Abstract
Background
Cerebrovascular diseases (CBVD) are the second major cause of death in the world.
Objective
To analyze the mortality trend of CBVD in Brazil (1996 to 2015) and its association with Human Development Index (HDI) and the Social Vulnerability Index (SVI).
Methods
This is an ecological study. We analyzed the mortality rate standardized by CBVD. Death data were obtained from the Mortality Information System (SIM) and populational data from the Brazilian Institute of Geography and Statistics (IBGE). The model of regression by inflection points (Joinpoint regression) was used to perform the temporal analysis, calculating the Annual Percent Change (APC) and Average Annual Percent Change (AAPC), with 95% of confidence interval and a significance of 5%. Trends were classified as increasing, decreasing or stationary. A multivariate regression model was used to analyze the association between mortality by CBVD, HDI and SVI.
Results
During this period, 1,850,811 deaths by CBVD were recorded. We observed a reduction in the national mortality rate (APC -2.4; p = 0.001). Twenty federation units showed a significant trend, of which 13 showed reduction, including all states in the Midwest (n=4), Southeast (n=4) and South (n=3). The HDI was positively associated and the SVI was negatively associated with mortality (p = 0.046 and p = 0.026, respectively).
Conclusion
An unequal epidemiological course of mortality was observed between the regions, being higher in the Southeast and South states, with a significative tendency of reduction, and lower in the North and Northeast states, but with a significative tendency of increase. HDI and SVI showed an association with mortality. (Arq Bras Cardiol. 2021; 116(1):89-99)
Brain Diseases/mortality; Epidemiology; Community Development; Social Vulnerability; Time Seies Studies; Morbimortality; Stroke/mortality; Emergency Medical Emergencies/organization and administration
Resumo
Fundamento
As doenças cerebrovasculares (DCBV) constituem a segunda causa de mortes no mundo.
Objetivo
Analisar a tendência da mortalidade por DCVB no Brasil (1996-2015) e associação com o índice de desenvolvimento humano (IDH) e o índice de vulnerabilidade social (IVS).
Métodos
Trata-se de estudo ecológico envolvendo as taxas de mortalidade padronizadas por DCBV. Os dados dos óbitos foram obtidos do Sistema de Informações sobre Mortalidade e os dados populacionais, do Instituto Brasileiro de Geografia e Estatística. Para as análises temporais, foi utilizado o modelo de regressão por pontos de inflexão, sendo calculado o percentual de variação anual (annual percent change [APC]) e médio do período (average annual percent change [AAPC]), com intervalo de confiança de 95% e significância de 5%. As tendências foram classificadas em crescente, decrescente ou estacionária. O modelo de regressão multivariada foi utilizado para testar a associação entre a mortalidade por DCBV, IDH e IVS.
Resultados
Foram registrados 1.850.811 óbitos por DCBV no período estudado. Observou-se redução da taxa de mortalidade nacional (APC: -2,4; p = 0,001). Vinte unidades federativas apresentaram tendências significativas, sendo 13 de redução, incluindo todos das regiões Centro-Oeste (n = 4), Sudeste (n = 4) e Sul (n = 3). O IDH teve associação positiva e o IVS, associação negativa com a mortalidade (p = 0,046 e p = 0,026, respectivamente).
Conclusão
O estudo mostrou comportamento epidemiológico desigual da mortalidade entre as regiões, sendo maior nos estados do Sudeste e Sul, porém com tendência significativa de redução, e menor nos estados do Norte e Nordeste, mas com tendência significativa de crescimento. O IDH e o IVS associaram-se com a mortalidade. (Arq Bras Cardiol. 2021; 116(1):89-99)
Encefalopatias/mortalidade; Epidemiologia; Desenvolvimento da Comunidade; Vulnerabilidade Social; Estudos de Séries Temporais; Morbimortalidade; Acidente Vascular Cerebral/mortalidade; Serviços Médicos de Emergência/organização e administração
Introduction
Chronic non-communicable diseases (CNCD) have occupied a prominent place in the epidemiological scenario, representing the biggest global health problem and causing about 38 million deaths annually (70% of all deaths), 16 million of which are considered premature (age < 70 years).11. World Health Organization. (WHO). Health statistics and information systems. Estimates for 2000-2016. [Internet]. Genebra: WHO; 2018. [Acesso em 21 out 2018].Disponível em: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html.
http://www.who.int/healthinfo/global_bur...
In Brazil, approximately 75% of deaths are caused by CNCD, which represents more than 1 million deaths each year.22. Malta DC, França E, Abreu DMX, Perillo RD, Salmen MC, Teixeira RA, et al. Mortality due to noncommunicable diseases in Brazil, 1990 to 2015, according to estimates from the Global Burden of Disease study. São Paulo Med J. 2017;135(3):213-21.
The CNCD group consists of four subgroups: cardiovascular diseases (CVD), cancer, chronic respiratory disease and diabetes mellitus. Among the CVD, cerebrovascular diseases (CBVD) stand out, being the second leading cause of mortality in the world, behind ischemic heart diseases. Together, they were responsible for 15.2 million deaths in 2016.11. World Health Organization. (WHO). Health statistics and information systems. Estimates for 2000-2016. [Internet]. Genebra: WHO; 2018. [Acesso em 21 out 2018].Disponível em: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html.
http://www.who.int/healthinfo/global_bur...
,33. World Health Organization. The top 10 causes of death [Internet]. Genebra: WHO; 2018. [Acesso em 22 oute 2018]. Disponível em: http://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
http://www.who.int/news-room/fact-sheets...
