Abstract
Objective:
To evaluate the efficiency of the contact lens adaptation in relation to the improvement of visual acuity in patients with keratoconus.
Methods:
A retrospective study of 175 patients (326 eyes) with keratoconus was carried out from March 2004 to June 2015. Data on sex, age, number of adapted eyes, keratoconus severity, and visual acuity with glasses and contact lenses were collected.
Results:
Of the classified eyes, 267 (81.9%) had moderate keratoconus (45 to 52D). The most frequent age group was 10-39 years of age (84%) and the success rate at the end of treatment was 92.3% (good or satisfactory visual acuity).
Conclusion:
Adaptation of contact lenses was effective in providing important improvement of visual acuity in patients with keratoconus.
Keywords:
Keratoconus; Cornea; Visual acuity; Observational Study; Eyeglasses
Resumo
Objetivo:
Avaliar a eficácia na adaptação de lentes de contato em relação à melhora da acuidade visual em pacientes portadores de ceratocone.
Métodos:
Foi realizado um estudo retrospectivo, através de revisão de prontuários médicos, em 175 pacientes (326 olhos) portadores de ceratocone, atendidos no período de março/2004 a junho/2015. Foram coletados os dados sobre sexo, idade, número de olhos adaptados, severidade do ceratocone e acuidade visual com óculos e com lentes de contato.
Resultados:
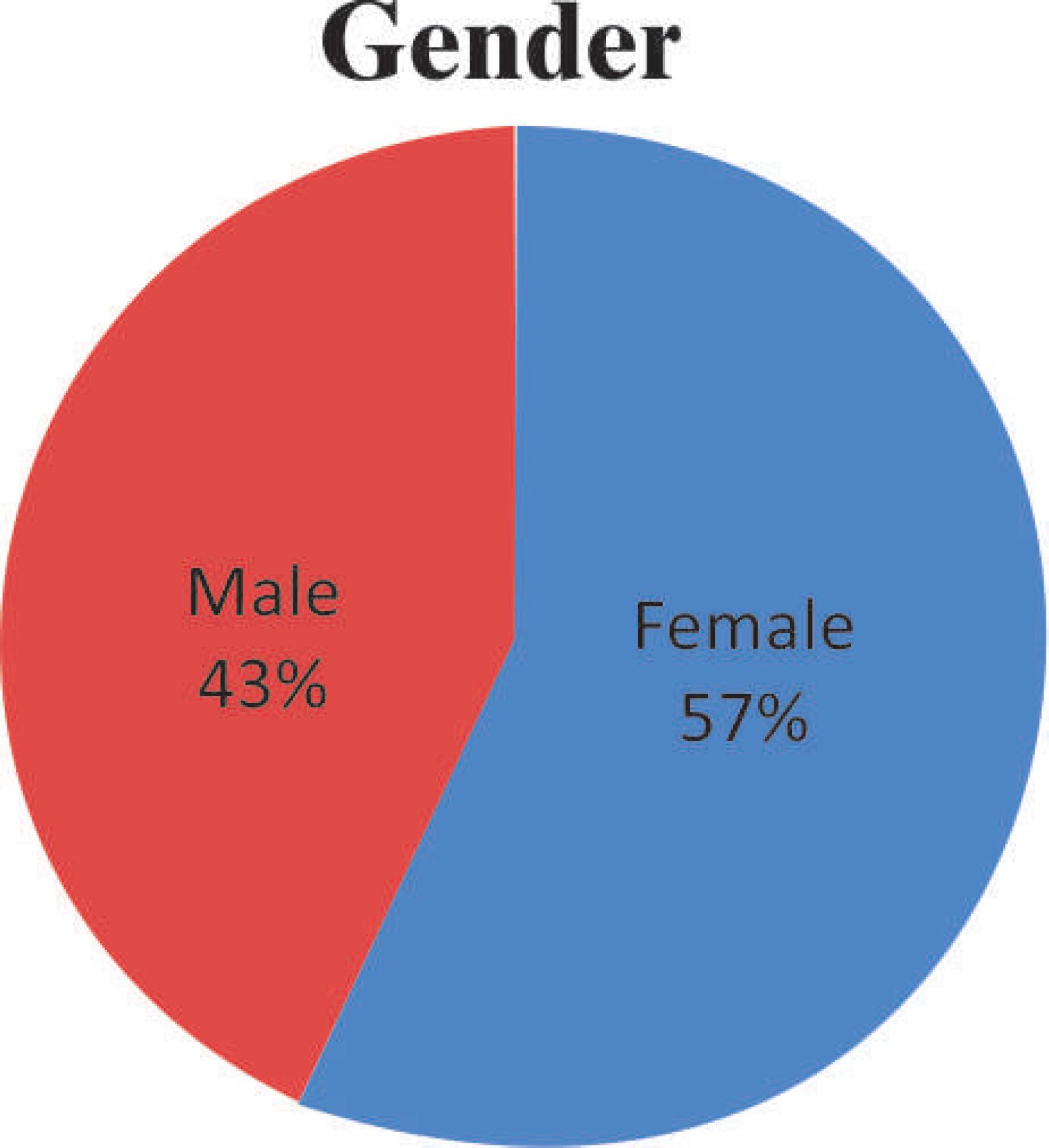
Dos pacientes avaliados, 100 pacientes (57,4%) eram do sexo feminino e 75 pacientes (42,6%) do sexo masculino. Dos olhos classificados, 267 (81,9%) tinham ceratocone moderado (45 a 52D). A faixa etária mais frequente foi de 10-39 anos (84%) e a taxa de sucesso ao fim do tratamento foi de 92,3% (acuidade visual boa ou satisfatória).
Conclusão:
A adaptação de lentes de contato mostrou-se eficaz em proporcionar importante melhora da acuidade visual em pacientes portadores de ceratocone.
Descritores:
Ceratocone; Córnea; Acuidade visual; Estudo observacional; Óculos
Introduction
Keratoconus is a noninflammatory disorder of the cornea of undetermined etiology and characterized by stromal thinning and protrusion, causing the cornea to have a conical shape. The onset of the disease occurs around puberty, with slow subsequent progression to the third or fourth decade of life, when it usually stops, although ectasia may stop progressing at any time. (11 Kanski JJ. Oftalmologia clínica: Uma abordagem sistemática. Rio de Janeiro: Elsevier, 2008.)
