Abstracts
OBJECTIVE: To characterize the conditions treated in the Mobile Medical Emergency Services (SAMU) in Porto Alegre, from January to June 2008. METHODS: A cross- sectional, descriptive and exploratory study was performed. Data from the information system of the SAMU were used, which were dowloaded into the Microsoft Excel program. Descriptive data analysis was performed. RESULTS: Neurologic, cardiovascular, respiratory, digestive and metabolic disorders were most prevalent; most of these occurred in the age group ranging between 41-60 years. Public hospitals and emergency care units were the main ports of entry for patients treated at SAMU. CONCLUSION: These results may contribute to better organization and point of service qualification requirements for the nursing staff that has substantial involvement in patient care.
Emergency medical services; Prehospital care; Health services
OBJETIVO: Caracterizar os agravos clínicos atendidos pelo Serviço de Atendimento Móvel de Urgência (SAMU), de Porto Alegre, no período de janeiro a junho de 2008. MÉTODOS: Estudo transversal, descritivo, exploratório. Utilizaram-se dados do sistema de informações do SAMU que foram transportados para o Programa Excel. O tratamento e análise dos dados foram descritivos. RESULTADOS: Os agravos neurológicos, cardiovasculares, respiratórios, digestivos e metabólicos foram os mais prevalentes, e a maioria ocorreu na faixa etária de 41-60 anos. Os hospitais públicos e unidades de pronto-atendimento foram as principais portas de entrada dos pacientes atendidos pelo SAMU. CONCLUSÃO: Os resultados podem contribuir para uma melhor organização do serviço e apontam necessidades de qualificação do atendimento de enfermagem que tem participação decisiva no cuidado ao paciente.
Serviços médicos de emergência; Assistência pré-hospitalar; Serviços de saúde
OBJETIVO: Caracterizar los agravios clínicos atendidos por el Servicio de Atención Móvil de Urgencia (SAMU), de Porto Alegre, en el período de enero a junio del 2008. MÉTODOS: Estudo transversal, descriptivo, exploratorio. Se utilizaron datos del sistema de informaciones del SAMU que fueron pasados al Programa Excel. El tratamiento y análisis de los datos fueron descriptivos. RESULTADOS: Los agravios neurológicos, cardiovasculares, respiratorios, digestivos y metabólicos fueron los más prevalentes, y la mayoría ocurrió en el grupo etáreo de 41-60 años. Los hospitales públicos y unidades de pronta-atención fueron las principales puertas de entrada de los pacientes atendidos por el SAMU. CONCLUSION: Los resultados pueden contribuir para una mejor organización del servicio y señalan necesidades de calificación de la atención de enfermería que tiene participación decisiva en el cuidado al paciente.
Servicios médicos de urgencia; Atención prehospitalaria; Servicios de salud
ORIGINAL ARTICLE
Conditions treated in the Mobile Medical Emergency Services in Porto Alegre - RS*
Agravios clínicos atendidos por el Servicio de Atención Móvil de Urgencia (SAMU) de Porto Alegre - RS
Giselda Quintana MarquesI; Maria Alice Dias da Silva LimaII; Rosane Mortari CiconetIII
IPh.D in Nursing. "Universidade Federal do Rio Grande do Sul" - UFGRS - Porto Alegre (RS), Brazil; Nurse of the "Secretaria Municipal da Saúde de Porto Alegre" - Porto Alegre (RS), Brazil
IIPh.D in Nursing. Associate Professor of the School of Nursing of the "Universidade Federal do Rio Grande do Sul" - UFRGS - Porto Alegre (RS), Brazil
IIIMaster in Nursing. "Universidade Federal do Rio Grande do Sul" - UFRGS - Porto Alegre (RS), Brazil; Nurse of the Mobile Emergency Care Service of the City of Porto Alegre Department of Health - Porto Alegre (RS), Brazil
Corresponding Author
ABSTRACT
OBJECTIVE: To characterize the conditions treated in the Mobile Medical Emergency Services (SAMU) in Porto Alegre, from January to June 2008.
METHODS: A cross- sectional, descriptive and exploratory study was performed. Data from the information system of the SAMU were used, which were dowloaded into the Microsoft Excel program. Descriptive data analysis was performed.
RESULTS: Neurologic, cardiovascular, respiratory, digestive and metabolic disorders were most prevalent; most of these occurred in the age group ranging between 41-60 years. Public hospitals and emergency care units were the main ports of entry for patients treated at SAMU.