Of the Latin American countries, Brazil has one of the highest mortality rates due to CBVD. In the last decades, there was a significant increase in the number of deaths, from 104,000 in 1990 to 144,000 in 2015. On the other hand, the country has experienced a reduction in mortality rates, especially regarding early mortality, which decreased from 51.4% in 1990 to 35.1% in 2015.44. Lotufo PA, Goulart AC, Passos VMA, Satake FM, Souza MFM, França EB, et al. Cerebrovascular disease in Brazil from 1990 to 2015: Global Burden of Disease 2015. Rev Bras Epidemiol. 2017;20(1):129-41.
The impact of CBVD on morbidity and mortality is a challenge for the economic and social development of nations, especially in developing countries, which concentrate about 80% of all CBVD deaths.11. World Health Organization. (WHO). Health statistics and information systems. Estimates for 2000-2016. [Internet]. Genebra: WHO; 2018. [Acesso em 21 out 2018].Disponível em: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html.
http://www.who.int/healthinfo/global_bur...
,55. Alwan A, Maclean DR, Riley LM, d’Espaignet ET, Mathers CD, Stevens GA, et al. Monitoring and surveillance of chronic non-communicable diseases: progress and capacity in high-burden countries. Lancet. 2010;376(9755):1861-8. Monitoring the temporal behavior of indicators in Brazil, a country of continental dimensions and with important socio-spatial inequalities, is of fundamental importance for the definition of public policies that can impact the population’s health situation.66. Vincens N, Stafström M. Income inequality, economic growth and stroke mortality in Brazil: longitudinal and regional analysis 2002-2009. PLoS One. 2015;10(9):e0137332.
In this sense, this study aimed to analyze the trend of mortality from CBVD in Brazil (1996-2015) and its association with the Human Development Index (HDI) and the Social Vulnerability Index (SVI).
Methods
Study design, population and period
This is an ecological study involving all CBVD deaths that occurred in Brazil from 1996 to 2015 and the HDI and SVI. The entire country, the country regions and the federation units were adopted as the analysis units.
Variables
We analyzed the following sociodemographic variables: gender (male, female and unknown), age groups – in years (0-4, 5-9, 10-14, 15-19, 20-29, 30-39, 40-49, 50- 59, 60-69, 70-79, 80 and over and unknown age), education - in years (illiterate, 1-3, 4-7, 8-11, 12 or more and unknown education) and marital status (single, married, widowed, divorced, other and unknown marital status). For the time series analysis, the variable mortality rate standardized by age and gender due to CBVD was included. For the association component, two social indices were selected: i) the HDI and its three dimensions (longevity, education and income) and ii) SVI and its three dimensions (urban infrastructure, human capital and income and work). These two indices measure, respectively, the degree of human development and the degree of social vulnerability to which a population is exposed.
Data source and data collection
Death data were collected from the Ministry of Health’s Mortality Information System (SIM) (http://datasus.saude.gov.br/).77. Brasil. Ministério da Saúde. Sistema de informações sobre mortalidade (SIM). [Acesso em 13 de agosto 2018]. Disponível em: http://datasus.saude.gov.br/.
http://datasus.saude.gov.br/...
The International Disease Code (ICD-10) I60 to I69 was considered: I60- Subarachnoid hemorrhage; I61- Intracerebral hemorrhage; I62- other non-traumatic intracranial hemorrhages; I63- Cerebral infarction; I64- Stroke not specified as hemorrhagic or ischemic; I65- Occlusion / stenosis of pre-cerebral arteries that do not result in cerebral infarction; I66- Occlusion / stenosis of cerebral arteries that do not result in cerebral infarction; I67- Other cerebrovascular diseases; I68- Cerebrovascular disorders in diseases classified elsewhere; and I69- Sequelae of cerebrovascular diseases.88. Organização Mundial da Saúde. Classificação estatística internacional de doenças e problemas relacionados à saúde- CID 10. 10ª revisão. São Paulo: Centro Colaborador da Organização Mundial da saúde para a Classificação de Doenças em Português. Brasília, DF: OMS; 1995. The population data necessary to calculate the indicators were obtained from the Brazilian Institute of Geography and Statistics (IBGE).99. Instituto Brasileiro de Geografia e Estatística. Sistema de Recuperação automática de dados- SIDRA. [Acesso em 15 de julho 2018]. Disponível em: https://sidra.ibge.gov.br/home /ipp/Brasil.
https://sidra.ibge.gov.br/home...
To obtain the rates the following equations were used:
a) Annual mortality rate: number of deaths due to CBVD in the local and year /local population and year X 100,000 inhabitants;
b) Mortality rate for the period (1996-2015): mean number of deaths from CBVD of the time series (1996-2015)/population median of the time series (population mean of 2005 and 2006) x 100.000 inhabitants.
Finally, the HDI was obtained from the human development atlas (http://atlasbrasil.org.br/2013/) and the SVI from the social vulnerability atlas (http://ivs.ipea.gov.br/index.php/pt/), based on the year 2010. It should be noted that the HDI and SVI data are only calculated in the census years.
Standardization of mortality rates
In order to reduce the effects of the population-demographic structure, the crude rates were standardized by gender and age using the direct method, considering the Brazilian population in 2010 (census year) as the standard population and the following age groups: 0-4, 5 -9, 10-14, 15-19, 20-29, 30-39, 40-49, 50-59, 60-69, 70-79 and 80 or more.
