Abstract
Background
There is currently a worldwide effort to increase the options for autogenous hemodialysis access.
Objectives
To evaluate patency and complications of brachial vein transposition compared to other autogenous hemodialysis accesses.
Methods
A retrospective evaluation of 43 patients and 45 procedures. Patients who did not have adequate superficial veins according to duplex scanning were allocated to brachial vein transposition. The sample was thus divided in two groups, as follows: A: brachial vein transposition n=10 and B: other autogenous accesses n=35.
Results
There were no statistical differences between the two groups in terms of age diabetes, systemic arterial hypertension, dyslipidemias, arteriopathies, neoplasms, kidney disease stage, donor artery diameter, recipient vein diameter, systolic blood pressure in the operated limb, postoperative ischemia, hematoma, or infection. There were no statistical differences in terms of patency on day 7: A 80% vs. B 90% p=0.6, on day 30: A 80% vs. B 86% p=0.6, or on day 60: A 60% vs. B 80% p=0.22. There were statistical differences between the groups for number of previous fistulae A 1.0 ± 0.44 vs. B 0.6 ± 0.3 p = 0.04 and upper limb edema A: 20% x B 0% p = 0.04. A vein with diameter of less than 3 mm was associated with an increased risk of early occlusion (RR = 8 p = 0.0125). During the study period there were no procedures using grafts.
Conclusions
Transposition of brachial vein is an alternative to arteriovenous graft.
Keywords:
brachial vein; graft; fistula first; brachial artery; hemodialysis access; arteriovenous fistula
Resumo
Contexto
Atualmente, observa-se um esforço mundial para aumento do número de acessos autógenos para hemodiálise.
Objetivos
Avaliar a perviedade e as complicações da transposição da veia braquial em comparação aos outros acessos autógenos para hemodiálise.
Métodos
Avaliação retrospectiva de 43 pacientes, com 45 procedimentos. Os pacientes que não apresentaram veias do sistema venoso superficial adequadas ao Duplex Scan pré-operatório foram submetidos à transposição da veia braquial. Esses procedimentos foram divididos em dois grupos: A: uso da veia braquial, n = 10. B: demais acessos, n = 35.
Resultados
Não houve diferença estatística entre os grupos no que se refere à idade, diabetes, hipertensão arterial sistêmica, dislipidemias, arteriopatias, neoplasias, estágio da doença renal, diâmetro da artéria doadora e da veia receptora, pressão arterial sistólica no membro operado, isquemia pós-operatória, formação de hematoma e infecção. Não houve diferença quanto à perviedade aos 7 dias A: 80% vs. B: 90%, p = 0,6; aos 30 dias A: 80% vs. B: 86%, p = 0,6; e aos 60 dias A: 60% vs. B: 80%, p = 0,22. Houve diferença entre os grupos quanto ao número de fístulas prévias A: 1,0 ± 0,44 vs. B: 0,6 ± 0,3, p = 0,04; e quanto ao edema em membro superior A: 20% vs. B: 0%, p = 0,04. A veia doadora menor que 3 mm esteve associada ao maior risco de oclusão precoce (RR = 8, p = 0,0125). Nesse período, não houve nenhum procedimento com o uso de prótese sintética.
Conclusões
A veia braquial transposta é uma alternativa à prótese sintética.
Palavras-chave:
veia braquial; prótese; fistula first; artéria braquial; aceso para hemodiálise; fístula arteriovenosa
INTRODUCTION
An autogenous arteriovenous fistula using superficial forearm veins is the first choice for hemodialysis access because of its greater patency, lower rate of infection and lower morbidity and mortality.11 Pham XD, Kim JJ, Ihenachor EJ, et al. Comparison of brachial artery-brachial vein arteriovenous fistulas with av grafts in patients with poor superficial venous anatomy. J Vasc Surg. 2017;65(2):444-51. http://dx.doi.org/10.1016/j.jvs.2016.09.037. PMid:27986484.
http://dx.doi.org/10.1016/j.jvs.2016.09....
,22 Morisson B, Araújo AL, Harduin LO, et al. A pilot study comparing bovine mesenteric artery and expanded polytetrafluoroethylene grafts as non-autogenous hemodialysis options. J Vasc Bras. 2018;17(4):303-9. http://dx.doi.org/10.1590/1677-5449.007117. PMid:30787948.
http://dx.doi.org/10.1590/1677-5449.0071...
The National Kidney Foundation Dialysis Outcomes Quality Initiative (NKF-DOQI) recommends that at least 65% of patients should have an autogenous arteriovenous fistula for access.33 National Kidney Foundation. 2006 updates clinical practice guidelines and recommendations. New York: KDOQI [cited 2019 Maio 26]. Available from: https://www.kidney.org/sites/default/files/docs/12-50-0210_jag_dcp_guidelines-pd_oct06_sectionb_ofc.pdf
https://www.kidney.org/sites/default/fil...
Chronic kidney disease requiring dialysis is a serious condition with high mortality and its prevalence is growing exponentially in Brazil. Over the last two decades, the number of patients on hemodialysis has tripled in Brazil, reaching 120 thousand in 2016. Annual mortality can reach 20%, primarily associated with cardiovascular events and sepsis. Infections related to central venous catheters and synthetic grafts contribute to the high sepsis rates.44 Sesso RC, Lopes AA, Thomé FS, Lugon JR, Martins CT. Brazilian chronic dialysis survey 2016. J Bras Nefrol. 2017;39(3):261-6. http://dx.doi.org/10.5935/0101-2800.20170049. PMid:29044335.
http://dx.doi.org/10.5935/0101-2800.2017...
Strategies to increase use of autologous veins to construct arteriovenous fistulas for hemodialysis are increasingly encouraged.
