Abstracts
Sexually transmitted diseases (STDs) have a significant prevalence in both the general population and pregnant women. Accordingly, we consider the physiological changes of the maternal organism that can alter the clinical course of these diseases. In addition, obstetric and neonatal complications may occur, resulting in increased maternal and infant morbidity and mortality. We explore features of the natural course and treatment during pregnancy of the major STDs: soft chancre, donovanosis, gonorrhea, chlamydia, viral hepatitis, genital herpes, human papillomavirus (HPV) infection, lymphogranuloma venereum, syphilis, and vulvovaginitis. We believe that health professionals should pay careful attention to STDs, particularly in relation to early diagnosis and precautions on the use of drugs during pregnancy. Prevention and partner treatment to achieve effective results are also extremely relevant.
Maternal welfare; Pregnancy; Sexually transmitted diseases
As doenças sexualmente transmissíveis (DSTs) apresentam prevalência significativa tanto na população geral quanto nas gestantes. Nestas, em especial, devem-se considerar as alterações fisiológicas em seu organismo que podem, inclusive, alterar o curso dessas doenças. Complicações obstétricas e neonatais podem ocorrer em decorrência delas, acarretando aumento da morbimortalidade materno-infantil. Abordam-se, neste artigo, as particularidades da história natural e terapêutica no período gestacional das principais DSTs: cancro mole, donovanose, gonorreia, clamidíase, hepatites virais, herpes genital, infecção pelo papilomavírus humano (HPV), linfogranuloma venéreo, sífilis e vulvovaginites. As DSTs devem ser enfrentadas com extrema atenção e conscientização por parte dos profissionais de saúde, principalmente, no tocante ao diagnóstico, que deve ser o mais precoce possível, e ao tratamento, que apresenta limitações na terapêutica durante a gestação, pela toxicidade de muitos dos medicamentos comumente empregados. A prevenção e o tratamento do parceiro são importantes para que as ações sejam efetivas.
Bem-estar materno; Doenças sexualmente transmissíveis; Gravidez
CONTINUING MEDICAL EDUCATION
IMD; Postgraduate student, Prof. Rubem David Azulay Institute of Dermatology - Santa Casa da Misericordia do Rio de Janeiro (IDPRDA - SCMRJ) - Rio de Janeiro (RJ), Brazil
IIMD; Postgraduate student, Prof. Rubem David Azulay Institute of Dermatology - Santa Casa da Misericordia do Rio de Janeiro (IDPRDA - SCMRJ) - Rio de Janeiro (RJ), Brazil
IIIMSc; Head of the Service of Dermatology, Prof. Rubem David Azulay Institute of Dermatology - Santa Casa da Misericordia do Rio de Janeiro (IDPRDA - SCMRJ); Professor, Postgraduate Program, Pontifical Catholic University of Rio de Janeiro; Professor, Souza Marques Technical Educational Foundation and Federal University of Rio de Janeiro - Rio de Janeiro (RJ), Brazil
IVPhD - MSc in Infectious/Parasitic Diseases, Federal University of Rio de Janeiro (UERJ); PhD in Epidemiology, University of Maryland; Researcher, Department of Biological Sciences, Public Health National School (ENSP) - Rio de Janeiro (RJ), Brazil
VPhD - MSc in Dermatology, UFRJ; Associate Professor of Dermatology, Prof. Rubem Azulay Institute of Dermatology - Santa Casa da Misericordia do Rio de Janeiro (IDPRDA - SCMRJ) - Rio de Janeiro (RJ), Brazil
VIPhD - MSc in Dermatology, Fluminense Federal University (UFF); PhD in Infectious/Parasitic Diseases, Federal University of Rio de Janeiro (UFRJ); Head of the Sanitary Dermatology Sector (STD/Hanseniasis), Prof. Rubem Azulay Institute of Dermatology - Santa Casa da Misericordia do Rio de Janeiro (IDPRDA - SCMRJ). Associate Researcher, Laboratory of Hanseniasis and Sousa Araujo Ambulatory - Oswaldo Cruz Institute (IOC) - FIOCRUZ - Rio de Janeiro (RJ), Brazil
Mailing address
ABSTRACT
Sexually transmitted diseases (STDs) have a significant prevalence in both the general population and pregnant women. Accordingly, we consider the physiological changes of the maternal organism that can alter the clinical course of these diseases. In addition, obstetric and neonatal complications may occur, resulting in increased maternal and infant morbidity and mortality. We explore features of the natural course and treatment during pregnancy of the major STDs: soft chancre, donovanosis, gonorrhea, chlamydia, viral hepatitis, genital herpes, human papillomavirus (HPV) infection, lymphogranuloma venereum, syphilis, and vulvovaginitis. We believe that health professionals should pay careful attention to STDs, particularly in relation to early diagnosis and precautions on the use of drugs during pregnancy. Prevention and partner treatment to achieve effective results are also extremely relevant.
Keywords: Maternal welfare; Pregnancy; Sexually transmitted diseases
INTRODUCTION
Gestational alterations such as relative immunosuppression and anatomical and hormone changes may affect the course of sexually transmitted diseases (STDs). Infections in the mother may impact both maternal and fetal health and transmission may occur during pregnancy, delivery and in the post-partum period.
Data from the National Program on STD/AIDS of the Ministry of Health (MS) about the prevalence of some STDs in populations of six Brazilian capitals indicate that, among 3,303 pregnant women, prevalence of chlamydia was 9.4%, syphilis, 2.6% and gonococcal infection, 1.5%. Among viral STDs, the human papillomavirus infection (HPV) prevailed with 40.4%. The same study indicated a prevalence of 0.5% for both the human immunodeficiency virus (HIV) and for hepatitis B virus (HBV), and of 22.7% for type 2 herpes virus (HSV-2). 1,2
The diagnosis and treatment of these infections will depend on the type of infection, incubation period and infectivity, clinical presentation of the disease, availability of accurate and fast diagnostic tests and of specific treatment. In pregnant women, the risks of diagnostic and therapeutic procedures must be considered. HIV, syphilis and HBV serologies are normally done during pre-natal visits, whereas those for Chlamydia and gonorrhea are often neglected. In addition, even if these serologies are performed, pregnant women are often not told about the results due to negligence or disorganization of the health system.
We will explore below the main STDs during the gestational period: soft chancre, donovanosis, gonorrhea, chlamydia, genital herpes, HPV infection, hepatitis B and C, lymphogranuloma venereum, syphilis, and vulvovaginitis.
1. SOFT CHANCRE
It is an infectious contagious disease often localized in the external genitalia and occasionally in the anal region. It is also known as chancroid, venereal chancre and Ducrey's chancre1. The disease is popularly known in Brazil as "cavalo". Fetal alterations caused by exclusive infection by Haemophilus ducreyi during pregnancy have not been reported. 3 When complications such as premature amniorrhexis occur, there is associated gonococcal, and streptococcal (group B) co-infection, chlamydia infection or bacterial vaginosis. 1,3,4
Etiologic agent and transmission
It is a sexually transmitted disease caused by the fastidious Gram-negative streptobacillus Haemophilus ducreyi.
