Abstracts
OBJECTIVE: To evaluate the positivity of cholangiography in patients without formal indication of this exam undergoing elective cholecystectomy. METHODS: We included, in the study, 100 patients whose clinical, laboratory and imaging not older than 10 days before the operation showed no change and therefore kept us unsuspicious of choledocholithiasis. The cholangiographies were analyzed and examined by the surgical team, the radiologist and the authors. The reports were compared and correlated with patients' previous clinical and laboratory findings. RESULTS: The incidence of preoperatively unsuspected choledocholithiasis was only one case (1%). CONCLUSION: The use of selective cholangiography is safe and should be used in the treatment of calculous cholecystitis.
Laparoscopic cholecystectomy; Choledocolithiasis; Cholelithiasis; Cholangiography
OBJETIVO: A colecistectomia laparoscópica é o tratamento de escolha para pacientes com colecistopatia calculosa, embora o manejo da coledocolitíase associada ainda permaneça assunto controverso. O presente estudo baseou-se na análise prospectiva de pacientes submetidos à colecistectomia eletiva com colangiografia peroperatória, pretendendo assim avaliar a positividade do exame contrastado das vias biliares em pacientes com colelitíase sem indicação para colangiografia. MÉTODOS: Foram incluídos, no estudo, 100 pacientes cujos parâmetros clínicos, laboratoriais e de imagem feitos até no máximo 10 dias antes da colecistectomia não apresentaram qualquer alteração no pré-operatório e, portanto, considerados pacientes insuspeitáveis para coledocolitíase. As colangiografias foram analisadas e examinadas pela equipe cirúrgica, pelo radiologista e pelos autores deste estudo. Os laudos foram comparados e correlacionados com achados clínicos e laboratoriais prévios dos pacientes. RESULTADOS: A incidência de coledocolitíase insuspeitável no pré-operatório foi de apenas um único caso entre 100 pacientes sem indicação para o exame (1% de positividade). CONCLUSÃO: Com base neste material, pode-se concluir que o emprego da colangiografia seletiva é segura e deve ser empregada no tratamento da colecistite calculosa.
Colecistectomia laparoscópica; Coledocolitíase; Colelitíase; Colangiografia
ORIGINAL ARTICLE
IProfessor, Department of Digestive Surgery, Universidade Federal do Triangulo Mineiro - UFTM, Uberaba-MG-BR
IIMedical School Graduate, Universidade Federal do Triangulo Mineiro - UFTM, Uberaba-MG - Brazil
IIIAssociate Professor, General Surgery and Surgical Technique, Universidade Federal do Triangulo Mineiro - UFTM, Uberaba-MG-BR
IVAssistant Professor, General Surgery and Surgical Technique, Universidade Federal do Triangulo Mineiro - UFTM, Uberaba-MG-BR
VAssociate Professor, Digestive Surgery, Universidade Federal do Triangulo Mineiro - UFTM, Uberaba-MG-BR
Correspondence to
ABSTRACT
OBJECTIVE: To evaluate the positivity of cholangiography in patients without formal indication of this exam undergoing elective cholecystectomy.
METHODS: We included, in the study, 100 patients whose clinical, laboratory and imaging not older than 10 days before the operation showed no change and therefore kept us unsuspicious of choledocholithiasis. The cholangiographies were analyzed and examined by the surgical team, the radiologist and the authors. The reports were compared and correlated with patients' previous clinical and laboratory findings.
RESULTS: The incidence of preoperatively unsuspected choledocholithiasis was only one case (1%).
CONCLUSION: The use of selective cholangiography is safe and should be used in the treatment of calculous cholecystitis.
Keywords: Laparoscopic cholecystectomy, choledocholithiasis, cholelithiasis, cholangiography.
INTRODUCTION
Laparoscopic cholecystectomy (LC) is now the preferred treatment for patients with cholecystolithiasis, while handling associated choledocholitiasis still remains controversial1,2.
Ludwig et al., in a German study, found that only 6% of institutions use perioperative cholangiography (POC) systematically during LCs, 49.5% of them use it selectively and 43% of institutions do not perform any diagnostic procedure at the time of LC3.
Although the systematic use of POC is still defended by a considerable number of surgeons who choose for the perioperative instrumentation of the biliary duct, the largest part argues that the POC, conducted in a systematic way, has not been cost-effective4, increasing operative time and the number of false-positive diagnoses, overestimating choledocholitiasis5,6, and especially increasing the proportion of patients undergoing unnecessary instrumentation of the biliary tract with the inherent risks of morbidity and mortality5,7.