CONCLUSION: These results may contribute to better organization and point of service qualification requirements for the nursing staff that has substantial involvement in patient care.
Keywords: Emergency medical services; Prehospital care; Health services
RESUMEN
OBJETIVO: Caracterizar los agravios clínicos atendidos por el Servicio de Atención Móvil de Urgencia (SAMU), de Porto Alegre, en el período de enero a junio del 2008.
MÉTODOS: Estudo transversal, descriptivo, exploratorio. Se utilizaron datos del sistema de informaciones del SAMU que fueron pasados al Programa Excel. El tratamiento y análisis de los datos fueron descriptivos.
RESULTADOS: Los agravios neurológicos, cardiovasculares, respiratorios, digestivos y metabólicos fueron los más prevalentes, y la mayoría ocurrió en el grupo etáreo de 41-60 años. Los hospitales públicos y unidades de pronta-atención fueron las principales puertas de entrada de los pacientes atendidos por el SAMU.
CONCLUSIÓN: Los resultados pueden contribuir para una mejor organización del servicio y señalan necesidades de calificación de la atención de enfermería que tiene participación decisiva en el cuidado al paciente.
Descriptores: Servicios médicos de urgencia; Atención prehospitalaria; Servicios de salud
INTRODUCTION
Users suffering from clinical health problems in situations that destabilize their vital condition require early and adequate intervention. This is one of the reasons to seek health services, among which are the mobile pre-hospital care services.
Emergency Pre-Hospital Care (PHC) can be defined as all types of care provided out of the context of a hospital, aiming to successfully meet the demands of individuals seeking the Sistema Único de Saúde (SUS - Unified Health System). The mobile PHC seeks to reach a victim as early as possible, making it necessary to provide them with adequate care and/or transportation to a health service hierarchically integrated with SUS(1).
In Brazil, demands made to the Serviços de Atendimento Móveis de Urgência - SAMU 192 (Mobile Emergency Care Services) have been focused on clinical health problems. This characteristic was identified in the following Brazilian cities: Ribeirão Preto, in the state of São Paulo, totaling 54.9% of all treatments(2); Olinda, in the state of Pernambuco, 57%(3); and Porto Alegre, in the state of Rio Grande do Sul, 64.8%(4). Data are in agreement with morbidity and mortality indicators and national risk factors(5), which show that clinical health problems are more prevalent and responsible for high disease and death indices.
SAMU actions are performed by basic and advanced life support teams, which guarantee pre-hospital health care, based on emergency medical regulations. Basic life support teams, comprised of drivers and nursing assistants/technicians, perform non-invasive support procedures, which involve the initial approach to the victim, basic ventilation and circulation care, immobilization and transportation to emergency services. Advanced life support teams, comprised of drivers, nurses and doctors, perform invasive procedures for ventilator and circulatory support and transport patients between hospitals, something known as medical transportation.
SAMU care consists of a series of responsibilities: telephone operators take emergency calls and trigger access to the health service; doctors see to the demands made by telephone and attempt to give the best response to each demand; nursing professionals help patients, based on distance prescriptions; vehicle drivers participate in health interventions, in addition to driving ambulances; and radio operators have a key role in subsequent transportation(6).
The relevance of nursing work when patient care is provided should be emphasized, because it is present in the services rendered, both in basic support units (BSU), where nursing assistants/technicians work, and in advanced support units (ASU), where nurses work.
In Brazil, the establishment of SAMUs is a recent strategy; thus, there are no official instruments that store information about services provided or establish a descriptive baseline of services in the entire country(3). Characterization of clinical health problems enables one to delve into questions that have been insufficiently dealt with in mobile pre-hospital performance in emergency care, once the majority of studies have focused on traumatic events, especially those related to traffic(4,7-8).
In this sense, the present study aimed to characterize clinical health problems treated in the SAMU of the city of Porto Alegre, between January and June 2008.
METHODS
An exploratory, descriptive, cross-sectional study was conducted in the SAMU of Porto Alegre. This public/city service provides health care in psychiatric, traumatic, obstetric and clinical emergency situations, in public roads, health services or homes, in addition to the transportation of patients requiring inter-health service transfers. The population of Porto Alegre is comprised of 1,360,590 inhabitants, corresponding to 13.4% of the total population in the state of Rio Grande do Sul(9).
Part of the SAMU structure is situated in the Hospital de Pronto Socorro (HPS), where the service management, emergency regulation center and mobile basic and advanced life support units are located. A total of 11 decentralized bases comprise its structure, spread around different areas of the city, where 12 BSU and three ASU are installed.