Autogenous accesses are associated with double the 1-year primary patency and nine times greater 2-year patency when compared with prosthetic accesses.55 Perera GB, Mueller MP, Kubaska SM, Wilson SE, Lawrence PF, Fujitani RM. Superiority of autogenous arteriovenous hemodialysis access: maintenance of function with fewer secondary interventions. Ann Vasc Surg. 2004;18(1):66-73. http://dx.doi.org/10.1007/s10016-003-0094-y. PMid:14727162.
http://dx.doi.org/10.1007/s10016-003-009...
Over recent years, with the advent of endovascular procedures, secondary patency of hemodialysis grafts has increased, but at a cost that is six times greater than autogenous fistula.66 Roy-Chaudhury P, Sukhatme VP, Cheung AK. Cheung hemodialysis vascular access dysfunction: a cellular and molecular viewpoint. J Am Soc Nephrol. 2006;17(4):1112-27. http://dx.doi.org/10.1681/ASN.2005050615. PMid:16565259.
http://dx.doi.org/10.1681/ASN.2005050615...
In efforts to increase the prevalence of use of autologous fistulae, Koontz and Hellings,77 Koontz PG Jr, Helling TS. Subcutaneous brachial vein arteriove- nous fistula for chronic hemodialysis. World J Surg. 1983;7(5):672-4. http://dx.doi.org/10.1007/BF01655353. PMid:6636812.
http://dx.doi.org/10.1007/BF01655353...
in 1983, and Bazan and Schanzer88 Bazan HA, Schanzer H. Transposition of the brachial vein: a new source for autologous arteriovenous fistulas. J Vasc Surg. 2004;40(1):184-6. http://dx.doi.org/10.1016/j.jvs.2004.03.044. PMid:15218484.
http://dx.doi.org/10.1016/j.jvs.2004.03....
, in 2006, described use of brachial vein transposition (in the superficial and anterior directions) as hemodialysis vascular access. Other studies demonstrated increased patency and lower rates of complications of this type of access over the short and long terms, compared with arteriovenous grafts.11 Pham XD, Kim JJ, Ihenachor EJ, et al. Comparison of brachial artery-brachial vein arteriovenous fistulas with av grafts in patients with poor superficial venous anatomy. J Vasc Surg. 2017;65(2):444-51. http://dx.doi.org/10.1016/j.jvs.2016.09.037. PMid:27986484.
http://dx.doi.org/10.1016/j.jvs.2016.09....
,99 Karam L, Rawa M, Shoenfeld R, Bourquelot P. Brachial vein transposition is a promising ultimate upper limb autologous arteriovenous angioaccess despite its many pitfalls. J Vasc Surg. 2017;67(1):236-43. http://dx.doi.org/10.1016/j.jvs.2017.05.120. PMid:28733096.
http://dx.doi.org/10.1016/j.jvs.2017.05....
The objectives of the present study are to evaluate the patency and complications of brachial vein transposition compared with other autogenous accesses using the standard superficial veins and to present this method as an alternative to synthetic prostheses as access for hemodialysis.
METHODS
The protocol was evaluated and authorized by the institutional Research Ethics Committee and registered on the Plataforma Brasil. Free and informed consent forms were unnecessary because this is a retrospective, observational, case-control study. All data were analyzed taking precautions to maintain patient confidentiality, protecting patients’ data.
A retrospective case-control analysis was conducted of patients who had arteriovenous fistulas constructed for hemodialysis from August 2012 to May 2014. These patients were divided into two groups, as follows: Group A: brachial vein transposition (case group); and group B: other types of access (control group). All patients underwent color Doppler ultrasonography examination of arteries and veins for preoperative mapping. In the brachial vein transposition group, surgery was performed using the technique described by Bazan and Schanzer.88 Bazan HA, Schanzer H. Transposition of the brachial vein: a new source for autologous arteriovenous fistulas. J Vasc Surg. 2004;40(1):184-6. http://dx.doi.org/10.1016/j.jvs.2004.03.044. PMid:15218484.
http://dx.doi.org/10.1016/j.jvs.2004.03....
After brachial plexus block, an oblique incision was made in the cubital fossa, followed by dissection of the brachial vein and artery. This incision was extended cranially, following the brachial vein longitudinally. The vein was dissected and its tributaries were ligated with 4-0 silk sutures. Shorter tributaries with larger diameters were ligated using 7-0 polypropylene continuous sutures. The brachial vein was then displaced from its bed and a subcutaneous tunnel was opened along the anterior aspect of the arm, into which the vein was transposed (superficial and anterior displacement). An end-to-side anastomosis was constructed between the distal extremity of the vein and the brachial artery in the cubital fossa between the end of the vein and the side of the artery with 7-0 polypropylene, after intra-arterial and intravenous local administration of heparin solution at a proportion of 1:10088 Bazan HA, Schanzer H. Transposition of the brachial vein: a new source for autologous arteriovenous fistulas. J Vasc Surg. 2004;40(1):184-6. http://dx.doi.org/10.1016/j.jvs.2004.03.044. PMid:15218484.
http://dx.doi.org/10.1016/j.jvs.2004.03....