Statistical analysis
For the temporal analysis, the inflection point regression model (joinpoint regression model) was used. The model tests whether a line with multiple segments is more adequate to explain the temporal behavior of a data set when compared to a straight line or one with fewer segments. Therefore, the joinpoint allows identifying the trend of each indicator (whether stationary, increasing or decreasing), the points in time in which there is a change in this trend (joins), as well as the annual percentage variation (APC- Annual Percent Change) and the total period (AAPC- Average Annual Percent Change).1010. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-51. In the model configuration, the following parameters were adopted: minimum number of joins: zero; maximum number of joins: three; selection of the best model: Monte Carlo permutation test (n = 4499 permutations); error autocorrelation method: method based on date; confidence interval: 95% (95% CI); and significance level: 5%.
For the analysis of the association between social indicators and the standardized mortality rate, the multivariate regression model (OLS - Ordinary Least Square) was adopted.
For the analyses, the software Joinpoint Regression 4.5.0.1 (National Cancer Institute. USA), GeoDa 1.10.0.8 (University of Illinois at Urbana-Champaign, USA) and QGis 2.14.11 (Open Source Geospatial Foundation, USA) were used. The territorial meshes necessary for making the maps came from IBGE.
Ethical aspects
This study used secondary data in the public domain, in which it is not possible to identify the subjects. For this reason, the local Research Ethics Committee approval has been waived.
Results
Between 1996 and 2015, 1.850.811 deaths due to CBVD were recorded in Brazil, resulting in a mean of 92.540 cases/year. Of this total, 50.68% (n = 938.044) occurred in males and 77.80% (n = 1.440.170) in elderly people. The age group of 80 years or over was the only age group with a higher proportion of females than males. There was a high rate of low level of education: 39.94% (n = 739.233) were illiterate or had up to three years of schooling. In this variable, a high proportion of unknown fields was observed (38.29% / n = 708.685) (Table 1).
When analyzing the time series, the mortality rate due to CBVD in the Brazilian population, considering both genders, showed a linear trend of reduction (APC -2.4%; 95% CI -2.7 to -2.0; p = 0.001), from 72.3/100,000 (1996) to 46.4/100,000 (2015). Similar behaviors were observed in the male population (APC -2.3%; 95% CI -2.6 to -1.9; p = 0.001) and in the female population (APC -2.4%; 95% CI -2.8 to -2.0; p = 0.001), of which rates decreased from 77.8 and 71.4/100.000 to 51.1 and 45.2/100.000, respectively (Figure 1).
Spatial distribution and trend of mortality rates standardized by Cerebrovascular diseases (CBVD) in Brazilian states, all population and according to gender. Brazil, 1996-2015. APC: Annual Percent Change; hab.: inhabitant; nº: number; 95%CI: 95% Confidence Interval; CBVD: Cerebrovascular diseases.
Figure 1 shows that the spatial distribution of the mean rates is heterogeneous, being higher in the Southeast and South states and lower in the North states. The highest overall mean rates were observed in the states of Paraná (75/100,000) and Espírito Santo (71.3/100,000) and the lowest in the states of Rio Grande do Norte (40.9/100,000) and Bahia (48.0/100,000). The same scenario was observed for male mortality (Paraná with 83.4/100,000 and Espírito Santo with 79.8/100,000). In the female population, the highest rates were observed in Paraná (71.2/100,000) and Rio Grande do Sul (69.2/100,000) and the lowest in Rio Grande do Norte (40.7/100,000) and Bahia (49.1/100,000).
The trend in mortality rates was also analyzed considering the complete time series (1996-2015). The North region was the only one that showed a tendency towards an increase in mortality in the general population (APC 0.4%; 95% CI 0.1 to 0.8; p <0.001) and in the male population (APC 0.7%; 95% CI 0.3 to 1.1; p <0.001). The Midwest, Southeast and South regions showed a decreasing trend, both in the general population and in the male and female populations. The Southeast region showed the highest percentage of reduction in the time series (APC 3.8%) (Table 2).
In the stratified analysis by federation unit, 20 states showed significant trends, 7 showed increasing trends and 13 decreasing trends. All states in the Midwest, South and Southeast regions showed decreasing trends, with emphasis on Rio de Janeiro and Santa Catarina, with the highest reduction percentages. On the other hand, 5 of the 7 states with increasing trends are located in the northeast region (Maranhão, Piauí, Paraíba, Alagoas and Sergipe) and two in the north (Amazonas and Tocantins) (Table 2).