The prevalence of keratoconus in the general population is relatively high, although the definition of cases varies in different series. There is a wide range of prevalence reported in the general population, ranging from 50 to 230 per 100,000 population. (22 Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297-319.,33 Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293-322.) There is no difference in incidence and prevalence between genders. (33 Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293-322.,44 Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: current scenario. Br J Ophthalmol. 2011;95(8):1044-50.) Some evidence suggests a higher incidence in Asians from the Indian subcontinent. (55 Georgiou T, Funnell CL, Cassels-Brown A, O'Conor R. Influence of ethnic origin on the incidence of keratoconus and associated atopic disease in Asians and white patients. Eye (Lond). 2004;18(4):379-83.,66 Pearson AR, Soneji B, Sarvananthan N, Sandford-Smith JH. Does ethnic origin influence the incidence or severity of keratoconus? Eye (Lond). 2000;14(Pt 4):625-8.)
The role of heredity is not clearly defined, and most patients do not present family occurrence of the disease. The descendants of keratoconus patients are affected in 10% of cases, and the dominant autosomal transmission pattern with incomplete penetrance was proposed. (11 Kanski JJ. Oftalmologia clínica: Uma abordagem sistemática. Rio de Janeiro: Elsevier, 2008.)
Both eyes are affected in almost all cases. Corneal topography and pachymetry-tomography evaluations are essential for the diagnosis and follow-up in keratoconus patients. (77 Módis L Jr, Németh G, Szalai E, Flaskó Z, Seitz B. Scanning-slit topography in patients with keratoconus. Int J Ophthalmol. 2017;10(11):1686-92.,88 Crawford AZ, Patel DV, McGhee CN. Comparison and repeatability of keratometric and corneal power measurements obtained by Orbscan II, Pentacam, and Galilei corneal tomography systems. Am J Ophthalmol. 2013;156(1):53-60.) About 50% of normal contralateral eyes evolve to keratoconus in 16 years, with the highest risk being in the first 6 years of the disease. (11 Kanski JJ. Oftalmologia clínica: Uma abordagem sistemática. Rio de Janeiro: Elsevier, 2008.)