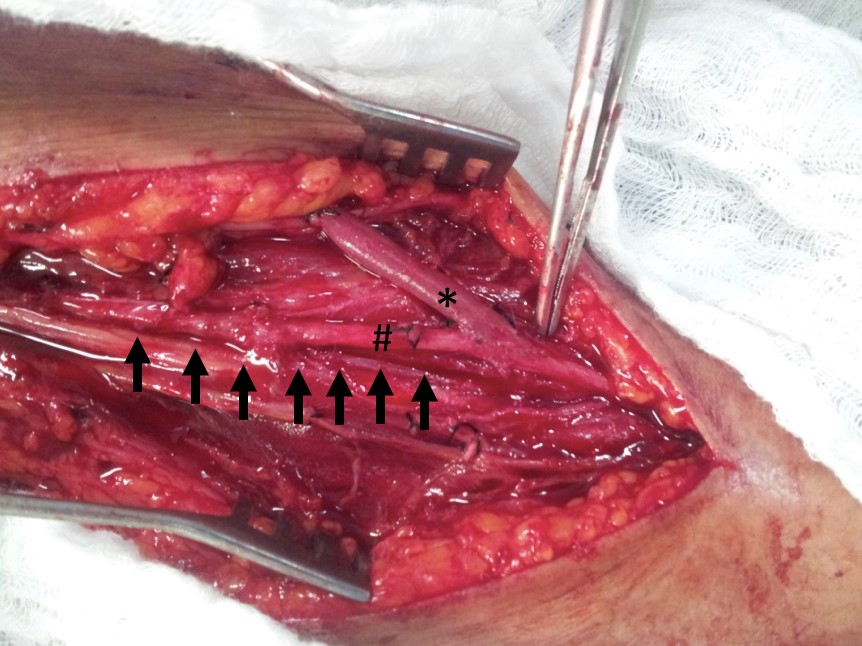
(Figure 1).
Arteriovenous fistula from the brachial artery to the brachial vein. The brachial vein is indicated with asterisks (*). The brachial artery is indicated with a hash (#). The brachial vein’s anatomic bed is indicated with arrows (the vein itself has been dissected and displaced from its anatomic position).
In the other access group, radiocephalic, brachiocephalic, brachiobasilic, ulnar-basilic and radiobasilic fistulae were constructed according to our routine protocols, with brachial plexus block and with intra-arterial and intravenous local administration of heparin solution at a proportion of 1:100. Brachiobasilic fistulae were constructed during a single intervention with superficial and anterior displacement of the vein.1010 Casey K, Tonnessen BH, Mannava K, Noll R, Money SR, Sternbergh WC 3rd. Brachial versus basilic vein dialysis fistulas: a comparison of maturation and patency rates. J Vasc Surg. 2008;47(2):402-6. http://dx.doi.org/10.1016/j.jvs.2007.10.029. PMid:18241763.
http://dx.doi.org/10.1016/j.jvs.2007.10....
A range of variables were analyzed, including age, gender, comorbidities, number of previous fistulae, systolic blood pressure in the operated limb, arterial and venous diameters, and kidney disease stage. Patients were followed up at consultations after 7, 30, and 60 days. Postoperative complications such as hematoma, infection, or ischemia were analyzed in both groups. Patency was established by detection of thrill on palpation along the path of the fistula.
Data were expressed as mean (± SD) and counts. Non-categorical variables such as mean age were assessed using Student’s t test. The Mann-Whitney U test was used to compare arterial and venous diameters, number of prior surgeries, and systolic pressure in the operated limb. Categorical variables (patency at 7, 30, and 60 days) was studied using the chi-square test with Yates’ correction or Fischer’s test, where appropriate. Results with p < 0.05 were considered statistically significant. All statistical analyses were conducted using Prism 8 for IOS version 8.0.1 (GraphPad Software Inc).
RESULTS
The sample comprised 43 patients and a total of 45 procedures. Patients were divided into two groups, as follows, Group A: brachial vein transposition, with 10 procedures; and Group B: other types of access, with 35 procedures. In the other accesses group, the following numbers of fistula procedures were conducted: radiocephalic: 16; brachiocephalic: 7; brachiobasilic: 8; ulnar-basilic: 3; and radiobasilic: 1. There were no statistically significant differences between groups in terms of age, diabetes, systemic arterial hypertension, dyslipidemia, arteriopathies, cancer, kidney disease stage, postoperative ischemia, hematoma formation, or infection (Table 1).
There were no differences between the two groups in variables related to anatomy or clinical examination (Table 2). There were no differences in patency at 7 days, A: 80% vs. B: 90%, p = 0.6; 30 days, A: 80% vs. B: 86%, p = 0.6; or 60 days, A: 60% vs. B: 80%, p = 0.22 (Figure 2).
There was a difference between the groups in terms of number of previous fistulae: A: 1.0 ± 0.44 vs. B: 0.6 ± 0.3, p = 0.04. There was also a difference in upper limb edema at 7 days (A: 20% vs. B: 0%, p = 0.04). The edema was limited to the forearm and had fully resolved by 30 days. Overall patency was 87% at 7 days, 84% at 30 days, and 76% at 60 days. There were no deaths in the brachial vein transposition group. There was one death in the other accesses group (2.86%, p = 0.9 compared with the brachial vein transposition group). Analysis of the patency data for both groups revealed that a donor vein smaller than 3 mm was associated with a 60% 7-day occlusion rate (n = 5). Donor veins exceeding 3 mm had a 7.5% occlusion rate at 7 days (n = 40). A donor vein smaller than 3 mm was associated with an increased risk of early occlusion (RR = 8, p = 0.0125). There was no difference in overall patency between diabetic patients (85.71%) and patients without diabetes (83.87%) at 7 days (n > 0.99).
DISCUSSION
Over recent years, efforts have been made to reduce use of synthetic prosthetic grafts for definitive hemodialysis access.1111 Center for Medicare & Medicaid Services. Questions and answers. Baltimore: CMS.gov; 2004 [cited novembro de 2019 26]. Available from: https://www.cms.gov/Medicare/End-Stage-Renal-Disease/ESRDQualityImproveInit/downloads/FFFAQs.pdf
https://www.cms.gov/Medicare/End-Stage-R...