Matthew et al., in a meta-analysis, reported 4,209 preoperatively POCs performed in unsuspected patients for gallstones in the bile duct. Among those, they found 170 (4%) cases of choledocholithiasis in patients with no history of pancreatitis, nor clinical, biochemical or ultrasound alterations suggestive of biliary ducts stones. They also emphasized that only 15% of those with silent, unsuspected, untreated choledocholithiasis will have some type of complication, i.e., only 0.6% without previous indication for the bile ducts contrast examination6.
It should be stated that the literature contains well-defined criteria for inclusion of patients with possible choledocholithiasis who should be submitted to cholangiography. However, it does not safely excludes asymptomatic patients, those for whom the contrast exam would not be indicated8-11.
Thus, this study intended to assess the positivity of cholangiography in patients with cholelithiasis with no indication for this exam.
METHODS
This study was based on a prospective analysis of patients undergoing elective laparoscopic cholecystectomy with perioperative cholangiography. As a criterion for inclusion in the study, patients undergoing elective laparoscopic cholecystectomy should necessarily be suffering from cholecystolithiasis and not showing any recent clinical, laboratory or ultrasound changes that would lead to choledocholithiasis suspicion. Cholangiography was then performed during surgery12,13.
We analyzed one hundred consecutive laparoscopic cholecystectomies with perioperative cholangiography in patients with cholecystolithiasis without formal preoperative indication of contrast examination of biliary tract in the period of May 2008 through February 2009.
The criteria for the indication of cholangiography during surgery are present or past history of jaundice, acute cholecystitis or acute pancreatitis over the past six months, laboratory parameters, elevated bilirubin, canalicular enzymes (alkaline phosphatase and gamma-GT), and ultrasonography with recent dilatation of the biliary three and / or choledocholithiasis6,14. Thus, the finding of one or more changes in these parameters was considered an exclusion factor of the patient for this study by presenting formal criteria for indication of POC.
Perioperatively, POC was performed when there was difficulty in identifying the main biliary duct.
The study was approved by the UFTM Ethics in Research Committee and all patients were enrolled after signing an informed consent.
One hundred patients were included in the study. They had clinical, laboratory and imaging exams, not older than 10 days before the operation, showing no relevant change, and were therefore considered unsuspected for choledocholithiasis.
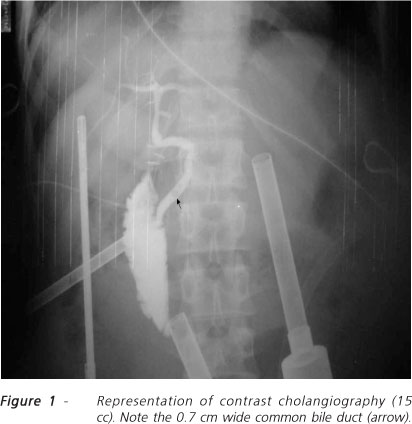
In all cases, cholangiography was preceded by administration of a muscle relaxant (eosin / glucagon) and was carried out with warm 30% iodinated contrast solution slowly injected through a transparent catheter placed in the common bile duct through the cystic duct, thus avoiding spasm of the sphincter of Oddi. The technique used was described by Mirizzi15, with three X-rays: the first after the introduction of 3 to 5 cc, the second to complete 8 to 10 cc, and the third with the rest of the contrast, totaling 15 cc.
The first two X-rays aimed the visualization of calculi, stenosis and the passage of contrast medium into the duodenum, demonstrating that the duct had no bile duct obstruction. The third radiographiy focused on the visualization of the intra-hepatic biliary tree16.
The cholangiographies were analyzed by the surgical team, the radiologist and the authors of this study. The reports were compared and correlated with the patients' previous clinical and laboratory findings.
RESULTS
One hundred elective laparoscopic cholecystectomies with perioperative cholangiography were performed, with an average time of 13.54 minutes for the contrast examination.
Among the patients examined, 16 cases were male and 84 were female. Mean age for men was 44.07 years and 45.64 for women. Regarding skin color, individuals we distributed as follows: 81% Caucasians, 4% African Brazilians and 15% mulattoes*. Therefore, we found a significant predominance of white women aged between the fourth and fifth decades.
