ABSTRACT
Objective: To map scientific evidence related to social determinants of adherence to antiretroviral therapy among adolescents and young people living with HIV.
Method: Scoping review according to JBI methodology, carried out on 20 databases. The inclusion criteria were: adolescents and young people living with HIV (10 and 24 years old), studies related to adherence to antiretroviral therapy (self-reported adherence, viral suppression, pill counts, or pharmacy refill records).
Results: Thirty-nine studies were identified, published between 1999 and 2024, which allowed mapping the determinants that promote and limit adherence to treatment among adolescents and young people living with HIV, being focused on individual characteristics, lifestyle, social and community networks, living and working conditions, socioeconomic, cultural and environmental conditions (Dimensions 1 to 5).
Conclusion: The social determinants of adherence interact in a complex way, which affects the context of antiretroviral therapy, both positively and negatively, and are directly interconnected with the living conditions of adolescents and young people living with HIV.
DESCRIPTORS:
HIV; Adolescent; Young Adult; Medication Adherence; Social Determinants of Health
RESUMO
Objetivo: Mapear as evidências científicas relacionadas aos determinantes sociais da adesão à terapia antirretroviral entre adolescentes e jovens vivendo com HIV.
Método: Scoping review de acordo com metodologia JBI para revisão de escopo, realizada em 20 bases de dados. Os critérios de inclusão foram: adolescentes e jovens vivendo com HIV (10 e 24 anos), estudos relacionados a adesão à terapia antirretroviral (adesão autorrelatada, supressão viral, contagem de comprimidos ou registros de reabastecimento de farmácia).
Resultados: Identificaram-se 39 estudos, publicados entre 1999 e 2024, que possibilitaram mapear os determinantes promotores e limitantes da adesão ao tratamento entre adolescentes e jovens vivendo com HIV, sendo voltados às características individuais, estilo de vida, redes sociais e comunitárias, condições de vida e trabalho, condições socioeconômicas, culturais e ambientais (Dimensões de 1 a 5).
Conclusão: Os determinantes sociais da adesão interagem de forma complexa, o que afeta o contexto da terapia antirretroviral, tanto de forma positiva quando negativa, e estão diretamente interligados às condições de vida dos adolescentes e jovens vivendo com HIV.
DESCRITORES:
HIV; Adolescente; Adulto Jovem; Adesão à Medicação; Determinantes Sociais da Saúde
RESUMEN
Objetivo: Mapear la evidencia científica relacionada con los determinantes sociales de la adherencia a la terapia antirretroviral entre adolescentes y jóvenes que viven con VIH.
Método: Revisión del alcance según la metodología del JBI para la revisión del alcance, realizado en 20 bases de datos. Los criterios de inclusión fueron: adolescentes y jóvenes viviendo con VIH (10 y 24 años), estudios relacionados con la adherencia a la terapia antirretroviral (adherencia autoinformada, supresión viral, recuento de pastillas o registros de recarga de farmacia).
Resultados: Se identificaron 39 estudios, publicados entre 1999 y 2024, que permitieron mapear los determinantes que promueven y limitan la adherencia al tratamiento entre adolescentes y jóvenes que viven con VIH, siendo centrado en las características individuales, estilo de vida, redes sociales y comunitarias, condiciones de vida y de trabajo, condiciones socioeconómicas, culturales y ambientales (Dimensiones 1 a 5).
Conclusión: Los determinantes sociales de la adherencia interactúan de forma compleja, lo que afecta el contexto de la terapia antirretroviral, tanto positiva como negativamente, y están directamente interconectados con las condiciones de vida de los adolescentes y jóvenes que viven con VIH.
DESCRIPTORES:
VIH; Adolescente; Adulto Joven; Cumplimiento de la Medicación; Determinantes Sociales de la Salud
INTRODUCTION
Across the world, adolescents and young people have represented a growing proportion of people living with HIV. In 2022, there were 480,000 adolescents and young people between 10 and 24 years old newly infected with HIV, of which 140,000 were adolescents between 10 and 19 years old. Furthermore, 25% of adolescent girls and 17% of adolescent boys aged 15–19 are from Eastern and Southern Africa, regions most affected by HIV. They were tested in the past 12 months and received their last test result. If current trends continue, there will be 183,000 new HIV infections among adolescents and young adults each year by 2030(1).
Treatment coverage among adolescents and young people living with HIV aged 15 to 24 years was estimated at 55%, significantly lower than the 75% coverage among those who are older(2). Therefore, the need for adherence to HIV treatment is highlighted, as this can save lives when started early and used appropriately. However, it is known that every year several adolescents and young people succumb to AIDS-related complications as a result of poor adherence to or treatment abandonment(3).
Adolescents and young people living with HIV face the burden of the unique physical, psychological and social challenges of adolescence and young adulthood, while also dealing with a stigmatized infectious disease that requires lifelong care, and often do not seek health care assistance(4). This therefore reflects in negative health outcomes among adolescents and young people when compared to other age groups(5).
Thus, it becomes required to adapt services for adolescents and young people in equitable, accessible, acceptable, appropriate, and effective ways(6). In line with this, part of the United Nations Sustainable Development Goals include ending the AIDS epidemic and the goal of achieving universal coverage of sexual and reproductive health services by 2030(7). To achieve these goals, it is necessary to identify the factors that facilitate and limit adherence to HIV treatment among adolescents and young people, helping professionals to develop an individualized and comprehensive care plan for each patient(2).
That said, new initiatives are needed to fight persistent barriers to accessing treatment services among adolescents and young people living with HIV, and strategies have to be created to achieve global goals. Although there is literature on adherence to treatment among this population, it does not show the social determinants of adherence that promote and limit the continuity of treatment, as well as access to health services, which constituted a knowledge gap to be explored. Within this framework, the objective of this study was to map scientific evidence related to social determinants of adherence to antiretroviral therapy among adolescents and young people living with HIV.
METHOD
Design of Study
This is a scoping review, according to JBI methodology, which aims to map the current literature, as well as list the main concepts in the area and knowledge gaps, allowing new studies(8). This scoping review was reported as per the checklist Preferred Reporting Items for Systematic Reviews and MetaAnalyses extension for Scoping Reviews (PRISMA-ScR)(9). The protocol is registered in the Open Science Framework with the identifier osf.io/j8bwa (https://doi.org/10.17605/OSF.IO/EM5TB).
Guiding Question
To develop the guiding question, the acronym PCC (Population, Concept, and Context) was considered, in which Population (P) is adolescents and young people; Concept (C) is adherence to antiretroviral therapy (ART); and Context (C) is living with HIV/AIDS. Thus, the question was obtained: What is the scientific evidence related to social determinants of adherence to antiretroviral therapy among adolescents and young people living with HIV?
Inclusion Criteria
Studies in which the population consisted of adolescents and young people, considering the age range between 10 and 24 years, were included(10). Regarding the concept, the studies were related to adherence to antiretroviral therapy, and adherence was explicitly measured using any method, such as subjective measurement (self-reported adherence), physiological methods (viral suppression), or pharmacological measurements (pill counts, pharmacy refill records), with the aim of finding the largest number of studies to identify the knowledge gap. Regarding the context, it was broad, since it considered living with HIV in all aspects, whether biological, psychological, social, cultural or spiritual, and without restriction of location. Furthermore, studies published in full were considered, without restrictions on language, time limit, and methodological design. Articles published in journals and grey literature were also eligible.
Search Strategy
From the preliminary search in the Medical Literature and Retrieval System online (MEDLINE) via National Center for Biotechnology Information (NCBI/PubMed) and Web of Science, the words in the text contained in the titles and abstracts of the relevant articles were considered to develop the complete search strategy. Subsequently, a pilot of the final search was conducted in two databases, MEDLINE via NCBI/PubMed and EMBASE. After these steps, the definitive search was carried out and, for each database and/or information source included, the search strategy, including the identified index terms and keywords, were adapted. Searches were carried out in the following databases: Web of Science (WOS), MEDLINE via NCBI/PubMed, Science Direct, Scopus, EMBASE via Elsevier, Scientific Electronic Library Online (SciELO), COCHRANE and the Latin American and Caribbean Literature in Health Sciences (LILACS); Spanish Bibliographic Index in Health Sciences (IBECS); Nursing Database (BDENF); Western Pacific Region Index Medicus (WPRIM); Peruvian Literature in Health Sciences (LIPECS); World Health Organization’s Institutional Repository for Information Sharing (WHO IRIS); Brazilian Bibliography of Dentistry (BBO) via the Virtual Health Library (VHL), accessed through the Journals Portal of the Coordination for the Improvement of Higher Education Personnel (CAPES). Additional strategies considered were the search in gray literature sources: Cybertesis, PeerJ Prepint, MedRxiv, OpenGrey, bioRxiv Preprints, Catalog of Theses and Dissertations, and cross-reference search. The searches were conducted between July and September 2024.
