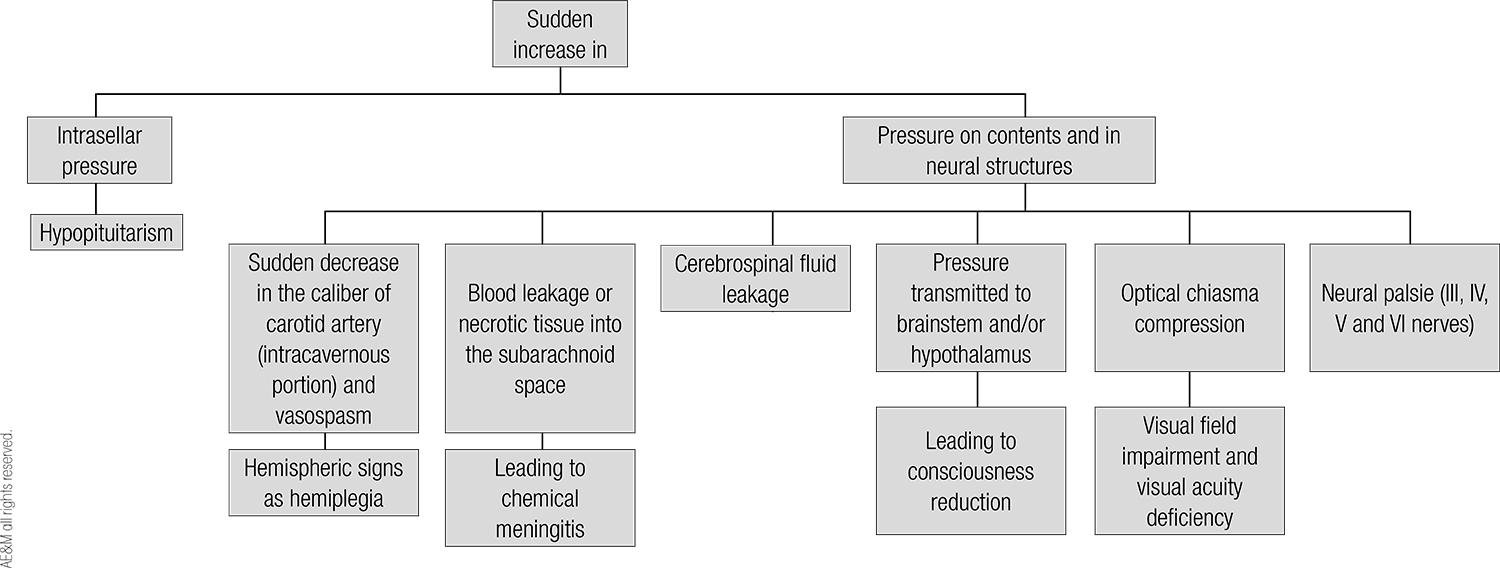
Pituitary apoplexy is characterized by sudden increase in pituitary gland volume secondary to ischemia and/or necrosis, usually in a pituitary adenoma. Most cases occur during the 5th decade of life, predominantly in males and in previously unknown clinically non-functioning pituitary adenomas. There are some predisposing factors as arterial hypertension, anticoagulant therapy and major surgery. Clinical picture comprises headache, visual impairment, cranial nerve palsies and hypopituitarism. Most cases improve with both surgical and expectant management and the best approach in the acute phase is still controversial. Surgery, usually by transsphenoidal route, is indicated if consciousness and/or vision are impaired, despite glucocorticoid replacement and electrolyte support. Pituitary function is impaired in most patients before apoplexy and ACTH deficiency is common, which makes glucocorticoid replacement needed in most cases. Pituitary deficiencies, once established, usually do not recover, regardless the treatment. Sellar imaging and endocrinological function must be periodic reevaluated. Arch Endocrinol Metab. 2015;59(3):259-64
Pituitary; apoplexy; pituitary adenoma; hypopituitarism