Abstracts
Although its rarity, the adventitial cystic disease of the popliteal artery (ACDPA) must be remembered in the differential diagnosis of intermittent claudication in young patient's lower limbs. Brazilian literature presents a few cases of this disease. This study is a case report of ACDPA in a male patient, with a literature review, comparing to popliteal artery entrapment syndrome.
Intermittent claudication; popliteal artery; cysts
Apesar de sua raridade, a doença cística da artéria poplítea (DCAP) deve ser lembrada no diagnóstico diferencial de claudicação intermitente de membros inferiores em pacientes jovens. A literatura brasileira apresenta poucos relatos dessa doença. Este trabalho reportou o caso de um paciente masculino portador de DCAP e revisou a literatura, traçando um paralelo com a síndrome de aprisionamento da artéria poplítea.
Claudicação intermitente; artéria poplítea; cistos
CASE REPORT
IVascular Surgeon specialized at the Brazilian Society of Angiology and Vascular Surgery (SBACV), Novo Hamburgo (RS), Brazil
IIPhysician, Novo Hamburgo (RS), Brazil
IIIVascular Surgeon specialized at the SBACV; Professor of Vascular Surgery at Universidade Luterana do Brasil (ULBRA), Canoas (RS), Brazil
Correspondence
ABSTRACT
Although its rarity, the adventitial cystic disease of the popliteal artery (ACDPA) must be remembered in the differential diagnosis of intermittent claudication in young patient's lower limbs. Brazilian literature presents a few cases of this disease. This study is a case report of ACDPA in a male patient, with a literature review, comparing to popliteal artery entrapment syndrome.
Keywords: Intermittent claudication, popliteal artery, cysts.
Introduction
Cystic disease of the popliteal artery (CDPA) and popliteal artery entrapment syndrome (PAES) are the leading causes of lower limb claudication in young patients. CDPA has been little studied due to its rarity. Its etiology is not clear, and its existence must always be remembered by the vascular surgeon. The Brazilian literature presents some case reports1-5, references in meetings6-8, and a personal communication on this theme2.
Case description
RLS, 39-year-old Caucasian male, soccer teacher, complained of calf pain for 1 year and its worsening for 8 years, when he started presenting paleness and 100-m intermittent claudication of right lower limb, followed by right foot paresthesia. The patient's history indicated right ruptured cruciate ligament 18 years earlier, confirmed by magnetic resonance imaging, which showed anterior ruptured cruciate ligament, injured meniscus, severe arthrosis on the right knee and mild arthrosis on the left knee (Figure 1). The patient did not present risk factors for atherosclerotic disease. Physical examination revealed important muscle hypertrophy on both calves. Distal arterial pulses were present, but disappeared during passive dorsiflexion maneuvers of the feet and extension of the knees.
Doppler ultrasonography imaging suggested right popliteal artery aneurysm with disappearance of arterial flow after prolonged calf contraction (Figures 2 and 3). Arteriography of the right inferior limb showed absence of medial popliteal artery deviation (Figure 4).
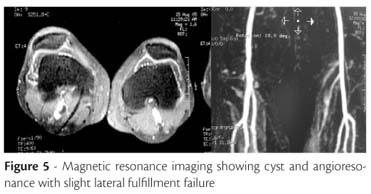
Magnetic resonance imaging confirmed the aneurysmal formation in the right popliteal artery, ruling out anomalous muscle insertions (Figure 5).
Retrospectively, subtle signs of lateral entrapment of the popliteal artery in juxta-articular position were identified by angiographic images.
The treatment was open surgical intervention via posterior approach of the right popliteal fossa. A large multilocular adventitial cyst was observed in the popliteal artery, between its distal and medium thirds. The rest of the vessel had no anatomical alterations (Figure 6).
The exploration of the popliteal fossa did not identify Baker cyst or muscle compression.