Secondary source data were used and collected from information system records of the SAMU emergency regulation center of Porto Alegre, referring to clinical demands that had been seen to between January and June 2008 and subsequently sent to Excel spreadsheets. The variables studied were: individual requesting service/origin of demand, type of health problem, age group and patient destination. Health problems classified as being of a clinical nature by the regulation doctor (RD) were selected for analysis. Non-inclusion of obstetric and psychiatric events was due to the specifications of this particular population and of the gateway to specialized services, which would justify the fact that such areas should be delved into.
Health problems of a clinical nature were grouped in the following order of frequency, according to the classification adopted by the regulation doctor, after a probable diagnosis was made: neurological, heart-related, respiratory, digestive, metabolic and infectious health problems, among others. Exogenous intoxications, although included in the group of health problems due to external causes, were classified as being of a clinical nature by the regulation doctor, thus being a part of the "other health problems" group in this study. The classification adopted by the SAMU was used to categorize data on age: children (less than 6 years); schoolchildren and pre-adolescents (7-14 years); adolescents (15-20 years); young adults (21-40 years); adults (41-60 years); elderly individuals (61-79 years); and individuals aged more than 80 years. With regard to patient destination, the following categories were used: patient is not transported to health services, public hospitals, SUS-affiliated hospitals, private hospitals, military hospitals and 24-hour emergency care units (ECU).
Data were treated and analyzed in a descriptive way, using absolute and percent numbers, and subsequently shown in tables.
The present study was conducted in accordance with the ethical principles of the Brazilian Ministry of Health's Resolution 196/96 on human research(10), guaranteeing patient anonymity with regards to the information collected. Institutional authorization was obtained to use SAMU's database and the Department of Health Ethics Committee of the city of Porto Alegre approved this research project (CEP 258/2008).
RESULTS
SAMU met a total of 14,787 demands, of which 13,715 (92.75%) originated from the population. The remaining 1,072 (7.24%) demands were met by health services, the Public Transportation Company and the Military Police. Of all these demands, 7,293 (49.32%) were classified as clinical health problems by the regulation doctor; 5,809 (39.28%), as traumatic events; 861 (5.82%), as simple transportation; 442 (2.98%), as psychiatric problems; 379 (2.56%), as obstetric problems; and three (0.02%) were not classified.
Neurological health problems, corresponding to 1,462 (20.04%) demands, were those most frequently treated by the team, followed by heart problems with 1,275 (17.42%) demands, and respiratory problems, 946 (12.97%). Among all the health problems treated, demands made due to convulsion were the most prevalent, totaling 804 (11.02%) cases, followed by syncope/fainting episodes, with 482 (6.60%) cases. The remaining health problems had percentages lower than 5%, as shown in Table 1.
A total of 1,172 (16.07%) demands did not include records of type of health problem in the information system of the medical regulation center.
The 41-to-60-year age group concentrated the majority of demands, 2,011 (27.54%); followed by the 61-to-79-year age group, with 1,784 (24.46%); and the 21-to-40-year age group, with 1,079 (14.80%).
Neurological health problems increase after the age of 21 years, with a higher concentration among those in the 41-to-60-year age group and a reduction after the age of 61 years, and convulsions had similar characteristics. Patients with a diagnosis of cerebrovascular accident (CVA) were concentrated after the age of 41 years and the 61-to-79-year age group showed the highest frequency of demands, which subsequently decreased in the "more than 80 years" age group.
Heart problems showed a higher concentration between the ages of 41 and 79 years, reaching a peak in the 41-to-60-year age group. Although including a lower number of demands when compared to the these first health problems, respiratory and metabolic problems were also concentrated between the ages of 41 and 79 years, with a peak of demands in the 61-to-79-year age group. Digestive problems were distributed among the age groups after the age of 21 years, with a higher concentration between the ages of 41 and 79 years, while infectious problems were concentrated in the 21-to-40-year age group.
Syncope/fainting episodes were distributed among all age groups, with increasing values until the age of 79 years. In-bed patients and those with sequelae had an increase after the age of 21 years, reaching a peak between the ages of 41 and 79 years.
The health problems most frequently treated among children aged 0-6 years and 7-14 years were respiratory problems, especially asthma, and neurological problems, especially convulsion. In the 15-to-21-year age group, neurological problems were observed, with an emphasis on convulsions and neuro/others, followed by respiratory problems, especially asthma and pneumonia. In this age group, the following were also present: syncope/fainting episodes, exogenous intoxication and abdominal pain.
