Abstract
This systematic review compared the oral health status between institutionalized and non-institutionalized elders. The following electronic databases were searched: PubMed (Medline), Scopus, Web of Science, Lilacs and Cochrane Library, in a comprehensive and unrestricted manner. Electronic searches retrieved 1687 articles, which were analyzed with regards to respective eligibility criteria. After reading titles and abstracts, five studies were included and analyzed with respect their methodological quality. Oral status of institutionalized and non-institutionalized elderly was compared through meta-analysis. Included articles involved a cross-sectional design, which investigated 1936 individuals aged 60 years and over, being 999 Institutionalized and 937 non-institutionalized elders. Studies have investigated the prevalence of edentulous individuals, the dental caries experience and the periodontal status. Meta-analysis revealed that institutionalized elderly have greater prevalence of edentulous (OR = 2.28, 95%CI = 1.68-3.07) and higher number of decayed teeth (MD = 0.88, 95%CI = 0.71-1.05) and missed teeth (MD = 4.58, 95%CI = 1.89-7.27). Poor periodontal status did not differ significantly between groups. Compared to non-institutionalized, institutionalized elders have worse dental caries experience.
Key words
Institutionalization; Homes for the aged; Dental caries; Tooth loss
Resumo
Esta revisão sistemática comparou o estado de saúde bucal entre idosos institucionalizados e não institucionalizados. As seguintes bases de dados eletrônicas foram pesquisadas: PubMed (Medline), Scopus, Web of Science, Lilacs e Cochrane Library, de forma abrangente e irrestrita. Pesquisas eletrônicas recuperaram 1.687 artigos, que foram analisados com relação aos respectivos critérios de elegibilidade. Após a leitura de títulos e resumos, cinco estudos foram incluídos e analisados quanto à qualidade metodológica. A condição bucal de idosos institucionalizados e não institucionalizados foi comparada por meio de meta-análise. Os artigos incluídos envolveram um delineamento transversal, que investigou 1.936 indivíduos acima de 60 anos, sendo 999 institucionalizados e 937 não institucionalizados. Investigou-se a prevalência de edentulismo, a experiência de cárie e a condição periodontal. A meta-análise revelou que idosos institucionalizados possuem maior prevalência de edentulismo (OR = 2,28, IC95% = 1,68-3,07), maior número de dentes cariados (DM = 0,88, IC95% = 0,71-1,05) e de dentes perdidos (DM = 4.58, IC95% = 1,89-7,27). A condição periodontal ruim não diferiu significativamente entre os grupos. Comparados aos não institucionalizados, os idosos institucionalizados tem pior experiência de cárie.
Palavras-chave
Institucionalização; Casas para os idosos; Cárie dentária; Perda dentária
Introduction
It has been observed an evident process of population aging worldwide. In spite of being a global phenomenon, each country shows different characteristics. Variety in the way people are getting older is the main mark of this demographic scenario and it can be observed among different nations, cities, or even between neighborhoods of the same city11 Moreira RS, Nico LS, Tomita NE. Oral health conditions among the elderly in southeastern São Paulo State. J Appl Oral Sci 2009; 17(3):170-178..
According to the World Health Organization (WHO), the global population is increasing at the annual rate of 1.7%, whilst the population of those over 60 years is increasing at a rate of 3%. In addition, United Nations estimates that further increase in the population of older persons is almost inevitable, since this is the fastest growing population segment in most countries22 United Nations (UN), Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2017 Revision, Key Findings and Advance Tables. New York: UN; 2017. [Working Paper No. ESA/P/WP/248].. This may impact the way society deal with older population, since both the developed and the less-developed countries are expected to experience significant shifts in the age distribution of the population by 205022 United Nations (UN), Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2017 Revision, Key Findings and Advance Tables. New York: UN; 2017. [Working Paper No. ESA/P/WP/248]..
The demographic and epidemiological transitions in which many countries have been going through indicate an urgent need to investigate the predictors and prevalence of health issues in older population33 Moreira RS, Nico LS, Tomita NE, Ruiz T. A saúde bucal do idoso brasileiro: revisão sistemática sobre o quadro epidemiológico e acesso aos serviços de saúde bucal. Cad Saude Publica 2005; 21(6):1665-1675.. Although advances in medicine and dentistry have resulted in people living longer and presenting better oral and general health44 Hamasaha AA, Warren JJ, Hand JS, Levy SM. Coronal and root caries in the older Iowans: 9- to 11-year incidence. Spec Care Dentist 2005; 25(2):106-110.,55 Murray PE, Ede-Nichols D, Garcia-Godoy F. Oral health in Florida nursing homes. Int J Dent Hyg 2006; 4(4):198-203., it has been observed an increased population that is dependent of their daily activities and, therefore, living in long-term care facilities. Nevertheless, the health condition of elders that live in long-term care institutions may be also investigated and compared to those who live independently in the community.
An increasing number of older adults are permanently homebound and unable to access routine medical or dental care because of chronic illness and functional impairment66 American Academy of Home Care Physicians. Public Policy Statement [online]. [cited 2018 Aug 10]. Available at: http://www.aahcp.org/?Pub_Policy_Statement
http://www.aahcp.org/?Pub_Policy_Stateme...
. In addition, they need support to maintain their oral health77 Aghili H, Ahadian H, Baghiani M. Dental health and treatment needs of elderly home residents and nonresidents in Yazd city. J Health Res 2010; 6(1):116-122.,88 Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2005; 33(2):81-92.. Homebound older adults typically do not see a dentist for years, their oral health deteriorates, resulting not only in pain and infection, but also into compromised ability to eat and socialize. In consequence, it is observed a worsening of their already compromised overall physiological functioning and quality of life99 Sanders AE, Slade GD, Lim S, Reisine ST. Impact of oral disease on quality of life in the US and Australian populations. Community Dent Oral Epidemiol 2009; 37(2):171-181..