Epidemiology
Women are often asymptomatic carriers. The disease affects a man for every 10 to 20 women, usually from 15 to 30 years old. 3 Incidence is greater in tropical regions and in populations with poor hygiene. 4
Clinical aspects
After an incubation period of 1 day to two weeks, chancroid begins with a small lesion, which can be a macula, papule, vesicle or pustule that rapidly progresses to an ulcer. In most cases ulcers affect the labia, furcula, vaginal introitus, uterine wall or perineum. 1,3 Adjacent lesions by autoinoculation are common. Ulcers are painful with a dirty bed and fetid odor. It may be associated with syphilis, characterizing the so-called Rollet's (mixed) chancre. The inguinal bubo, often unilateral and painful, is rare in women due to the regional drainage that does not occur in the inguinal ganglia, 1,3,4 but in the deep or perirectal iliacs. 4
Diagnosis
Diagnosis is based on clinical manifestations. Bacterioscopy of Gram-stained smear of ulcer exudate or bubo aspirate may be performed. Gram-negative streptobacilli in "school of fish" configuration with 50% positivity are observed. Culture reveals round, grayish colonies that easily detach from the medium. Polymerase chain reaction is the gold standard, despite being expensive and of limited access. Biopsy is rarely performed and is exclusively used to dismiss other diagnoses. 3,4
Differential diagnosis
Differential diagnosis is done with diseases that cause genital ulcers and inguinal adenopathies. The most frequent are hard chancre (primary syphilis), genital herpes, lymphogranuloma venereum, donovanosis, infected traumatic lesions, pyodermitis and neoplasms. Attention should be paid to the likely evolution of the disease when Rollet's chancre is present. 1,3
Treatment
Treatment regimens are: intramuscular ceftriaxone 250 mg single dose or oral erythromycin stearate 500 mg every 6 hours for 7 days. Erythromycin estolate is counter-indicated in pregnancy due to hepatoxicity (cholestatic hepatitis). 5 Patients who do not tolerate erythromycin can use oral azithromycin 1 g single dose or thiamphenicol 5 g single dose. 1,4,6 If after a week of treatment active lesions still remain, treatment must be repeated. Quinolones are counter-indicated in pregnancy. Recent sexual partners (last 10 days) must also be treated, even without clinical symptoms of the disease.1,4
DONOVANOSIS
Also known as granuloma venereum or granuloma inguinale, donovanosis is a disease of chronic evolution that affects mainly the skin and mucosae of the genital, perianal and inguinal regions; it may exceptionally affect other regions. It is characterized by painless, auto-inoculating ulcer-vegetating lesions. It is very little contagious and very uncommon these days. 1,3 Pregnancy considerably aggravates the disease, leading to an increase in the number of lesions. 4
Etiologic agent and transmission
The disease is caused by the Gram-negative bacterium Klebsiella granulomatis and is often sexually transmitted, although the mechanisms of transmission are not well known. Many authors also consider the possibility of non-sexual contagion. 1,4 There are no reports of histotoxic effects of this bacterium on fetal development. 3,6,7 However, abortion and surgical manipulation of lesions may facilitate dissemination.4
Epidemiology
Difficulty in cultivating the etiologic agent contributes to the perpetuation of doubts about this disease. There is greater prevalence in tropical and subtropical regions, and the disease is more frequent in blacks. It affects men and women equally, especially those aged between 20 and 40 years. 3 Low socioeconomic status, poor hygiene, and sexual promiscuity constitute risk factors. 4
Clinical aspects
The incubation period ranges from 30 days to 6 months. 1 The disease begins with a painless papule or nodule that, upon evolving, ulcerates and enlarges, taking an ulcer-vegetating aspect. The bed of the lesion is soft and deep red, with irregular, elevated, well-defined and hard edges. Lesions may chronically evolve with genitalia deformity, paraphimosis or elephantiasis. 3 The occurrence of general symptoms or adenopathies is rare, although normally unilateral pseudo-buboes (inguinal lesions characterized by hard masses or floating abscesses that drain and become ulcers; they represent subcutaneous granulation tissue and are not enlarged lymphnodes) may develop.1
Extragenital donovanosis occurs in 3 to 6% of the cases and may be due to autoinoculation, contiguity, lymphatic or hematogenic dissemination.
Pregnancy may aggravate the disease, leading to an increase in the number of lesions. If internal genitalia are affected, the risk of hematogenic dissemination is higher and this may cause complications during pregnancy and labor. 4
Diagnosis
The diagnosis is based on the clinical characteristics of lesions and presence of the causal agent in direct or histologic examination. Identification of Donovan bodies in the biopsy is done through Wright, Giemsa or Leishman stain, which shows dark oval structures inside vacuoles or outside of the cells. 1,3 Although the epidermis is absent from the center of the lesion, hyperplasia is found in the edges and simulates spinocellular carcinoma (pseudoepitheliomatous hyperplasia). Culture is not commonly done. 4
Differential diagnosis
Differential diagnosis is done with primary syphilis, soft chancre, lymphogranuloma venereum, condyloma acuminatum, American tegumentary leishmaniasis, some systemic micoses, cutaneous tuberculosis, atypical mycobacteriosis, cutaneous amebiasis, and ulcerated neoplasms. 1,3
Treatment
The drug of choice is erythromycin stearate (500 mg), taken orally every 6 hours for 21 days or until healed. The concomitant use of gentamicin from the start must be considered. Doxycycline and ciprofloxacin are counter-indicated. Surgical reconstruction of chronic lesions should be postponed to the end of pregnancy. When there is risk of perineal laceration, a cesarean section is indicated. 6,7 Due to low infectivity, it is not necessary to treat sexual partners.1
3. GONORRHEA and CHLAMYDIA INFECTION
Gonorrhea in pregnancy may be associated with a higher risk of prematurity, premature rupture of membranes, fetal losses, delayed intra-uterine growth, and fever in the puerperium. Postpartum bartholinitis, peri-hepatitis, arthritis, endocartitis and endometritis may occur. About 25% of women with gonorrhea or Chlamydia become infertile. Complications in the newborn include conjunctivitis, atypical interstitial pneumonitis, bronchitis and otitis media. 6
Etiologic agent and transmission
Neisseria gonorrhoeae is a Gram-negative intracellular diplococcus, aerobic and sensitive to most antiseptics. It is sexually transmitted, with a risk of transmission of 50%. 1
In chlamydia infection C. trachomatis D-K serotypes are implicated. C. trachomatis is a necessarily intracellular bacterium that is sexually transmitted, with a risk of transmission of 20%. 1
Epidemiology
In Brazil, infections of the genito-urinary tract caused by Chlamydia and Gonococcus correspond by far to the highest estimates in the sexually active population. It is estimated that the number of gonorrhea cases corresponds to 56% of the total number of sexually transmitted diseases recorded based on data from the Ministry of Health. 8 National data show that the incidence of Chlamydia in pregnancy ranges between 2 and 9.4%. 3,4,6
Clinical aspects
In women these infections may cause asymptomatic vulvovaginitis and cervicitis in 80% of the cases. Prolonged infection may evolve to pelvic inflammatory disease (PID) and cause sterility, ectopic pregnancy and chronic pelvic pain. Fitz-Hugh-Curtis syndrome consists in peritonitis, pelvic abscesses or perihepatitis due to gonococcal dissemination sencondary to acute salpingitis. 4 In addition to the possible alterations during pregnancy already mentioned, gonococcal infection may also affect the newborn and may cause conjunctivitis, septicemia, arthritis, abscesses in the hair scalp, pneumonia, meningitis, endocardititis and stomatitis.1
Chlamydia infection has clinical manifestations similar to those of gonorrhea, except for a longer period of incubation, varying from 14 to 21 days. Chlamydia infection during pregnancy may lead to the premature rupture of membranes, pre-term labor, puerperal endometritis and conjunctivitis and pneumonia in the newborn.1
Diagnosis
In gonococcal cervicitis, culture in selective medium (modified Thayer-Martin) of endocervical samples is considered ideal. 1 In women, Gram-staining sensitivity does not surpass 30%, and this does not occur in men. Both culture and PCR are considered gold standards. Conclusive diagnosis of Chlamydial cervicitis can be made by culture and direct immunofluorescence of uterine wall sample. Triage tests for Chlamydia and Gonococcus using nucleic acid amplification techniques (NAAT) have as advantage the possibility to detect the agent, even in samples collected through non-invasive methods, such as urine, with similar sensitivity to that of culture. 1,7 However, these exams are not routinely available in developing countries such as ours.