In clinical management, the main objective is to allow keratoconus patients to have an optical correction enabling good visual acuity. At the onset of the disease, correction is made with glasses, and as progression occurs with increased irregular astigmatism, contact lenses may be necessary to promote an improvement of visual acuity. Most keratoconus patients wear contact lenses for a long period of time. (99 Smiddy WE, Hamburg TR, Kracher GP, Stark WJ. Keratoconus. Contact lens or keratoplasty? Ophthalmology. 1988;95(4):487-92.)
Rigid contact lenses are indicated for irregular astigmatism by neutralizing the corneal surface, and advances in its designs and materials have provided an increase in the number of well-adapted keratoconus patients. In one series, the main reason for failure of contact lens treatment resulting in the need for keratoplasty was inadequate visual acuity (43%), followed by contact lens intolerance (32%), frequent lens displacement (17%), and peripheral thinning (12%). (1010 Dana MR, Putz JL, Viana MA, Sugar J, McMahon TT. Contact lens dailure in keratoconus management. Ophthalmology. 1992;99(8):1187-92.)
Methods
A retrospective study was carried out through the review of medical records in 795 patients, with 274 of them having keratoconus and being treated at the Contact Lens Department of Instituto Benjamin Constant from March 2004 to June 2015. We selected 175 patients (326 eyes) who maintained the minimum follow-up of 12 months in our service with good adaptation to contact lenses. Adaptation of the contact lens was considered successful, allowing visual acuity improvement, comfort and time of use greater than 6 hours in the eyes with at least two months of follow-up.
Patients with other ocular conditions or who had undergone previous ocular surgical procedures were excluded from the study.
Rigid monochrome corneal contact lenses with special designs, rigid scleral lenses, special gelatinous contact lenses, and rigid corneal lenses on gelatinous lenses (knight fitting) were adapted.
Data were collected on gender, age, number of adapted eyes, keratoconus severity, and visual acuity (VA) with glasses and after adaptation of contact lenses.
The keratoconus was classified with the help of computerized keratoscopy according to the maximum corneal curvature measurements, such as: incipient (up to 45D), moderate (above 45D to 52D), advanced (above 52D to 60D), and severe (above 60D). (1111 Duque WD, Rehder JR, Leca RG. Avaliação da eficácia na adaptação de lentes de contato com relação à melhora visual em pacientes portadores de ceratocone. Rev Bras Oftalmol. 2012;71(5):313-6.,1212 Schirmbeck T, Paula JS, Martin LF, Crósio Filho H, Romão E. Eficácia e baixo custo no tratamento do ceratocone com o uso de lentes de contato rígidas gás-permeáveis. Arq Bras Oftalmol. 2005;68(2):219-22.)
Visual acuity (decimal scale) was classified according to the Snellen optotype table as good (up to 0.6), satisfactory (below 0.6 to 0.3), low (below 0.3 up to 0.1), and very low (worse than 0.1). Patients who had satisfactory or good visual acuity after adapting to contact lenses were considered successful in adaptation.
For the descriptive analysis a frequency measure of the simple prevalence type was used, besides the use of measures of central tendency and dispersion. For the comparative analysis, the Student’s t test was used for numerical variables, the chi-square test for categorical variables with a significance level of 95% (p<0.05).
Results
Adaptation was performed in 326 eyes of the 175 patients evaluated, with 100 patients (57.4%) being females and 75 patients (42.6%) males (Figure 1).
Of the total number of cases of keratoconus patients included in the present study, 1 patient was in the age group from 0-9 years (0.6%), 49 patients (28%) from 10-19 years, 98 patients (56%) from 20-39 years, 26 patients (14.8%) from 40-64 years, and 1 patient (0.6%) > 64 years (Figure 2).
The eyes were analyzed and 7 (2.1%) were classified as incipient keratoconus, 267 (81.9%) as moderate, 41 (12.5%) as advanced, and 11 (3.3%) as severe (Figure 3).
Of the adaptations made, 151 (86.2%) were binocular and 24 (13.7%) monocular (Figure 4).