It has been shown that the oral health status of older people is poor, and living in nursing homes may increase the likelihood of oral and dental diseases, as well as the need for oral care77 Aghili H, Ahadian H, Baghiani M. Dental health and treatment needs of elderly home residents and nonresidents in Yazd city. J Health Res 2010; 6(1):116-122.,1010 Lamster IB. Oral health care services for older adults: a looming crisis. Am J Public Health 2004; 94(5):699-702.. However, it is not clear whether oral health of people living in long-term care facilities differ from those living independently in the community.
Therefore, the aim of this systematic review is to compare the oral health status between institutionalized and non-institutionalized older people. This study addresses the following question, according to the PECO (Population/Exposition/Control/Outcomes) strategy: Does non-institutionalized (Control group) elders (Population) have a better oral health status (Outcomes) compared to institutionalized ones (Exposition)? The hypothesis was that the institutionalized elderly people present a higher prevalence of oral disorders and poorer oral status.
Material and methods
This systematic review followed the recommendations of Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)1111 Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLos Med 2009; 6(7): e1000097. (http://www.prisma-statement.org). It was also registered in PROSPERO database.
Literature search strategy
The search strategy covered electronic databases and the reference lists of such articles published up to February 2018. The following electronic databases were searched: PubMed (Medline), Scopus, Web of Science, Lilacs and Cochrane Library, in a comprehensive and unrestricted manner with regards to year or language of publication. The MeSH terms used for research were ‘’aged’’, ‘’aged, 80 and over’’ (population); ‘’institutionalization’’, ‘’homes for the aged’’ (exposition); ‘’dental caries’’, ‘’tooth loss’’, ‘’periodontitis’’, ‘’gingivitis’’, ‘’dental plaque’’, ‘’dental plaque index’’ and ‘’stomatitis, denture’’ (outcomes). The search strategy was adapted for each database. In addition, free terms related each topic were included, using the Boolean operators “AND” and “OR” to match the search terms (Table 1).
Eligibility criteria
The eligibility criteria of the terms used for the research were based on the elements of the population (elderly individuals), exposition (institutionalized elderly), control (non-institutionalized elderly) and outcomes (oral health status).
Only observational studies were selected in this systematic review. Case reports, case series, in vitro studies, literature reviews, editorials, letters to editor and randomized clinical trials (RCT) were excluded.
Screening, data extraction and qualitative synthesis
Two independent reviewers (IPSF and YWC) retrieved relevant publications involving oral health status of institutionalized and non-institutionalized elderly. Titles and abstracts were analyzed during initial screening. Subsequently, full-texts articles that appeared to meet the inclusion criteria were retrieved for confirming eligibility. A reference manager and processing software (Mendeley ® Desktop, Elsevier) was used to organize references, remove duplicates and reading titles and abstracts. Disagreements were resolved by consensus after discussion with a third reviewer (LFDA). Both reviewers also performed data extraction by computing information in an electronic spreadsheet.
The following information was retrieved from the included studies: authors, country, study design, number of elderly (institutionalized and non-institutionalized), age, exclusion criteria, outcomes included, statistical analysis, main results and conclusion. In the event that details were not clear to the reviewers, the authors were contacted by e-mail for clarification. Data were summarized in a data extraction table that shows an overview of included studies.
Quality assessment
The methodological quality of the included studies was analyzed using the Fowkes and Fulton (1991) quality assessment tool1212 Fowkes FGR, Fulton PM. Critical appraisal of published research: indroductory guidelines. BMJ 1991; 302(6785):1136-1140.. The purpose of this guideline is to make a critical analysis of the included studies, considering the following aspects: study design, study sample, control group, quality of measurements and outcomes, completeness and distorting influence. Summarized questions assessed the risk of bias, the presence of confounding factors and if the results occurred by chance. Separately, two examiners (IPSF and YWC) performed the classification of the articles making a checklist. Any disagreements were resolved by consensus.
Quantitative synthesis (Meta-analysis)
A quantitative synthesis (meta-analysis) was conducted for oral health status outcomes described within at least two of the included studies. Based on that, extracted data from the proportion of edentulous individuals, prevalence of poor periodontal status, number of decayed teeth and number of missed teeth were analyzed into blocks. Meta-analyses were performed in the Open Meta-Analyst software v.10.12 (available at www.cebm.brown.edu/openmeta/index.html)1313 Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw 2012; 49(5):1-15..
Prevalence data (dichotomous) were used to calculate the Odds Ratio (OR) and 95% Confidence Interval (95%CI) parameters, used for comparisons between institutionalized and non-institutionalized groups. Continuous data (means and standard deviations) were analyzed using the Mean Difference (MD) and 95%CI. All analyses were performed using the Random effect and the Hedge estimator methods, under 5% significance1414 Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. Journal of Educational Statistics 1981; 6(2):107-128.. The heterogeneity parameter I2 was calculated for each meta-analysis.