Accesses using superficial autogenous veins have lower complication rates and better long-term patency.44 Sesso RC, Lopes AA, Thomé FS, Lugon JR, Martins CT. Brazilian chronic dialysis survey 2016. J Bras Nefrol. 2017;39(3):261-6. http://dx.doi.org/10.5935/0101-2800.20170049. PMid:29044335.
http://dx.doi.org/10.5935/0101-2800.2017...
Notwithstanding its retrospective nature and the limited number of patients, in this study use of the transposed brachial vein was associated with similar results to other autogenous arteriovenous fistula methods using the customary superficial veins (cephalic and basilic veins). It was observed that 60-day patency was lower with brachial vein transposition when compared with the other autogenous fistulae, although the difference was not statistically significant. This may be related to the low number of patients. Since a trend to lower patency in the brachial vein transposition group was observed, it is possible that statistical significance would have been observed with a larger number of patients. Primary patency at 60 days was 60% with brachial vein transposition, whereas in the other accesses group primary patency was 80%. Several authors have observed similar results for patency. In 2008, Casey et al.1010 Casey K, Tonnessen BH, Mannava K, Noll R, Money SR, Sternbergh WC 3rd. Brachial versus basilic vein dialysis fistulas: a comparison of maturation and patency rates. J Vasc Surg. 2008;47(2):402-6. http://dx.doi.org/10.1016/j.jvs.2007.10.029. PMid:18241763.
http://dx.doi.org/10.1016/j.jvs.2007.10....
compared brachial vein transposition with transposition of the basilic vein, finding 12-month patency rates of 40% for the brachial vein and 50% for the basilic vein. In 2009, Lioupis et al.1212 Lioupis C, Mistry H, Chandak P, Tyrrell M, Valenti D. Autogenous brachial-brachial fistula for vein access. Haemodynamic factors predicting outcome and 1 year clinical data. Eur J Vasc Endovasc Surg. 2009;38(6):770-6. http://dx.doi.org/10.1016/j.ejvs.2009.08.004. PMid:19758825.
http://dx.doi.org/10.1016/j.ejvs.2009.08...
observed 1-year primary patency of 46% in a series of 17 patients. In 2017, Karam et al.99 Karam L, Rawa M, Shoenfeld R, Bourquelot P. Brachial vein transposition is a promising ultimate upper limb autologous arteriovenous angioaccess despite its many pitfalls. J Vasc Surg. 2017;67(1):236-43. http://dx.doi.org/10.1016/j.jvs.2017.05.120. PMid:28733096.
http://dx.doi.org/10.1016/j.jvs.2017.05....
observed 1-year primary patency of 50% in a retrospective study with 64 patients who underwent brachial vein transposition. Patency rates at 2, 3, and 4 years were 42%, 37%, and 27% respectively. In 2017, Pham et al. compared brachial vein transposition with synthetic grafts, observing 1-year primary patency of 62% for brachial vein transposition and 25% for synthetic grafts.11 Pham XD, Kim JJ, Ihenachor EJ, et al. Comparison of brachial artery-brachial vein arteriovenous fistulas with av grafts in patients with poor superficial venous anatomy. J Vasc Surg. 2017;65(2):444-51. http://dx.doi.org/10.1016/j.jvs.2016.09.037. PMid:27986484.
http://dx.doi.org/10.1016/j.jvs.2016.09....
In 2016, Kotsis et al.1313 Kotsis T, Moulakakis KG, Mylonas SN, Kalogeropoulos P, Dellis A, Vasdekis S. Brachial artery-brachial vein fistula for hemodialysis: one- or two-stage procedure-a review. Int J Angiol. 2016;25(1):14-9. http://dx.doi.org/10.1055/s-0035-1558465. PMid:26900307.
http://dx.doi.org/10.1055/s-0035-1558465...
conducted a review covering 380 procedures, observing 12-monthy patency rates ranging from 24% to 77%.
Donor vein diameter of less than 3 mm was the greatest predictor of early failure. Several other authors have observed similar results. In 2009, Lauvao et al.1414 Lauvao LS, Ihnat DM, Goshima KR, Chavez L, Gruessner AC, Mills JL Sr. Vein diameter is the major predictor of fistula maturation. J Vasc Surg. 2009;49(6):1499-504. http://dx.doi.org/10.1016/j.jvs.2009.02.018. PMid:19497513.
http://dx.doi.org/10.1016/j.jvs.2009.02....
analyzed a range of different factors, finding that vein diameter was the greatest predictor of successful construction of definitive vascular accesses for hemodialysis. A 2016 review by Bashar et al.1515 Bashar K, Conlon PJ, Kheirelseid EA, Aherne T, Walsh SR, Leahy A. Arteriovenous fistula in dialysis patients: factors implicated in early and late AVF maturation failure. Surgeon. 2016;14(5):294-300. http://dx.doi.org/10.1016/j.surge.2016.02.001. PMid:26988630.
http://dx.doi.org/10.1016/j.surge.2016.0...
also highlighted the importance of using donor veins with adequate caliber and reported a directly proportional relationship between vein caliber and patency.