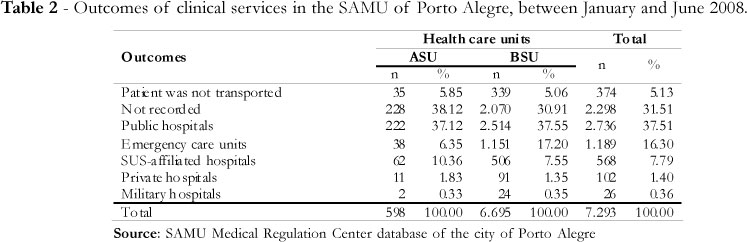
The BSU met 6,695 (91.80%) clinical demands, while the ASU met 598 (8.19%). The frequencies of outcomes of service provided to patients are shown in Table 2.
A total of 374 (5.13%) demands did not involve patients being transported to a health service. The percentages were similar, both in the ASU, with 35 (5.85%), and BSU, with 339 (5.06%). In these situations, the patient remained in the location of the event, because teams observed that there was an improvement or stabilization of their health condition, so that the emergency or death status could be disregarded.
A significant number of outcomes were not recorded in the information system of the medical regulation center, totaling 2,298 (31.51%) demands.
Public hospitals received 2,736 (37.51%) patients, of which 222 (37.12%) demands were met by the ASU and 2,514 (37.55%) by the BSU. The remaining SUS-affiliated hospitals, which received 568 (7.79%) patients; private hospitals, 102 (1.40%); and military hospitals, 26 (0.36%), participated with lower percentages, when compared to public hospitals.
The relevant participation of the ASU in receiving patients could be observed, totaling 1,189 (16.30%) demands, of which 38 (6.35%) were met by the ASU and 1,151 (17.20%) by the BSU.
Table 3 shows data on the following destinations of patients transported to health services by the SAMU. A total of 24 hospitals and four emergency units were the gateways used by SAMU patients.
Hospital A was the one most frequently used as gateway, receiving 1,301 (28.15%) patients, of which 73 (21.79%) were transported by the ASU and 1,228 (28.65%) by the BSU. The second most frequent gateway was hospital B, which received 942 (20.38%) patients, of which 91(27.16%) were transported by the ASU and 851(19.85%) by the BSU.
ECU 1 stands out as the one that received the majority of patients, with 600 (12.99%) demands, followed by ECU 2, with 285 (6.16%); ECU 3, with 165 (3.57%); and ECU 4, with 139 (3%). Hospitals C, D, E and F had percentages that were similar to those of the ECU, receiving 208 (4.5%), 172 (3.72%), 162 (3.5%), and 113 (2.44%) patients, respectively. The remaining ones showed irrelevant percentages of service.
DISCUSSION
The demands for service received by the SAMU were primarily made by the population, whereas health units and institutions included lower percentages. Studies identified users' preference for emergency services, instead of health professionals or units to which they have a connection(11-13). The phenomenon of spontaneous search for emergency services has been associated with the user's perception of signs and symptoms of health impairment. Based on the symptomatology, users follow symbolic mechanisms that lead them to the decision of what can be done to investigate or recover normality. They adjust the availability of services to their family and work context. From this point on, they structure their demands according to a health service. In this adjustment, the time factor appears as a determinant of decision-making, regulating the type of demand and service one will be provided(14).
In view of the fact that the number of demands met by SAMU is significant, it could be suggested that the population is aware of the fact that this service is one of the fastest and most efficient means of access to different technologies, whether one is provided health care or transported to a health service.
In the SAMU, the relevance of demands is defined by the regulation doctor. Situations that pose a risk to hemodynamic or ventilation conditions and/or cause functional impairment are considered to be an emergency, in addition to situations that require intervention by a health professional, due to the severity of symptoms, whether they are physical, social or psychological in nature. When it comes to critical situations, the regulator doctor triggers the best response, which can be a BSU or ASU being sent to the respective location.
Basic support teams are those that provide most of the care to SAMU users, which is in agreement with results of other studies(2,15). During the service, teams evaluate the patient and give this information to the regulation doctor, who prescribes the conduct and guides the service to which the patient must be sent to. During transportation, the team guarantees the conditions necessary for patient stabilization and provides admission to the emergency unit(6).