Results
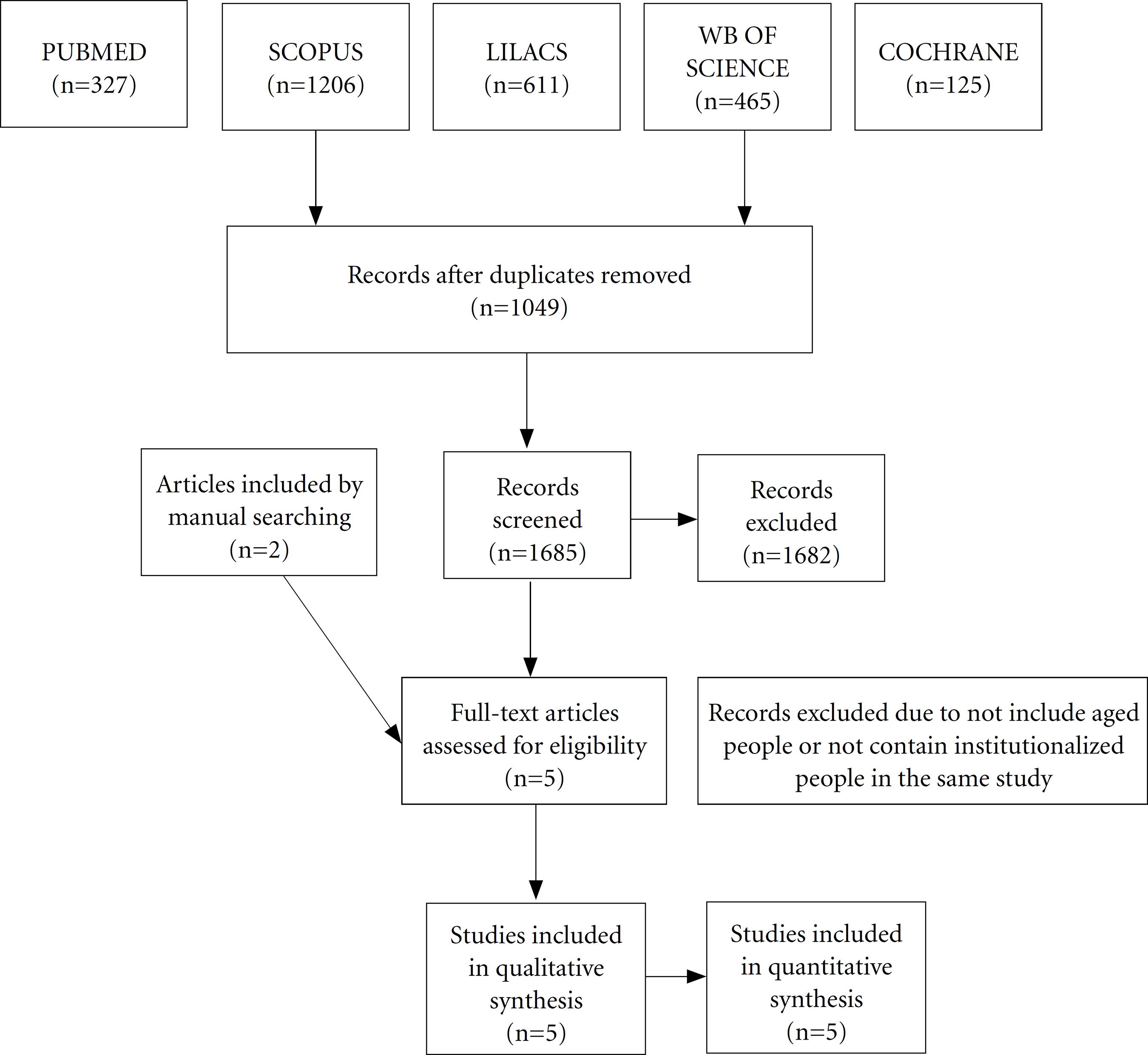
Screening of eligible publications, according to each reference database, is shown in Figure 1 (Prisma Flow Diagram). The initial search identified 2734 potential articles. Following the removal of the duplicates, 1685 articles remained. After reading the titles and abstracts, 3 articles were selected for full-text reading. Two additional studies were found after manual search. Five studies were included for data extraction and qualitative synthesis, as shown in Table 2. All studies were used to perform, at least, one of the four meta-analyses.
Characteristics of included studies
Included studies were published between 1999 and 2016 and involving a total number of 1936 aged people (999 institutionalized and 937 non-institutionalized). Full description of studies is presented on Table 2. Studies were conducted in Finland, Hong Kong, Italy, Greece and Netherlands, having all of them a cross-sectional study design1515 Pajukoski H, Meurman JH, Snellmann-Gröhn S, Sulkava R. Oral health in hospitalized and nonhospitalized community-dwelling elderly patients. Oral Surgery Oral Medicine Oral Pathology 1999; 88(4):437-443.
16 McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54.
17 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.
18 Triantos D. Intra-oral findings and general health conditions among institutionalized and non-institutionalized elderly in Greece. J Oral Pathol Med 2005; 34(10):577-582.-1919 Niesten D, Witter D, Bronkhorst E, Creugers N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J Dent 2016; 55:33-39.. One study included individuals 60 years and over1616 McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54., three considered 65 years and over1717 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.
18 Triantos D. Intra-oral findings and general health conditions among institutionalized and non-institutionalized elderly in Greece. J Oral Pathol Med 2005; 34(10):577-582.-1919 Niesten D, Witter D, Bronkhorst E, Creugers N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J Dent 2016; 55:33-39., and one enrolled elders 70 years and over1515 Pajukoski H, Meurman JH, Snellmann-Gröhn S, Sulkava R. Oral health in hospitalized and nonhospitalized community-dwelling elderly patients. Oral Surgery Oral Medicine Oral Pathology 1999; 88(4):437-443..
The oral conditions evaluated within included studies were: edentulism (number of edentulous individuals), oral lesions, periodontal status, as well as dental caries experience, including the number of decayed, missed and filled teeth. The periodontal status was assessed through Community Periodontal Index (CPI). The dental caries experience, however, was not evaluated the same way along the different studies.