Patients who underwent brachial vein transposition had undergone a higher number of previous fistula surgeries when compared with those who underwent other surgical methods employing autologous veins. Forty percent of the patients who had brachial vein transposition had already had prior surgery to construct other types of access, compared with 22% in the other accesses group. In 2009, Lioupis et al.1212 Lioupis C, Mistry H, Chandak P, Tyrrell M, Valenti D. Autogenous brachial-brachial fistula for vein access. Haemodynamic factors predicting outcome and 1 year clinical data. Eur J Vasc Endovasc Surg. 2009;38(6):770-6. http://dx.doi.org/10.1016/j.ejvs.2009.08.004. PMid:19758825.
http://dx.doi.org/10.1016/j.ejvs.2009.08...
observed that 53% of patients who underwent brachial vein transposition had undergone prior surgery for construction of definitive hemodialysis access. In a 2017 study comparing brachial vein transposition to arteriovenous prostheses, Pham et al.11 Pham XD, Kim JJ, Ihenachor EJ, et al. Comparison of brachial artery-brachial vein arteriovenous fistulas with av grafts in patients with poor superficial venous anatomy. J Vasc Surg. 2017;65(2):444-51. http://dx.doi.org/10.1016/j.jvs.2016.09.037. PMid:27986484.
http://dx.doi.org/10.1016/j.jvs.2016.09....
observed that 28% of the patients who underwent brachial vein transposition had had prior surgery to construct definitive accesses. These findings are to be expected, since in this study, for patients to be allocated to brachial vein transposition, they should not have superficial veins with diameters exceeding 3 mm. Consequently, patients who had already undergone a previous procedure for construction of definitive access were selected for the brachial vein transposition group.
Postoperative edema of the upper limb was observed 7 days after the operation in 20% of the patients who had brachial vein transposition. Patients who underwent other methods of autogenous access construction did not exhibit edema during the same period. Edema had resolved completely by 30 days. This is a very common finding, according to published data. In 2008, Casey et al.1010 Casey K, Tonnessen BH, Mannava K, Noll R, Money SR, Sternbergh WC 3rd. Brachial versus basilic vein dialysis fistulas: a comparison of maturation and patency rates. J Vasc Surg. 2008;47(2):402-6. http://dx.doi.org/10.1016/j.jvs.2007.10.029. PMid:18241763.
http://dx.doi.org/10.1016/j.jvs.2007.10....
published a retrospective study comparing transposition of the basilic vein to brachial vein transposition, reporting 5.8% edema in the group that underwent brachial vein transposition. In 2005, Angle and Chandra1616 Angle N, Chandra A. The two-stage brachial artery-brachial vein autogenous fistula for hemodialysis: an alternative autogenous option for hemodialysis access. J Vasc Surg. 2005;42(4):806-10. http://dx.doi.org/10.1016/j.jvs.2005.05.045. PMid:16242575.
http://dx.doi.org/10.1016/j.jvs.2005.05....
published a study of 20 patients who underwent brachial vein transposition, observing edema in 5% of them. In 2007, Elwakeel et al.1717 Elwakeel HA, Saad EM, Elkiran YM, Awad I. Unusual vascular access for hemodialysis: transposed venae comitante of the brachial artery. Ann Vasc Surg. 2007;21(5):560-3. http://dx.doi.org/10.1016/j.avsg.2007.03.026. PMid:17823039.
http://dx.doi.org/10.1016/j.avsg.2007.03...
conducted a study with 21 patients who underwent brachial vein transposition, observing edema in 19%. In a 2009 study with 17 patients, Lioupis et al.1212 Lioupis C, Mistry H, Chandak P, Tyrrell M, Valenti D. Autogenous brachial-brachial fistula for vein access. Haemodynamic factors predicting outcome and 1 year clinical data. Eur J Vasc Endovasc Surg. 2009;38(6):770-6. http://dx.doi.org/10.1016/j.ejvs.2009.08.004. PMid:19758825.
http://dx.doi.org/10.1016/j.ejvs.2009.08...
observed edema in 18%. In 2009, Jennings et al.1818 Jennings WC, Sideman MJ, Taubman KE, Broughan TA. Brachial vein transposition arteriovenous fistulas for hemodialysis access. J Vasc Surg. 2009;50(5):1121-5, discussion 1125-6. http://dx.doi.org/10.1016/j.jvs.2009.07.077. PMid:19782506.
http://dx.doi.org/10.1016/j.jvs.2009.07....
published a review including 53 patients, reporting postoperative edema in 7%. In 2006, Dorobantu et al.1919 Dorobantu LF, Stiru O, Iliescu VA, Novelli E. The brachio-brachial arteriovenous fistula: a new method in patients without a superficial venous system in the upper limb. J Vasc Access. 2006;7(2):87-9. http://dx.doi.org/10.1177/112972980600700209.
http://dx.doi.org/10.1177/11297298060070...
observed postoperative edema in 34.6% of a series of 33 patients. These findings are to be expected since the brachial vein plays an important role in venous drainage of the arm. However, this edema is not persistent, possibly because of the dense way of venous collaterals in the upper limb.
Transposition of the brachial vein has proven an alternative to using arteriovenous grafts. During the study period, no surgery was performed using prosthetic grafts. Some authors have reported similar results, with reduced use of grafts.99 Karam L, Rawa M, Shoenfeld R, Bourquelot P. Brachial vein transposition is a promising ultimate upper limb autologous arteriovenous angioaccess despite its many pitfalls. J Vasc Surg. 2017;67(1):236-43. http://dx.doi.org/10.1016/j.jvs.2017.05.120. PMid:28733096.
http://dx.doi.org/10.1016/j.jvs.2017.05....
,1111 Center for Medicare & Medicaid Services. Questions and answers. Baltimore: CMS.gov; 2004 [cited novembro de 2019 26]. Available from: https://www.cms.gov/Medicare/End-Stage-Renal-Disease/ESRDQualityImproveInit/downloads/FFFAQs.pdf
https://www.cms.gov/Medicare/End-Stage-R...