Of the total adapted cases, 262 (80.3%) were with rigid monochrome corneal lenses, 56 (17, 1%) with rigid contact lenses with special designs, 3 (0.92%) with scleral rigid lenses, 2 with special gelatinous contact lenses, and 1 knight adaptation (Figure 5).
Good visual acuity with glasses was observed in 34 (10.4%) eyes; satisfactory visual acuity in 164 (50.3%) eyes; low visual acuity in 97 (29.7%) eyes, and very low visual acuity in 31 eyes (9.5%).
Most of the adapted eyes had an improvement in the visual acuity after adaptation to the lenses, only 1 (0.3%) remained with very low visual acuity, and 24 eyes (7.36%) remained with low visual acuity. The eyes with satisfactory or good visual acuity which were considered successful in the treatment accounted for a percentage of 92.3% of the adapted cases, being this value statistically significant (p value <0.05) (Figure 6).
Discussion
The adaptation of rigid contact lenses is the main option for visual rehabilitation in keratoconus patients when the glasses no longer provide satisfactory visual acuity. High order aberrations or irregular astigmatism cannot be corrected with glasses or GCL. Therefore, RCL are used to improve visual acuity in keratoconus patients.
When keratoconus patients use RCL, the higher order aberrations derived from the anterior surface of the cornea are relieved, resulting in higher quality of vision with RCL than with glasses in the eyes with keratoconus. However, recent studies of higher order aberrations in keratoconus patients have revealed a problem of irregular residual astigmatism. Since there is a problem in the correction of higher order aberrations with GCL, it was necessary to develop optical surfaces customized for GCL with a design based on wavefront aberrometry. It is difficult to prescribe a fully customized GCL for each patient due to prohibitive manufacturing costs. (1313 Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT et al. Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci. 1998;39(13):2537-46.
14 Lim N, Vogt U. Characteristics and functional outcomes of 130 patients with keratoconus attending a specialist contact lens clinic. Eye (Lond). 2002;16(1):54-9.
15 Kosaki R, Maeda N, Bessho K, Hori Y, Nishida K, Suzaki A et al. Magnitude and orientation of Zernike terms in patients with keratoconus. Invest Ophthalmol Vis Sci. 2007;48(7):3062-8.
16 Negishi K, Kumanomido T, Utsumi Y, Tsubota K. Effect of higher-order aberrations on visual function in keratoconic eyes with a rigid gas permeable contact lens. Am J Ophthalmol. 2007;144(6):924-9.
17 Rahman W, Anwar S. An unusual case of keratoconus. J Pediatr Ophthalmol Strabismus. 2006;43(6):373-5.-1818 Li X, Rabinowitz YS, Rasheed K, Yang H. Longitudinal study of the normal eyes in unilateral keratoconus patients. Ophthalmology. 2004;111(3):440-6.)
The prescription of surgical procedures in keratoconus patients should be reserved only for cases of failure to adapt contact lenses. Thus, it is very important for the ophthalmologist to adaptat contact lens to keratoconus patients, as this allows postponing the need for invasive procedures. (1919 Key J, Benett SE. Rigid gas permeable (RGP) extended wear contact lenses. K. RP, Contact lenses: the CLAO guide to basic sience and clinical pratice. Dubuque: Kendal/ Hunt Publishing Company; 1995. p. 51-74.)
The highest prevalence of keratoconus observed in our study ranged from 10 to 39 years, accounting for 84% of the total number of patients. These data are similar to those found in the study by Duque et al., where 74% of patients were in the age group of 11 and 30 years. (1111 Duque WD, Rehder JR, Leca RG. Avaliação da eficácia na adaptação de lentes de contato com relação à melhora visual em pacientes portadores de ceratocone. Rev Bras Oftalmol. 2012;71(5):313-6.) Schirmbeck et al. carried out a study in 2005 to evaluate the relation between the efficacy and cost of gas-permeable rigid contact lenses in the treatment of keratoconus in a total of 126 patients, 68% of whom were in the age group of 11 at 30 years. (1212 Schirmbeck T, Paula JS, Martin LF, Crósio Filho H, Romão E. Eficácia e baixo custo no tratamento do ceratocone com o uso de lentes de contato rígidas gás-permeáveis. Arq Bras Oftalmol. 2005;68(2):219-22.) Fatima et al. revealed that the average age of keratoconus incidence was 24 years. (2020 Fatima T, Acharya MC, Mathur U, Barua P. Demographic profile and visual rehabilitation of patients with keratoconus attending contact lens clinic at a tertiary eye care centre. Cont Lens Anterior Eye. 2010;33(1):19-22.)