To construct the search strategy, the Boolean operators AND and OR were used, associated with the MeSH (Medical Subject Headings), DeCS (Health Sciences Descriptors), Emtree and uncontrolled descriptors (Chart 1).
Construction, descriptors/keywords and Boolean operators used in the database – Maringá, PR, Brazil, 2024.
Source Selection
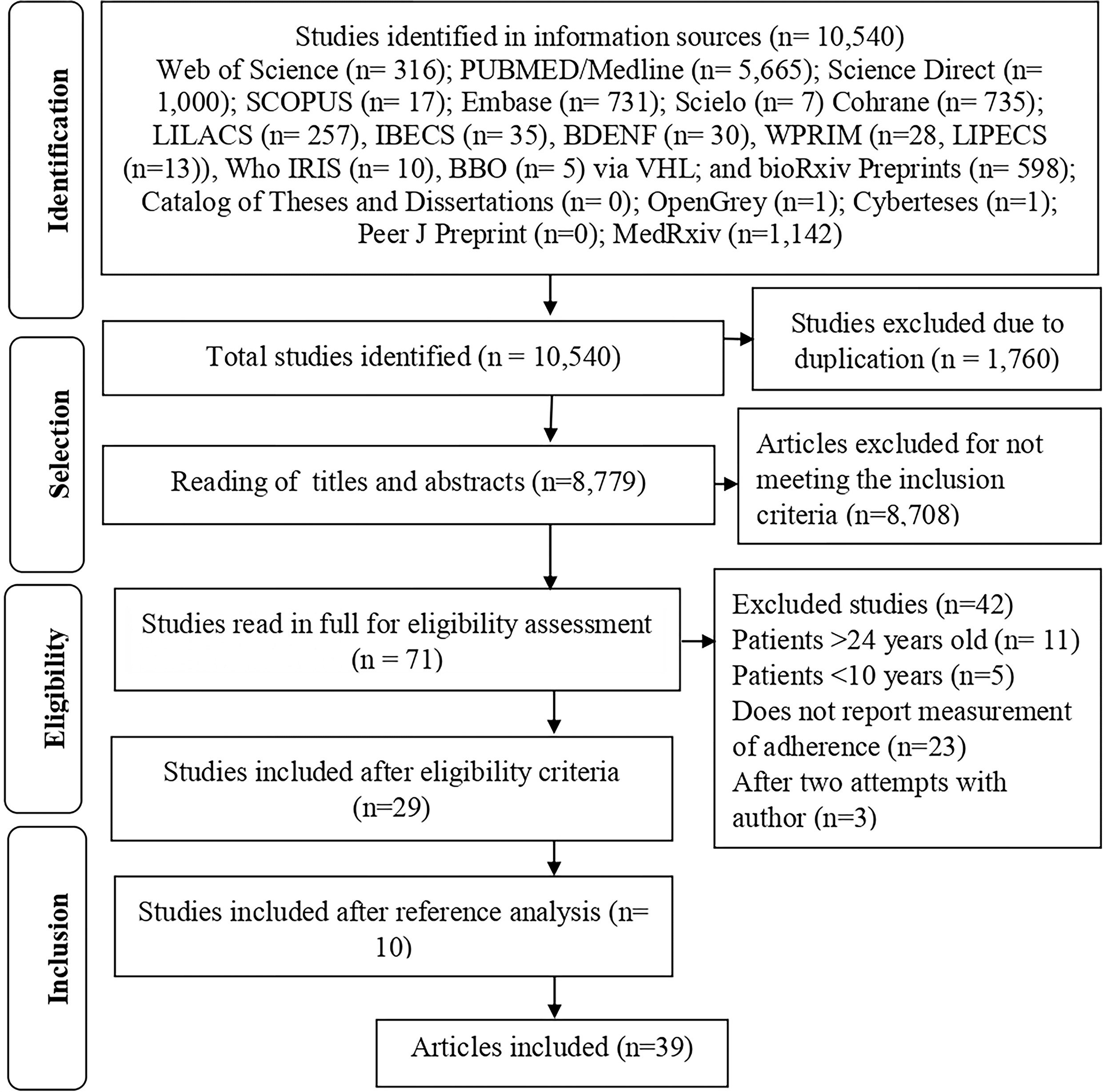
After searching the information sources, the results were exported to the application Rayyan® of Qatar Computing Research Institute (QCRI). Thus, of the 10,540 publications, 1,760 were excluded due to duplication. Subsequently, 8,779 studies were analyzed, being selected by title and abstract by two independent reviewers to maintain the blinding process; subsequently, the selected studies were compared and a consensus was reached. There was no need for a third reviewer. After that, 8,708 were excluded because they did not meet the inclusion criteria.
During the full reading, an in-depth reading was carried out applying the eligibility criteria. The study information was organized and stored in electronic spreadsheets to ensure better interpretation and comparison between reviewers.
The articles included in the final sample were organized into an instrument in Microsoft Excel®, which is adapted in accordance with the JBI methodology(8) and contained the data characterizing the publications (authors, year, title, language, country, source of information, method, adherence measure, population, main results).
Data Analysis, Extraction and Presentation
A careful reading was carried out to classify the texts and, subsequently, the results were extracted. In addition, a manual search was performed to verify the list of references of the studies included in the review, which resulted in the inclusion of ten more articles. This stage was intended to find studies that were not linked to databases. At the end, 39 publications were part of this study. Figure 1 shows the process of searching, excluding, and selecting publications according to PRISMA(9).
Flowchart for identifying and selecting articles included in the scoping review. Maringa, PR, Brazil, 2024.
All information from the included studies was stored in spreadsheets and analytical charts. The included studies were analyzed in light of the Social Determinants of Health(11), which facilitated the process of interpreting and comparing the productions, consequently helping in the description of evidence and data mapping, which were related to the description of the social determinants of adherence among adolescents and young people living with HIV. The determinants were presented in a chart.
Considering that this study is a scoping review that used already available publications, assessment by a Research Ethics Committee is not required. However, the research was developed considering the ethical aspects related to the selected articles authorship.
RESULTS
The application of search strategies in information sources allowed the identification of 10,540 publications. During the title and abstract selection, 71 studies were obtained for full analysis, and of these, after applying the eligibility criteria, 39 studies were selected, whose results answered the guiding question(12–50).
General Characteristics of The Included Studies
It was observed that 37 (94.87%)(12–21,23–50) presented the text available in English, one (2.56%) in French(22) and one (2.56%) in Portuguese(18). The publication period covered the years 1999 to 2024, with 20 publications relating to the period 2017–2024(31–50). Of the 39 studies, 17 were reported to have been developed on the African continent: five in Uganda(24,30,39,45–46), three in South Africa(42,44,50), two in Botswana(21,37), Kenya(36,40), Ethiopia(47,48) and Zambia(35,36), one in each of the following: Zimbabwe(27), Sub-Saharan Africa(28), Malawi(32), Cameroon(41), Nigeria(43) and Eswatini(49); in North America, 15 studies were developed, all from the United States of America(12–17,19–20,23,25,26,29,31,33,38); in Latin America, only one study was carried out in Brazil(18); and in Europe a publication from Belgium was found(22).
Objectives, Methods, Adherence Measures and Participants of Included Studies
Regarding the objectives of the studies, most publications were designed to determine the factors associated with adherence to HIV treatment among adolescents and young people, in relation to the promoting and limiting outcomes of the continuity of the follow-up. Other publications have focused on assessing adherence, as well as patients’ experiences regarding barriers and facilitators to adherence.