Differential diagnosis
Differential diagnosis of gonorrhea and Chlamydia infection should be done with other causes of cervicitis and vaginal discharge, such as trichomoniasis, candidiasis and bacterial vaginosis.
Treatment
In cases of gonococcal infection, an injectable and single dose treatment should be prioritized. Among cephalosporins, ceftriaxone appears to be the most effective drug and should be administered intramuscularly in a single 250mg dose. The use of ciprofloxacin and ofloxacin is counterindicated during pregnancy. Treatment should be controled through endocervical, urethral and vaginal fornix culture three days after medication. In the infected newborn, the main manifestation is gonococcal ophthalmia, whose prophylaxis is done with the administration of an aqueous 1% silver nitrate solution into the eyes (Credé's method). Other therapeutical options are 0.5% ophthalmic erythromycin ointment or 1% tetracycline, with a single application. 6
To treat Chlamydia infection, a single dose of oral azithromycin (1 g) may be used, 9 in addition to oral erythromycin stearate 500mg every 6 hours for 7 days or oral amoxacylin 500 mg every 8 hours for 7 days. For neonatal ophthalmia erythromycin stearate 50mg/kg/day for 14 days is also used. 4,6 Sexual partners should be treated in the presence of these infections, preferably with single dose drugs. 1,4
4. VIRAL HEPATITIDES
Viral hepatitides are a serious public health issue in Brazil and in the world. They are caused by different etiologic and hepatropic agents. 1 We will explore the viral hepatitides transmitted by the B and C viruses.
Etiologic agent and transmission
The hepatitis B virus (HBV) belongs to the Hepadnaviridae family. Structurally, it has a lipid envelope and a dense central nucleus with DNA. 10 Transmission of HBV occurs parenterally, through infected bodily fluids and mainly through unprotected sex. Vertical transmission (mother-child) is also a frequent cause of dissemination of the virus, 11 being more frequent at the end of pregnancy. 6
The hepatitis C virus (HCV) belongs to the Flaviviridae family and is constituted by a nucleus with a single-stranded RNA molecule surrounded by a lipid envelope. Like the HIV virus, HCV is extremely mutagenic, making the development of an efficient vaccine difficult. 10 The main form of transmission of HCV is parenterally. Sexual transmission is rare (less than 1% of risk in steady partners); it mainly occurs in individuals with multiple sexual partners and in those with risky sexual practice (without the use of condom). 11 The coexistence of an STD facilitates transmission. Vertical transmission of HCV occurs in 3-5% of the cases, with an increased risk in pregnant women with the HIV virus or with a high HCV viral load. 1
Epidemiology
Distribution of viral hepatitides is universal. According to the MH, there is high regional variation in the prevalence of each type of hepatitis in Brazil, with an approximate estimate of about 2 million chronic carriers of hepatitis B and three million of hepatitis C. Many individuals ignore their asymptomatic condition and this contributes to the maintenance of the HBV and HCV transmission chain. 1
Clinical aspects
The period of incubation of HBV varies from 30 to 180 days, from contagion to the development of the first symptoms. Only 30% of the cases present jaundice. After benign acute hepatitis B, 90 to 95% of adult patients will evolve to a cure. Chronicity of the disease, defined as the persistence of the virus for more than 6 months, varies based on the age range. In newborns of women who show evidence of viral replication, chronification occurs in up to 90% of the cases and in cases without evidence of viral replication, in about 40%. With regard to children younger than 5 years, 30% will become chronic carriers of the disease. The rate of adult individuals with chronic hepatitis B is low, about 5 to 10% of infected individuals. 7,11 Vertical transmission of HBV is considered to be the main cause of hepatocellular carcinoma in the future. 6
The period of incubation of HCV ranges from 15 to 150 days. Despite the fact that only 20% of HCV infected individuals develop jaundice, the chance of chronification is high, occurring in about 70 to 85% of the cases. Of these, approximately 30% develop severe histological forms or cirrhosis within 20 years, when not treated. The others progress more slowly and may never develop severe hepatopathy. 11 During pregnancy both acute and chronic HCV infections do not carry a higher risk of causing fetal abnormalities or perinatal complications. 12 The risk of transmission of HCV to the newborn is 2 to 3 times higher if the woman is HIV-positive. 7
Chronic hepatitis is asymptomatic or oligosymptomatic in most cases, with clinical manifestations in advanced stages of hepatic involvement.
Diagnosis
Hepatic function tests, despite being sensitive indicatos of damage to the hepatic parenchyma, are not specific for hepatitides. Molecular biology tests detect the presence of the virus nucleic acid (DNA OF HBV and RNA of HCV). They can be qualitative (presence or absence of the virus in the sample), quantitative (indicates the viral load of the sample) or of genotype (indicate the genotype of the virus). PCR and hybridization, among others, are examples. 11 Serologic markers of hepatitis B and C are detailed in the table 1:
The tracking of hepatitis B with the surface antigen (HBsAG) must be done in the first pre-natal visit. Women at an increased risk may be vaccinated during pregnancy and should be monitored again before or at the time of labor. 13 The performance of serologic triage tests for hepatitis C during pre-natal visits is also indicated. 12
Differential diagnosis
Several diseases may have similar clinical manifestations: brucelosis, reactional colestasis, sclerosing colangitis, colelitiasis, dengue fever, granulomatous diseases of the liver, non-alcoholic hepatic steatosis, yellow fever, alcohol and drug hepatitis, herpes simplex, leptospirosis, mononucleosis, hepatic neoplasm (primary or metastatic), ricketsiosis, secondary syphilis and toxoplasmosis. 10,11
During pregnancy, some diseases such as intrahepatic colestasis of pregnancy, ecclampsia, acute steatosis of pregnancy and HELLP syndrome (plateletopenia, increase of hepatic enzymes and hemolisis) may simulate viral hepatitides. 7
Treatment
Acute hepatitis B will be treated symptomatically and with rest, hydration and diet. If a healthy pregnant woman is exposed to a real risk of contamination by HBV, she will receive human anti-hepatitis B immunoglobulin (HAHBIG) in the dose of 0.06 ml/kg, intramuscularly, repeated in a month. Vaccination should be initiated in the regimen of three doses. 1,6,11 In relation to chronic hepatitis B, the use of interpheron-alpha and lamivudine to reduce viral replication is counterindicated in pregnancy and lactation. The use of lamivudine should only be considered when the benefits outweigh the potential risks.14 All pregnant women should be submitted to routine serologic tests for HBsAG during prenatal visits, even if they have been previously tested or immunized. Pregnant women who did not have prenatal medical care and those at risk (use of injectable drugs, history of more than one sexual partner in the last 6 months or HBsAG positive partner, diagnosed with or undergoing treatment for STD) or with clinical hepatitis, should be submitted to serologic testing when admitted to the hospital. Newborn of an HBV-infected mother should be immunized with vaccine and immunoglobulin (0.5 ml) administered in different places IM, within the first 12 hours of birth. The immunization regimen should be completed afterwards. 1,6,11 In Brazil, vaccination against hepatitis B is part of the basic immunization schedule. The first dose should be administered to all newborns right after birth, and subsequent doses are given in the first and sixth months of life. 1,11 Premature newborns weighing less than 2.000 g should get 4 doses of the vaccine due to the possibility of reduction of immunogenicity caused by the vaccine. 15 HBsAG positive mothers can breastfeed their infants if they receive proper immunoprophylaxis. 16