The results reveal that the number of demands for services provided to children and adolescents is lower, significantly increasing among those aged more than 21 years and being more concentrated in the 41-to-60-year age group. This indicates that an economically active population has been prematurely affected by health problems that require immediate care.
The percentage of heart problems in the population cared for by the SAMU is high, when compared to morbidity data of the city of Porto Alegre, where circulatory diseases correspond to 13.6%(5) of all diseases. With regard to respiratory problems, the percentage of services is approximately the same as that of local morbidity, 13.4%(5). If age groups per set of causes are compared in Porto Alegre(5), circulatory system diseases correspond to increasing percentages, from the age of 20 years on, with a steep increase after the age of 50 years. In the SAMU, the presence of such health problems increases from the age of 41 years on and it decreases among those aged more than 80 years.
The high number of neurological demands is mostly due to convulsions, present in all age groups, although especially in those aged more than 21 years. These findings corroborated those identified in the SAMU of Porto Alegre, when neurological problems corresponded to 39.02% of the services provided, followed by heart problems, 15.7%; and respiratory problems, 11.8%(16). The high number of services may be associated with the difficulty in accessing continuous primary care, the medication or low adherence to treatment.
Differently from the SAMU of Porto Alegre, gastrointestinal problems were those most frequently treated in the city of Ribeirão Preto(2). Local and regional characteristics in the profile of emergency care can indicate gaps in the availability of services in certain cities or regions, thus resulting in an increase in the number of demands for emergency services.
With regard to the participation of health services as users' gateway to SAMU, except for the lack of records of destinations of patients and those who had not been transported to health services, 47% of patients were sent to a hospital service and 16.3% to an ECU. Hospitals A and B stood out in terms of patients received, corresponding to 48.53% of all gateways. The remaining ones had lower individual participations.
The role of public emergency care units should be emphasized in the reception of patients. The numerical performance of the group formed by ECU 1 and ECU 2 was higher than that of the majority of hospitals, except for hospitals A, B, C, D and E.
Public services were the main gateways of clinical patients to the City Health System, thus indicating the SUS-funded system as the main gateway in emergency situations. SUS-affiliated hospitals had a proportionately lower participation, compared to public hospitals.
Private and military hospitals recorded an insignificant number of SAMU patient destinations. It is believed that this fact is particularly associated with inter-service transfers, where treatment could be continued, in addition to the referral of patients who had health plans, which could be regulated by private services.
With the advent of the SUS, the change of legislation enabled the public system participation in the funding of health care services and hospitalizations to significantly increase in all segments of the country, resulting in a decrease in direct private spending(17). Nonetheless, population access to health services is very unequal yet, whether because of the different forms of SUS funding or the restricted availability of services in the public system, which does not meet all health care demands. This causes access to also be determined by the population's socioeconomic condition.
As emergency care services frequently deal with an excessive number of patients, there are greater difficulties in receiving patients transported by SAMU. These considerations are associated with the role of regulation of emergencies, which are made operational by regulation centers. Emergency requirements are quick response pressure points and, as a result, centers must be capable of meeting the demands and directing patients to the most appropriate services for their care to continue. In addition, they contribute to the identification of lack of services and health care gaps and point to user needs, facilitating the construction of a more just, comprehensive and universal system.
The fact that only two hospitals are the main gateway of SAMU patients indicates difficulties in the regulation center's political competence, because the participation of institutions and services is very restricted yet.
CONCLUSIONS
Neurological, heart, respiratory, digestive and metabolic health problems were those most prevalent, the majority of which occurred in the 41-to-60-year age group. Public hospitals and emergency care units were the main gateways of patients treated by SAMU, thus revealing the differences in participation of health services.
The regulation of emergency service gateways sums up the entire effort of caring for patients requiring SAMU in the best way possible. In this way, the relationship with health services is a necessary condition to provide them with early and adequate care, in the shortest time interval possible.
The results of the present study can contribute to better service organization and point to the need of nursing care qualification, considering the fact that its participation is crucial to patient care. In the majority of situations, nursing professionals are the first ones to arrive at the location of event, they make the first decisions, provide care and maintain communication with the patient and their family, the regulation doctor and the health services used as gateway to emergencies. Thus, the responsibilities involved with the nursing team performance are increased according to mobile PHC. This is because, when dealing with the needs of users and in the relationship with services, these professionals can increase their understanding of such needs and contribute to better user care planning.
REFERENCES
-
1Brasil. Ministério da Saúde. Política Nacional de Atenção às Urgências. 2a ed. ampl. Brasília: Ministério da Saúde; 2006.