Regarding the methods used in the studies, it was noted that 28 (71.79%) are quantitative(12–17,19–23,26–30,32,34,38–41,44,46,47), 23 with cross-sectional design(12–16,20–23,26–30,32,34,38–42,44,46,47,49,50), three prospective cohorts(17,19,50), one retrospective(42), and one, a retrospective longitudinal(49) cohort; five (12.82%) were qualitative(18,24,31,37,45), one phenomenological(45), and four were descriptive(18, 24, 31, 37); three (7.69%) mixed methods(35,36,43), with only one categorized as convergent parallel(24), two (5.12%) systematic reviews with meta-analysis(25, 48), and one (2.58%) of quantitative and qualitative approach(33).
Regarding adherence measures, 51 forms were mentioned, 35 (68.62%) of which were subjective medication measures aimed at self-reported adherence(12,14–17,19–46,48,50), nine (17.64%) of physiological methods(14,18,22,23,25,33,42,49,50), and seven (13.72%) of pharmacological measurements(13,21,24,25,45,48,50). Of the 39 studies, it was observed that 28 (71.80%) used only one measure of adherence(12–17,19–21,26,27,29–32,34–40,43–47,50), eight (20.51%) used two medications(18,22–24,41,42,48,49), and three (7.69%) studies used three adherence measures(25,28,33). Regarding the participants, there was only one study carried out with adolescents and young people together with their families(33). With respect to the participants’ age range, it was noted that 15 (38.47%) studies included adolescents and young people (10–24 years old)(12,13,16,18–20,22,23,26,29,31,38,43,45,47) and 24 (61.53%) only adolescents (10–19 years old)(14,15,17,21,24,25,27,28,30–37,39–42,44,46,48–50).
Conceptual Framework
The promoting and limiting factors identified in the included studies were organized into five dimensions related to the determinants influencing adherence to treatment among adolescents and young people living with HIV: Dimension 1 – Individual Characteristics; Dimension 2 – Lifestyle and individual behaviors; Dimension 3 – Social and community networks; Dimension 4 – Living and health conditions; Dimension 5 – Socioeconomic, cultural, and environmental conditions. The determinants were summarized in Chart 2.
Summary of determinants identified in the studies included (n = 39) in the scoping review. Maringa, PR, Brazil, 2024.
This review found that factors related to individual characteristics, lifestyle, social and community networks, living and working conditions, socioeconomic, cultural and environmental conditions of adolescents and young people influenced adherence to HIV treatment, being constantly shaped by being multilevel, that is, interacting in a complex way. Thus, the social determinants of adherence affect the context of antiretroviral treatment, both positively and negatively, and are directly linked to the living conditions of adolescents and young people living with HIV (Figure 2).
Conceptual synthesis of the results from the final sample of social determinants of adherence among adolescents and young people living with HIV. Maringá, Paraná, Brazil, 2024.
DISCUSSION
The studies included in the review cover a wide range of countries and continents, such as North America, Latin America, Africa, Asia and Europe, and are high, middle and low average income per capita countries. Geographical and cultural diversities are important to understand how different social, economic, and cultural contexts influence adherence to antiretroviral therapy among adolescents and young people. Adapting intervention strategies must consider these contextual variations(51).
Regarding the temporality of the materials found, a significant part of the studies were published between 2017 and 2024. This fact is especially due to the launch of the United Nations General Assembly Political Declaration on ending AIDS and reducing new HIV infections. Since the launch of this declaration in 2016, countries around the world have committed to accelerating their actions to combat HIV and AIDS to end the epidemic by 2030(52).
It is clear that the minority of studies used a qualitative approach, and are essential for exploring the barriers and facilitators of adherence to ART among adolescents and young people. The qualitative approach allows for a more in-depth analysis of the perceptions, experiences and social contexts of adolescents and young people living with HIV, in addition to elucidating psychosocial and cultural issues that affect adherence, which may not be captured by quantitative studies(53,54).
Regarding the dimension of the individual characteristics of adolescents and young people living with HIV, it was noted that greater knowledge of serological status and of the importance of antiretroviral therapy are determinants that promote adherence. Therefore, if young people have access to information and understand it, it means they have knowledge about HIV/AIDS and ART. This evidence helps managers make decisions about training and keeping counselors and health professionals up to date so that they can, in turn, communicate accurate information to adolescents and young people(55).
Thus, health literacy has been a factor that influences adherence to treatment for numerous infections and diseases, especially HIV and AIDS. Patients who receive information appropriate to their level of understanding have significant results throughout treatment(56,57). The HIV knowledge and beliefs of adolescents and young people living with HIV play an essential role in their experience(58).
Linked to these individual factors, personal goals and the desire to live, combined with satisfaction with life, are aspects that promote adherence to treatment. A cross-sectional study carried out in China showed that people who accept their HIV diagnosis adhere to treatment and carry it out correctly. Consequently, they have a higher quality of life and life expectancy(59). Acceptance of HIV as a chronic condition helps to change the behavior of adolescents and young people and, in turn, leads them to change their lifestyle, with the aim of becoming undetectable and non-communicable (U = NC)(58).
However, some personal characteristics hinder the implementation of correct treatment, such as early adults and being male. Thus, being young is already a factor, since their responsibility is seen as a barrier, related to the fatigue of undergoing continuous treatment, in addition to comparison with people from the same social circle and involvement in other activities and habits specific to the age group. Furthermore, young men have more difficulty seeking help from health services, due to their own gender stereotype, undermining men’s engagement across the care cascade. Therefore, as this is a phase in which they receive less social and family support, older adolescents and young people are more likely to not adhere to treatment or have poor adherence(57).
Furthermore, a systematic review and meta-analysis conducted with orphaned adolescents showed that orphanhood status is a significant barrier to ART adherence, especially in low-income countries. Dependence on caregivers, which may be inconsistent or insufficient, compounds this challenge, indicating the need for interventions that increase social support and improve caregiver education about the importance of treatment adherence(60).
Added to this, we see that many teenagers and young people present occasional lapses in taking their antiretroviral medications due to forgetfulness, which is often caused by the psychological stress of having the infection and/or illness and having to take the medication daily(61).
Regarding the dimension of lifestyle and individual behaviors, it was noted that psychological well-being is an important determinant that must be taken into account in people living with HIV, especially adolescents and young people, as it is one of the factors that contribute to treatment success. These individuals dedicate themselves to treatment with the aim of prolonging their lives and adopting a healthy lifestyle, with a routine that minimizes psychological suffering, capable of experiencing situations of resilience in the face of the condition(62).
However, mental disorders and psychological distress, such as anxiety and depression, are common in the lives of these young people, which, combined with the abuse of legal and illegal substances, can lead to treatment abandonment(62). Therefore, experiencing emotional dissonance and having difficulty embracing one’s own identity shows that mental health is fragile, impacting treatment(58).
In the social and community networks dimension, it was noted that support, whether social, from the family or from a health professional, is a determinant that contributes positively to adherence to antiretroviral therapy among adolescents and young people living with HIV. Social relationships are necessary for all individuals, especially for people living with a chronic illness, where a support network and trusting relationships are important for coping with the disease(63). A study conducted with Peruvian adolescents highlighted how social and cultural factors, including family support and social dynamics, influence adherence to treatment. The use of social ecological models in these studies emphasizes the need to consider multiple levels of influence, from the individual to the community level, when designing interventions to improve ART adherence(53).
Moreover, trustful relationships established with healthcare professionals are important for some patients, being, in most cases, the only source of support and guidance(57). A systematic review of the literature identified that counseling and education about antiretroviral therapy are facilitators of treatment adherence, when considering the patient in their entirety, including the individual’s ethnic, cultural, socioeconomic aspects and educational level(56,57).
In this same sense, peer support is important for facing treatment; however, some young people feel embarrassed and different when they relate to partners who do not have the same condition, not finding mutual support(64). In this way, some adolescents and young people living with HIV continually seek and may have received support from other significant people and the community in their lives, making treatment and diagnosis something easier in their daily lives(58).
Damaged family dynamics, the relationship between a young person living with HIV and other family members, and trauma in the home environment are still determining factors that have negatively influenced adherence to antiretroviral therapy. Stigma and prejudice, in most cases, come from the family itself, and contribute to depressive symptoms and suicidal ideation(57).