In example, Niestem et al. evaluated the prevalence of individuals with at least one carious tooth, whilst Pajukoski et al. and McMillan et al. considered the number (mean and standard deviation) of decayed teeth. The DMFT index (decayed, missed and filled teeth) was reported in McMillan et al. and Bitetti et al., however the later did not present standard deviation values.
Most of studies presented a descriptive analysis and statistical comparison between groups using chi-square or t test, when applicable. Included studies showed greater number of edentulous individuals among institutionalized elderly1515 Pajukoski H, Meurman JH, Snellmann-Gröhn S, Sulkava R. Oral health in hospitalized and nonhospitalized community-dwelling elderly patients. Oral Surgery Oral Medicine Oral Pathology 1999; 88(4):437-443.
16 McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54.
17 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.-1818 Triantos D. Intra-oral findings and general health conditions among institutionalized and non-institutionalized elderly in Greece. J Oral Pathol Med 2005; 34(10):577-582.. In addition, the periodontal status did not differ significantly between institutionalized and non-institutionalized individuals1515 Pajukoski H, Meurman JH, Snellmann-Gröhn S, Sulkava R. Oral health in hospitalized and nonhospitalized community-dwelling elderly patients. Oral Surgery Oral Medicine Oral Pathology 1999; 88(4):437-443.
16 McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54.-1717 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.. Greater caries experience was observed among institutionalized individuals compared to non-institutionalized ones1515 Pajukoski H, Meurman JH, Snellmann-Gröhn S, Sulkava R. Oral health in hospitalized and nonhospitalized community-dwelling elderly patients. Oral Surgery Oral Medicine Oral Pathology 1999; 88(4):437-443.
16 McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54.-1717 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.,1919 Niesten D, Witter D, Bronkhorst E, Creugers N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J Dent 2016; 55:33-39.. Additional outcomes were reported by Triantos1818 Triantos D. Intra-oral findings and general health conditions among institutionalized and non-institutionalized elderly in Greece. J Oral Pathol Med 2005; 34(10):577-582. (oral lesions, denture stomatitis), and no differences were reported between groups. None of studies reported the use of dentures comprehensively.
Quality assessment
The quality assessment of included studies revealed that all of them do not have any important issues that would compromise the quality of those investigations. As observed in Table 3, none of studies present any risk of bias or any confounding factors. In addition, it was judged that results did not occur by chance1212 Fowkes FGR, Fulton PM. Critical appraisal of published research: indroductory guidelines. BMJ 1991; 302(6785):1136-1140..
Quantitative synthesis (Meta-analysis)
Meta-analysis of all included studies1515 Pajukoski H, Meurman JH, Snellmann-Gröhn S, Sulkava R. Oral health in hospitalized and nonhospitalized community-dwelling elderly patients. Oral Surgery Oral Medicine Oral Pathology 1999; 88(4):437-443.
16 McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54.
17 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.
18 Triantos D. Intra-oral findings and general health conditions among institutionalized and non-institutionalized elderly in Greece. J Oral Pathol Med 2005; 34(10):577-582.-1919 Niesten D, Witter D, Bronkhorst E, Creugers N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J Dent 2016; 55:33-39. revealed that institutionalized elderly have a greater proportion of edentulous individuals (OR = 2.28, 95%CI = 1.685-3.073) compared to non-institutionalized (Figure 2A). This meta-analysis exhibited an acceptable heterogeneity index (I2 = 47,81%, p = 0.147). Only one of the studies1919 Niesten D, Witter D, Bronkhorst E, Creugers N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J Dent 2016; 55:33-39. did not reject the null hypothesis.
Meta-analyses and respective forest-plots of the comparison between institutionalized and non-institutionalized individuals within included studies. Oral health status was compared regarding following outcomes: frequency of edentulous individuals (A), prevalence of poor periodontal status (B), number of decayed teeth (C) and number of missed teeth (D). Odds Ratio (OR) parameter estimated the chance of institutionalized elderly being edentulous (A) or having poor periodontal status (B). Mean Difference parameter estimated the outcome’s difference between institutionalized and non-institutionalized elderly for carious (C) and missed (D) teeth. I2 index indicate the heterogeneity of included studies.
With regards to the periodontal status, three studies were considered for meta-analysis1515 Pajukoski H, Meurman JH, Snellmann-Gröhn S, Sulkava R. Oral health in hospitalized and nonhospitalized community-dwelling elderly patients. Oral Surgery Oral Medicine Oral Pathology 1999; 88(4):437-443.
16 McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54.-1717 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516. (Figure 2B). Although the heterogeneity can be considered high (I2 = 88,20%, p < 0.001), summarized conclusion showed no differences between the institutionalized and non-institutionalized elderly (OR = 0.635, 95%CI = 0.305-1.324). High heterogeneity may be due to the variation on number of teeth within groups.
Meta-analyses also revealed that institutionalized individuals had greater number of decayed (Figure 2C) and missed (Figure 2D) teeth. The mean difference on the number of decayed teeth was 0.878 (95%CI = 0.708-1.048) and the heterogeneity for this was considered adequate (I2 = 37.83%, p = 0.205). The mean difference on the number of missed teeth was 4.580 (95%CI = 1.890-7.271), but the heterogeneity was high (I2 = 89,83%, p = 0.002).
Discussion
The increasing number of institutionalized elderly is due, in part, to the proportional growth of the elderly population. In view of the worsening of the health status of the elderly and the impossibility of families offering full-time care, the elderly are often referred to long-term care homes. Since these elderly people present greater morbidity associated with their health status, a higher prevalence of systemic and oral diseases is expected2020 Adam H, Preston AJ. The oral health of individuals with dementia in nursing homes. Gerodontology 2006; 23 (2):99-105.