The evaluation of keratocellular density in patients with keratoconus made in Turkey in 2011 classified the eyes, with moderate and advanced totaling 71.8% of the total 68 eyes evaluated.21 In India in 2010, eyes classified as moderate and advanced totaled 69.1%. (2121 Kastl PR, Donzis PB, Cole HP 3rd, Rice J, Baldone JA. A 20-year retrospective study of the use of contact lenses in keratoconus. CLAO J. 1987;13(2):102-4.) In the present study, the data found was of 267 cases (81.9%) of moderate keratoconus and 41 cases (12.5%) of advanced keratoconus.
In the medical literature, we can find several examples of successful contact lens adaptations in keratoconus patients, corroborating with the data found in the present study, in which 92.3% of the adapted cases were successful in the treatment. In a retrospective study carried out by Kastl over a 20-year period, 95% of keratoconus patients had successful lens adaptation, with 81% having visual acuity equal to or greater than 0.5. (2121 Kastl PR, Donzis PB, Cole HP 3rd, Rice J, Baldone JA. A 20-year retrospective study of the use of contact lenses in keratoconus. CLAO J. 1987;13(2):102-4.) In the study by Schirmbeck et al. the success in adapting contact lens to the improvement of visual acuity was 86.19%. (1212 Schirmbeck T, Paula JS, Martin LF, Crósio Filho H, Romão E. Eficácia e baixo custo no tratamento do ceratocone com o uso de lentes de contato rígidas gás-permeáveis. Arq Bras Oftalmol. 2005;68(2):219-22.) In another study carried out in India by Fatima et al. in 2010, 79.5% of a total of 142 eyes were successful regarding acuity after contact lens adaptation.20 Timucin et al. evaluated in Turkey in 2011 that approximately 85% of the eyes analyzed went from vision considered subnormal or legal blindness for a satisfactory visual acuity after adaptation of contact lenses. (2222 Timucin OB, Karadag MF, Cinal A. Assessment of keratocyte density in patients with keratoconus not using contact lenses. Cornea. 2011;30(5):576-9.) In a Brazilian study carried out in São Paulo, 93% of patients were successful with contact lenses at the end of treatment (final visual acuity better than 0.3). (1111 Duque WD, Rehder JR, Leca RG. Avaliação da eficácia na adaptação de lentes de contato com relação à melhora visual em pacientes portadores de ceratocone. Rev Bras Oftalmol. 2012;71(5):313-6.)
In the study carried out by Cukierman et al. in the period from 2000 to 2003, in the majority of cases of keratoconus (94.29%) there was adaptation of rigid monochrome contact lenses, and in only 5.71% of cases special design lenses. (2323 Cukierman E, Boldrim E. Perfil do setor de lentes de contato da Santa Casa de Misericórida do Rio de Janeiro. Rev Bras Oftalmol. 2005;64(2):77-82.) However, in the last 10 years of the present study, there was a great development of materials and designs for the contact lenses available on the market, providing a change in the types of contact lens used, with better adaptation in the majority of cases of keratoconus, allowing delay or even avoiding the indication of surgical procedures in the most severe cases. (2222 Timucin OB, Karadag MF, Cinal A. Assessment of keratocyte density in patients with keratoconus not using contact lenses. Cornea. 2011;30(5):576-9.)
Conclusion
The adaptation of contact lenses proved to be effective in providing important improvement of visual acuity in keratoconus patients, with their practice and mastery by the ophthalmologist being very important.
-
Institution: Instituto Benjamin Constant
References
-
1Kanski JJ. Oftalmologia clínica: Uma abordagem sistemática. Rio de Janeiro: Elsevier, 2008.
-
2Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297-319.
-
3Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293-322.