Therefore, it is essential to invest in social support for these patients, together with their family members who know about the diagnosis, and the healthcare team, so that their quality of life and survival can be improved through adherence to ART(65). Furthermore, it is highlighted that only one study(33) brought the perspective of the family caregiver. This result highlights the need to develop new studies in this area with the aim of improving adherence to antiretroviral therapy together with the support of family members of adolescents and young people living with HIV.
It can be seen that in the dimension of living and health conditions, the promoting determinants are related to treatment and accessibility to health services. It is possible to identify that the viral load <1000 copies/ml or undetectable and a CD4+ count level ≥ 500 cells/mm3 or increased is associated with adherence, as young people feel encouraged to continue treatment. HIV suppression is an essential strategy for optimizing the health and well-being of those living with the infection. Routine viral load (VL) and CD4+ count testings are essential to improve treatment opportunities and are a particularly useful tool among groups at high risk of virological failure, such as adolescents(66).
A study carried out in the United Kingdom and Ireland showed that in young people who started ART before the age of 10, the CD4+ count decreased from the age of 10 onwards, and that viral suppression <400 copies/ml over time presented mean CD4+ counts that approached mild immunodeficiency (350–500 cells/mm3) at the age of 20(67).
Adverse effects of antiretrovirals have been considered a limiting factor in ART adherence, as adolescents and young people living with HIV often struggle with self-management of treatment. Many have symptoms due to HIV disease, comorbid conditions, and/or adverse effects of antiretrovirals(62).
Adverse effects directly affect adherence, as they affect the daily lives of adolescents and/or young people and, consequently, their quality of life. Thus, to be able to neutralize barriers while improving facilitators, treatment optimization with dolutegravir (DTG)-based regimens, approaches oriented by peers, such as youth and adolescent peer supporters, and differentiated service delivery models including multi-month dispensing is an excellent strategy to minimize the impact of treatment on their lives(68,69,70).
Geographical distance has been preponderant in adherence to HIV treatment and care, mainly due to its chronicity. In general, it is a factor that limits access to health services, being a barrier that directly interferes with the rates of adherence and abandonment of treatment when the distances are greater(65,71). The lack of financial resources also affects access to treatment and, combined with distance, can interfere with both the individual’s own health outcomes and the dynamics of services, as they end up missing appointments and routines or abandoning treatment(65,72).
Likewise, accessibility to health services associated with distance from residence and individuals’ socioeconomic factors are barriers to good adherence to ART, increasing the adolescents’ vulnerability(57). Conversely, when adolescents and young people live close to the HIV service, they end up seeking the service more frequently, precisely because they do not need to pay for the service and because they live close to the place where they can consult and collect their medication(30,45).
Therefore, it is important that specialized HIV services be integrated with other levels of health services, especially those that make up primary care, as the lack of integration has hindered the development of prevention and promotion strategies and actions for this population(71).
That said, it is essential that health services focused on HIV also monitor absences and their reasons, and thus seek alternatives for greater adherence to follow-up consultations and the use of ART. Furthermore, patients must be made aware so that they can take responsibility for their own health, so that they can get involved in their care and, consequently, improve their quality of life(73).
The dimension of socioeconomic, cultural, and environmental conditions highlights the need for society and adolescents and young people living with HIV to reduce stigma. A study conducted in the Philippines showed that dealing with stereotypes about HIV contributed to the way adolescents and young people assume the judgments of others (perceived stigma) and thus internalize the stigma that changes their beliefs about themselves and the disease(58). It is also clear that stigma and discrimination are caused by misinformation about the disease and come from both themselves and others around them(58).
There is evidence that prejudice, discrimination, stigma, and fear of disclosing the diagnosis have significantly impaired adherence to antiretroviral therapy. A study carried out with adolescents in Ethiopia highlighted that the barriers of stigma, prejudice, discrimination and fear of disclosing the diagnosis have been the most prevalent. Thus, the research encourages interventions aimed at improving social support and reducing stigma, prejudice and discrimination, thus enabling adolescents and young people to leave fear aside and be able to live better with HIV(74).
Recent qualitative studies, such as those carried out in sub- Saharan African countries and Peru(53,54), highlight the critical role of stigma, fear of disclosure and emotional challenges faced by adolescents, which are determinants for optimal adherence to ART. It is noteworthy that the COVID-19 pandemic has exacerbated these barriers, increasing social isolation and hindering access to health services, which has had a negative impact on adherence to ART in several regions of the world(75).
Poverty has also been a deeply stigmatized phenomenon due to aspects of social inequality, in addition to being a factor that contributes to food and housing insecurity, negatively impacting adherence to treatment. Therefore, it becomes essential to address resource insecurity to get to the heart of HIV-related stigma(76).
Adolescents and young people living with HIV in low- and middle-income countries come from different geographic and socioeconomic backgrounds; consequently, they are at higher risk of psychosocial, developmental and comorbid problems, becoming a particularly vulnerable group in terms of treatment adherence. In addition, there are also discrepancies within resource scenarios, lack of structure, and ineffective communication among healthcare providers(77).
All of these dimensions have implications for public health promotion strategies in the context of treatment adherence among adolescents and young people living with HIV, including the design and development of family-based, social and health professional interventions. Effective strategies must be multifaceted, addressing behavioral, social, and structural factors to minimize poor adherence and loss to follow-up.
In this context, international efforts are being made with the aim of ending HIV as a public health problem by 2030, with the proposal that social inequalities be combated and intersectoral actions be expanded. Achieving the 95-95-95 target should be the goal of all countries in the world, and this requires the availability of timely testing and treatment, combined with viral load remission. Along with the adherence to drug therapy, it is also necessary for adolescents and young people living with HIV to adopt an active self-care approach, by undertaking a healthy lifestyle, attending appointments, taking tests, collecting medication on the scheduled date, as well as taking the medication correctly daily. This way, the focus of care is on adolescents and young people living with HIV; therefore, health professionals must encourage an active stance in their own treatment(78).
Study Limitations
As a limitation, it should be highlighted that all types of adherence measures were considered, which implies possible biases in the sample as well as the methodological heterogeneity associated with each type of measure, making it impossible to generalize the data. Another limitation is the non-inclusion of texts in other indexing databases; therefore, it is recognized that important published research may have been omitted with the search strategy used in this review. Nevertheless, it should be noted that all scientific rigor required for a scoping review was followed in accordance with JBI recommendations. Furthermore, the results of the conceptual synthesis should be interpreted with caution, since they present different epidemiological and socioeconomic scenarios, as well as measures and strategies implemented, operational and organizational aspects, and the format of the health system in each country.
Advances in Nursing and Health
Health professionals, especially nurses who work in HIV outpatient clinics and Primary Health Care (PHC) serving adolescents and young people, can benefit from the results, since the synthesized conceptual framework brings to light everyday situations that directly influence treatment. Consequently, with promoting and limiting determinants being recognized, the process of searching for strategies makes the reduction of rates of poor adherence and non-adherence to treatment less arduous and more specific. Based on this study, new research can be carried out to eliminate the factors that are known to limit the treatment of adolescents and young people living with HIV on several fronts and in different contexts.
CONCLUSION
Mapping the determinants that promote and/or limit adherence to antiretroviral therapy among adolescents and young people living with HIV allowed mitigating the (re)structuring of public policies in relation to clinical practice, especially in health services that meet the needs of this public, in reducing social inequalities and promoting adherence to treatment, consequently leading to the achievement of goals by 2030. The summarized findings highlight that adherence to treatment is based on personal beliefs and knowledge, routine dynamics in the family environment, and access to health services. This study also indicates the need for new research that seeks to capture the diversity of factors that reflect on the lived experience and behaviors related to adherence to antiretroviral treatment in the context of adolescence and youth.
DATA AVAILABILITY
The dataset supporting the findings of this study is not publicly available, however, all data supporting the findings of this study are available upon request to the corresponding author.
