Abstracts
White Piedra is a rare fungal infection of the hair shaft, caused by a yeast-like fungus (Trichosporon beigelii), characterized by yellow nodules on the pubic hair, moustache, beard and hair on the axillae and scalp. The objective was to register the presence of 15 cases of White Piedra in Espírito Santo diagnosed at the Dermatology Service in Vitória, over five years. All patients were female with nodules in the scalp hair, 13 were of mixed race and ten were between two and six years old. The hot and humid climate of the region together with the patients' habits regarding use of conditioning creams favored the infection. Moistening the hair with water can facilitate visualization of the nodules.
Mycoses; Piedra; Trichosporon
A piedra branca é infecção fúngica do pêlo, rara, causada pelo Trichosporon beigelii, caracterizada por nódulos amarelados nos pêlos genitais, bigode, barba, axilas e raramente, no couro cabeludo. O estudo registra 15 casos, diagnosticados em serviço de dermatologia de Vitória, durante cinco anos, todos de pacientes do sexo feminino, com nódulos nos pêlos do couro cabeludo. Os autores supõem que o clima quente e úmido da região e o hábito de as pacientes utilizarem cremes recondicionadores nos fios dos cabelos tenham favorecido a infecção. O umedecimento dos fios com água facilita a visualização dos nódulos.
Micoses; Piedra; Trichosporon
CASE REPORT
Study on 15 cases of white piedra in Grande Vitória (Espírito Santo - Brazil) over a five-year period* * Work done at School of Medicine, Santa Casa de Misericórdia de Vitória - Espírito Santo - EMESCAM.
Lucia Martins DinizI; João Basilio de Souza FilhoII
IAssistant Professor - Service of Post-graduation in Dermatology at Emescam and responsible for the Mycology Laboratory
IITitular Professor, Service of Post-graduation in Dermatology at Emescam
Correspondence Correspondence to Lucia Martins Diniz Rua Carlos Martins, 634 - Bairro Jardim Camburi Vitória ES CEP 29090-060 Tels.: (27) 3337-4236 / 3325- 0940 E-mail: diniz@tecnosite.com.br
ABSTRACT
White Piedra is a rare fungal infection of the hair shaft, caused by a yeast-like fungus (Trichosporon beigelii), characterized by yellow nodules on the pubic hair, moustache, beard and hair on the axillae and scalp. The objective was to register the presence of 15 cases of White Piedra in Espírito Santo diagnosed at the Dermatology Service in Vitória, over five years. All patients were female with nodules in the scalp hair, 13 were of mixed race and ten were between two and six years old. The hot and humid climate of the region together with the patients' habits regarding use of conditioning creams favored the infection. Moistening the hair with water can facilitate visualization of the nodules.
Keywords: Mycoses; Piedra; Trichosporon.
INTRODUCTION
White Piedra is a rare, chronic fungal infection of the hair cuticle, described originally by Beigel in 1865.1 The etiological agent is the yeast Trichosporon beigelii. Molecular studies have determined that there are six species of Trichosporon: T. ashii, T. asteroides, T. cutaneum(synonym of T. beigelii), T. mucoides, T. ovoides and T. inkin. The last two species are also involved in cases of white piedra, while the remaining species are responsible for pneumonitis, mucous infections, endocarditis, keratitis, hepatitis and peritonitis, etc.2-5
White piedra has a universal distribution, but with a predilection for temperate and tropical areas. In Brazil, its frequency is highest in the northern regions. It affects individuals of both sexes and any age group.1,4,6
Trichosporon beigelii inhabits soil, water and vegetation, but has also been found in monkeys and horses, making up part of the normal cutaneous flora (though mainly in the inguinocrural area) and the oral mucous membrane.1,4 However, the means of transmission remains unknown. It has been observed that white piedra is not related to a lack of hygiene nor to a lower socioeconomic level and it is not transmitted sexually.1,4,5
It is clinically characterized by the presence of soft, asymptomatic nodules, varying in color from white to light brown, with various shapes and sizes, and involving the hair shafts of the genital areas, armpits, beard and moustache. It affects the scalp less frequently, although it may involve the eyelashes and eyebrows.6-11 The hair follicle does not suffer alteration, but the underlying skin may be affected with erythematous, squamous lesions that are humid and pruriginous, and without distinct borders.9,10 In the genital area a synergism is observed between Trichosporon beigelii and the Coryneform, bacteria that are normal participants in the flora of that area.5,6 In immunodepressed patients T. beigelii may be disseminated, producing pustular, nodular, purpuric or necrotic cutaneous lesions.6