-
4Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: current scenario. Br J Ophthalmol. 2011;95(8):1044-50.
-
5Georgiou T, Funnell CL, Cassels-Brown A, O'Conor R. Influence of ethnic origin on the incidence of keratoconus and associated atopic disease in Asians and white patients. Eye (Lond). 2004;18(4):379-83.
-
6Pearson AR, Soneji B, Sarvananthan N, Sandford-Smith JH. Does ethnic origin influence the incidence or severity of keratoconus? Eye (Lond). 2000;14(Pt 4):625-8.
-
7Módis L Jr, Németh G, Szalai E, Flaskó Z, Seitz B. Scanning-slit topography in patients with keratoconus. Int J Ophthalmol. 2017;10(11):1686-92.
-
8Crawford AZ, Patel DV, McGhee CN. Comparison and repeatability of keratometric and corneal power measurements obtained by Orbscan II, Pentacam, and Galilei corneal tomography systems. Am J Ophthalmol. 2013;156(1):53-60.
-
9Smiddy WE, Hamburg TR, Kracher GP, Stark WJ. Keratoconus. Contact lens or keratoplasty? Ophthalmology. 1988;95(4):487-92.
-
10Dana MR, Putz JL, Viana MA, Sugar J, McMahon TT. Contact lens dailure in keratoconus management. Ophthalmology. 1992;99(8):1187-92.
-
11Duque WD, Rehder JR, Leca RG. Avaliação da eficácia na adaptação de lentes de contato com relação à melhora visual em pacientes portadores de ceratocone. Rev Bras Oftalmol. 2012;71(5):313-6.
-
12Schirmbeck T, Paula JS, Martin LF, Crósio Filho H, Romão E. Eficácia e baixo custo no tratamento do ceratocone com o uso de lentes de contato rígidas gás-permeáveis. Arq Bras Oftalmol. 2005;68(2):219-22.
-
13Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT et al. Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci. 1998;39(13):2537-46.
-
14Lim N, Vogt U. Characteristics and functional outcomes of 130 patients with keratoconus attending a specialist contact lens clinic. Eye (Lond). 2002;16(1):54-9.
-
15Kosaki R, Maeda N, Bessho K, Hori Y, Nishida K, Suzaki A et al. Magnitude and orientation of Zernike terms in patients with keratoconus. Invest Ophthalmol Vis Sci. 2007;48(7):3062-8.
-
16Negishi K, Kumanomido T, Utsumi Y, Tsubota K. Effect of higher-order aberrations on visual function in keratoconic eyes with a rigid gas permeable contact lens. Am J Ophthalmol. 2007;144(6):924-9.
-
17Rahman W, Anwar S. An unusual case of keratoconus. J Pediatr Ophthalmol Strabismus. 2006;43(6):373-5.
-
18Li X, Rabinowitz YS, Rasheed K, Yang H. Longitudinal study of the normal eyes in unilateral keratoconus patients. Ophthalmology. 2004;111(3):440-6.
-
19Key J, Benett SE. Rigid gas permeable (RGP) extended wear contact lenses. K. RP, Contact lenses: the CLAO guide to basic sience and clinical pratice. Dubuque: Kendal/ Hunt Publishing Company; 1995. p. 51-74.
-
20Fatima T, Acharya MC, Mathur U, Barua P. Demographic profile and visual rehabilitation of patients with keratoconus attending contact lens clinic at a tertiary eye care centre. Cont Lens Anterior Eye. 2010;33(1):19-22.
-
21Kastl PR, Donzis PB, Cole HP 3rd, Rice J, Baldone JA. A 20-year retrospective study of the use of contact lenses in keratoconus. CLAO J. 1987;13(2):102-4.
-
22Timucin OB, Karadag MF, Cinal A. Assessment of keratocyte density in patients with keratoconus not using contact lenses. Cornea. 2011;30(5):576-9.
-
23Cukierman E, Boldrim E. Perfil do setor de lentes de contato da Santa Casa de Misericórida do Rio de Janeiro. Rev Bras Oftalmol. 2005;64(2):77-82.
Publication Dates
-
Publication in this collection
May-Jun 2018
History
-
Received
04 Oct 2017 -
Accepted
11 Mar 2018