Currently, there is no available vaccine for hepatitis C and prophylaxis with immunoglobulin is ineffective after exposure. In the lack of active or passive immunization, prevention of hepatitis C includes behavioral changes and caution to avoid contact with infected individuals. 10 Breastfeeding babies born to mothers with positive anti-HCV test results should be tested for HCV infection. If they test positive, they should be monitored for evaluation of chronic hepatic disease. 7 Drugs currently used to treat HCV infection - ribavirin and pegylated interferon alpha are counterindicated in pregnancy and breastfeeding. 16 Breastfeeding is allowed if the mother is infected with HCV, but if the breasts have fissures or bleeding, breastfeeding should be avoided. 7
5. GENITAL HERPES
Genital herpes is a predominantly sexually transmitted disease; it is also transmitted via orogenital contact. Over the last few years, it has gained prominence among the etiology of genital ulcers because it accounts for a high percentage of HIV transmission cases. 17 Maternal prime infection may result in abortion, microcephalia, delayed intra-uterine growth, congenital herpes, neonatal herpes and fetal death. Even though transplacental transmission may occur (1:3,500 pregnancies), fetal contamination occurs more frequently through the birth canal (50% of infection when there is active lesion),1 leading to neonatal herpes, a disease with high morbimortality. 6
Etiologic agent and transmission
The herpes simplex viruses 1 and 2 (HSV-1 and HSV-2) are DNA-viruses that belong to the Herpesviridae family. Although both may provoke lesions in any part of the body, HSV-2 clearly predominates in genital lesions and HSV-1 in perioral lesions. Transmission occurs through mucosal surfaces or bodily fluids. HSV-2 is mainly sexually transmitted, but transmission may also occur during delivery, which can be extremely severe to the newborn. The disease tends to latency and, more frequently, relapse, since the virus resides in the sacral ganglia. 3
Epidemiology
HSV-2 is the etiologic agent of about 80-90% of genital herpes cases and of 10-20% of oral herpes cases. The opposite is true for HSV-1. After the first year, recurrence of genital lesions is observed in 50% of the patients infected with HSV-1 for the first time, as compared with 90% of those infected with HSV-2.18 It is believed that up to 1% of pregnant women show HSV -2 in the culture of material collected from their vagina. 19
The risk of neonatal herpes is higher when women become infected during pregnancy (30-50%) as compared with those that have recurrent episodes during the same period (1%). 3
Clinical aspects
After a period of incubation of 3 to 14 days (prime infection) vesicular lesions develop and within a few days they become exulcerated or even small ulcers (Figure 1). Lesions are often preceded by symptoms such as burning, paresthesia, pruritus and pain. Cutaneous lesions are spontaneously healed within 15 to 21 days.
In neonatal herpes, lesions are often cutaneous, but when they involve the eyes, kidneys, intestine and central nervous system they are more severe. HSV is one of the causes of the TORCH syndrome (toxoplasmosis, others, rubeola, cytomegalovirus, herpes), which is characterized by manifestations of variable intensity in newborns such as fever, small size for gestational age, purpuric eruption, hepatosplenomegaly, jaundice, ear and eye problems, mental retardation, delayed growth and even death.
Diagnosis
Diagnosis is by clinical manifestations. Tzanck smear test (visualization of ballooning multinucleated cells - Figure 2) and gynecological examination of cervical cytology are not conclusive methods, although Tzanck method is very helpful when positive. 1 A much more precise method, of high sensitivity and specificity, but rarely employed is the serology of specific glucoproteins (gG), and this allows the differentiation between HSV-1 and 2 (gG1 for HSV-1 and gG2 for HSV-2).18 PCR is a high sensitivity method, but very little accessible in daily medical practice. Likewise, culture of the virus is also a fairly unavailable procedure, even though it is the most specific technique for the diagnosis of herpes infection. Its sensivitivity is greater for vesicular lesions and decreases for pustules, exulcerations and crusts. 1
Differential diagnosis
Soft chancre, syphilis, donovanosis, lymphogranuloma venereum, and ulcerations after trauma should be the differential diagnosis of genital herpes.
Treatment
Herpetic lesions during pregnancy should be treated especially in cases of prime infection in any trimester of the pregnancy. 1 It is not well known whether acyclovir, famcyclovir or valacyclovir are safe during pregnancy, but acyclovir is the most used drug. Oral administration of acyclovir is recommended, but the regimen is unclear: 400mg, three times a day, for 7 to 10 days7 or 400mg every 4 h, 5 times a day for the same period of time. Severe genital herpes infections in pregnant women (for instance those that may occur in HIV positive women) should be treated with acyclovir administered endonovenously; it is recommended in the dose of 5-10mg/kg, three times a day for 7-10 days.6 Prelabor prophylaxis for 10 days from the 36th week of gestation may be considered, with 400 mg, three times a day, for 7 to 10 days, both if prime infection occurred during pregnancy or if recurrences were frequent during the same period. 18 Immunomodulary drugs such as levamisole are counterindicated during pregnancy. 6
Some authors recommend that a c-section be performed in pregnant women who show clinical lesions at the time of delivery. Others indicate the use of systemic antiviral drugs at the time of delivery or before labor, as mentioned above. Still, others recommend both measures. 6 Newborns exposed to the virus must be isolated in the nursery.4
6. HPV INFECTION
Pregnancy may facilitate the development, growth or reappearance of lesions caused by the human papillomavirus (HPV). In infected pregnant women, there seems to be a higher frequency of obstetrical complications.6
Etiologic agent and transmission
HPV is a virus with a DNA nucleus that belongs to the Papovaviridae family, with more than a hundred identified types, of which more than 30 may infect the genital tract. 7 These are classified into two subgroups based on their oncogenic potential: low (6, 11, 42, 43, 44) or high risk (16,18, 33, 35, 39, 45, 46, 51, 52, 56, 58, 59, 68). Transmission may occur sexually, vertically or, very rarely, by fomites. Vertical transmission may occur by hematogenic route (transplacental) or by ascending contamination or through the birth canal, which may result in the dreaded and rare laryngeal papillomatosis. In this context, c-section is not mandatory because it is not known whether it prevents vertical transmission of HPV. 6
Epidemiology
Infection by HPV more frequently affects young adults beginning their sexual life. 19 There is great variation in the prevalence of HPV infection in different populations and also in the frequency of the different viral types. 1,3,10 Among the risk factors associated with HPV infection, the number of sexual partners throughout life is one of the most important. 20
Clinical aspects
Clinically, genital HPV, denominated condyloma acuminatum, presents with humid, isolated or grouped vegetating lesions, or sessile papules that resemble a common wart; they may look like a cauleflower (Figure 3). During pregnancy, condyloma acuminatum tends to increase in size and may reach large proportions due to higher vascularization and hormonal and immunologic alterations, which may even lead to obstruction of the birth canal. 1
Diagnosis
The diagnosis of condilomatous lesions is based on clinical manifestations, and biopsy should be done in special cases, such as lack of response or exacerbation of lesions during or after treatment, diagnostic doubt, and immunodepressed patients. The application of a 0.05 acetic acid solution to the site of the lesions allows the visualization of a whitish area in their surface. When lesions are present in the skin but not in the mucosa or semi-mucosa, observation of the whitish area is more difficult and the test results should be carefully read. Viral identification may be done through a method of hybrid capture in which saline solution is applied to the surface of lesions and the material is collected with a proper brush. Its use is not practical because it does not modify the therapeutic conduct. 1,3,6
Differential diagnosis
It must be done with contagious molluscum, micropapillomatosis, condyloma syphiliticum, intradermal nevum and seborrheic keratosis.