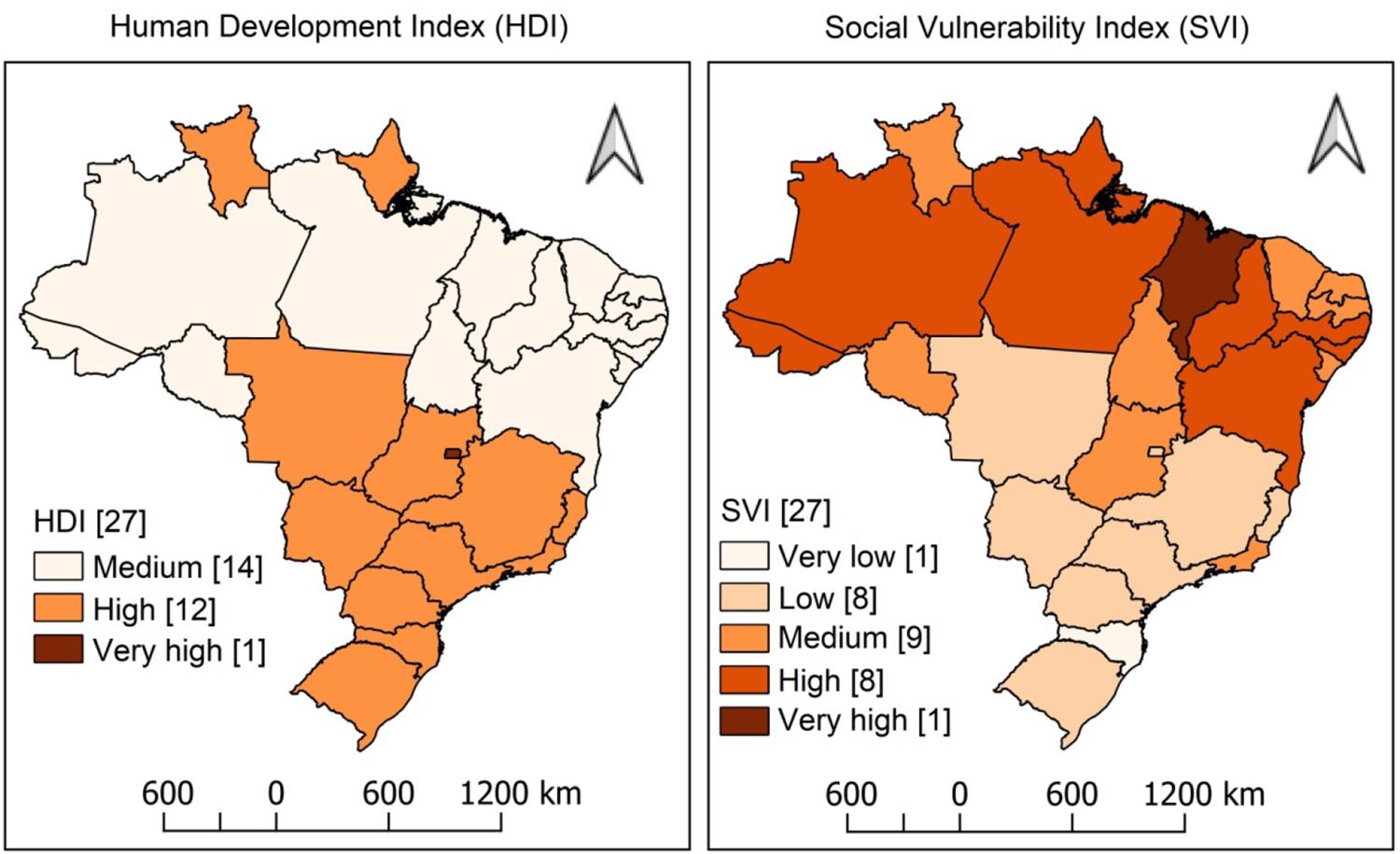
Only the Federal District was classified with very high HDI (HDI 0.824). All states in the Northeast and five in the North had medium HDI (between 0.600 and 0.699), with Alagoas and Maranhão standing out with the lower values (HDI 0.631 and 0.639, respectively). In parallel, these same states in the North and Northeast regions had the highest values in the SVI, especially Maranhão with very high SVI (SVI 0.521). All eight states classified as showing high social vulnerability are located in the North (n = 4) and Northeast (n = 4) regions (Figure 2).
– Spatial distribution of the Human Development Index (HDI) and the Social Vulnerability Index (SVI) in Brazilian states. Brazil, 2010.
The temporal regression model showed the states of the North and Northeast regions with the largest number of segments in the time series (joins), representing greater oscillation in rates over the years. The mortality rate in the Northeast showed four time segments: slight growth (1996-2003), stationary behavior (2003-2006), downward trend (2006-2010) and again a stationary behavior (2010-2015). Among the states in this region, only Bahia showed a linear behavior (Table 3).
Finally, the regression model showed a positive association between the mean mortality rate and the Municipal Human Development Index (p = 0.046), with the income dimension (p = 0.029), and a negative association with the general SVI (p = 0.026) and also in two dimensions: human capital (p = 0.046) and income and work (p = 0.018) (Table 4).
Discussion
Brazil has one of the highest mortality rates due to CBVD among the countries of Latin America and much higher than those observed in developed nations.1111. Lavados PM, Hennis AJ, Fernandes JG, Medina MT, Legetic B, Hoppe A, et al. Stroke epidemiology, prevention, and management strategies at a regional level: Latin America and the Caribbean. Lancet Neurol. 2007;6(4):362-72. However, a temporal decline behavior has been observed over the last decades,11. World Health Organization. (WHO). Health statistics and information systems. Estimates for 2000-2016. [Internet]. Genebra: WHO; 2018. [Acesso em 21 out 2018].Disponível em: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html.
http://www.who.int/healthinfo/global_bur...
in the male and female populations, corroborating the national and international literature.1212. Soares GP, Brum JD, Oliveira GM, Klein CH, Silva NAS. Mortalidade por todas as causas e por doenças cardiovasculares em três estados do Brasil, 1980 a 2006. Rev Panam Salud Publica. 2010;28(4):258-66.
13. Garritano CR, Luz PM, Pires MLE, Barbosa MTS, Batista KM. Analysis of the mortality trend due to cerebrovascular accident in Brazil in the XXI century. Arq Bras Cardiol. 2012;98(6):519-27.
14. Feigin VL, Abajobir AA, Abate KH, Adc-Allah F, Abdulle AM, Abera SF, et al. Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16(11):877-97.-1515. Cabral NL, Gonçalves ARR, Longo AL, Moro CHC, Costa G, Amaral CH, et al. Trends in stroke incidence, mortality and case fatality rates in Joinville, Brazil: 1995-2006. J Neurol Neurosurg Psychiatry. 2009;80:749-54.