21 Montal S, Tramini P, Triay JA, Valcarcel J. Oral hygiene and the need for treatment of the dependent institutionalised elderly. Gerodontology 2006; 23 (2):67-72.
22 Branca S, Bennati E, Ferlito L, Spallina G, Cardillo E, Malaguarnera M, Motta M, IMUSCE. The Health care in the extreme longevity. Arch Gerontol Geriatr 2009; 49(1):32-34.
23 Shimazaki Y, Soh I, Koga T, Miyazaki H, Takehara T. Relationship between dental care and oral health in institutionalized elderly people in Japan. J Oral Rehabil 2004; 31(9):827-842.-2424 Zenthofer A, Dieke R, Dieke A, Wege KC, Rammelsberg P, Hassel AJ. Improving oral hygiene in the long-term care of the elderly - a RCT. Community Dent Oral Epidemiol 2013; 41 (3):261-268.. In this sense, the results of this systematic review and meta-analysis point out that institutionalized elderly present a poorer oral health status compared to non-institutionalized ones.
First of all, the poorer oral health status detected in this meta-analysis may not be considered due to the process of institutionalization. All of the included studies presented a cross-sectional design, which is not accurate to detect cause-effect relationship. Nevertheless, poorer oral health status may be a result of the poorer general health condition, which leads to the elder’s institutionalization2020 Adam H, Preston AJ. The oral health of individuals with dementia in nursing homes. Gerodontology 2006; 23 (2):99-105.
21 Montal S, Tramini P, Triay JA, Valcarcel J. Oral hygiene and the need for treatment of the dependent institutionalised elderly. Gerodontology 2006; 23 (2):67-72.-2222 Branca S, Bennati E, Ferlito L, Spallina G, Cardillo E, Malaguarnera M, Motta M, IMUSCE. The Health care in the extreme longevity. Arch Gerontol Geriatr 2009; 49(1):32-34.. Besides that, most of the nursing care homes are not prepared to provide full dental health care2323 Shimazaki Y, Soh I, Koga T, Miyazaki H, Takehara T. Relationship between dental care and oral health in institutionalized elderly people in Japan. J Oral Rehabil 2004; 31(9):827-842.
24 Zenthofer A, Dieke R, Dieke A, Wege KC, Rammelsberg P, Hassel AJ. Improving oral hygiene in the long-term care of the elderly - a RCT. Community Dent Oral Epidemiol 2013; 41 (3):261-268.-2525 Adams R. Qualified nurses lack adequate knowledge related to oral health, resulting in inadequate oral care of patients on medical wards. J Adv Nurs 1996; 24 (3):552-560..
With regards to the oral care provided within long term facilities, some factors can contribute to the deterioration of the oral health of the elderly: first, caregivers often present limited knowledge about the oral priorities of the elderly, in addition to insufficient time to perform them; secondly, access to dental care centers is limited, especially related to situations of mobility difficulties; finally, oral problems are of little importance for the elderly, considering the context of the multi-morbidity of these2525 Adams R. Qualified nurses lack adequate knowledge related to oral health, resulting in inadequate oral care of patients on medical wards. J Adv Nurs 1996; 24 (3):552-560.,2626 Santinucci D, Attard N. The oral health of institutionalized older adults in Malta. Int J Prosthodont 2015; 28(2):146-148..
In addition to logistical challenges in getting homebound elderly to a dentist, medical-care usually does not cover dental costs. Although nursing facilities must provide or arrange for the provision of dental services for residents2727 Federal Nursing Home Reform Act from the Omnibus Budget Reconciliation Act of 1987 [on-line]. [cited 2018 Aug 10]. Available at: http://www.allhealth.org/Brief ingMaterials/OBRA87Summary-984.pdf
http://www.allhealth.org/Brief ingMateri...
, there is no law mandating provision of oral health care for institutionalized elderly2828 Ornstein KA, DeCherrie L, Gluzman R, Scott ES, Kansal J, Shah T, Katz R, Soriano TA. Significant unmet oral health needs of homebound elderly adults. J Am Geriatr Soc 2015; 63(1):151-157.. The arrangements within each long-term care facilities depends if it is public or private, in addition to have well prepared staff to provide oral care, in example of technical oral health professionals2929 Yi Mohammadi JJ, Franks K, Hines S. Effectiveness of professional oral health care intervention on the oral health of residents with dementia in residential aged care facilities: a systematic review protocol. JBI Database System Rev Implement Rep 2015; 13(10):110-122.. However, these aspects were not considered within the studies included in the present systematic review and meta-analysis.
Another important factor is that the institutionalized elderly present physical limitations and/or cognitive impairment that make them unable to perform their own oral hygiene or remove their prosthesis, favoring the onset or worsening of dental caries, oral infections and pain. Such situations can lead to potentially negative consequences, such as nutritional deficiencies, weight loss and systemic problems, leading to a decrease in the quality of life. These aspects put into evidence the conditions of systemic repercussion, in detriment of oral health2929 Yi Mohammadi JJ, Franks K, Hines S. Effectiveness of professional oral health care intervention on the oral health of residents with dementia in residential aged care facilities: a systematic review protocol. JBI Database System Rev Implement Rep 2015; 13(10):110-122.. Physical and cognitive impairment are frequently the main reason for institutionalization. The critical condition of such individuals leads to a higher dependency, which usually impact the provision of oral health care2929 Yi Mohammadi JJ, Franks K, Hines S. Effectiveness of professional oral health care intervention on the oral health of residents with dementia in residential aged care facilities: a systematic review protocol. JBI Database System Rev Implement Rep 2015; 13(10):110-122.