Treatment
During pregnancy, physical therapeutic methods are preferred: electroctrocauterization, CO2 laser, cryocauterization and surgical methods. The latter should be performed with caution to avoid excessive blood loss. Chemical, chemotherapic and immunotherapic methods are counterindicated in pregnancy due to embriotoxicity (podophyllin, bleomycin and 5-fluorouracil). 6 Imiquimod and podophyllotoxin should not be used during pregnancy. Trichloroacetic acid may be used in pregnancy and is recommended by some authors in concentrations lower than 80%. Since its pattern of absortion is unknown, the risk of umbilical vasoconstriction induction cannot be ignored. 6 Extensive lesions oftentimes require waiting until the puerperal period, when they tend to go into remission. When lesions are obstructing the birth canal, a c-section is indicated. Subclinical lesions should be monitored during pregnancy through cervical-vaginal cytological examination and reevaluated in the puerperal period for definitive treatement. 1,3,6
7. LYMPHOGRANULOMA VENEREUM
Also known as Nicolas-Favre disease, it is popularly known as "mula" in Portuguese. The obstetrical relevance of lymphogranuloma venereum (LGV) lies in the fact that it may be associated with other STDs and also may make labor and delivery of women with stenosing perirectal lesions more difficult. Apparently, LGV is not associated with direct harm to the fetus. 6
Etiologic agent and transmission
The causal agent of LGV is Chlamydia trachomatis, serotypes L1, L2, and L3, and it is exclusively sexually transmitted.
Epidemiology
The disease is distributed worldwide with high rates of prevalence and predominance in tropical and subtropical regions. About 70 to 80% of the cases are asymptomatic and often undetected. 21 In Brazil, the disease is more observed in the Northern and Northeast regions. It classicaly shows greater incidence in the sexually active population, with predominance between 20 and 40 years of age.
Clinical aspects
After a period of incubation from 3 to 30 days, the disease progresses into three stages: inoculation lesion, regional lymphatic dissemination and sequelae. The first stage begins with the formation of papule, pustule, vesicle, exulceration or a simple painless violaceus edema, especially in the balanopreputial groove and internal face of the labia minora, which recedes spontaneously and is many times unnoticed. The second stage occurs from one to six weeks after the initial lesion and corresponds to inguinal lymphoadenopathy in males, being unilateral in 70% of the cases. In females, the site of adenopathy is associated with the localization of the inoculation lesion due to the female anatomy, since lymphatics of the vaginal mucosa and uterine wall drain into the deep or perirectal iliac ganglia. 4 Ganglionary involvement may progress with fluctuating points, corresponding to multipl foci of necrosis that fistulize and release a dense purulent material through multiple holes (watering can rose). Regarding sequelae, they tend to occur more frequently in women and in those who practice anal sex due to vaginal and/or rectal involvement, which may lead to chronic lymphatic obstruction (denominated esthiomene in women), rectal, vesical and anal fistules and rectal stenosis. 3,4
Diagnosis
In most cases diagnosis is based on clinical data and laboratory confirmartion is unnecessary. Tissue culture aims at identifying the inclusion corpuscles in the monolayers of McCoy or HeLa-229 cells, although this technique is not widely available. Direct immunofluorescence can detect bacterial antigens through fluorescent monoclonal antibodies. The complement fixation test and the ELISA (Enzyme-Linked Immunosorbent Assay), which are serologic tests, turn positive after the fourth week of infection. Titer greater than 1:64 suggests, but does not confirm, recent infection, thus the frequent need for pairing after two weeks due to the necessary time for positivation. A four-fold elevation of the titer signals active infection. 4 Serologic tests, however, are also positive in cases of uretritis, cervicitis, conjunctivitis, and psitacosis (caused by other subtypes of Chlamydia). Moreover, the microimmunofluorescence test (MIF) detects the presence of specific antibodies against Chlamydia trachomatis in serum and other secretions. In this test, presence of IgM indicates new infection. 1,4 Histopatological examination does not define the diagnosis in isolation, so an additional serologic exam is recommended. PCR, although of high operational cost, is the most precise technique for diagnosis. 6 Contrary to the reality found in developing countries, nucleic acid amplification techniques (NAAT) are widely available in developed countries.
Differential diagnosis
Soft chancre, syphilis, scrofuloderma, catscratch disease and Hodgkin's disease should be considered.
Treatment
Pregnant women should preferably receive erythromycin (stearate or ethylsuccinate) 500mg orally every 6 hours for 21 days. Oral thiamphenicol can also be used in the dose of 1.5 g for 21 days, but only in the final trimesters of pregnancy. Drainage of buboes (by surgical incision) is contraindicated, except in cases of intense compression for patient's relief and it should be done with thick bevel needles. Late lesions with fibrosis and stenosis in the birth canal may indicate the need for a cesarean section. 1,6 Sexual partners should be treated in case of sexual contact thirty days before the development of clinical manifestations.1
8. SYPHILIS
Syphilis is an infectious disease considered to be systemic from the start, of chronic evolution, subject to acute outbreaks and periods of latency when not treated. It may be spread by sexual contact, blood transfusion and indirectly by uncommon routes, such as contaminated objects and tattoos (acquired syphilis) or vertically (congenital syphilis). 22 Syphilis in pregnancy may lead to abortion, prematurity, neonatal death or development of the disease in the newborn (early and late congenital syphilis). The severity of congenital syphilis is due to the fact that transplacental infection is massive.
Etiologic agent and transmission
Vertical transmission of the spirochetal bacterium Treponema pallidum, by transplacental route, may occur at any time during pregnancy. However, cases of asymptomatic newborns are more associated with transmission in the third trimester. The older the maternal disease, the lower the risk of transmission to the newborn. A pregnant woman who contracted the disease before becoming pregnant or during pregnancy may spread congenital syphilis. In every successive pregnancy with untreated disease the chance of transmission is reduced, but not completely eliminated, continuing to exist in each pregnancy. With regard to sexual transmission, lesions of primary syphilis and some of its secondary stage are rich in treponema and highly infecting, even though in the secondary stage there are high-titer circulating antibodies. 1,22 Therefore, the rate of transmission is higher in the early stages of the disease, when the number of spirochetes in blood circulation is greater, reaching 70100% in the primary and secondary stages. However, in the early latent stage it decreases to 40% and in the late latent stage to 10%. 22
Epidemiology
According to oficial data from the MH it is estimated that of the three million women who give birth in our country per year, 2.6% have syphilis at the time of delivery. 1,3 The WHO estimates that the rate of vertical transmission is 25%, which shows that shyphilis in pregnancy is one of the greatest publich health challenges. 23 This is fairly peculiar because congenital syphilis has been a disease of compulsory notification since 1986, whereas syphilis in pregnancy only recently started to be notified, based on the MH/SVS Nº 33 regulation, of July 14, 2005. We should not forget the high number of unnotified cases, despite this administrative ordinance.
According to the MH, of the cases notified in 2005, nearly 80% of the mothers had the six minimum prenatal visits recommended and more than half of them were diagnosed during pregnancy. However, in only 13% of these cases the partner was treated.
Clinical aspects
After an incubation period ranging from 3 to 90 days (after 21 days on average), a hard chancre, a typical lesion of primary syphilis, appears. In women, lesions are hardly detected at this stage because they are localized in the interior of the genital tract. Clinical manifestations of the secondary stage develop after disappearance of the chancre and involve the skin and mucous membranes, mainly in the form of syphilitic roseolas. 24 Nevertheless, cutaneous lesions may take on various aspects, which make the diagnosis very challenging.