Several authors have emphasized that such reduction in mortality can be explained by the expansion of access to health services and the adoption of prevention strategies.1414. Feigin VL, Abajobir AA, Abate KH, Adc-Allah F, Abdulle AM, Abera SF, et al. Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16(11):877-97.,1515. Cabral NL, Gonçalves ARR, Longo AL, Moro CHC, Costa G, Amaral CH, et al. Trends in stroke incidence, mortality and case fatality rates in Joinville, Brazil: 1995-2006. J Neurol Neurosurg Psychiatry. 2009;80:749-54. In Brazil, the implementation of primary health care (PHC) stands out. The Family Health Strategy (FHS) develops actions to control risk factors, such as encouraging physical activity and adopting healthy eating habits, smoking control programs, diagnosis and systematic monitoring of chronic conditions (hypertension and diabetes, for example) and access to pharmaceutical assistance.1616. Malta DC, Morais Neto OL, Silva Junior JB. Presentation of the strategic action plan for coping with chronic diseases in Brazil from 2011 to 2022. Epidemiol Serv Saúde. 2011;20(4):425-38.,1717. Pinto LF, Giovanella L. The Family Health Strategy: expanding access and reducing hospitalizations due to ambulatory care sensitive conditions (ACSC). Cienc Saúde Coletiva. 2018;23(6):1903-13. Between 1998 and 2017 there was a significant increase in the number of family health teams, going from approximately 2.000 to 41.000, reaching a coverage of 70% of the Brazilian population, which corresponds to approximately 143 million people.1717. Pinto LF, Giovanella L. The Family Health Strategy: expanding access and reducing hospitalizations due to ambulatory care sensitive conditions (ACSC). Cienc Saúde Coletiva. 2018;23(6):1903-13.,1818. Malta DC, Santos MAS, Stopa SR, Vieira JEB, Melo EA, Reis AAC. Family Health Strategy Coverage in Brazil,according to the National Health Survey, 2013. Cienc Saude Coletiva. 2016;21(2):327-38. Studies showed an association between the expansion of primary care and the reduction of mortality from diseases such as acute myocardial infarction and cerebrovascular diseases.1919. Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ. 2014;349:g4014.
In addition to PHC, Brazil has also advanced in the care of patients with CBVD. In 1997, the first stroke unit was implemented in Brazil, located in Joinville/SC. Based on this experience, in 2008, the Ministry of Health started the organization of the national stroke care network, resulting in Ordinance number 665/2012, with the purpose of implementing stroke referral services across the country.2020. Brasil. Ministério da Saúde do Brasil.. Portaria nº 665, de 12 de abril de 2012. [Acesso em 16 de set 2018]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2012/PRT0665_1 2_04_2012.html.
http://bvsms.saude.gov.br/bvs/saudelegis...
,2121. Brasil. Ministério da Saúde do Brasil. Acidente vascular cerebral. [Acesso em 19 de set 2018]. Disponível em: http://portalms.saude.gov.br/saude-de-a-z/acidente-vascular-cerebral-avc.
http://portalms.saude.gov.br/saude-de-a-...
Another important action is the Strategic Action Plan for Confronting Chronic Noncommunicable Diseases (NCDs). Implemented in 2011 by the Ministry of Health, the plan established a set of goals for the country, such as the reduction of premature mortality due to NCDs, the prevalence of smoking and alcohol consumption in the population, an increase in the prevalence of physical activity and fruit consumption and containment of obesity increase.2222. Brasil. Ministério da Saúde do Brasil (BR). Plano de Ações Estratégicas para o Enfrentamento das Doenças Crônicas Não Transmissíveis (DCNT) no Brasil 2011-2022. Brasília: Ministério da Saúde; 2011.
In the regional analysis, we found a heterogeneous behavior in the pattern of mortality from CBVD in the country, corroborating other studies.44. Lotufo PA, Goulart AC, Passos VMA, Satake FM, Souza MFM, França EB, et al. Cerebrovascular disease in Brazil from 1990 to 2015: Global Burden of Disease 2015. Rev Bras Epidemiol. 2017;20(1):129-41.,2323. Guimarães RM, Andrade SSCA, Machado EL, Bahia CA, Oliveira MM, Jacques FVL. Regional differences in cardiovascular mortality transition in Brazil, 1980 to 2012. Diferenças regionais na transição da mortalidade por doenças cardiovasculares no Brasil, 1980 a 2012. Rev Panam Salud Publica. 2015;37(2):83-89. Mortality rates were higher in the Southeast and South, but with a significant decreasing trend. In contrast, the North and Northeast regions had the lowest rates, but with a significant increasing trend over the historical series. This heterogeneous epidemiological-spatial context is the result of social, economic, demographic and epidemiological differences between the regions. Because of this, the results must be analyzed from the perspective of three dimensions: i) demographic and epidemiological transition; ii) social determinants of health and iii) quality of information systems.
Since the 1940s, Brazil has going through important demographic changes: a reduction in the overall mortality rate and a decline in birth rates have resulted in major changes in the demographic regime and in the age structure of the population, with a significant increase in the number of elderly individuals.2424. Alves JED. A transição demográfica e a janela de oportunidade. São Paulo: Instituto Fernand Braudel de Economia Mundial; 2008. In 2000, this population was just over 14.2 million, increasing to 19.6 million in 2010, and is expected to reach 41.5 million by 2030,2525. Instituto Brasileiro de Geografia e estatística. Estudos e análises – Informação Demográfica e Socioeconômica. Nº 3: Mudança Demográfica no Brasil no Início do Século XXI Subsídios para as projeções da população. Rio de Janeiro: IBGE; 2015. with a greater concentration in the Southeast and South regions. The impact of the population aging process on the pattern of morbidity and mortality is significant, since it implies an increase in chronic diseases,2626. Mendes ACG, Sá DA, Miranda GMD, Lyra TM, Tavares RAW.. The public healthcare system in the context of Brazil’s demographic transition: current and future demands. Cad Saúde Pública. 2012;28(5):955-64. among which CBVD stand out. In our study, 77.8% of deaths occurred among the elderly.
