial index to all-cause and cardiovascular disease mortality: the Strong Heart Study. Circulation. 2004;109(6):733-9
Publication Dates
-
Publication in this collection
Apr 2014
History
-
Received
24 Sept 2013 -
Accepted
04 Feb 2014