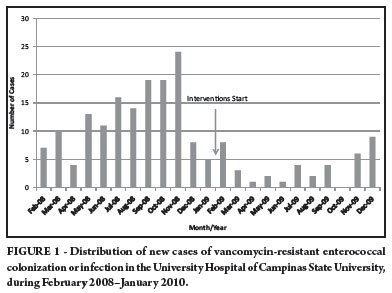
INTRODUCTION: Vancomycin-resistant enterococci (VRE) can colonize or cause infections in high-risk patients and contaminate the environment. Our objective was to describe theepidemiological investigation of an outbreak of VRE, the interventions made, and their impact on its control. METHODS: We conducted a retrospective, descriptive, non-comparative study by reviewing the charts of patients with a VRE-positive culture in the University Hospital of Campinas State University, comprising 380 beds, 40 of which were in intensive care units (ICUs), who were admitted from February 2008-January 2009. Interventions were divided into educational activity, reviewing the workflow processes, engineering measures, and administrative procedures. RESULTS: There were 150 patients, 139 (92.7%) colonized and 11 (7.3%) infected. Seventy-three percent were cared for in non-ICUs (p = 0.028). Infection was more frequent in patients with a central-line (p = 0.043), mechanical ventilation (p = 0.013), urinary catheter (p = 0.049), or surgical drain (p = 0.049). Vancomycin, metronidazole, ciprofloxacin, and third-generation cephalosporin were previously used by 47 (31.3%), 31 (20.7%), 24 (16%), and 24 (16%) patients, respectively. Death was more frequent in infected (73%) than in colonized (17%) patients (p < 0.001). After the interventions, the attack rate fell from 1.49 to 0.33 (p < 0.001). CONCLUSIONS: Classical risk factors for VRE colonization or infection, e.g., being cared for in an ICU and previous use of vancomycin, were not found in this study. The conjunction of an educational program, strict adhesion to contact precautions, and reinforcement of environmental cleaning were able to prevent the dissemination of VRE.
Enterococcus; Vancomycin resistance; Disease outbreaks; Epidemiology; Infection control