30 Bots-VantSpijker PC, VanobbergenJN, Schols JM, Schaub RM, Bots CP, de Baat C. Barriers of Delivering Oral Health Care to Older People Experienced by Dentists: A Systematic Literature Review. Community Dent Oral Epidemiol 2014; 42(2):113-121.-3131 Dolan TA, Atchison KA. Implications of access, utilization and need for oral health care by the non-institutionalized and institutionalized elderly on the dental delivery system . J Dent Educ 1993; 57(12):876-887..
With regards to the service offered by long-term care institutions, it is observed absence of oral care protocols and high employee turnover, which results in a lack of the continuity of care. In addition, employees report that oral care is a burden and a physically demanding work2929 Yi Mohammadi JJ, Franks K, Hines S. Effectiveness of professional oral health care intervention on the oral health of residents with dementia in residential aged care facilities: a systematic review protocol. JBI Database System Rev Implement Rep 2015; 13(10):110-122.. Factors involving dentists include: lack of adequate equipment; reduction of the time available for private practice; and apathy of administrators and employees of the institutions in relation to dental activities3030 Bots-VantSpijker PC, VanobbergenJN, Schols JM, Schaub RM, Bots CP, de Baat C. Barriers of Delivering Oral Health Care to Older People Experienced by Dentists: A Systematic Literature Review. Community Dent Oral Epidemiol 2014; 42(2):113-121.,3131 Dolan TA, Atchison KA. Implications of access, utilization and need for oral health care by the non-institutionalized and institutionalized elderly on the dental delivery system . J Dent Educ 1993; 57(12):876-887..
Although the included studies in this systematic review and meta-analysis indicate that institutionalized elderly have poorer oral status, the prevalence of oral disorders among non-institutionalized elderly is also considered high1616 McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54.,1717 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.. The missing teeth consists the most evident finding of dental care experience among elderly people1616 McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54.,1717 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.,1919 Niesten D, Witter D, Bronkhorst E, Creugers N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J Dent 2016; 55:33-39.. It is important to highlight that institutionalized individuals might have poorer oral status before being admitted into institutional long-term care3232 Chalmers JM, Carter KD, Spencer AJ. Oral diseases and conditions in community-living older adults with and without dementia. Spec Care Dentist 2003; 23(1):7-17.
33 Philip P, Rogers C, Kruger E, Tennant M. Caries experience of institutionalized elderly and its association with dementia and functional status. Int J Dent Hyg 2012; 10(2):122-127.-3434 Tonsekar PP, Jiang SS, Yue G. Periodontal disease, tooth loss and dementia: Is there a link? A systematic review. Gerodontology 2017; 34(2):151-163.. Therefore, results of this study may be evaluated with care, since higher caries experience may not be due to institutionalization, but associated with poor general health during life course3434 Tonsekar PP, Jiang SS, Yue G. Periodontal disease, tooth loss and dementia: Is there a link? A systematic review. Gerodontology 2017; 34(2):151-163.,3535 Philip P, Rogers C, Kruger E, Tennant M. Oral hygiene care status of elderly with dementia and in residential aged care facilities. Gerodontology 2012; 29(2): e306-311..
The high caries experience observed in the elderly population, in general, is due to the inefficiency of the methods of prevention and dental treatment received during the course of life3636 Ramsay SE, Whincup PH, Watt RG, Tsakos G, Papacosta AO, Lennon LT, Wannamethee SG. Burden of poor oral health in older age: findings from a population-based study of older British men. BMJ Open 2015; 5(12): e009476.. Poor periodontal status was also present in institutionalized and non-institutionalized elderly. Although dental practice has been transformed and advanced over the last few years, it is necessary to assume that the elderly accumulates signs of a denaturing and iatrogenic dental practice3737 Aragón F, Zea-Sevilla MA, Montero J, Sancho P, Corral R, Tejedor C, Frades-Payo B, Paredes-Gallardo V, Albaladejo A. Oral health in Alzheimer's disease: a multicenter case-control study. Clin Oral Investig 2018; 22(9):3061-3070..
From the results of this study, it can be suggested that institutionalized elders may experience a poorer oral status, which calls attention to their general health. Sometimes, increased number of edentulous individuals is related to the lack of knowledge of family members and other health professionals, who suggest the removal of teeth in the elderly with neurodegenerative diseases or in a condition of dependence3838 Furuta M, Takeuchi K, Adachi M, Kinoshita T, Eshima N, Akifusa S, Kikutani T, Yamashita Y. Tooth loss, swallowing dysfunction and mortality in Japanese older adults receiving home care services. Geriatr Gerontol Int 2018; 18(6):873-880.. The loss of teeth may impact the nutrition of elders, resulting into other systemic complications. Besides that, poor periodontal status may also be associated with other systemic illness.
The difference in the caries experience between institutionalized and non-institutionalized elderly people is generally due to the lack of personal motivation, historical less self-care, past low access to health services and greater systemic impairment, which leads to direct attention to other aspects than the oral health. Although this meta-analysis did not show differences on the periodontal status, two of three included studies exhibited higher prevalence of periodontal pockets. This can also be a result of neglecting the own oral health during life course.
Non-institutionalized elderly people are more often inserted in the social context, being more attentive with their personal care and, consequently, with their oral hygiene1717 Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.. In addition, community-dwelling elderly have the autonomy to maintain their adequate health levels, presenting greater perception about oral health3939 Carvalho C, Manso AC, Escoval A, Salvado F, Nunes C. Self-perception of oral health in older adults from an urban population in Lisbon, Portugal. Rev Saude Publica 2016; 50(1):53..