REFERENCES
-
1. United Nations International Children’s Emergency Fund [Internet]. To ramp up our efforts in the fight against AIDS, there is a need for more concentrated focus on adolescents and young people. Nova York: UNICEF; 2024 [cited 2024 Sept 15]. Available from: https://data.unicef.org/topic/hivaids/adolescents-young-people/
» https://data.unicef.org/topic/hivaids/adolescents-young-people/ -
2. Frescura L, Godfrey-Faussett P, Feizzadeh AA, El-Sadr W, Syarif O, Ghys PD. Achieving the 95 95 95 targets for all: A pathway to ending AIDS. PLoS One. 2022;17(8):e0272405. doi: http://doi.org/10.1371/journal.pone.0272405. PubMed PMID: 35925943.
» https://doi.org/10.1371/journal.pone.0272405 -
3. Iyun V, Technau KG, Vinikoor M, Yotebieng M, Vreeman R, Abuogi L, et al. Variations in the characteristics and outcomes of children living with HIV following universal ART in sub-Saharan Africa (2006-17): a retrospective cohort study. Lancet HIV. 2021;8(6):e353–62. doi: http://doi.org/10.1016/S2352-3018(21)00004-7. PubMed PMID: 33932330.
» https://doi.org/10.1016/S2352-3018(21)00004-7 -
4. Zimmerman A, Fawole A, Shahid M, Dow D, Ogbuoji O. Evidence Gaps in Economic Evaluations of HIV Interventions Targeting Young People: A Systematic Review. J Adolesc Health. 2024;75(5):709–24. doi: http://doi.org/10.1016/j.jadohealth.2024.06.013. PubMed PMID: 39140926.
» https://doi.org/10.1016/j.jadohealth.2024.06.013 -
5. Le Prevost M, Judd A, Crichton S, Foster C, Bamford A, Ford D. Factors associated with engagement in HIV care for young people living with perinatally acquired HIV in England: an exploratory observational cohort study. PLoS One. 2024;19(5):e0302601. doi: http://doi.org/10.1371/journal.pone.0302601. PubMed PMID: 38787861.
» https://doi.org/10.1371/journal.pone.0302601 -
6. World Health Organisation [Internet]. Making health services adolescent friendly Developing national quality standards for adolescent-friendly health services. Geneva: WHO; 2012 [cited 2024 Dec 19]. Available from: https://www.who.int/publications/i/item/9789241503594
» https://www.who.int/publications/i/item/9789241503594 -
7. United Nations [Internet]. 2030 Agenda for sustainable development. Transforming our World: the 2030 Agenda for Sustainable Development. Nova York: United Nations; 2016 [cited 2024 Dec 19]. Available from: https://sdgs.un.org/2030agenda
» https://sdgs.un.org/2030agenda -
8. Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Scoping reviews (2020). Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z, editors. JBI manual for evidence synthesis. Adelaide: JBI; 2024. doi: https://doi.org/10.46658/JBIMES-24.
» https://doi.org/10.46658/JBIMES-24 -
9. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. A declaração PRISMA 2020: diretriz atualizada para relatar revisões sistemáticas. Rev Panam Salud Publica. 2022;46(1):e112. doi: http://doi.org/10.26633/RPSP.2022.112. PubMed PMID: 36601438.
» https://doi.org/10.26633/RPSP.2022.112 -
10. World Health Organisation [Internet]. Adolescent health. Geneva: WHO; 2017 [cited 2024 July 7]. Available from: https://www.who.int/health-topics/adolescent-health/#tab=tab_1
» https://www.who.int/health-topics/adolescent-health/#tab=tab_1 -
11. Dahlgren G, Whitehead M. Policies and strategies to promote social equity in health. Stockholm: IFS; 1991 [cited 2024 July 7]. Available from: http://s2.medicina.uady.mx/observatorio/docs/eq/li/Eq_2007_Li_Dahlgren.pdf
» http://s2.medicina.uady.mx/observatorio/docs/eq/li/Eq_2007_Li_Dahlgren.pdf -
12. Belzer ME, Fuchs DN, Luftman GS, Tucker DJ. Antiretroviral adherence issues among HIV-positive adolescents and young adults. J Adolesc Health. 1999;25(5):316–9. doi: http://doi.org/10.1016/S1054-139X(99)00052-X. PubMed PMID: 10551660.
» https://doi.org/10.1016/S1054-139X(99)00052-X - 13. Martinez J, Bell D, Camacho R, Henry-Reid LM, Bell M, Watson C, et al. Adherence to antiviral drug regimens in HIV-infected adolescent patients engaged in care in a comprehensive adolescent and young adult clinic. J Natl Med Assoc. 2000;92(2):55–61. PubMed PMID: 10800292.
-
14. Murphy DA, Wilson CM, Durako SJ, Muenz LR, Belzer M. Antiretroviral medication adherence among the REACH HIV-infected adolescent cohort in the USA. AIDS Care. 2001;13(1):27–40. doi: http://doi.org/10.1080/09540120020018161. PubMed PMID: 11177463.
» https://doi.org/10.1080/09540120020018161 -
15. Murphy DA, Sarr M, Durako SJ, Moscicki AB, Wilson CM, Muenz LR. Barriers to HAART adherence among human immunodeficiency virus-infected adolescents. Arch Pediatr Adolesc Med. 2003;157(3):249–55. doi: http://doi.org/10.1001/archpedi.157.3.249. PubMed PMID: 12622674.
» https://doi.org/10.1001/archpedi.157.3.249 -
16. Hosek SG, Harper GW, Domanico R. Predictors of medication adherence among HIV-infected youth. Psychol Health Med. 2005;10(2):166–79. doi: http://doi.org/10.1080/1354350042000326584. PubMed PMID: 25705113.
» https://doi.org/10.1080/1354350042000326584 -
17. Murphy DA, Belzer M, Durako SJ, Sarr M, Wilson CM, Muenz LR. Longitudinal antiretroviral adherence among adolescents infected with human immunodeficiency virus. Arch Pediatr Adolesc Med. 2005;159(8):764–70. doi: http://doi.org/10.1001/archpedi.159.8.764. PubMed PMID: 16061785.
» https://doi.org/10.1001/archpedi.159.8.764 - 18. Suet MM. Estudo da adesão à terapêutica antirretroviral em adolescentes infectados pelo vírus da imunodeficiência (HIV) em um hospital de grande porte na Cidade do Rio de Janeiro [dissertação]. Rio de Janeiro: Escola Nacional de Saúde Pública Sergio Arouca, Fundação Oswaldo Cruz; 2010.
-
19. Martinez J, Harper G, Carleton RA, Hosek S, Bojan K, Clum G, et al. The impact of stigma on medication adherence among HIV-positive adolescent and young adult females and the moderating effects of coping and satisfaction with health care. AIDS Patient Care STDS. 2012;26(2):108–15. doi: http://doi.org/10.1089/apc.2011.0178. PubMed PMID: 22149767.
» https://doi.org/10.1089/apc.2011.0178 -
20. MacDonell K, Naar-King S, Huszti H, Belzer M. Barriers to medication adherence in behaviorally and perinatally infected youth living with HIV. AIDS Behav. 2013;17(1):86–93. doi: http://doi.org/10.1007/s10461-012-0364-1. PubMed PMID: 23142855.
» https://doi.org/10.1007/s10461-012-0364-1 -
21. Ndiaye M, Nyasulu P, Nguyen H, Lowenthal ED, Gross R, Mills EJ, et al. Risk factors for suboptimal antiretroviral therapy adherence in HIV-infected adolescents in Gaborone, Botswana: a pilot cross-sectional study. Patient Prefer Adherence. 2013;7:891–5. doi: http://doi.org/10.2147/PPA.S47628. PubMed PMID: 24049440.
» https://doi.org/10.2147/PPA.S47628 -
22. Vanthournout B, Van Der Kelen E, Elate D, Goetghebuer T, Hainaut M, Levy J. Évaluation clinique de l’adhésion au traitement antirétroviral chez des adolescents infectés par le VIH depuis la petite enfance. Arch Pediatr. 2013;20(4):348–55. doi: http://doi.org/10.1016/j.arcped.2013.01.015. PubMed PMID: 23466406.
» https://doi.org/10.1016/j.arcped.2013.01.015 -
23. Khokhar A, Sporter R, Rosenthal D. Health literacy is associated with medication adherence in adolescents and young adults with HIV-1 infection. J Allergy Clin Immunol. 2014;133(2):AB214. doi: http://doi.org/10.1016/j.jaci.2013.12.766.