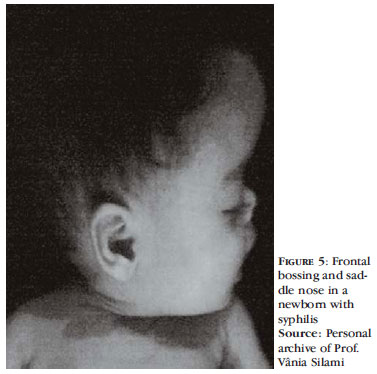
Clinical manifestations in the newborn will vary according to the stage of pregnancy in which the infection occurred. When the mother is infected in the last trimester, the infant is more likely to be born asymptomatic. Congenital syphilis may present with variable clinical manifestations: from hemorrhagic rhinitis, erithematous papular eruption, mucosal plaques, condyloma planum, radial periorificial fissures, pemphigus syphiliticus (Figure 4), microadenopathy and hepatosplenomegaly, intense crying and plateletopenia, among other possible manifestations in early congenital syphilis, to interstitial keratitis, sabre tibia, gummas, Clutton's joints and still other late manifestations. Stigmas such as Hutchinson's teeth (conic, smaller incisors with notches on their biting surface), Parrot's nodes, saddle nose, frontal bossing (Figure 5) and alterations in eye examination, with a "salt and pepper" aspect, may be present. 4
The fact that the newborn may be asymptomatic, but have the infection, alerts to the importance of triage serologic tests, both in the mother and newborn, regardless of the existence or unexistence of clinical signs of the infection. Breastfeeding is only counterindicated for syphilitic mothers if they have cutaneous lesions in the nipple area. 25
Diagnosis
The stage of the disease should be considered for adequate laboratory examination and proper diagnosis.
Direct exams, which show the presence of treponema, are indicated in primary syphilis (chancre), in mucocutaneous lesions of secondary stage (mucosal plaque, condyloma planus, and bulous lesion) and in early congenital syphilis. 1,22,26 They include direct examination by dark-field microscopy, Fontana-Tribondeau staining method, Burri's staining method, Giensa and Levaditi's staining methods, techniques with less resolution than dark-field microscopy, and direct immunofluorescence, which is highly specific and more than 90% sensitive. Serologic tests, in general, are the most frequently performed exams to diagnose syphilis. They are divided into non-treponemic tests - Veneral Disease Research Laboratory (VDRL) and Rapid Plasma Reagin (RPR), important for diagnosis and post-treatment follow-up, and treponemic tests, valid to confirm the infection. The latter include FTA-ABS (Fluorescent Treponemal Antibody Absorption) and TPHA (T. pallidum hemagglutination assay) and variants. 4,22 In addition to these, enzymatic immune assay (EIA) is becoming more popular in the USA as a tracing exam and may substitute nontreponemic tests used for this purpose. It is more specific than RPR and more sensitive than FTA-ABS for past infections. The PCR technique is fairly unemployed, but it may be used, especially for lesions of primary and congenital syphilis and neurosyphilis, with high sensitivity and specificity. Western-blot is another sensitive and specific test, but not routinely employed. 22,27
In Brazil, the MH recommends prenatal serologic triage for syphilis, with the performance of VDRL in the first visit. If negative, the test should be repeated at the beginning of the third trimester and again once labor starts. For pregnant women with positive serology, treatment must be controled through monthly exams until delivery. Serology is also recommended for women who have been admitted to the hospital for post-abortion curettage. Whenever possible, results with low VDRL titer should be confirmed with treponemic tests. If these tests cannot be performed, any titer should be viewed as indicative of active disease and women treated as syphilis carriers. 23
Differential diagnosis
In the primary phase of the disease, differential diagnosis is done with soft chancre, genital herpes, donovanosis, and lymphogranuloma venereum. In the second stage it is done with pharmacodermias, non-vesicular exanthematous diseases, virchowian hanseniasis and colagenoses. In tertiary syphilis, granulomatous diseases such as leprosy, tuberculosis and sarcoidosis should be considered. Attention should be paid to diseases that may yield false-positive results in non-treponemic tests, such as colagenoses, leprosy and chronic infections.
Treatment
Treatment of pregnant women infected with T. pallidum is equal to that of non-pregnant women and according to recommendations: intramuscular benzathine penicillin in the dose of 2,400,000 UI (1,200,000 in each glute), with one administration for primary syphilis, two for secondary syphilis and three for tertiary syphilis, with weekly intervals between them. Any other treatment or treatment conducted thirty days before delivery is considered inappropriate for the prevention of congenital syphilis. Treatment with penicillin is only considered efficient for both the mother and fetus when administered more than 30 days before delivery. 6 Sexual partners of syphilitic pregnant women (even those with negative VDRL) should be treated with a single dose of intramuscular benzathine penicillin 2,400,000 UI. If VDRL is positive, in any titer, treatment should be equal to that of tertiary syphilis. 24
If the pregnant woman is allergic to penicillin, she should be desensitized with oral administration of penicillin V in gradually smaller dilutions and in inversely higher volumes. This procedure should be done in a hospital for better management of possible reactions. Parenteral administration of penicillin should be done only 30 minutes after the end of the desensitization process. In case there is a reaction, the procedure should be suspended and an alternative treatment should be used. Treatment of allergic pregnant women with erythromycin stearate (500 mg every 6 hours for 15 days for primary, secondary and early latent syphilis or for 30 days for late latent syphilis) may cure the mother, but not the fetus. In HIV coinfected patients, the possibility of therapy failure should be considered. 1,6,24
When treatment is conducted in the secondary stage of the disease, there is a greater chance of Jarisch-Herxheimer reaction due to a massive release of dead treponemic antigens in blood circulation. The most typical symptoms are chills, fever, headache and muscle pain, which often appear 4 to 6 hours after administration of benzathine penicillin. In pregnant women this reaction may lead to fetal death, indicating the need for rigorous monitoring of secondary syphilis carriers with high VDRL titers. Prenatal treatment may result in failure in up to 14% of the cases and there is still the possibility of reinfection if the partner has not been simultaneously treated. Therefore, post-treatment follow-up should be conducted, according to the MH, with repetition of sorology in 3,6,9,12, and 18 months. 1 A patient is considered cured when there is a 3 to 4-fold reduction in VDRL titer as compared to the initial titer within a year. 28
9. VULVOVAGINITIS
It is characterized by inflammation or infection of the vulva, vagina and ectocervix, with presence of vaginal discharge and associated symptoms, such as vulvar pruritus, dyspareunia, dysuria and pelvic discomfort, although many cases can be completely asymptomatic. Several factors or aggressive agents can favor the development of vulvovaginitis by modifying the non-pathological vaginal flora. Endogenous infectious agents, trauma, use of tampons and pads, sexual transmission agents, hormone and anatomic changes, in addition to immunodepression, are among them. We will explore below bacterial vaginosis, thrichomoniasis, and vulvovaginal candidiasis.
Bacterial Vaginosis
Etiologic agent and transmission
It is caused by anaerobic bacteria such as Gardnerella vaginalis, Bacteroides sp, Mobiluncus sp, micoplasmas, peptoestreptococos. Infection normally sets in when there is an imbalance of the normal vaginal flora, with a decrease in the number of acidophilus lactobacillus, allowing the proliferation of these etiologic agents. It may be exceptionally sexually spread. 1
Epidemiology
It is the most common infection of the lower genital tract among women of reproductive age, regardless of pregnancy. Prevalence among Western pregnant women ranges between 14 and 21%; the incidence of bacterial vaginosis during pregnancy is higher than that of other infections such as asymptomatic bacteriuria and infection by Neisseria gonorrhoea, Chlamydia trachomatis and Trichomonas vaginalis. Multiple sexual partners, vaginal douche, smoking and premature sexual activity may be risk factors. 29,30
Clinical aspects
Similar to other vulvovaginitis, approximately 50% of women with bacterial vaginosis are asymptomatic. Vaginal discharge, when present, is characterized by a white-grayish exudate, with a creamy aspect and foul-smelling odor, which accentuates after intercourse or mestruation. Absence of pruritus and inflammatory signs is typical. 1,6,7
Diagnosis
The diagnosis is mainly clinical, associated with laboratory findings, and may be established when three of the four criteria below are confirmed: bacterioscopic examination revealing clue-cells; positive amine test after the addition of 0.01 KOH to the vaginal content, resulting in a fetid odor similar to that of fish; vaginal pH higher than 4.5 and presence of white-grayish discharge attached to the vaginal walls. 1
Differential diagnosis
Other causes of vaginal discharge.