- 2. Fernandes RJ. Caracterização da atenção pré-hospitalar móvel da Secretaria de Saúde do município de Ribeirão Preto - SP [dissertação]. Ribeirão Preto (SP): Escola de Enfermagem de Ribeirão Preto da Universidade de São Paulo; 2004.
- 3. Cabral APS, Souza WV. Serviço de Atendimento Móvel de Urgência (SAMU): análise da demanda e sua distribuição espacial em uma cidade do Nordeste brasileiro. Rev Bras Epidemiol. 2008;11(4):530-40.
- 4. Pereira WAP, Lima MADS. Atendimento pré-hospitalar: caracterização das ocorrências de acidente de trânsito. Acta Paul Enferm. 2006;19(3):279-83.
- 5. Brasil. Ministério da Saúde. Secretaria Executiva. Indicadores de Mortalidade e de Morbidade. Brasília(DF) [internet] 2005 e 2006 [citado 2007 Jun 4]. Disponível em:http://www.datasus.gov.br/idb
- 6. Ciconet RM. Atuação e articulação das ações das equipes de suporte básico de um serviço de atendimento móvel de urgência com a central de regulação e as portas de entrada da urgência [dissertação]. Porto Alegre: Escola de Enfermagem da Universidade Federal do Rio Grande do Sul; 2009. 145f.
- 7. Bastos YGL, Andrade SM, Soares DA. Características dos acidentes de trânsito e das vítimas atendidas em serviço pré-hospitalar em cidade do Sul do Brasil, 1997/2000. Cad Saúde Pública = Rep Public Health. 2005;21(3):815-22.
- 8. Ladeira RM, Barreto SM. Fatores associados ao uso de serviço de atenção pré-hospitalar por vítimas de acidentes de trânsito. Cad Saúde Pública = Rep Public Health. 2008;24(2):287-94.
-
9Rio Grande do Sul. Secretaria do Planejamento e Gestão. Fundação de Economia e Estatística. População dos municípios do Rio Grande do Sul com mais de 100.000 habitantes e participação percentual no total da população do Estado - 1991 e 2000. Disponivel em:http://www.fee.tche.br/sitefee/pt/content/resumo/pg_estado_tabela.php?id=5 Acesso: 17/09/2010.
-
10Brasil. Ministério da Saúde. Conselho Nacional de Saúde. Resolução nº 196, de 10 de outubro de 1996. Dispõe sobre as diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Brasília: 10 out. 1996.
- 11. Oliveira LH, Mattos RA, Souza AIS. Cidadãos peregrinos: os "usuários" do SUS e os significados de sua demanda a pronto-socorros e hospitais no contexto de um processo de reorientação do modelo assistencial. Ciênc Saúde Coletiva. 2009;14(5):1929-38.
- 12. Marques GQ, Lima MADS. User's demands to an emergency service and their welcoming in the health system. Rev Latinoam Enferm. 2007;15(1):13-9.
- 13. Garlet ER, Lima MADS, Santos JLG, Marques GQ. Organização do trabalho de uma equipe de saúde no atendimento ao usuário em situações de urgência e emergência. Texto & Contexto Enferm. 2009;18(2):266-72.
- 14. Pasarín MI, Sanmamed MJF, Calafell J, Borrell C, Rodrígues D, Campasol S, et al. Razones para acudir a los servicios de urgencias hospitalarios. La población opina. Gac Sanit. 2006;20(2):91-100.
- 15. Cenci DC, Lucena AF. Análise dos atendimentos do Serviço de Atendimento Móvel de Urgência - SAMU 192 - de Porto Alegre / RS. In: Mancia JR, Unicowski MAR, organizadores. O trabalho de enfermagem em pronto socorro: um fazer em discussão. Porto Alegre: ABEn; 2010. p. 34- 59. UFRGS - Porto Alegre (RS), Brasil;
- 16. Pereira RF, Pinto RD, Ciconet RM. Caracterização dos atendimentos prestados pelo SAMU. Rev HPS.1999/2000; 45/46:6-9.
- 17. Porto SM, Santos IS, Ugá MAD. A utilização de serviços de saúde por sistema de financiamento. Ciênc Saúde Coletiva. 2006;11(4):895-910.
Publication Dates
-
Publication in this collection
14 Oct 2011 -
Date of issue
2011
History
-
Received
14 Aug 2009 -
Accepted
05 Nov 2010