In making a differential diagnosis with black piedra, it can be noted that black piedra presents a harder nodule that adheres to the hair shaft, pediculosis, with axillary nodular trichomycosis and abnormalities of the hair stem, such as monilethrix, nodular trichorrhexis and trichoptilosis.5 When present in the genital region and affecting the underlying skin, the differential diagnosis is with dermatophytosis, candidiasis and erythrasma.9-11
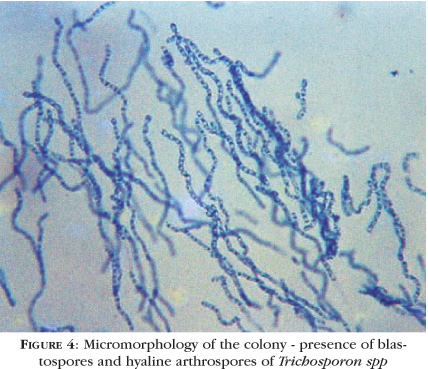
Laboratorial diagnosis is reached by analysis of the affected hairs under an optical microscope, using 20% potassium hydroxide in an aqueous solution of dimethyl sulfoxide. The diagnosis is positive when nodules are observed formed by mycelian elements (arthroconidia and blastoconidia, a binomial that characterizes the genus Trichosporon)9,10 arranged perpendicularly to the hair surface. After placing the affected hairs in Sabouraud's agar (without actidione) at room temperature, the moderate growth of a wrinkled, yellowish-white colony with a wax-like aspect may be observed. Later it acquires a grayish coloration. Micromorphology of the colony reveals hyaline hyphae, arthroconidia and blastoconidia.3,12 The genus Trichosporon does not ferment carbohydrates, but it assimilates glucose, galactose, sucrose, maltose, trehalose (probably) and lactose, and is urease-positive.3
The therapy of choice for white piedra is to cut the hair in the affected area, and, due to frequent recurrences, use of topical antifungals, such as imidazole, ciclopirox olamine, zinc pyrithione, etc.1,4,6
CASE REPORTS
A retrospective study was performed based on data obtained from medical records of patients that had undergone exams for fungal infections. The research was done at the laboratory of the Dermatology Service,
Santa Casa de Misericordia de Vitoria, Espirito Santo, Brazil, covering the period from January 1, 1998 until January 1, 2003. From the records with a clinical diagnosis of
white piedra the following were registered: name, age, sex, race, neighborhood and city of the patients' residence, location of the lesions and results of the direct mycological exams and culture for fungi.
Direct mycological exam of the patients' affected hairs was accomplished with the application of a drop of 20% potassium hydroxide in an aqueous solution of dimethyl sulfoxide on a microscope slide and covered by a cover slip. This was then observed under an optical microscope. For the macroscopic and microscopic evaluation of the colony, the affected hairs were cultivated on Sabouraud's agar (without actidione) and observed daily for 30 days
During the period selected for this study, 3,350 patients were seen for research of fungal infections at the laboratory. The patients were residents of various neighborhoods of greater Vitoria. The mean number of patients per year was 670. Of the total, only 15 (0.44%) presented a clinical diagnosis and laboratorial confirmation of white piedra, an average of three patients per year.
All 15 patients were female. Clinically they presented diminutive nodules, approximately one to two millimeters in diameter, yellowish-white in coloration, adhering to the shaft of scalp hair (Figure 1). These were asymptomatic and concentrated more in the frontoparietooccipital areas. There were no alterations in the hair follicle nor in the underlying skin. No other area of the body presented lesions. As for the patients' race, 13 (86.6%) were mixed and two (13.4%) were white. The age group most affected was the preschool phase, from two to six years of age (66.6%). Chart 1 shows the patients' distribution by age group.
Direct mycological exams of the strands of these 15 patients' hair revealed soft, yellowish-white nodules adhering to the hair shafts, though without altering them. The nodules were formed by fungal structures that were arthroconidial and blastoconidial disposed perpendicularly to the shafts, thus characterizing the genus Trichosporon spp (Figura 2).
The cultures in Sabouraud's agar of the 15 patients' affected hair revealed macroscopically the growth of a yeast-like colony, of a yellowish color, wrinkled, with a waxy appearance (Figure 3). For the micromorphology of the colonies, lactophenol cotton blue stain revealed septic hyphae, blastoconidia and arthroconidia, characteristic of the genus Trichosporon spp (Figure 4). Due to the lack of financial resources, molecular studies were not performed to determine the fungal species.