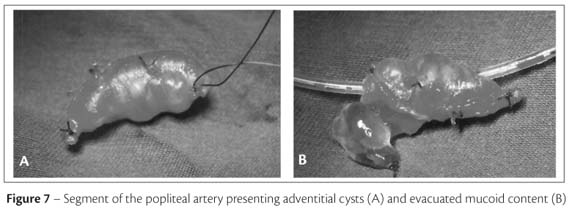
Dissection of the popliteal artery demonstrated an important involvement of the vessel by the cystic formation, without precise limits between them (Figure 7A), thus causing lumen compression due to the firm consistency of the cysts. The slight adherence to the adjacent tissues allowed release of the cystic mass without rupture or macroscopic extravasation of the content. Resection of the impaired arterial segment and interposition of the inverted ipsilateral internal saphenous vein segment were the chosen surgical techniques. Macroscopic analysis of the surgical specimen demonstrated a viscous substance in the cystic formation (Figure 7B). Histopathological analysis confirmed the adventitial mucinous degeneration with a material containing protein and histiocytes. The patient has had a 49-month follow-up and has reported absence of symptoms and of physical restriction.
Discussion
Lower limb intermittent claudication in young patients without evident etiological factors for arteriosclerotic disease is rare. The most common etiologies are PAES and CDPA, which is considered to be the cause of 1 in 1,200 cases of intermittent claudication2. Extrinsic compression and embolism of the popliteal artery, thromboangiitis obliterans and fibromuscular dysplasia3,4 are also diagnostic possibilities.
Some particularities of the differential diagnosis between PAES and CDPA are henceforth discussed taking into account the age, sex, clinical features, alterations found in semiologic maneuvers and imaging examinations.
Age
Symptoms of PAES are common in young individuals until the third decade of life, while those of CDPA occur preferentially between the fourth and the sixth decades. It is worth emphasizing that entrapment may go unnoticed for years, hence this hypothesis should not be rejected in individuals of all age groups1.
Genre
Both diseases are more common in males: PAES presents a frequency of 8:1 and CDPA of 4.7:12.
Clinical presentation
There are cases of PAES resulting only from calf muscular hypertrophy. However, the vast majority of cases are caused by congenital anomaly of the anatomical relation between the popliteal vessels and the remaining adjacent structures. In the described case, the presence of muscular hypertrophy made the diagnosis more difficult.
In both CDPA and PAES, there may be any degree of ischemic manifestations, depending on the extension of involvement and on the time of disease development. Both CDPA and PAES may also present asymptomatic periods. As a justification of this finding, some authors suggest that, in some cases, the synovial capsule and the cyst may communicate, thus modifying the intermittent pressure in its interior9. Spontaneous remission of the disease in a ten-year follow-up has been reported10.
In PAES, there is bilaterality in almost 25% of the cases11, while in CDPA there is only one case reported in literature12.
Semiologic maneuvers
In PAES, disappearance of distal pulses with knee extension and passive dorsiflexion of the feet are frequently found, as reported by McDonald13. The maneuver may be performed with the aid of computed tomography scan or ultrasonography11. However, one should be aware of the possibility of false negative results11 in the presence of hypertrophy of the calves, as confirmed by echocardiography in this case. Ishikawa14 described a maneuver of knee flexion with disappearance of the limb distal pulse related to CDPA.
Imaging techniques
Doppler ultrasonography, magnetic resonance imaging or computed tomography may be useful in the morphological identification of the artery and its relation with adjacent structures15-17. Due to the rarity of these findings, the image of a cyst may be mistaken for aneurysm or pseudoaneurysm, and the internal viscous substance may be mistaken for hypoechogenic mural thrombi. On the other hand, post-stenosis aneurysmal injuries may be found in 6.7% of the entrapments18. In CDPA, the arteriography can reveal compression of the artery affected by the cyst the scimitar sign15.
A detailed study can identify small alterations in images. In PAES, there may be medial deviation of the artery, presence of collateral circulation and decrease or absence of blood flow with active flexion of the feet. There are reports of entrapment without arterial deviation and with post-stenosis aneurysmal dilatation19.
Etiopathogeny of the cystic disease of the popliteal artery
CDPA is an uncommon morphological alteration. The disease has a higher incidence in the popliteal artery. There are reports of cases with involvement of the external, femoral, radial, ulnar and brachial iliac arteries20, and even veins21. Some authors report the presence of mucoid cysts originated in other sites of the vessel wall, besides the adventitia, as in the intima-media layers20,22. The etiology is unknown and controversial.