» https://doi.org/10.1016/j.jaci.2013.12.766 -
24. Nabukeera-Barungi N, Elyanu P, Asire B, Katureebe C, Lukabwe I, Namusoke E, et al. Adherence to antiretroviral therapy and retention in care for adolescents living with HIV from 10 districts in Uganda. BMC Infect Dis. 2015;15(1):520. doi: http://doi.org/10.1186/s12879-015-1265-5. PubMed PMID: 26573923.
» https://doi.org/10.1186/s12879-015-1265-5 -
25. Hudelson C, Cluver L. Factors associated with adherence to antiretroviral therapy among adolescents living with HIV/AIDS in low- and middle-income countries: a systematic review. AIDS Care. 2015;27(7):805–16. doi: http://doi.org/10.1080/09540121.2015.1011073. PubMed PMID: 25702789.
» https://doi.org/10.1080/09540121.2015.1011073 -
26. Chenneville T, Clutter MO, Hintz S, Walsh A, Emmanuel P, Lujan-Zilberman J, et al. Decisional capacity and medication adherence among youth with HIV. AIDS Care. 2015;27(3):338–41. doi: http://doi.org/10.1080/09540121.2014.993582. PubMed PMID: 25616658.
» https://doi.org/10.1080/09540121.2014.993582 -
27. Gross R, Bandason T, Langhaug L, Mujuru H, Lowenthal E, Ferrand R. Factors associated with self-reported adherence among adolescents on antiretroviral therapy in Zimbabwe. AIDS Care. 2015;27(3):322–6. doi: http://doi.org/10.1080/09540121.2014.969676. PubMed PMID: 25338010.
» https://doi.org/10.1080/09540121.2014.969676 -
28. Mutumba M, Musiime V, Lepkwoski JM, Harper GW, Snow RC, Resnicow K, et al. Examining the relationship between psychological distress and adherence to anti-retroviral therapy among Ugandan adolescents living with HIV. AIDS Care. 2016;28(7):807–15. doi: http://doi.org/10.1080/09540121.2015.1131966. PubMed PMID: 27294696.
» https://doi.org/10.1080/09540121.2015.1131966 -
29. Gross IM, Hosek S, Richards MH, Fernandez MI. Predictors and profiles of antiretroviral therapy adherence among African American adolescents and young adult males living with HIV. AIDS Patient Care STDS. 2016;30(7):324–38. doi: http://doi.org/10.1089/apc.2015.0351. PubMed PMID: 27410496.
» https://doi.org/10.1089/apc.2015.0351 -
30. Bermudez LG, Jennings L, Ssewamala FM, Nabunya P, Mellins C, McKay M. Equity in adherence to antiretroviral therapy among economically vulnerable adolescents living with HIV in Uganda. AIDS Care. 2016;28(Suppl. 2):83–91. doi: http://doi.org/10.1080/09540121.2016.1176681. PubMed PMID: 27392003.
» https://doi.org/10.1080/09540121.2016.1176681 -
31. Chenneville T, Machacek M, Walsh ASJ, Emmanuel P, Rodriguez C. Medication adherence in 13- to 24-year-old youth living with HIV. J Assoc Nurses AIDS Care. 2017;28(3):383–94. doi: http://doi.org/10.1016/j.jana.2016.11.002. PubMed PMID: 27931753.
» https://doi.org/10.1016/j.jana.2016.11.002 -
32. Kim MH, Mazenga AC, Yu X, Ahmed S, Paul ME, Kazembe PN, et al. High self-reported non-adherence to antiretroviral therapy amongst adolescents living with HIV in Malawi: barriers and associated factors. J Int AIDS Soc. 2017;20(1):21437. doi: http://doi.org/10.7448/IAS.20.1.21437. PubMed PMID: 28406275.
» https://doi.org/10.7448/IAS.20.1.21437 -
33. Xu L, Munir K, Kanabkaew C, Le Coeur S. Factors influencing antiretroviral treatment suboptimal adherence among perinatally HIV-infected adolescents in Thailand. PLoS One. 2017;12(2):e0172392. doi: http://doi.org/10.1371/journal.pone.0172392. PubMed PMID: 28207891.
» https://doi.org/10.1371/journal.pone.0172392 -
34. Naomi W, Peter G, Mbuthia J, Joshua M, Ndwiga T. Determinants of adherence to antiretroviral among HIV positive adolescents at comprehensive care clinic, Gertrude’s Children Hospital, Nairobi, Kenya. Am J Nurs Sci. 2018;7(1):23–30. doi: http://doi.org/10.11648/j.ajns.20180701.13.
» https://doi.org/10.11648/j.ajns.20180701.13 -
35. Okawa S, Mwanza Kabaghe S, Mwiya M, Kikuchi K, Jimba M, Kankasa C, et al. Psychological well-being and adherence to antiretroviral therapy among adolescents living with HIV in Zambia. AIDS Care. 2018;30(5):634–42. doi: http://doi.org/10.1080/09540121.2018.1425364. PubMed PMID: 29347827.
» https://doi.org/10.1080/09540121.2018.1425364 -
36. Mesic A, Halim N, MacLeod W, Haker C, Mwansa M, Biemba G. Facilitators and barriers to adherence to antiretroviral therapy and retention in care among adolescents living with HIV/AIDS in Zambia: a mixed methods study. AIDS Behav. 2019;23(9):2618–28. doi: http://doi.org/10.1007/s10461-019-02533-5. PubMed PMID: 31093820.
» https://doi.org/10.1007/s10461-019-02533-5 -
37. Madiba S, Josiah U. Perceived stigma and fear of unintended disclosure are barriers in medication adherence in adolescents with perinatal HIV in Botswana: a qualitative study. BioMed Res Int. 2019;2019(1):9623159. doi: http://doi.org/10.1155/2019/9623159. PubMed PMID: 31886271.
» https://doi.org/10.1155/2019/9623159 -
38. Dinaj-Koci V, Wang B, Naar-King S, MacDonell KK. A multi-site study of social cognitive factors related to adherence among youth living with HIV in the new era of antiretroviral medication. J Pediatr Psychol. 2019;44(1):98–109. doi: http://doi.org/10.1093/jpepsy/jsy076. PubMed PMID: 30272202.
» https://doi.org/10.1093/jpepsy/jsy076 -
39. Nabunya P, Bahar OS, Chen B, Dvalishvili D, Damulira C, Ssewamala FM. The role of family factors in antiretroviral therapy (ART) adherence self-efficacy among HIV-infected adolescents in southern Uganda. BMC Public Health. 2020;20(1):340. doi: http://doi.org/10.1186/s12889-020-8361-1. PubMed PMID: 32183762.
» https://doi.org/10.1186/s12889-020-8361-1 -
40. Gitahi-Kamau N, Wahome S, Bukusi EA, Ngure K. Determinants of antiretroviral therapy adherence among older adolescents living with HIV in Kenya during the transition to adult care; An observational study. J AIDS HIV Res. 2020;12(2):24–33. doi: http://doi.org/10.5897/JAHR2020.0513. PubMed PMID: 34540322.
» https://doi.org/10.5897/JAHR2020.0513 -
41. Bongfen MC, Torpey K, Ganle J, Ankomah A. Level of adherence and associated factors among HIV-positive adolescents on antiretroviral therapy in Cameroon. Afr J AIDS Res. 2020;19(4):269–75. doi: http://doi.org/10.2989/16085906.2020.1833055. PubMed PMID: 33337976.
» https://doi.org/10.2989/16085906.2020.1833055 -
42. Zhou S, Cluver L, Shenderovich Y, Toska E. Uncovering ART adherence inconsistencies: an assessment of sustained adherence among adolescents in South Africa. J Int AIDS Soc. 2021;24(10):e25832. doi: http://doi.org/10.1002/jia2.25832. PubMed PMID: 34708912.
» https://doi.org/10.1002/jia2.25832 -
43. Aderemi-Williams RI, Razaq AR, Abah IO, Opanuga OO, Akanmu AS. Adolescents and young adults knowledge, adherence and experiences while on antiretroviral therapy in a tertiary hospital in Lagos, Nigeria: a mixed-method study. J Int Assoc Provid AIDS Care. 2021;20. doi: http://doi.org/10.1177/23259582211062754. PubMed PMID: 34881662.