With respect to laboratory tests, we found that, for the inclusion criteria, all tests were within normal limits: AF: 65.72 U / l (rv: 122U / l), gamma-GT: 49.82 U / l (rv: 71 U / l), total bilirubin: 0.62 mg / dl (rv: 1.2 mg / dl) and direct bilirubin: 0.20 mg / dl (rv: 0.4 mg / dl).
There were not complications related to the exam, which could be accomplished in all cases.
The incidence of preoperatively unsuspected choledocholithiasis was only one case among 100 patients without indication for the exam (Figure 1). The unsuspected choledocholithiasis was found by cholangiography in a 67-year-old, Caucasian, female patient without clinical, laboratory or ultrasound suggestive of choledocholithiasis; FA: 72.0 U / l, gamma-GT: 19.0 U / l; TBb: 0.50 mg / dl; DBb: 0.10 mg / dl. There was, therefore, a prevalence of 1% positivity of cholangiography during surgery.
DISCUSSION
Perioperative cholangiography (POC) represents a significant advance in the diagnosis of lithiasis in the commom bile duct. Its indications aim to detect choledocholithiasis based on the assessment of the anatomy and topography of the gallbladder and bile duct for a safe dissection and with lower rates of injury to the bile ducts during LC17,18.
The natural history of unsuspected choledocholithiasis has been studied in various populations and therapeutic approach remains controversial for several groups. Some articles state that the PCO, when accomplished systematically, has a 10-12% positive result. However, when selectively and judiciously performed, it presented values equal to or less than 1% of positivity19, 6.
It was noted in this study a positivity of 1% for the perioperative examination, which is consistent with the values found in the literature4,5,7,12,10,17,19. It can be inferred, given this 1% choledocholithiasis positivity rate, that only 0.15% of patients would have postoperative complications based on the study of Matthew et al.
Another reported fact is that POC does not prevent, but may provide the perioperative diagnosis of, lesions to the biliary tract. It could also be useful in the identification of biliary ducts' anomalies, which did not occur in the patients studied.
Importantly, in this study, in addition to detailed clinical history, laboratory tests and imaging were performed in at most 10 days before surgery.
Another fact that must be considered is the time spent with cholangiography. In this study it was on average 13.54 min, which corresponds to 35% of the total surgical time of laparoscopic cholecystectomy, increasing the duration of anesthesia and total time of the procedure20, plus the cost of contrast, catheter, syringe and radiological films 5-8,10,12,17,19,21-23.
Some reports include age over 70 years as a risk for cholelithiasis and choledocholithiasis24,25.
It was noted that the patient who had choledocholithiasis in this study was 67 years old and her common bile duct was 0.7 cm wide, suggesting that the age of 65, not 70, should be included as a criterion for perioperative cholangiography.
Based on this material, we can conclude that the use of selective cholangiography is safe for the detection of choledocholithiasis and should be used in the surgical treatment of chronic calculous cholelithiasis.
REFERENCES
- 1. Caddy GR, Tham TC. Gallstone disease: symptoms, diagnosis and endoscopic management of common bile duct stones. Best Pract Res Clin Gastroenterol. 2008; 20(6):1085-101.
- 2 . Mandry AC, Bun M, Ued ML, Iovaldi ML, Capitanich P. Tratamiento laparoscópico de la lithiasis de la via biliar principal asociada a lithiasis vesicular. Cir Esp. 2008; 83(1):28-32
- 3. Ludwig K, Bernhardt J, Lorenz D. Value and consequences of routine intraoperative cholangiography during cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2002;12(3):154-9.
- 4. Yasojima EY, Lopes Filho GJ. Colangiografia peroperatória sistemática em colecistectomia videolaparoscópica. Rev Col Bras Cir. 2002;29(2):92-8.
- 5. Collins C, Maguire D, Ireland A, Fitzgerald E, O'Sullivan GC. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy. Ann Surg. 2004;239(1):28-33
- 6. Metcalfe MS, Ong T, Bruening MH, Iswariah H, Wemyss-Holden SA, Maddern GJ. Is laparoscopic intraoperative cholangiogram a matter of routine? Am J Surg. 2004;187(4):475-81.
- 7. Massarweh NN, Devlin A, Elrod JA, Symons RG, Flum DR. Surgeon knowledge, behavior, and opinions regarding intraoperative cholangiography. J Am Coll Surg. 2008;207(6):821-30. Epub 2008 Oct 2.