,1212 Lioupis C, Mistry H, Chandak P, Tyrrell M, Valenti D. Autogenous brachial-brachial fistula for vein access. Haemodynamic factors predicting outcome and 1 year clinical data. Eur J Vasc Endovasc Surg. 2009;38(6):770-6. http://dx.doi.org/10.1016/j.ejvs.2009.08.004. PMid:19758825.
http://dx.doi.org/10.1016/j.ejvs.2009.08...
,1717 Elwakeel HA, Saad EM, Elkiran YM, Awad I. Unusual vascular access for hemodialysis: transposed venae comitante of the brachial artery. Ann Vasc Surg. 2007;21(5):560-3. http://dx.doi.org/10.1016/j.avsg.2007.03.026. PMid:17823039.
http://dx.doi.org/10.1016/j.avsg.2007.03...
,1919 Dorobantu LF, Stiru O, Iliescu VA, Novelli E. The brachio-brachial arteriovenous fistula: a new method in patients without a superficial venous system in the upper limb. J Vasc Access. 2006;7(2):87-9. http://dx.doi.org/10.1177/112972980600700209.
http://dx.doi.org/10.1177/11297298060070...
Other authors have compared the results of brachial vein transposition with those of arteriovenous grafts for hemodialysis. In 2017, Pham et al.11 Pham XD, Kim JJ, Ihenachor EJ, et al. Comparison of brachial artery-brachial vein arteriovenous fistulas with av grafts in patients with poor superficial venous anatomy. J Vasc Surg. 2017;65(2):444-51. http://dx.doi.org/10.1016/j.jvs.2016.09.037. PMid:27986484.
http://dx.doi.org/10.1016/j.jvs.2016.09....
compared 29 patients who underwent superficial displacement of the brachial vein and 36 patients who underwent construction of prosthetic arteriovenous access. They observed greater primary patency, at 62%, in the group with brachial vein transposition, compared with 25% in the group with grafts.11 Pham XD, Kim JJ, Ihenachor EJ, et al. Comparison of brachial artery-brachial vein arteriovenous fistulas with av grafts in patients with poor superficial venous anatomy. J Vasc Surg. 2017;65(2):444-51. http://dx.doi.org/10.1016/j.jvs.2016.09.037. PMid:27986484.
http://dx.doi.org/10.1016/j.jvs.2016.09....
However, Torina et al.,2020 Torina PJ, Westheimer EF, Schanzer HR. Brachial vein transposition arteriovenous fistula: is it an acceptable option for chronic dialysis vascular access? J Vasc Access. 2008;9(1):39-44. http://dx.doi.org/10.1177/112972980800900107. PMid:18379979.
http://dx.doi.org/10.1177/11297298080090...
in a 2008 retrospective study with 149 patients observed 25% 1-year primary patency for patients who underwent brachial vein transposition and 50% for patients with access using grafts. In 2009, Lioupis et al.1212 Lioupis C, Mistry H, Chandak P, Tyrrell M, Valenti D. Autogenous brachial-brachial fistula for vein access. Haemodynamic factors predicting outcome and 1 year clinical data. Eur J Vasc Endovasc Surg. 2009;38(6):770-6. http://dx.doi.org/10.1016/j.ejvs.2009.08.004. PMid:19758825.
http://dx.doi.org/10.1016/j.ejvs.2009.08...
also compared use of an arteriovenous prosthesis to brachial vein transposition in a retrospective study with 108 patients. Primary patency at 18 months was lower in the brachial vein transposition group, at 27%, compared with 55% for prosthetic arteriovenous access. In both studies, reported brachial vein transposition patency was substantially lower than rates reported by other authors.11 Pham XD, Kim JJ, Ihenachor EJ, et al. Comparison of brachial artery-brachial vein arteriovenous fistulas with av grafts in patients with poor superficial venous anatomy. J Vasc Surg. 2017;65(2):444-51. http://dx.doi.org/10.1016/j.jvs.2016.09.037. PMid:27986484.
http://dx.doi.org/10.1016/j.jvs.2016.09....
,99 Karam L, Rawa M, Shoenfeld R, Bourquelot P. Brachial vein transposition is a promising ultimate upper limb autologous arteriovenous angioaccess despite its many pitfalls. J Vasc Surg. 2017;67(1):236-43. http://dx.doi.org/10.1016/j.jvs.2017.05.120. PMid:28733096.
http://dx.doi.org/10.1016/j.jvs.2017.05....
,1111 Center for Medicare & Medicaid Services. Questions and answers. Baltimore: CMS.gov; 2004 [cited novembro de 2019 26]. Available from: https://www.cms.gov/Medicare/End-Stage-Renal-Disease/ESRDQualityImproveInit/downloads/FFFAQs.pdf
https://www.cms.gov/Medicare/End-Stage-R...
12 Lioupis C, Mistry H, Chandak P, Tyrrell M, Valenti D. Autogenous brachial-brachial fistula for vein access. Haemodynamic factors predicting outcome and 1 year clinical data. Eur J Vasc Endovasc Surg. 2009;38(6):770-6. http://dx.doi.org/10.1016/j.ejvs.2009.08.004. PMid:19758825.
http://dx.doi.org/10.1016/j.ejvs.2009.08...
-1313 Kotsis T, Moulakakis KG, Mylonas SN, Kalogeropoulos P, Dellis A, Vasdekis S. Brachial artery-brachial vein fistula for hemodialysis: one- or two-stage procedure-a review. Int J Angiol. 2016;25(1):14-9. http://dx.doi.org/10.1055/s-0035-1558465. PMid:26900307.
http://dx.doi.org/10.1055/s-0035-1558465...
The single intervention surgical technique was chosen, as described by Bazan and Schanzer.88 Bazan HA, Schanzer H. Transposition of the brachial vein: a new source for autologous arteriovenous fistulas. J Vasc Surg. 2004;40(1):184-6. http://dx.doi.org/10.1016/j.jvs.2004.03.044. PMid:15218484.
http://dx.doi.org/10.1016/j.jvs.2004.03....