» https://doi.org/10.1177/23259582211062754 -
44. Steinert JI, Shenderovich Y, Smith M, Zhou S, Toska E, Cluver L. Economic well-being and associated mediating pathways to improved antiretroviral therapy adherence among adolescents living with HIV: a prospective cohort study in South Africa. J Acquir Immune Defic Syndr. 2022;91(4): 343–52. doi: http://doi.org/10.1097/QAI.0000000000003071. PubMed PMID: 35969470.
» https://doi.org/10.1097/QAI.0000000000003071 -
45. Jjumba I, Kanyesigye M, Ndagijimana G, Wattira J, Olong C, Olok RA, et al. Perceived barriers and facilitators to antiretroviral therapy adherence among youth aged 15-24 years at a regional HIV clinic in SouthWestern Uganda: a qualitative study. Afr Health Sci. 2022;22(2):54–62. doi: http://doi.org/10.4314/ahs.v22i2.7. PubMed PMID: 36407355.
» https://doi.org/10.4314/ahs.v22i2.7 -
46. Byansi W, Nabunya P, Muwanga J, Mwebembezi A, Damulira C, Mukasa B, et al. The relationship between life satisfaction, personal health, quality of life, and medication adherence among adolescents living with HIV in southwestern Uganda. Z Gesundh Wiss. 2023;31(7):1177–84. doi: http://doi.org/10.1007/s10389-021-01632-9. PubMed PMID: 37576468.
» https://doi.org/10.1007/s10389-021-01632-9 -
47. Zurbachew Y, Hiko D, Bacha G, Merga H. Adolescent’s and youth’s adherence to antiretroviral therapy for better treatment outcome and its determinants: multi-center study in public health facilities. AIDS Res Ther. 2023;20(1):91. doi: http://doi.org/10.1186/s12981-023-00588-y. PubMed PMID: 38115098.
» https://doi.org/10.1186/s12981-023-00588-y -
48. Mengesha MM, Teshome A, Ajema D, Tura AK, Hallström IK, Jerene D. The association between HIV diagnosis disclosure and adherence to anti-retroviral therapy among adolescents living with HIV in Sub-Saharan Africa: a systematic review and meta-analysis. PLoS One. 2023;18(5):e0285571. doi: http://doi.org/10.1371/journal.pone.0285571. PubMed PMID: 37167342.
» https://doi.org/10.1371/journal.pone.0285571 -
49. Hlophe LD, Constança SS, Diribsa TB, Peter SN. Determinants of anti-retroviral therapy adherence among adolescents living with HIV in the Kingdom of Eswatini. medRxiv. 2023. Preprint. doi: https://doi.org/10.1101/2023.09.25.23296.
» https://doi.org/10.1101/2023.09.25.23296 -
50. Zhou S, Cluver L, Knight L, Edun O, Sherman G, Toska E. Longitudinal trajectories of antiretroviral treatment adherence and associations with durable viral suppression among adolescents living with HIV in South Africa. J Acquir Immune Defic Syndr. 2024;96(2):171–9. doi: http://doi.org/10.1097/QAI.0000000000003408. PubMed PMID: 38771754.
» https://doi.org/10.1097/QAI.0000000000003408 -
51. Campbell L, Masquillier C, Thunnissen E, Ariyo E, Tabana H, Sematlane N, et al. Social and structural determinants of household support for ART adherence in low- and middle-income countries: a systematic review. Int J Environ Res Public Health. 2020;17(11):3808. doi: http://doi.org/10.3390/ijerph17113808. PubMed PMID: 32471153.
» https://doi.org/10.3390/ijerph17113808 -
52. United Nations Programme on HIV/Aids [Internet]. Declaração Política de 2016 da ONU sobre o Fim da AIDS põe o mundo no caminho da Aceleração da Resposta para o fim da epidemia até 2030. Brasília: UNAIDS; 2016 [cited 2024 Dec 19]. Available from: https://unaids.org.br/2016/06/declaracao-politica-2016-ps/#:~:text=A%20Declara%C3%A7%C3%A3o%20Pol%C3%ADtica%20de%202016,a%20n%C3%ADvel%20mundial%20at%C3%A9%202020
» https://unaids.org.br/2016/06/declaracao-politica-2016-ps/#:~:text=A%20Declara%C3%A7%C3%A3o%20Pol%C3%ADtica%20de%202016,a%20n%C3%ADvel%20mundial%20at%C3%A9%202020 -
53. Galea JT, Wong M, Muñoz M, Valle E, Leon SR, Díaz Perez D, et al. Barriers and facilitators to antiretroviral therapy adherence among Peruvian adolescents living with HIV: a qualitative study. PLoS One. 2018;13(2):e0192791. doi: http://doi.org/10.1371/journal.pone.0192791. PubMed PMID: 29447226.
» https://doi.org/10.1371/journal.pone.0192791 -
54. Asaolu IO, Gunn JK, Center KE, Koss MP, Iwelunmor JI, Ehiri JE. Predictors of HIV testing among youth in Sub-Saharan Africa: a cross-sectional study. PLoS One. 2016;11(10):e0164052. doi: http://doi.org/10.1371/journal.pone.0164052. PubMed PMID: 27706252.
» https://doi.org/10.1371/journal.pone.0164052 -
55. Kawuki J, Gatasi G, Sserwanja Q, Mukunya D, Musaba MW. Comprehensive knowledge about HIV/AIDS and associated factors among adolescent girls in Rwanda: a nationwide cross-sectional study. BMC Infect Dis. 2023;23(1):382. doi: http://doi.org/10.1186/s12879-023-08187-y. PubMed PMID: 37286932.
» https://doi.org/10.1186/s12879-023-08187-y -
56. Mgbako O, Conard R, Mellins CA, Dacus JD, Remien RH. A systematic review of factors critical for HIV health literacy, ART adherence and retention in care in the U.S. for racial and ethnic minorities. AIDS Behav. 2022;26(11):3480–93. doi: http://doi.org/10.1007/s10461-022-03680-y. PubMed PMID: 35445996.
» https://doi.org/10.1007/s10461-022-03680-y -
57. Hlophe LD, Tamuzi JL, Shumba CS, Nyasulu PS. Barriers and facilitators to anti-retroviral therapy adherence among adolescents aged 10 to 19 years living with HIV in sub-Saharan Africa: a mixed-methods systematic review and meta-analysis. PLoS One. 2023;18(5):e0276411. doi: http://doi.org/10.1371/journal.pone.0276411. PubMed PMID: 37200399.
» https://doi.org/10.1371/journal.pone.0276411 -
58. Sombrea DP, Santarin SLM, Verde TGM, Tidalgo AD, Tolosa CS. The unheard stories: experiences of young people living with human immunodeficiency virus in dealing with discrimination in the Philippines. HIV AIDS. 2024;16:33–43. doi: http://doi.org/10.2147/HIV.S438280. PubMed PMID: 38375060.
» https://doi.org/10.2147/HIV.S438280 -
59. Gao C, Xiao X, Zhang L, Xu H, Wang M, Wang H. The relationship between acceptance of illness and quality of life among men who have sex with men living with human immunodeficiency virus: a cross-sectional study. Int J Nurs Sci. 2022;9(3):313–20. doi: http://doi.org/10.1016/j.ijnss.2022.05.001. PubMed PMID: 35891907.
» https://doi.org/10.1016/j.ijnss.2022.05.001 -
60. Kamau SG, Akatusasira R, Namatovu A, Kibet E, Ssekitto JM, Mamun MA, et al. The level of antiretroviral therapy (ART) adherence among orphan children and adolescents living with HIV/AIDS: a systematic review and meta-analysis. PLoS One. 2024;19(2):e0295227. doi: http://doi.org/10.1371/journal.pone.0295227. PubMed PMID: 38381726.
» https://doi.org/10.1371/journal.pone.0295227 -
61. Kamangu JWN, Mboweni SH. Factors impacting ART adherence among HIV-Positive older adolescents and younger adults in Namibia: a qualitative analysis. Open Public Health J. 2024;17(1):e18749445299654. doi: http://doi.org/10.2174/0118749445299654240402033559.