- 8. Berci G, Sackier JM, Paz-Partlow M. Routine or selected intraoperative cholangiography during laparoscopic cholecystectomy? Am J Surg. 1991;161(3):355-60.
- 9. Borjeson J, Liu SK, Jones S, Matolo NM. Selective intraoperative cholangiography during laparoscopic cholecystectomy: how selective? Am Surg. 2000;66(7):616-8.
- 10. Castro Pérez R, Delgado Fernández JC, Dopico Reyes E, Echevarría Hernández F, González Garcia P. Colangiografía transopearatoria en colecistectomía laparoscópica: ¿sistemática o selectiva? Rev Cubana Cir. 2000;39(1):61-7.
- 11. Wu SC, Chen FC, Lo CJ. Selective intraoperative cholangiography and single-stage management of common bile duct stone in laparoscopic cholecystectomy. World J Surg. 2005;29(11):1402-8.
- 12. Campos T, Parreira JG, Moricz A, Rego REC, Silva RA, Pacheco AM Jr, et al. Fatores preditivos de coledocolitíase em doentes com litíase vesicular. Rev Assoc Med Bras. 2004;50(2):188-94.
- 13. Verbesey JE, Birkett DH. Common bile duct exploration for choledocholithiasis. Surg Clin North Am. 2008;88(6):1315-28.
- 14. Keus F, Broeders IA, van Laarhoven CJ. Gallstone disease: surgical aspects of symptomatic cholecystolithiasis and acute cholecystitis. Best Pract Res Clin Gastroenterol. 2006;20(6):1031-51.
- 15. Mirizzi PL. Operative cholangiography. Surg Gynecol Obstet. 1937;65:702-10.
- 16. Watson MJ, Hamilton EC, Jones DB. Laparoscopic common bile duct exploration. Oper Tech Gen Surg. 2005;7(1):23-38.
- 17. Araújo Neto NP, Gonçalves JE, Bromberg SH, Guz B, Zanoto A. Predição da coledocolitíase pela associação de indicadores clínicos e laboratoriais em dois momentos do pré-operatório da colecistectomia. Rev Col Bras Cir. 2005;32(1):41-6.
- 18. Saad N, Darcy M. Iatrogenic bile duct injury during laparoscopic cholecystectomy. Tech Vasc Interv Radiol. 2008;11(2):102-10.
- 19. Gil SM, Braga JF, Centurion SAR, Gil BZ. Estudo da incidência de coledocolitíase em pacientes com colecistite calculosa aguda e crônica submetidos à colecistectomia videolaparoscópica. Rev Col Bras Cir. 2007;34(4):214-7.
- 20. Livingston EH, Miller JA, Coan B, Rege RV. Costs and utilization of intraoperative cholangiography. J Gastrointest Surg. 2007;11(9):1162-7. Epub 2007 Jun 30.
- 21. Charfare H, Cheslyn-Curtis S. Selective cholangiography in 600 patients undergoing cholecystectomy with 5-years follow-up for residual bile duct stones. Ann R Coll Surg Engl. 2003;85(3):167-73.
- 22. Astudillo PS, Minuzzi F, Allende FS. Valor de la colangiografia operatoria em la cirurgia biliar laparoscopica. Rev Argent Cirug. 1994;66(1-2):19-25.
- 23. Snow LZ, Weinstein LS, Hannon JK, Lane DR. Evaluation of operative cholangiography in 2043 patients undergoing laparoscopic cholecystectomy: a case for the selective operative cholangiogram. Surg Endosc. 2001;15(1):14-20. Erratum in: Surg Endosc 2001;15:532.
- 24. Gutt CN, Oniu T, Mehrabi A, Kashfi A, Schemmer P, Büchler MW. Robot-assisted abdominal surgery. Br J Surg. 2004;91(11):1390-7.
- 25. Chitwood WR Jr, Nifong LW, Chapman WH, Felger JE, Bailey BM, Ballint T, et al. Robotic surgical training in an academic institution. Ann Surg. 2001;234(4):475-84; discussion 484-6.
Assessment of positive perioperative cholangiography in patients undergoing elective laparoscopic cholecystectomy
Publication Dates
-
Publication in this collection
04 Feb 2011 -
Date of issue
Dec 2010
History
-
Received
03 Nov 2009 -
Accepted
30 Jan 2010