Studies indicate that the risk of mortality from CBVD in the elderly population is substantially higher than in other age groups. One reason is the accumulation of risk factors, such as hypertension, diabetes, dyslipidemia, alcoholism, smoking and inappropriate eating habits.2727. Pires SL, Gagliardi RJ, Gorzoni ML. Study of the main risk factors frequencies for ischemic cerebrovascular disease in elderly patients. Arq Neuropsiquiatr. 2004;62(3-B):844-51.,2828. Duncan BB, Chor D, Aquino EML, Bensenor IM, Mill JG, Scdmidt MI, et al. Chronic Non-Communicable Diseases in Brazil: priorities for disease management and research.. Rev Saúde Pública. 2012;46(Suppl.1):126-34. In Brazil, for example, the prevalence of hypertension can affect 68% of the elderly population.2929. Picon RV, Fuchs FD, Moreira LB, Fuchs SC. Prevalence of hypertension among elderly persons in urban Brazil: a systematic review with meta-analysis. Am J Hypertens. 2013;26(4):541-8.
Furthermore, the demographic transition process occurs concurrently with a second transition, the epidemiological one, characterized by changes in the population’s illness profile.3030. Vasconcelos AMN, Gomes MMF. Transição demográfica: a experiência brasileira. Epidemiol Serv Saúde. 2012;21(4):539-48. In the last decades, there has been a decline in infectious and parasitic diseases and an increase in the occurrence of chronic-degenerative diseases, many of which increase the risk of mortality from CBVD.2727. Pires SL, Gagliardi RJ, Gorzoni ML. Study of the main risk factors frequencies for ischemic cerebrovascular disease in elderly patients. Arq Neuropsiquiatr. 2004;62(3-B):844-51. The North and Northeast regions are the most exposed to social vulnerability and show the lowest human development index, resulting in higher mortality from diseases related to an unfavorable social context and less from CBVD. In contrast to what was observed in the most developed regions of the country (Southeast and South). In this sense, the higher rates observed in the more developed states reflect social differences, and, consequently, greater participation of chronic conditions in the mortality profile. On the other hand, more vulnerable regions may have lower rates due to the persistence of mortality due to diseases related to poverty.3232. Araújo JD. Epidemiological Polarization in Brazil. Epidemiol Serv Saúde. 2012;21(4):533-8.
The two transitions do not occur homogeneously in Brazil, with a mismatch between regions.3131. Schramm JMA, Oliveira AF, Leite IC, Valente JG, Gadelha AMJ, Portela MC, et al. Demographic transition: the Brazilian experience. Cienc Saude Coletiva. 2004;9(4):897-908. This phenomenon explains, in parts, the differences between Brazilian regions regarding CBVD mortality. This scenario justifies the positive association between CBVD mortality and human development and its negative association with social vulnerability, which represents the influence of the epidemiological and social context on the population’s mortality profile.
However, the isolated analysis of the rates is not enough to understand the epidemiological dynamics of CBVD. In the North and Northeast regions, in general, the rates showed a temporal pattern of growth and, in the Southeast and South regions, a decline was observed. These findings reflect the influence of social determinants of health on the pattern of mortality from CBVD. Socioeconomic conditions, including human development, income status and educational situation, have a significant influence on the risk of an individual dying from this group of diseases.44. Lotufo PA, Goulart AC, Passos VMA, Satake FM, Souza MFM, França EB, et al. Cerebrovascular disease in Brazil from 1990 to 2015: Global Burden of Disease 2015. Rev Bras Epidemiol. 2017;20(1):129-41.,66. Vincens N, Stafström M. Income inequality, economic growth and stroke mortality in Brazil: longitudinal and regional analysis 2002-2009. PLoS One. 2015;10(9):e0137332.,3333. Cabral NL, Longo A, Moro C, Ferst P, Oliveira FA, Vieira CV, et al.et al. Education level explains differences in stroke incidence among city districts in Joinville, Brazil: a three-year population-based study. Neuroepidemiology. 2011;36(4):258-64.
34. Bensenor IM, Goulart AC, Szwarcwald CL, Vieira MLFP, Malta DC, Lotufo PA. Prevalence of stroke and associated disability in Brazil: National Health Survey-2013. Arq Neuro-Psiquiatr. 2015;73(9):746-50.-3535. Lucena DMM, Figueiredo FWS, Sousa LVA, Paiva LS, Almeida TCC, Galego SJ, et al. Correlation between municipal human development index and stroke mortality: a study of Brazilian capitals. BMC Res Notes. 2018;11:540.
A recent study of the Global Burden of Disease showed that Brazilian states located at the lower tertile of the Social Development Index showed lower reductions in mortality rates, when compared to states located in the upper tertile of development. The lower tertile comprised only states in the North and Northeast regions.44. Lotufo PA, Goulart AC, Passos VMA, Satake FM, Souza MFM, França EB, et al. Cerebrovascular disease in Brazil from 1990 to 2015: Global Burden of Disease 2015. Rev Bras Epidemiol. 2017;20(1):129-41. It is suggested that better living conditions have a dual influence on the mortality trend: i) reduce risk factors for the occurrence of disease events; and ii) contribute to patient survival when such events occur, reducing the chance of death.