In 1998, South African authors presented a theory called "unifier hypothesis" considering that the cysts were traces of ganglion cells in non-axial vessel junctions23.
Other authors indicate that repeated trauma is a possible etiologic factor2. The present case support this hypothesis, here represented by the degenerative alterations and ligamentous lesion of the right knee resulting from past trauma, as shown by magnetic resonance imaging.
Some authors9,22,24 report cystic communication with the knee. This fact supports the hypothesis that adventitial cysts are actually synovial cysts that infiltrated the adventitia. Conversely, there is no explanation for the difference in the amount of hyaluronic acid found in the synovial fluid in comparison to the content of the cysts25. The presence of macroscopic communications of the cyst with other adjacent structures was not identified.
Saudi authors suggested, in 2007, the possibility of association of CDPA with the intimomedial mucoid degeneration. Meanwhile, other authors found it related to the etiology of aneurysmal formations20.
Treatment
Simple aspiration of the cysts may be performed under echographic26, tomographic11 or transoperative9,17 guidance. When considering the possibility of simple cyst evacuation, one must observe the structure of the reminiscent artery and pay attention to the possibility of unsuccessful intervention and recurrence, which occurs in 10% of cases in some reports10. Due to the viscosity of the fluid, simple aspiration may not be easy9. In this case, adventitia resection is an alternative27. Angioplasty must only be considered in exceptional cases28,29. When there is arterial occlusion, fibrosis or partial destruction of its wall by the cyst, excision and replacement by a venous graft are recommended, an alternative considered to be reliable and safe, with lower recurrence rate3,4,29.
Conclusion
This paper reported the case of a patient presenting a clinical picture compatible with CDPA (which etiology remains unknown), who underwent successful conventional surgical treatment.
References
- 1. Maffei FH, Barbosa AG, Rollo HA, Neser A, Lastoria S. Adventitial cystic disease of the popliteal artery in Brazil: additional data on the geographical distribuition of the disease. Angiology. 1982;33:339-42.
- 2. Castiglia V. Doença cística das artérias. In: Maffei FHA, Lastória S, Yoshida WB, Rollo HA. Doenças vasculares periféricas. Rio de Janeiro: Medsi; 2002. p. 1291-304.
- 3. Cardoso EJ, Teixeira RJ, Galego G, Boabaid RS. Doença cística da adventícia da artéria poplítea. Arquivos Catarinenses de Medicina. 1991;20:181-3.
- 4. Miranda Junior F, Francisco Junior J, Burihan E. Cisto de artéria poplítea. Rev Bras Cir. 1982;72:221-2.
- 5. Rollo HA, Gama JC, Lastoria S, Yoshida WB, Maffei FH. Cisto de adventícia em artéria poplítea. Relato de dois casos. AMB Rev Assoc Med Bras. 1982;28:79-81.
- 6. Alioti R, Prado RF, Boemer VM e col. Doença cística da artéria poplítea: relato de dois casos. J Vasc Bras. 2005;4:S119.
- 7. Siqueira MK, Van Bellen B. Doença cística da artéria poplítea: relato de caso e revisão de literatura. J Vasc Bras. 2005;4:S166.
- 8. Navarro TP, Castro KP, Junior ACR, Gomes CV, Caetano D. Doença cística de artéria poplítea em paciente assintomático - relato de caso. J Vasc Bras. 2007;6:42.
- 9. Cassar K, Engeset J. Cystic adventitial disease: a trap for the unwary. Eur J Vasc Endovasc Surg. 2005;29:93-6.
- 10. Pursell R, Torrie EP, Gibson M, Galland RB. Spontaneous and permanent resolution of cystic adventitial disease of the popliteal artery. J R Soc Med. 2004;97:77-8.
- 11. Jasinski RW, Masselink BA, Partridge RW, Deckinga BG, Bradford PF. Adventitial cystic disease of the popliteal artery. Radiology. 1987;163:153-5.