Two-stage surgery for superficial transposition of the brachial vein has been described by several authors. In 2016, Kotsis et al.1313 Kotsis T, Moulakakis KG, Mylonas SN, Kalogeropoulos P, Dellis A, Vasdekis S. Brachial artery-brachial vein fistula for hemodialysis: one- or two-stage procedure-a review. Int J Angiol. 2016;25(1):14-9. http://dx.doi.org/10.1055/s-0035-1558465. PMid:26900307.
http://dx.doi.org/10.1055/s-0035-1558465...
published a review in which they observed lower patency among patients who underwent single-stage surgery. One disadvantage of the one-step approach is related to the small diameter of the brachial veins and their structure, which is often delicate and irregular. The fixed anatomy of the brachial vein makes it susceptible to injury during transposition, and this can cause postoperative bleeding, hematoma, stenosis, and thrombosis.1616 Angle N, Chandra A. The two-stage brachial artery-brachial vein autogenous fistula for hemodialysis: an alternative autogenous option for hemodialysis access. J Vasc Surg. 2005;42(4):806-10. http://dx.doi.org/10.1016/j.jvs.2005.05.045. PMid:16242575.
http://dx.doi.org/10.1016/j.jvs.2005.05....
A similar line of reasoning can be applied to superficial transposition of the basilic vein. In 2013, Vrakas et al.2121 Vrakas G, Defigueiredo F, Turner S, Jones C, Taylor J, Calder F. A comparison of the outcomes of one-stage and two-stage brachiobasilic arteriovenous fistulas. J Vasc Surg. 2013;58(5):1300-4. http://dx.doi.org/10.1016/j.jvs.2013.05.030. PMid:23810301.
http://dx.doi.org/10.1016/j.jvs.2013.05....
described a 3.2 times greater risk of access failure among patients who underwent single-stage superficial transposition of the basilic vein. The choice of single-stage surgery observed in this study was because of the profile of the patients treated by the public healthcare system. These patients face difficulties that hinder access to health services and a second procedure could have been impossible for some of them.
This study is subject to certain limitations that should be mentioned. It is a retrospective study with a limited follow-up period and a small number of patients. However, the subject is still an ongoing debate in the literature, on which few studies have been published. There is still a knowledge gap in relation to comparisons between brachial vein transposition and use of arteriovenous prostheses. Additional studies are still needed, with larger patient samples and, preferably, prospective and randomized designs.
-
How to cite: Castro-Santos G, Salles AG, Anjos GS, Procópio RJ, Navarro TP. Brachial vein transposition: an alternative to hemodialysis arteriovenous graft. J Vasc Bras. 2019;18:e20190077. https://doi.org/10.1590/1677-5449.190077
-
Financial support: None.
-
The study was carried out at Hospital das Clínicas, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, (MG), Brazil.
REFERÊNCIAS
-
1Pham XD, Kim JJ, Ihenachor EJ, et al. Comparison of brachial artery-brachial vein arteriovenous fistulas with av grafts in patients with poor superficial venous anatomy. J Vasc Surg. 2017;65(2):444-51. http://dx.doi.org/10.1016/j.jvs.2016.09.037 PMid:27986484.
» http://dx.doi.org/10.1016/j.jvs.2016.09.037 -
2Morisson B, Araújo AL, Harduin LO, et al. A pilot study comparing bovine mesenteric artery and expanded polytetrafluoroethylene grafts as non-autogenous hemodialysis options. J Vasc Bras. 2018;17(4):303-9. http://dx.doi.org/10.1590/1677-5449.007117 PMid:30787948.
» http://dx.doi.org/10.1590/1677-5449.007117 -
3National Kidney Foundation. 2006 updates clinical practice guidelines and recommendations. New York: KDOQI [cited 2019 Maio 26]. Available from: https://www.kidney.org/sites/default/files/docs/12-50-0210_jag_dcp_guidelines-pd_oct06_sectionb_ofc.pdf
» https://www.kidney.org/sites/default/files/docs/12-50-0210_jag_dcp_guidelines-pd_oct06_sectionb_ofc.pdf -
4Sesso RC, Lopes AA, Thomé FS, Lugon JR, Martins CT. Brazilian chronic dialysis survey 2016. J Bras Nefrol. 2017;39(3):261-6. http://dx.doi.org/10.5935/0101-2800.20170049 PMid:29044335.
» http://dx.doi.org/10.5935/0101-2800.20170049 -
5Perera GB, Mueller MP, Kubaska SM, Wilson SE, Lawrence PF, Fujitani RM. Superiority of autogenous arteriovenous hemodialysis access: maintenance of function with fewer secondary interventions. Ann Vasc Surg. 2004;18(1):66-73. http://dx.doi.org/10.1007/s10016-003-0094-y PMid:14727162.
» http://dx.doi.org/10.1007/s10016-003-0094-y -
6Roy-Chaudhury P, Sukhatme VP, Cheung AK. Cheung hemodialysis vascular access dysfunction: a cellular and molecular viewpoint. J Am Soc Nephrol. 2006;17(4):1112-27. http://dx.doi.org/10.1681/ASN.2005050615 PMid:16565259.
» http://dx.doi.org/10.1681/ASN.2005050615 -
7Koontz PG Jr, Helling TS. Subcutaneous brachial vein arteriove- nous fistula for chronic hemodialysis. World J Surg. 1983;7(5):672-4. http://dx.doi.org/10.1007/BF01655353 PMid:6636812.