A limitation of the included studies of this systematic review rests on the absence of socioeconomic variables. A study carried out with Lebanese elderly showed that oral health condition can be influenced by socioeconomic status, including the following variables: level of schooling, housing level (based on property prices and real estate), work experience (past or recent)4040 El Osta N, El Osta L, Khabbaz LR, Saad R, Abi-Ghosn C, Hennequin M, Tubert-Jeannin S, Fakhouri J. Social inequalities in oral health in a group of older people in a Middle Eastern country: a cross-sectional survey. Aging Clin Exp Res 2018; 30(12):1513-1521.. In addition to these, other socio-demographic variables should be added, besides age and sex: marital status, number of members in the residence and use of dental services4040 El Osta N, El Osta L, Khabbaz LR, Saad R, Abi-Ghosn C, Hennequin M, Tubert-Jeannin S, Fakhouri J. Social inequalities in oral health in a group of older people in a Middle Eastern country: a cross-sectional survey. Aging Clin Exp Res 2018; 30(12):1513-1521.. Only one of the included studies in this meta-analysis considered the effect of socio-economical status, however the dependent variable were not the oral health status, but the oral-health related quality of life1919 Niesten D, Witter D, Bronkhorst E, Creugers N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J Dent 2016; 55:33-39..
Another limitation of the included studies consists the age of the elderly participants, in which the minimum age for the elderly to be included was 65 years, considering three of five included studies. The World Health Organization (WHO) establishes that the minimum age to be considered as elderly is 60 years4141 World Health Organization (WHO). The Uses of Epidemiology in the Study of the Elderly. Technical Report Series 706. Geneva: WHO, 1984.. Only one of the included studies considered the age of 60 years and over1919 Niesten D, Witter D, Bronkhorst E, Creugers N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J Dent 2016; 55:33-39.. This may be due to increased life expectancy in developed countries.
The cross-sectional design may also represent a limitation to associate the process of institutionalization to poorer oral health. However, no cohort studies compared the oral status of institutionalized and non-institutionalized elderly. Overall, few studies had compared the oral health status of institutionalized and non-institutionalized elderly. More epidemiological surveys with standardized methods, and with a cohort perspective, are recommended to allow future meta-analysis regarding the oral heath of elderly population. It is important that further studies can be conducted in this direction, providing enough data for other more robust systematic reviews.
Although some of the meta-analyses reported in the present study presented a high heterogeneity index, conclusions regarding the comparison of the oral health status can be considered sound. Higher dental caries experience and greater prevalence of edentulous are evident within institutionalized population. These aspects may also impact the general health, including the masticatory efficiency, nutritional status and frailty of institutionalized elderly.
Conclusion
Considering the results of the included studies in this systematic review and meta-analysis, we conclude that institutionalized elderly have poorer oral status compared to non-institutionalized ones.
Acknowledgment
The first author received support by the Brazilian Agency CAPES. The authors deny any conflicts of interest related to this study.
References
-
1Moreira RS, Nico LS, Tomita NE. Oral health conditions among the elderly in southeastern São Paulo State. J Appl Oral Sci 2009; 17(3):170-178.
-
2United Nations (UN), Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2017 Revision, Key Findings and Advance Tables New York: UN; 2017. [Working Paper No. ESA/P/WP/248].
-
3Moreira RS, Nico LS, Tomita NE, Ruiz T. A saúde bucal do idoso brasileiro: revisão sistemática sobre o quadro epidemiológico e acesso aos serviços de saúde bucal. Cad Saude Publica 2005; 21(6):1665-1675.
-
4Hamasaha AA, Warren JJ, Hand JS, Levy SM. Coronal and root caries in the older Iowans: 9- to 11-year incidence. Spec Care Dentist 2005; 25(2):106-110.
-
5Murray PE, Ede-Nichols D, Garcia-Godoy F. Oral health in Florida nursing homes. Int J Dent Hyg 2006; 4(4):198-203.
-
6American Academy of Home Care Physicians. Public Policy Statement [online]. [cited 2018 Aug 10]. Available at: http://www.aahcp.org/?Pub_Policy_Statement
» http://www.aahcp.org/?Pub_Policy_Statement -
7Aghili H, Ahadian H, Baghiani M. Dental health and treatment needs of elderly home residents and nonresidents in Yazd city. J Health Res 2010; 6(1):116-122.
-
8Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2005; 33(2):81-92.
-
9Sanders AE, Slade GD, Lim S, Reisine ST. Impact of oral disease on quality of life in the US and Australian populations. Community Dent Oral Epidemiol 2009; 37(2):171-181.
-
10Lamster IB. Oral health care services for older adults: a looming crisis. Am J Public Health 2004; 94(5):699-702.
-
11Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLos Med 2009; 6(7): e1000097.
-
12Fowkes FGR, Fulton PM. Critical appraisal of published research: indroductory guidelines. BMJ 1991; 302(6785):1136-1140.
-
13Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw 2012; 49(5):1-15.
-
14Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. Journal of Educational Statistics 1981; 6(2):107-128.
-
15Pajukoski H, Meurman JH, Snellmann-Gröhn S, Sulkava R. Oral health in hospitalized and nonhospitalized community-dwelling elderly patients. Oral Surgery Oral Medicine Oral Pathology 1999; 88(4):437-443.
-
16McMillan AS, Wong MC, Lo EC, Allen PF. The impact of oral disease among the institutionalized and non-institutionalized elderly in Hong Kong. J Oral Rehabil 2003; 30(1):46-54.
-
17Bitteti E, Senna A, Strohmenger L. Oral health comparison between the institutionalized and non institutionalized elderly. Minerva Stomatol 2004; 53(9):507-516.