- 12. Ortiz M WR, Lopera JE, Gimenéz CR, Restrepo S, Moncada R, Castañeda-Zúñiga WR. Bilateral adventitial cystic disease of the popliteal artery: a case report. Cardiovasc Intervent Radiol. 2006;29:306-10.
- 13. McDonald PT, Easterbrook JA, Rich NM, et al. Popliteal artery entrapment syndrome. Clinical, noninvasive and angiographic diagnosis. Am J Surg. 1980;139:318-25.
- 14. Ishikawa K, Mishima Y, Kobayashi S. Cystic adventitial disease of the popliteal artery. Angiology. 1961;12:357-66.
- 15. Fox CJ, Rasmussen TE, O'Donnell SD. Cystic adventitial disease of the popliteal artery. J Vasc Surg. 2004;39:1351.
- 16. Brodmann M , Stark G, Pabst E, et al. Cystic adventitial degeneration of the popliteal artery - the diagnostic value of duplex. Eur J Radiol. 2001;38:209-12.
- 17. Papavassiliou VG, Nassim A, Awad EM, Bell PR. Adventitial cystic disease of the popliteal artery: diagnosis and treatment. A case report. J Cardiovasc Surg (Torino). 2002;43:399-401.
- 18. Castiglia V. Síndrome do aprisionamento da artéria poplítea. In: Maffei FHA, Lastória S, Yoshida WB, Rollo HA. Doenças vasculares periféricas. Rio de Janeiro: Medsi; 2002. p. 1305-16.
- 19. Elias DA, White LM, Rubenstein JD, Christakis M, Merchant N. Clinical evaluation and mr imaging features of popliteal artery entrapment and cystic advential disease. AJR Am J Roentgenol. 2003;180:627-32.
- 20. Wali MA, Dewan M, Renno WM, Ezzeddin M. Mucoid degeneration of the brachial artery: case report and a review of literature. J R Coll Surg Edinb. 1999;44:126-9.
- 21. Dix FP, McDonald M, Obomighie J, et al. Cystic adventitial disease of the femoral vein presenting as deep vein thrombosis: a case report and review of the literature. J Vasc Surg. 2006;44:871-4.
- 22. Unno N, Kaneko H, Uchiyama T, Yamamoto N, Nakamura S. Cystic adventitial disease of the popliteal artery: elongation into the media of the popliteal artery and communication with the knee joint capsule: report of a case. Surg Today. 2000;30:1026-9.
- 23. Levien LJ, Benn CA. Adventitial cystic disease: a unifying hypothesis. J Vasc Surg. 1998;28:193-205.
- 24. Galle C, Cavenaile JC, Hoang AD, et al. Adventitial cystic disease of the popliteal artery communicating with the knee joint. A case report. J Vasc Surg. 1998;28:738-41.
- 25. Rispoli P, Moniaci D, Zan S, et al. Cystic adventitial disease of the popliteal artery. Report of 1 case and review of the literature. J Cardiovasc Surg (Torino). 2003;44(2):255-8.
- 26. Asciutto G, Mumme A, Marpe B, Hummel T, Geier B. Different approaches in the treatment of cystic adventitial disease of the popliteal artery. Chir Ital. 2007;59:467-73.
- 27. Stierli P, Mauch J, Koella C, Huber A, Eugster T, Gürke L. Circumferential removal of the adventitia for cystic degeneration of the popliteal artery. Br J Surg. 2005;92:56-7.
- 28. Setacci F, Sirignano P, de Donato G, Chisci E, Palasciano G, Setacci C. Adventitial cystic disease of the popliteal artery: experience of a single vascular and endovascular center. J Cardiovasc Surg (Torino). 2008;49:235-9.
- 29. Khoury M. Failed angioplasty of a popliteal artery stenosis secondary to cystic adventitial disease a case report. Vasc Endovascular Surg. 2004;38:277-80.
Cystic disease of the popliteal artery: a case report
Publication Dates
-
Publication in this collection
09 Feb 2011 -
Date of issue
Sept 2010
History
-
Received
12 Feb 2010 -
Accepted
28 Apr 2010