Finally, it is necessary to reflect on the quality of the mortality records. It is a challenge to adequately monitor the population’s health conditions. The inadequate filling out of the death certificates, resulting in a high number of garbage codes, the difficulties in carrying out epidemiological investigations with undefined recorded deaths and the lack of trained human resources to act in the death surveillance services are common problems evidenced throughout the country, although the North and Northeast regions are the most affected by the problem.3636. Brasil. Ministério da Saúde. Manual para investigação do óbito com causa mal definida. Brasília: Ministério da Saúde; 2009.,3737. IshitaniI LH, Teixeira RA, Abreu DMX, Paixão LMMM, França EB. Quality of mortality statistics’ information: garbage codes as causes of death in Belo Horizonte, 2011-2013. Rev Bras Epidemiol. 2017;20(1):34-45. The dubious quality of the information is an important limitation of this study.
Between 1996 and 2005, the percentage of deaths with undefined causes in these regions was higher than 20%, being even higher in the elderly population when compared to other age groups.3838. Jorge MHPM, Laurenti R, Lima-Costa MF, Gotlieb SLD, Chiavegatto Filho ADP. Brazilian mortality of elderly persons: the question about ill-defined underlying causes of death. Epidemiol Serv Saúde. 2008;17(4):271-81. In this sense, mortality rates in the North and Northeast, for example, may be higher than the ones we disclosed in this study. On the other hand, it is necessary to highlight that in recent years, important advances in the quality of information have been observed in these regions.1313. Garritano CR, Luz PM, Pires MLE, Barbosa MTS, Batista KM. Analysis of the mortality trend due to cerebrovascular accident in Brazil in the XXI century. Arq Bras Cardiol. 2012;98(6):519-27.
Conclusion
Mortality from CBVD in Brazil shows an irregular epidemiological behavior across the regions. The highest rates were observed in states with a better human development index and less social vulnerability, but with a decreasing trend over the time series. On the other hand, in less developed states and with greater vulnerability, the rates were lower, but with an upward trend. In this sense, we recommend that public policies should be developed considering the regional/local context.
Referências
-
1World Health Organization. (WHO). Health statistics and information systems. Estimates for 2000-2016. [Internet]. Genebra: WHO; 2018. [Acesso em 21 out 2018].Disponível em: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html
» http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html -
2Malta DC, França E, Abreu DMX, Perillo RD, Salmen MC, Teixeira RA, et al. Mortality due to noncommunicable diseases in Brazil, 1990 to 2015, according to estimates from the Global Burden of Disease study. São Paulo Med J. 2017;135(3):213-21.
-
3World Health Organization. The top 10 causes of death [Internet]. Genebra: WHO; 2018. [Acesso em 22 oute 2018]. Disponível em: http://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
» http://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death -
4Lotufo PA, Goulart AC, Passos VMA, Satake FM, Souza MFM, França EB, et al. Cerebrovascular disease in Brazil from 1990 to 2015: Global Burden of Disease 2015. Rev Bras Epidemiol. 2017;20(1):129-41.
-
5Alwan A, Maclean DR, Riley LM, d’Espaignet ET, Mathers CD, Stevens GA, et al. Monitoring and surveillance of chronic non-communicable diseases: progress and capacity in high-burden countries. Lancet. 2010;376(9755):1861-8.
-
6Vincens N, Stafström M. Income inequality, economic growth and stroke mortality in Brazil: longitudinal and regional analysis 2002-2009. PLoS One. 2015;10(9):e0137332.
-
7Brasil. Ministério da Saúde. Sistema de informações sobre mortalidade (SIM). [Acesso em 13 de agosto 2018]. Disponível em: http://datasus.saude.gov.br/
» http://datasus.saude.gov.br/ -
8Organização Mundial da Saúde. Classificação estatística internacional de doenças e problemas relacionados à saúde- CID 10. 10ª revisão. São Paulo: Centro Colaborador da Organização Mundial da saúde para a Classificação de Doenças em Português. Brasília, DF: OMS; 1995.
-
9Instituto Brasileiro de Geografia e Estatística. Sistema de Recuperação automática de dados- SIDRA. [Acesso em 15 de julho 2018]. Disponível em: https://sidra.ibge.gov.br/home /ipp/Brasil.
» https://sidra.ibge.gov.br/home -
10Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-51.
-
11Lavados PM, Hennis AJ, Fernandes JG, Medina MT, Legetic B, Hoppe A, et al. Stroke epidemiology, prevention, and management strategies at a regional level: Latin America and the Caribbean. Lancet Neurol. 2007;6(4):362-72.
-
12Soares GP, Brum JD, Oliveira GM, Klein CH, Silva NAS. Mortalidade por todas as causas e por doenças cardiovasculares em três estados do Brasil, 1980 a 2006. Rev Panam Salud Publica. 2010;28(4):258-66.
-
13Garritano CR, Luz PM, Pires MLE, Barbosa MTS, Batista KM. Analysis of the mortality trend due to cerebrovascular accident in Brazil in the XXI century. Arq Bras Cardiol. 2012;98(6):519-27.
-
14Feigin VL, Abajobir AA, Abate KH, Adc-Allah F, Abdulle AM, Abera SF, et al. Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16(11):877-97.
-
15Cabral NL, Gonçalves ARR, Longo AL, Moro CHC, Costa G, Amaral CH, et al. Trends in stroke incidence, mortality and case fatality rates in Joinville, Brazil: 1995-2006. J Neurol Neurosurg Psychiatry. 2009;80:749-54.
-
16Malta DC, Morais Neto OL, Silva Junior JB. Presentation of the strategic action plan for coping with chronic diseases in Brazil from 2011 to 2022. Epidemiol Serv Saúde. 2011;20(4):425-38.