-
18Triantos D. Intra-oral findings and general health conditions among institutionalized and non-institutionalized elderly in Greece. J Oral Pathol Med 2005; 34(10):577-582.
-
19Niesten D, Witter D, Bronkhorst E, Creugers N. Oral health-related quality of life and associated factors in a care-dependent and a care-independent older population. J Dent 2016; 55:33-39.
-
20Adam H, Preston AJ. The oral health of individuals with dementia in nursing homes. Gerodontology 2006; 23 (2):99-105.
-
21Montal S, Tramini P, Triay JA, Valcarcel J. Oral hygiene and the need for treatment of the dependent institutionalised elderly. Gerodontology 2006; 23 (2):67-72.
-
22Branca S, Bennati E, Ferlito L, Spallina G, Cardillo E, Malaguarnera M, Motta M, IMUSCE. The Health care in the extreme longevity. Arch Gerontol Geriatr 2009; 49(1):32-34.
-
23Shimazaki Y, Soh I, Koga T, Miyazaki H, Takehara T. Relationship between dental care and oral health in institutionalized elderly people in Japan. J Oral Rehabil 2004; 31(9):827-842.
-
24Zenthofer A, Dieke R, Dieke A, Wege KC, Rammelsberg P, Hassel AJ. Improving oral hygiene in the long-term care of the elderly - a RCT. Community Dent Oral Epidemiol 2013; 41 (3):261-268.
-
25Adams R. Qualified nurses lack adequate knowledge related to oral health, resulting in inadequate oral care of patients on medical wards. J Adv Nurs 1996; 24 (3):552-560.
-
26Santinucci D, Attard N. The oral health of institutionalized older adults in Malta. Int J Prosthodont 2015; 28(2):146-148.
-
27Federal Nursing Home Reform Act from the Omnibus Budget Reconciliation Act of 1987 [on-line]. [cited 2018 Aug 10]. Available at: http://www.allhealth.org/Brief ingMaterials/OBRA87Summary-984.pdf
» http://www.allhealth.org/Brief ingMaterials/OBRA87Summary-984.pdf -
28Ornstein KA, DeCherrie L, Gluzman R, Scott ES, Kansal J, Shah T, Katz R, Soriano TA. Significant unmet oral health needs of homebound elderly adults. J Am Geriatr Soc 2015; 63(1):151-157.
-
29Yi Mohammadi JJ, Franks K, Hines S. Effectiveness of professional oral health care intervention on the oral health of residents with dementia in residential aged care facilities: a systematic review protocol. JBI Database System Rev Implement Rep 2015; 13(10):110-122.
-
30Bots-VantSpijker PC, VanobbergenJN, Schols JM, Schaub RM, Bots CP, de Baat C. Barriers of Delivering Oral Health Care to Older People Experienced by Dentists: A Systematic Literature Review. Community Dent Oral Epidemiol 2014; 42(2):113-121.
-
31Dolan TA, Atchison KA. Implications of access, utilization and need for oral health care by the non-institutionalized and institutionalized elderly on the dental delivery system . J Dent Educ 1993; 57(12):876-887.
-
32Chalmers JM, Carter KD, Spencer AJ. Oral diseases and conditions in community-living older adults with and without dementia. Spec Care Dentist 2003; 23(1):7-17.
-
33Philip P, Rogers C, Kruger E, Tennant M. Caries experience of institutionalized elderly and its association with dementia and functional status. Int J Dent Hyg 2012; 10(2):122-127.
-
34Tonsekar PP, Jiang SS, Yue G. Periodontal disease, tooth loss and dementia: Is there a link? A systematic review. Gerodontology 2017; 34(2):151-163.
-
35Philip P, Rogers C, Kruger E, Tennant M. Oral hygiene care status of elderly with dementia and in residential aged care facilities. Gerodontology 2012; 29(2): e306-311.
-
36Ramsay SE, Whincup PH, Watt RG, Tsakos G, Papacosta AO, Lennon LT, Wannamethee SG. Burden of poor oral health in older age: findings from a population-based study of older British men. BMJ Open 2015; 5(12): e009476.
-
37Aragón F, Zea-Sevilla MA, Montero J, Sancho P, Corral R, Tejedor C, Frades-Payo B, Paredes-Gallardo V, Albaladejo A. Oral health in Alzheimer's disease: a multicenter case-control study. Clin Oral Investig 2018; 22(9):3061-3070.
-
38Furuta M, Takeuchi K, Adachi M, Kinoshita T, Eshima N, Akifusa S, Kikutani T, Yamashita Y. Tooth loss, swallowing dysfunction and mortality in Japanese older adults receiving home care services. Geriatr Gerontol Int 2018; 18(6):873-880.
-
39Carvalho C, Manso AC, Escoval A, Salvado F, Nunes C. Self-perception of oral health in older adults from an urban population in Lisbon, Portugal. Rev Saude Publica 2016; 50(1):53.
-
40El Osta N, El Osta L, Khabbaz LR, Saad R, Abi-Ghosn C, Hennequin M, Tubert-Jeannin S, Fakhouri J. Social inequalities in oral health in a group of older people in a Middle Eastern country: a cross-sectional survey. Aging Clin Exp Res 2018; 30(12):1513-1521.
-
41World Health Organization (WHO). The Uses of Epidemiology in the Study of the Elderly. Technical Report Series 706. Geneva: WHO, 1984.
Publication Dates
-
Publication in this collection
03 June 2020 -
Date of issue
June 2020
History
-
Received
25 May 2018 -
Accepted
03 Oct 2018 -
Published
05 Oct 2018