Treatment
Bacterial vaginosis has been associated with several adverse effects during pregnancy, such as premature rupture of the amniotic membranes, corioamnionitis, premature labor, postpartum endometritis, intra-amniotic infection and low birth weight. Therefore, all symptomatic pregnant women should be treated and also those asymptomatic with a high risk of pre-term delivery, such as those with a prior history of premature labor. Treatment can be done with oral metronidazole 250 mg three times a day for 7 days or, still, metronidazole 500 mg every 12 hours for 7 days. Another option is oral clindamycin 300 mg every 12 hours for 7 days. 7 Patients must be treated after the first trimester of pregnancy and during breastfeeding. Sexual partners do not necessarily need to be treated. 1
Thrichomoniasis
Etiologic agent and transmission
Thrichomoniasis is an infection caused by Trichomonas vaginalis, an anaerobic, flagellated protozoan, with a typical continuous movement, mainly sexually transmitted.
Epidemiology
According to the WHO, the rates of prevalence of thrichomoniasis among women in developing countries reach 15% or more. Such rates make thrichomoniasis one of the most prevalent diseases worldwide. 31 It is likely that up to 25 million pregnant women throughout the world are infected with thrichomoniasis. 32
Clinical aspects
The disease may be asymptomatic in up to 30% of the cases, including for long periods of time. The incubation period ranges from 4 to 28 days. After incubation, there is abundant purulent, foamy, foulsmelling vaginal discharge (present in about 50% of the cases). Other symptoms that may be present are pruritus and/or vulvar irritation, hyperemia of the mucosa with reddish plaques (diffuse or focal colpitis, with a strawberry cervix aspect), urinary symptoms such as dysuria and polyuria. Vaginal thrichomoniasis is associated with harmful effects in pregnancy, such as premature rupture of membranes, premature labor and low birth weight. 1,7
Diagnosis
The diagnosis is established by direct fresh examination, which may show the presence of mobile flagellated protozoans. Culture is also viable and is indicated for children and in suspicious cases with repeatedly negative smears. If the agent is found in routine oncotic cytology, treatment is indicated. Another diagnostic option is PCR, which limited by high cost. Since thrichomoniasis is considered an STD, women who have been diagnosed with the disease must undergo triage for other STDs. 1,3
Differential diagnosis
Other causes of vaginal discharge.
Treatment
In pregnant women, the treatment recommended by the MH after the third trimester and during lactation is done with a single dose of oral metronidazole 2 g or, in resistant cases, oral metronidazole 400 mg every 12 hours for 7 days. 1 In addition to alleviating the symptoms of vaginal discharge and avoiding new episodes of sexual transmission, treatment prevents respiratory or genital infection in the newborn. So far, no study has shown association of metronidazole and teratogenic effects when used during pregnancy. It is classified as a category B drug by the Food and Drug Administration, USA. During treatment, sexual relations should be avoided. Adequate counseling is also important. Pregnant women should be advised on the need to use preservatives and on the permanent risk of sexual transmission. 7 Sexual partners should always be treated, without the need for diagnostic confirmation. During treatment, alcoholic beverages should be avoided due to the antabuse effect (results from the interaction of imidazoles with alcohol, characterized by discomfort, nausea, dizziness and a metallic taste in the mouth) and sexual relations must be suspended. 1
Vulvovaginal candidiasis
Etiologic agent and transmission
Candida albicans is the most common etiologic agent, responsible for up to 90% of the cases. Occasionally, it may be caused by other species such as C. tropicalis, C. glabrata, C. krusei and C. Parapsilosi. It may be sexually transmitted, but this is not considered the main form of transmission. These are commensal fungi of the vaginal and digestive mucosa that become pathogenic when they alter the normal pattern of the vaginal medium. 1
Epidemiology
Vulvovaginal candidiasis is the most common type of acute vaginitis in tropical countries. Studie show that about 25% of adult women have asymptomatic colonization and 75% of them will show clinical infection at some point in their lives. 33
Clinical aspects
The clinical manifestations of candidiasis are characterized by vaginal and vulvar pruritus, a predominant symptom, and a whitish and thick odorless discharge. The vagina and uterine wall may be covered with white plaques attached to the mucosa. Fissures and maceration of the skin due to itching and scratching may also be observed. Vulvar hyperemia and edema are also frequent, as well as dysuria and dyspareunia. 1
During pregnancy, increase of glycogen in the vaginal epithelium leads to reduction of pH to levels considered below normal, acidifying the medium. This change favors the development of the fungus, which only happens in an acidic environment. 6 In addition to this alteration observed during pregnancy, other factors may facilitate the development of vulvovaginal candidiasis, such as decompensated diabetes mellitus, obesity, use of oral contraceptives, antibiotics, corticoids or immunosuppressors, synthetic or poorly ventilated clothing that increase local humidity and heat, poor hygiene habits, contact with allergenic and irritating substances and immunodefficiencies. 1
Diagnosis
Direct fresh examination of the vaginal content with 10% KOH solution, which reveals the presence of hyphae, pseudo-hyphae and less specifically, birefringent spores. Culture in Saboraud or Nickerson medium should be done when symptoms are indicative of the disease and when it is difficult to confirm the diagnosis by direct fresh examination. 1,6
Differential diagnosis
Contact dermatitis, irritation and trauma by intercourse, hypersensititvity and other causes of vaginal discharge.
Treatment
In pregnant women, the MH recommends treatment after the first trimester of pregnancy and during lactation with miconazole 2%, cream administered vaginally before bedtime for 7 days. Another option is clotrimazole 1% cream applied to the vagina at night for 6 to 12 days or nystatin 100,000 UI applied vaginally before bedtime for 14 days. 1 For recurring cases of candidiasis in pregnancy, some authors recommend the correction of vaginal pH with genital baths with sodium bicarbonate diluted in water. 6 Partners do not need to be treated since sexual transmission is not common, except in symptomatic and recidivous cases. 1
CONCLUSION
Physiological alterations of the maternal organism may alter the course of STDs and lead to obstetrical and neonatal complications. We believe this work will raise the awareness of health professionals about the diagnosis, which should be as early as possible, and treatment of these diseases because it explores the particularities of the natural and therapeutic history of the main STDs in the gestational period. Treatment, which oftentimes has limitations due to inherent toxicity, must preserve the physical integrity of the mother and baby, eliminating risks and complications. Preventive measures and the treatment of sexual partners also contribute substantially to the effectiveness of our actions. In this context, triage of STDs during prenatal care is extremely important for early diagnosis and better therapy management.
ACKNOWLEDGEMENTS:
The authors would like to thank Professor Vânia Glória Silamo Lopes (Department of Pathology, Fluminense Federal University) for granting the photos of congenital syphilis, and Dr. Airá Novello Vilar for granting the photo of the herpetic lesion content microscopy.
REFERENCES
- 1. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Programa Nacional de DST/AIDS. Manual de Controle das Doenças Sexualmente Transmissíveis. 4Ş ed. Brasília: Ministério da Saúde, 2006.