» https://doi.org/10.2174/0118749445299654240402033559 -
62. Tarantino N, Norman B, Enimil A, Osei Asibey S, Martyn-Dickens C, Guthrie K, et al. HIV symptom severity and associated factors among young people with HIV in Ghana. AIDS Care. 2024;36(10):1462–70. doi: http://doi.org/10.1080/09540121.2023.2299332. PubMed PMID: 38184890.
» https://doi.org/10.1080/09540121.2023.2299332 -
63. Malo VF, Ritchwood TD, Relf MV, Bekker LG. Does type of social support influence medication adherence among South African adolescents living with HIV? a quantitative analysis of pilot data. J Assoc Nurses AIDS Care. 2022;33(4):492–8. doi: http://doi.org/10.1097/JNC.0000000000000325. PubMed PMID: 35034084.
» https://doi.org/10.1097/JNC.0000000000000325 -
64. Verma A, Kota KK, Bangar S, Rahane G, Yenbhar N, Sahay S. Emotional distress among adolescents living with perinatal HIV in India: examining predictors and their mediating and moderating effects. Child Adolesc Psychiatry Ment Health. 2023;17(1):40. doi: http://doi.org/10.1186/s13034-023-00587-x. PubMed PMID: 36922846.
» https://doi.org/10.1186/s13034-023-00587-x -
65. Piran CMG, Cargnin AVE, Shibukawa BMC, Oliveira NN, Silva MD, Furtado MD. Abandono de la terapia antirretroviral entre adolescentes y jóvenes con VIH/SIDA durante el COVID-19: un estudio de casos y controles. Rev Lat Am Enfermagem. 2023;31:e3947. doi: http://doi.org/10.1590/1518-8345.6497.3947. PubMed PMID: 37341259.
» https://doi.org/10.1590/1518-8345.6497.3947 -
66. Bernays S, Lariat J, Cowan F, Senzanje B, Willis N, Nenguke ZM. “They test my blood to know how much blood is in my body”: the untapped potential of promoting viral load literacy to support adherence and viral suppression among adolescents living with HIV. J Int AIDS Soc. 2023;26(10):e26153. doi: http://doi.org/10.1002/jia2.26153. PubMed PMID: 37880186.
» https://doi.org/10.1002/jia2.26153 -
67. Castro H, Sabin C, Collins IJ, Okhai H, Schou Sandgaard K, Prime K, et al. Evolution of CD4 T-Cell count with age in a cohort of young people growing up with perinatally acquired human immunodeficiency virus. Clin Infect Dis. 2024;78(3):690–701. doi: http://doi.org/10.1093/cid/ciad626. PubMed PMID: 37820036.
» https://doi.org/10.1093/cid/ciad626 -
68. Nimwesiga C, Taremwa IM, Nakanjako D, Nasuuna E. Factors associated with retention in HIV care among HIV-Positive adolescents in public antiretroviral therapy clinics in Ibanda District, Rural South Western Uganda. HIV AIDS. 2023;15:71–81. doi: http://doi.org/10.2147/HIV.S401611. PubMed PMID: 36910020.
» https://doi.org/10.2147/HIV.S401611 -
69. Uganda. Ministry of Health Uganda. Consolidated guidelines for the prevention and treatment of HIV and aids in Uganda. Kampala: Ministry of Health Uganda; 2020 [cited 2024 Dec 20]. Available from: https://elearning.idi.co.ug/wp-content/uploads/2022/05/Consolidated-Guidelines-for-the-Prevention-and-Treatment-of-HIV-and-AIDS-in-Uganda-2020.pdf
» https://elearning.idi.co.ug/wp-content/uploads/2022/05/Consolidated-Guidelines-for-the-Prevention-and-Treatment-of-HIV-and-AIDS-in-Uganda-2020.pdf -
70. Uganda. Ministry of Health Uganda. Consolidated Guidelines for the Prevention and Treatment of HIV and AIDS in Uganda. Kampala: Ministry of Health Uganda; 2022 [cited 2024 Dec 20]. Available from: https://hivpreventioncoalition.unaids.org/en/resources/consolidated-guidelines-prevention-and-treatment-hiv-and-aids-uganda-november-2022
» https://hivpreventioncoalition.unaids.org/en/resources/consolidated-guidelines-prevention-and-treatment-hiv-and-aids-uganda-november-2022 -
71. Melo GC, Carvalho ACA, Moreira ADS, Paixão JTDS. Survival time and distance to access specialized treatment among people living with HIV/Aids in the state of Alagoas, Brazil. Rev Bras Epidemiol. 2021;24(Suppl. 1):e210019. doi: http://doi.org/10.1590/1980-549720210019.supl.1. PubMed PMID: 33886892.
» https://doi.org/10.1590/1980-549720210019.supl.1 -
72. Zhou S, Cluver L, Knight L, Edun O, Sherman G, Toska E. Longitudinal trajectories of antiretroviral treatment adherence and associations with durable viral suppression among adolescents living with HIV in South Africa. J Acquir Immune Defic Syndr. 2024;96(2):171–9. doi: http://doi.org/10.1097/QAI.0000000000003408. PubMed PMID: 38771754.
» https://doi.org/10.1097/QAI.0000000000003408 -
73. Kang JY, Farkhad BF, Chan MS, Michels A, Albarracin D, Wang S. Spatial accessibility to HIV testing, treatment, and prevention services in Illinois and Chicago, USA. PLoS One. 2022;17(7):e0270404. doi: http://doi.org/10.1371/journal.pone.0270404. PubMed PMID: 35895722.
» https://doi.org/10.1371/journal.pone.0270404 -
74. Shimbre MS, Bodicha BB, Gabriel ANA, Ghazal L, Jiao K, Ma W. Barriers and facilitators of transition of adolescents living with HIV into adult care in under-resourced settings of Southern Ethiopia: a qualitative study. BMC Public Health. 2024;24(1):2800. doi: http://doi.org/10.1186/s12889-024-20338-7. PubMed PMID: 39396968.
» https://doi.org/10.1186/s12889-024-20338-7 -
75. Ssentongo P, Heilbrunn ES, Ssentongo AE, Advani S, Chinchilli VM, Nunez JJ, et al. Epidemiology and outcomes of COVID-19 in HIV-infected individuals: a systematic review and meta-analysis. Sci Rep. 2021;11(1):6283. doi: http://doi.org/10.1038/s41598-021-85359-3. PubMed PMID: 33737527.
» https://doi.org/10.1038/s41598-021-85359-3 -
76. Logie CH, Sokolovic N, Kazemi M, Islam S, Frank P, Gormley R, et al. Does resource insecurity drive HIV-related stigma? Associations between food and housing insecurity with HIV‐related stigma in cohort of women living with HIV in Canada. J Int AIDS Soc. 2022;25(Suppl. 1):e25913. doi: http://doi.org/10.1002/jia2.25913. PubMed PMID: 35818863.
» https://doi.org/10.1002/jia2.25913 -
77. Petinger C, Crowley T, van Wyk B. Experiences of adolescents living with HIV on transitioning from pediatric to adult HIV care in low and middle-income countries: A Qualitative Evidence Synthesis Protocol. PLoS One. 2024;19(2):e0296184. doi: http://doi.org/10.1371/journal.pone.0296184. PubMed PMID: 38315638.
» https://doi.org/10.1371/journal.pone.0296184 -
78. United Nations Programme on HIV/Aids [Internet]. Political declaration on HIV and AIDS: ending inequalities and getting on track to end AIDS by 2030. Geneva: UNAIDS; 2021 [cited 2024 Dec 20]. Available from: https://www.unaids.org/en/resources/documents/2021/2021_political-declaration-on-hiv-and-aids
» https://www.unaids.org/en/resources/documents/2021/2021_political-declaration-on-hiv-and-aids
Publication Dates
-
Publication in this collection
18 Aug 2025 -
Date of issue
2025
History
-
Received
31 Jan 2025 -
Accepted
30 May 2025

 Social determinants of adherence to antiretroviral therapy among adolescents and young people living with HIV: a scoping review
Social determinants of adherence to antiretroviral therapy among adolescents and young people living with HIV: a scoping review


 Source: adaptation PRISMA-ScR Checklist(
Source: adaptation PRISMA-ScR Checklist( Source: Research data, 2024.
Source: Research data, 2024.