-
17Pinto LF, Giovanella L. The Family Health Strategy: expanding access and reducing hospitalizations due to ambulatory care sensitive conditions (ACSC). Cienc Saúde Coletiva. 2018;23(6):1903-13.
-
18Malta DC, Santos MAS, Stopa SR, Vieira JEB, Melo EA, Reis AAC. Family Health Strategy Coverage in Brazil,according to the National Health Survey, 2013. Cienc Saude Coletiva. 2016;21(2):327-38.
-
19Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ. 2014;349:g4014.
-
20Brasil. Ministério da Saúde do Brasil.. Portaria nº 665, de 12 de abril de 2012. [Acesso em 16 de set 2018]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2012/PRT0665_1 2_04_2012.html
» http://bvsms.saude.gov.br/bvs/saudelegis/gm/2012/PRT0665_1 2_04_2012.html -
21Brasil. Ministério da Saúde do Brasil. Acidente vascular cerebral. [Acesso em 19 de set 2018]. Disponível em: http://portalms.saude.gov.br/saude-de-a-z/acidente-vascular-cerebral-avc
» http://portalms.saude.gov.br/saude-de-a-z/acidente-vascular-cerebral-avc -
22Brasil. Ministério da Saúde do Brasil (BR). Plano de Ações Estratégicas para o Enfrentamento das Doenças Crônicas Não Transmissíveis (DCNT) no Brasil 2011-2022. Brasília: Ministério da Saúde; 2011.
-
23Guimarães RM, Andrade SSCA, Machado EL, Bahia CA, Oliveira MM, Jacques FVL. Regional differences in cardiovascular mortality transition in Brazil, 1980 to 2012. Diferenças regionais na transição da mortalidade por doenças cardiovasculares no Brasil, 1980 a 2012. Rev Panam Salud Publica. 2015;37(2):83-89.
-
24Alves JED. A transição demográfica e a janela de oportunidade. São Paulo: Instituto Fernand Braudel de Economia Mundial; 2008.
-
25Instituto Brasileiro de Geografia e estatística. Estudos e análises – Informação Demográfica e Socioeconômica. Nº 3: Mudança Demográfica no Brasil no Início do Século XXI Subsídios para as projeções da população. Rio de Janeiro: IBGE; 2015.
-
26Mendes ACG, Sá DA, Miranda GMD, Lyra TM, Tavares RAW.. The public healthcare system in the context of Brazil’s demographic transition: current and future demands. Cad Saúde Pública. 2012;28(5):955-64.
-
27Pires SL, Gagliardi RJ, Gorzoni ML. Study of the main risk factors frequencies for ischemic cerebrovascular disease in elderly patients. Arq Neuropsiquiatr. 2004;62(3-B):844-51.
-
28Duncan BB, Chor D, Aquino EML, Bensenor IM, Mill JG, Scdmidt MI, et al. Chronic Non-Communicable Diseases in Brazil: priorities for disease management and research.. Rev Saúde Pública. 2012;46(Suppl.1):126-34.
-
29Picon RV, Fuchs FD, Moreira LB, Fuchs SC. Prevalence of hypertension among elderly persons in urban Brazil: a systematic review with meta-analysis. Am J Hypertens. 2013;26(4):541-8.
-
30Vasconcelos AMN, Gomes MMF. Transição demográfica: a experiência brasileira. Epidemiol Serv Saúde. 2012;21(4):539-48.
-
31Schramm JMA, Oliveira AF, Leite IC, Valente JG, Gadelha AMJ, Portela MC, et al. Demographic transition: the Brazilian experience. Cienc Saude Coletiva. 2004;9(4):897-908.
-
32Araújo JD. Epidemiological Polarization in Brazil. Epidemiol Serv Saúde. 2012;21(4):533-8.
-
33Cabral NL, Longo A, Moro C, Ferst P, Oliveira FA, Vieira CV, et al.et al. Education level explains differences in stroke incidence among city districts in Joinville, Brazil: a three-year population-based study. Neuroepidemiology. 2011;36(4):258-64.
-
34Bensenor IM, Goulart AC, Szwarcwald CL, Vieira MLFP, Malta DC, Lotufo PA. Prevalence of stroke and associated disability in Brazil: National Health Survey-2013. Arq Neuro-Psiquiatr. 2015;73(9):746-50.
-
35Lucena DMM, Figueiredo FWS, Sousa LVA, Paiva LS, Almeida TCC, Galego SJ, et al. Correlation between municipal human development index and stroke mortality: a study of Brazilian capitals. BMC Res Notes. 2018;11:540.
-
36Brasil. Ministério da Saúde. Manual para investigação do óbito com causa mal definida. Brasília: Ministério da Saúde; 2009.
-
37IshitaniI LH, Teixeira RA, Abreu DMX, Paixão LMMM, França EB. Quality of mortality statistics’ information: garbage codes as causes of death in Belo Horizonte, 2011-2013. Rev Bras Epidemiol. 2017;20(1):34-45.
-
38Jorge MHPM, Laurenti R, Lima-Costa MF, Gotlieb SLD, Chiavegatto Filho ADP. Brazilian mortality of elderly persons: the question about ill-defined underlying causes of death. Epidemiol Serv Saúde. 2008;17(4):271-81.
-
Study AssociationThis study is not associated with any thesis or dissertation work.
-
Sources of Funding.There were no external funding sources for this study.
Publication Dates
-
Publication in this collection
03 Feb 2021 -
Date of issue
Jan 2021
History
-
Received
08 Aug 2019 -
Reviewed
05 Nov 2020 -
Accepted
27 Dec 2019