- 2. Martins TA, Bello PY, Pontes LRSK, Costa LV, Miralles IS, Queiroz TRBS. As doenças sexualmente transmissíveis são problemas entre gestantes no Ceará? DST J Bras Doenças Sex Transm. 2004;16:50-8.
- 3. Gavazzoni MF, Perissé ARS, Nery JAC. Sífilis e outras doenças sexualmente transmissíveis. In: Azulay-Abulafia L, Alves GF, Costa A. Dermatologia e Gravidez. Rio de Janeiro: Elsevier, 2009, p. 277-292.
- 4. Manela-Azulay M, Azulay DR. Doenças Sexualmente Transmissíveis. In: Dermatologia. Azulay RD, Azulay DR, Azulay-Abulafia L. 5 ed. Rio de Janeiro: Guanabara-Koogan; 2008. p.367-88.
- 5. Einarson A, Shuhaiber S, Koren G. Effects of antibacterials on the unborn child: what is known and how should this influence prescribing. Paediatr Drugs. 2001;3:803-16.
- 6. Duarte G. Doenças sexualmente transmissíveis e gravidez. In: Linhares IM, Duarte G, Giraldo PC, Bagnoli VR. Manual de Orientação, DST/AIDS - Federação Brasileira das Associações de Ginecologia e Obstetrícia (FEBRASGO). São Paulo; 2004. p. 118-41.
- 7. Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines. MMWR. 2006;55:1-94. (No. RR-11)
- 8. Penna GO, Hajjar LA, Braz TM. Gonorréia. Rev Soc Bras Med Trop. 2000;33:451-64.
- 9. Sarkar M, Woodland C, Koren G, Einarson AR. Pregnancy outcome following gestational exposure to azithromycin. BMC Pregnancy Childbirth. 2006;6:18.
- 10. Dienstag JL. Hepatite Viral Aguda. In: Braunwald E, Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, et al. Harrison Medicina Interna. 17 ed. Rio de Janeiro: McGraw-Hill Interamericana do Brasil; 2008. p.1932-48.
- 11. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Hepatites Virais: O Brasil está atento. 3 ed. Brasília, DF: Ministério da Saúde; 2008.
- 12. Conceição OJG, Focaccia R. Hepatite C e Gestação. II Consenso da Sociedade Paulista de Infectologia para Manuseio e Terapia da Hepatite C. Sociedade Paulista de Infectologia; 2004. p.10.
- 13. Melo VH, Pires do Rio SM. Projeto Diretrizes. Associação Médica Brasileira e Conselho Federal de Medicina. Assistência Pré-Natal. Federação Brasileira das Associações de Ginecologia e Obstetrícia (FEBRASGO). 2006, p.3-11.
- 14. Ministério da Saúde. Programa Nacional de Hepatites Virais. Protocolo Clínico e Diretrizes Terapêuticas Hepatite Viral Crônica B: Lamivudina, Interferon-alfa. Série C. Projetos, Programas e Relatórios. Brasília, DF; 2002.
- 15. Centers for Disease Control and Prevention. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP); Part 1: Immunization of Infants, Children, and Adolescents. MMWR. 2005;54: p.1-32. (No. RR-16)
- 16. Sousa AQ. I Consenso da Sociedade Brasileira de Infectologia para Diagnóstico e Manuseio da Hepatite B e Delta. Braz J Infect Dis. 2006;10(Sup.1):1-78.
- 17. Rodriguez MDM, Obasi A, Mosha F, Todd J, Brown D, Changalucha J, et al. Herpes simplex virus type 2 increases HIV incidence: a prospective study in rural Tanzania. AIDS. 2002;16:451-62.
- 18. Guedes ACM, Avelleira JCR, Lupi O, Abraham LS, Azulay DR, Azulay-Abulafia L. Doenças Virais de Interesse Dermatológico. In: Azulay RD, Azulay DR, Azulay-Abulafia L. Dermatologia. 5 ed. Rio de Janeiro: Guanabara-Koogan; 2008. p. 274-300.
- 19. Rama CH, Roteli-Martins CM, Derchain SFM, Longatto-Filho A, Gontijo RC, Sarian LOZ, et al. Prevalência do HPV em mulheres rastreadas para o câncer cervical. Rev Saúde Pública. 2008;42:123-30.
- 20. Clifford GM, Gallus S, Herrero R, Munõz N, Snijders PJF, Vaccarella S, et al. Worldwide distribution of Human papillomavirus types in cytologically normal women in the International Agency for Research on Cancer HPV prevalence surveys: a pooled analysis. Lancet. 2005;366:991-8.
- 21. Igansi CN. Prevalência de papilomavírus humano (HPV) e Chlamydia trachomatis (CT) e sua associação com lesões cervicais em uma amostra de mulheres assintomáticas de Porto Alegre, RS [dissertação]. Porto Alegre, RS: Universidade Federal do Rio Grande do Sul; 2005.
- 22. Avelleira JCR, Bottino G. Sífilis: diagnóstico, tratamento e controle. An Bras Dermatol. 2006;81:111-26.
- 23. Serviço de Vigilância Epidemiológica / Coordenação do Programa Estadual DST/AIDS-SP / Secretaria de Estado da Saúde - SES-SP. Informe técnico institucional: Sífilis congênita e sífilis na gestação. Rev Saúde Pública. 2008;42:768-72.
- 24. Saraceni V, Leal MC. Avaliação da efetividade das campanhas para eliminação da sífilis congênita na redução da morbi-mortalidade perinatal: Município do Rio de Janeiro, 1999-2000. Cad. Saúde Pública. 2003;19:1341-49.
- 25. Lamounier JA, Moulin ZS, Xavier CC. Recomendações quanto à amatentação na vigência de infecção materna. J Pediatr. 2004;80(5 Supl):S181-8.
- 26. Belda Jr W, Shiratsu R, Pinto V. Abordagem nas doenças sexualmente transmissíveis. An Bras Dermatol. 2009;84:151-9.
- 27. Rotta O. Diagnóstico sorológico da sífilis. An Bras Dermatol. 2005;80:299-302.
- 28. Manela-Azulay M, Azulay DR. Treponematoses, sífilis. In: Azulay RD, Azulay DR, Azulay-Abulafia L. Dermatologia. 5 ed. Rio de Janeiro: Guanabara-Koogan; 2008, p. 349-66.
- 29. Thinkhamrop J. Antibiotics for treating bacterial vaginosis in pregnancy: RHL commentary. The WHO Reproductive Health Library; Geneva: World Health Organization. [cited 2009 Aug 15]. Available from: http://apps.who.int/rhl/pregnancy_childbirth/complications/infection/jatcom/en/
- 30. Yudin MH. Screening and management of bacterial vaginosis in pregnancy. J Obstet Gynaecol Can. 2008;30:702-16.
- 31. Schmid G. Trichomoniasis treatment in women: RHL commentary. The WHO Reproductive Health Library; Geneva: World Health Organization. [cited 2009 Aug 23]. Available from: http://apps.who.int/rhl/rti_sti/gscom/en/index.html
- 32. Walker G. Interventions for trichomoniasis in pregnancy: RHL commentary. The WHO Reproductive Health Library; Geneva: World Health Organization. [cited 2009 Aug 23]. Available from: http://apps.who.int/rhl/rti_sti/gwacom/en/
- 33. Holanda AAR, Fernandes ACS, Bezerra CM, Ferreira MAF, Holanda MRR, Holanda JCP, et al. Candidíase vulvovaginal: sintomatologia, fatores de risco e colonização anal concomitante. Rev Bras Ginecol Obstet. 2007;29:3-9.
Sexually transmitted diseases during pregnancy: a synthesis of particularities
Publication Dates
-
Publication in this collection
27 Jan 2011 -
Date of issue
Dec 2010
History
-
Received
19 Apr 2010