DISCUSSION
White piedra is a rare fungal infection, but with clinical cases reported in South America, North America, Southern Asia, The Middle East, Europe, Japan and Australia. In Brazil, there are reports of cases in Paraiba, Rio de Janeiro, São Paulo, Belem and, as of this study, in greater Vitoria (in the districts of Serra, Vitoria, Vila Velha, Cariacica and Viana). Most of the Brazilian cases of white piedra refer to location in the genital areas. Lesions in the scalp hair have been reported in Paraiba, São Paulo and Rio of Janeiro.5,9-11,13
During the five years of the study (1998 to 2002), white piedra represented only 0.44% of the patients submitted to testing of fungi in the laboratory of the Dermatology Service of Santa Casa de Misericordia de Vitoria, thus reflecting its sporadic occurrence in that population.
The patients came from various areas of greater Vitoria and had a varied socioeconomic profile ranging from low to middle class. The disease was unrelated to lack of personal hygiene. This corroborated the statistical data of the study done in Paraiba that found no evidence of a correlation between these factors and the disease.5
All the patients were female and had woolly hair, of medium to long length, which suggests the habit of using greater amounts of conditioning creams, causing retention of humidity in the hair strands. This could contribute to the infection and persistence of the fungi. Most of the patients (66.6%) were in the preschool phase, between two and six years of age, but those responsible for the children denied that there were similar cases in students from the same school.
There have been previous reports of treatments for pediculated scalp hairs, in which there was no regression of the lesions, thus requiring further dermatological consultations. These references also report ease of visualizing the nodules adhering to hair strands after they were moistened with running water, a fact verified by the authors during the patients' exam.
The skin of the scalp was not affected, nor were there other cases in the family. All the patients or those responsible for them denied having bathed in stagnant water or in rivers, which argues against the hypothesis of contamination in such places. The climate of the area of greater Vitoria is humid and hot for most of the year, which probably favors infection by Trichosporon spp.
During the five years included in this study, no patients with nodules of black piedra were observed, also, there were no publications reporting cases of this disease in the state of Espírito Santo.
The patients were instructed to cut their hair and to use shampoos based on 2% zinc pyrithione or 2% ketoconazole for 30 days. Regression of the lesions was observed at the end of that time, and none returned to the previous clinical picture, demonstrating a complete absence of recurrence. q
REFERENCES
Received on June 16, 2003.
Approved by the Consultive Council and accepted for publication on October 16, 2003.
- 1. Zaitz C, Campbell I, Marques AS, Luiz LRB, Souza VM. Compêndio de micologia médica. Rio de Janeiro: MEDSI; 1998. p.72-4.
- 2. Lacaz CS, Porto E, Martins JEC, Heins-Vaccari EM, Melo NT. Tratado de Micologia Médica Lacaz. 9Ş ed. São Paulo: Sarvier; 2002. p. 631-3.
- 3. Lacaz CS, Porto E, Heins Vaccari EM, Melo NT. Guia para identificação: Fungos, Actinomicetos, Algas de interesse médico. São Paulo: Sarvier; 1998. p.138-9.
- 4. Talhari S, Neves RN. Dermatologia Tropical. Rio de Janeiro: MEDSI; 1995. p.122-3.
- 5. Pontes ZBVS, Ramos AL, Lima EO, Guerra MFL, Oliveira NMC, Santos JP. Clinical and Mycological Study of Scalp White Piedra in the State of Paraíba, Brazil. Mem Ins Oswaldo Cruz. 2002; 97: 747-50.
- 6. Guidelines of care for superficial mycotic infections of the skin: Piedra. J Am Acad Dermatol. 1996; 34: 122-4.
- 7. Sodré CT. Ceratofitoses. An Bras Dermatol. 1989; 64: 97-9.
- 8. Juang JM, Marques ERMC, Couto LWM, Metelmann U, Silva EH. Piedra Branca no couro cabeludo. An Bras Dermatol. 2000; 75 : 25.
- 9. Carneiro JA, Assis FA, Trindade Filho J, Carvalho CAQ. Piedra branca genital 40 casos. An Bras Dermatol. 1971; 46: 265-9.
- 10. Carneiro JÁ, Alonso AM, Araújo FA. Novos Casos de piedra branca genital (PBG). An Bras Dermatol. 1973; 48: 133-6.
- 11. Gondim-Gonçalves H, Mapurunga ACP, Melo-Monteiro C, Lowy G, Lima AAB. Piedra Branca - revisão de literatura a respeito de três casos. Rev Bras Med. 1991; 48: 541- 7.
- 12. Lacaz CS, Porto E, Martins JEC. An Bras Dermatol. 1989; 64 (Supl.1): 55-91.
- 13. Brito AC, Costa CAA. "Piedra" em Belém do Pará. An Bras Dermatol. 1966; 41: 227-8.
Publication Dates
-
Publication in this collection
25 Nov 2005 -
Date of issue
Feb 2005
History
-
Accepted
16 Oct 2003 -
Received
16 June 2003