» http://dx.doi.org/10.1007/BF01655353 -
8Bazan HA, Schanzer H. Transposition of the brachial vein: a new source for autologous arteriovenous fistulas. J Vasc Surg. 2004;40(1):184-6. http://dx.doi.org/10.1016/j.jvs.2004.03.044 PMid:15218484.
» http://dx.doi.org/10.1016/j.jvs.2004.03.044 -
9Karam L, Rawa M, Shoenfeld R, Bourquelot P. Brachial vein transposition is a promising ultimate upper limb autologous arteriovenous angioaccess despite its many pitfalls. J Vasc Surg. 2017;67(1):236-43. http://dx.doi.org/10.1016/j.jvs.2017.05.120 PMid:28733096.
» http://dx.doi.org/10.1016/j.jvs.2017.05.120 -
10Casey K, Tonnessen BH, Mannava K, Noll R, Money SR, Sternbergh WC 3rd. Brachial versus basilic vein dialysis fistulas: a comparison of maturation and patency rates. J Vasc Surg. 2008;47(2):402-6. http://dx.doi.org/10.1016/j.jvs.2007.10.029 PMid:18241763.
» http://dx.doi.org/10.1016/j.jvs.2007.10.029 -
11Center for Medicare & Medicaid Services. Questions and answers. Baltimore: CMS.gov; 2004 [cited novembro de 2019 26]. Available from: https://www.cms.gov/Medicare/End-Stage-Renal-Disease/ESRDQualityImproveInit/downloads/FFFAQs.pdf
» https://www.cms.gov/Medicare/End-Stage-Renal-Disease/ESRDQualityImproveInit/downloads/FFFAQs.pdf -
12Lioupis C, Mistry H, Chandak P, Tyrrell M, Valenti D. Autogenous brachial-brachial fistula for vein access. Haemodynamic factors predicting outcome and 1 year clinical data. Eur J Vasc Endovasc Surg. 2009;38(6):770-6. http://dx.doi.org/10.1016/j.ejvs.2009.08.004 PMid:19758825.
» http://dx.doi.org/10.1016/j.ejvs.2009.08.004 -
13Kotsis T, Moulakakis KG, Mylonas SN, Kalogeropoulos P, Dellis A, Vasdekis S. Brachial artery-brachial vein fistula for hemodialysis: one- or two-stage procedure-a review. Int J Angiol. 2016;25(1):14-9. http://dx.doi.org/10.1055/s-0035-1558465 PMid:26900307.
» http://dx.doi.org/10.1055/s-0035-1558465 -
14Lauvao LS, Ihnat DM, Goshima KR, Chavez L, Gruessner AC, Mills JL Sr. Vein diameter is the major predictor of fistula maturation. J Vasc Surg. 2009;49(6):1499-504. http://dx.doi.org/10.1016/j.jvs.2009.02.018 PMid:19497513.
» http://dx.doi.org/10.1016/j.jvs.2009.02.018 -
15Bashar K, Conlon PJ, Kheirelseid EA, Aherne T, Walsh SR, Leahy A. Arteriovenous fistula in dialysis patients: factors implicated in early and late AVF maturation failure. Surgeon. 2016;14(5):294-300. http://dx.doi.org/10.1016/j.surge.2016.02.001 PMid:26988630.
» http://dx.doi.org/10.1016/j.surge.2016.02.001 -
16Angle N, Chandra A. The two-stage brachial artery-brachial vein autogenous fistula for hemodialysis: an alternative autogenous option for hemodialysis access. J Vasc Surg. 2005;42(4):806-10. http://dx.doi.org/10.1016/j.jvs.2005.05.045 PMid:16242575.
» http://dx.doi.org/10.1016/j.jvs.2005.05.045 -
17Elwakeel HA, Saad EM, Elkiran YM, Awad I. Unusual vascular access for hemodialysis: transposed venae comitante of the brachial artery. Ann Vasc Surg. 2007;21(5):560-3. http://dx.doi.org/10.1016/j.avsg.2007.03.026 PMid:17823039.
» http://dx.doi.org/10.1016/j.avsg.2007.03.026 -
18Jennings WC, Sideman MJ, Taubman KE, Broughan TA. Brachial vein transposition arteriovenous fistulas for hemodialysis access. J Vasc Surg. 2009;50(5):1121-5, discussion 1125-6. http://dx.doi.org/10.1016/j.jvs.2009.07.077 PMid:19782506.
» http://dx.doi.org/10.1016/j.jvs.2009.07.077 -
19Dorobantu LF, Stiru O, Iliescu VA, Novelli E. The brachio-brachial arteriovenous fistula: a new method in patients without a superficial venous system in the upper limb. J Vasc Access. 2006;7(2):87-9. http://dx.doi.org/10.1177/112972980600700209
» http://dx.doi.org/10.1177/112972980600700209 -
20Torina PJ, Westheimer EF, Schanzer HR. Brachial vein transposition arteriovenous fistula: is it an acceptable option for chronic dialysis vascular access? J Vasc Access. 2008;9(1):39-44. http://dx.doi.org/10.1177/112972980800900107 PMid:18379979.
» http://dx.doi.org/10.1177/112972980800900107 -
21Vrakas G, Defigueiredo F, Turner S, Jones C, Taylor J, Calder F. A comparison of the outcomes of one-stage and two-stage brachiobasilic arteriovenous fistulas. J Vasc Surg. 2013;58(5):1300-4. http://dx.doi.org/10.1016/j.jvs.2013.05.030 PMid:23810301.
» http://dx.doi.org/10.1016/j.jvs.2013.05.030
Publication Dates
-
Publication in this collection
28 Nov 2019 -
Date of issue
2019
History
-
Received
10 July 2019 -
Accepted
15 Sept 2019