Abstract
OBJECTIVE:
We conducted a study to identify gender differences in factors associated with the first episode of non-adherence in the 12 months following the first antiretroviral prescription.
METHODS:
A concurrent prospective study of patients initiating antiretroviral therapy in Brazil was conducted from 2001-2002. The self-reported measurement of adherence was defined as an intake of less than 95% of the prescribed number of doses. Only the first occurrence of non-adherence was considered in this analysis. All analyses were stratified by gender. A Cox proportional hazard model was used to estimate the risk of non-adherence, and the time to non-adherence was estimated using the Kaplan-Meier method.
RESULTS:
The cumulative incidence of non-adherence was 34.6% (29.7% and 43.9% among men and women, respectively; p=0.010). Marital status (being married or in stable union; p=0.022), alcohol use in the month prior to the baseline interview (p=0.046), and current tobacco use (p=0.005) increased the risk of non-adherence among female participants only, whereas a self-reported difficulty with the antiretroviral treatment was associated with non-adherence in men only. For both men and women, we found that a longer time between the HIV test and first antiretroviral therapy prescription (p=0.028) also presented an increased risk of non-adherence.
CONCLUSIONS:
In this cohort study, the incidence of non-adherence was 1.5 times greater among women compared to men. Our results reinforce the need to develop interventions that account for gender differences in public referral centers. Additionally, we emphasize that, to achieve and maintain appropriate adherence levels, it is important to understand the barriers to seeking and utilizing health care services.
Antiretroviral Therapy; Adherence; Gender; Brazil
INTRODUCTION
A broad consensus in the literature supports the necessity of maintaining high rates of adherence
to antiretroviral therapy (ART) to achieve viral suppression (11. Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al.
Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med.
2000;133(1):21-30.); to prevent the emergence of resistant strains, disease progression and HIV transmission
(22. Fielden SJ, Rusch ML, Yip B, Wood E, Shannon K, Levy AR, et al. Nonadherence
increases the risk of hospitalization among HIV-infected antiretroviral naïve patients started on
HAART. J IntAssoc Physicians AIDS Care. 2008;7(5):238-44,
http://dx.doi.org/10.1177/1545109708323132.
http://dx.doi.org/10.1177/15451097083231...
-33. Kalichman SC, Cherry C, Amaral CM, Swetzes C, Eaton L, Macy R, et al. Adherence
to antiretroviral therapy and HIV transmission risks: implications for test-and-treat approaches to
HIV prevention. AIDS Patient Care STDS. 2010;24(5):271-7,
http://dx.doi.org/10.1089/apc.2009.0309.
http://dx.doi.org/10.1089/apc.2009.0309...
); and to improve
quality of life (44. Mannheimer SB, Matts J, Telzak E, Chesney M, Child C, Wu AW, et al. Quality of
life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS
Care. 2005;17(1):10-22, http://dx.doi.org/10.1080/09540120412331305098.
http://dx.doi.org/10.1080/09540120412331...
). Despite the necessity of high adherence
to ART, findings from a meta-analysis including 84 observational studies suggested that the mean
proportion of patients reporting an intake of ≥90% prescribed pills is 62% worldwide (55. Ortego C, Huedo-Medina TB, Llorca LS, Santos P, Rodríguez E, Warre MR, et al.
Adherence to Highly Active Antiretroviral Therapy (HAART): A Meta-Analysis. AIDS Behav.
2011;15(7):1381-96, http://dx.doi.org/10.1007/s10461-011-9942-x.
http://dx.doi.org/10.1007/s10461-011-994...
).
Although it is not completely clear which individual and/or structural factors are associated
with greater rates of adherence, evidence from the literature indicates that gender plays an
important role in determining differences in HIV therapeutics. For example, women seem to delay
initiation of ART more frequently (66. Mocroft A, Gill MJ, Davidson W, Phillips AN. Are There Gender Differences in
Starting Protease Inhibitors, HAART, and Disease Progression Despite Equal Access to Care? J Acquir
Immune Defic Syndr. 2000;24(5):475-82.), to have higher
incidence of treatment interruption (77. Moore DM, Zhang W, Genebat M, et al. Non-medically supervised treatment
interruptions among participants in a universally accessible antiretroviral therapy programme. HIV
Med. 2010;11(5):299-307, http://dx.doi.org/10.1111/j.1468-1293.2009.00779.x.
http://dx.doi.org/10.1111/j.1468-1293.20...
), to experience more
side effects (88. Currier JS, Spino C, Grimes J, Wosfy CB, Katzenstein DA, Hughes MD, et al.
Differences between women and men in adverse events and CD4+ responses to nucleoside analogue
therapy for HIV infection. J Acquir Immune DeficSyndr. 2000;24(4):316-24.), and to have more viral rebound after
initial suppression than men (99. Lima V, Harrigan R, Bangsberg DR, Hogg RS, Gross R, Yip B, Montaner JSG. The
combined effect of modern highly active antiretroviral therapy regimens and adherence on mortality
over time. J Acquir Immune DeficSyndr. 2009;50(5):529-36,
http://dx.doi.org/10.1097/QAI.0b013e31819675e9.
http://dx.doi.org/10.1097/QAI.0b013e3181...
); furthermore, women appear
to metabolize antiretroviral (ARV) drugs differently than men (1010. Mirjam-Colette K, Pisu M, Dumcheva A, Westfall AO, Kilby M, Saag MS. Gender
Differences in Discontinuation of Antiretroviral Treatment. J Acquir Immune DeficSyndr.
2009;52(3):336-41.).
There is also evidence that women living with HIV face different barriers to adherence than do
their male counterparts, including depression, stress, stigmatization, and specific social roles
related to gender. Furthermore, researchers suggest that, among females living with HIV, substance
abuse and alcohol use are predictive of poor adherence (1111. Berg KM, Demas AP, Howard AA, Schoenbaum EE, Gourevitc MN, Arnsten JH. Gender
differences in Factors Associated with Adherence to Antiretroviral Therapy. J Gen Intern Med.
2004;19(11):1111-7, http://dx.doi.org/10.1111/j.1525-1497.2004.30445.x.
http://dx.doi.org/10.1111/j.1525-1497.20...
-1212. Applebaum AJ, Richardson MA, Brady SM, Brief DJ, keane TM. Gender and Other
psychosocial factors as predictors of adherence to HAART in adults with comorbid HIV/aids,
psychiatric and substance related disorder. Aids Behav. 2009;13(1):60-5,
http://dx.doi.org/10.1007/s10461-008-9441-x.
http://dx.doi.org/10.1007/s10461-008-944...
). However, inconsistencies remain regarding the
association between gender and non-adherence. One possible explanation is that this relationship may
be confounded by unexamined social or behavioral factors. Furthermore, these associations have not
been extensively studied in developing countries (1313. Hawkins C, Chalamilla G, Okuma J, Spiegelman D, Hertzmark E, Aris E, et al. Sex
differencs in antiretroviral treatment outcomes among HIV-infected adults in an urban Tanzanian
setting. AIDS. 2011;25(9):1189-97, http://dx.doi.org/10.1097/QAD.0b013e3283471deb.
http://dx.doi.org/10.1097/QAD.0b013e3283...
).
We have previously reported data from a cohort study on adherence to ART (ATAR Project) in which
multivariate analyses indicated that unemployment, alcohol use, adverse reactions, number of pills,
changes in ART regimen, and a longer duration between the HIV test result and the first prescription
were predictors of non-adherence. Gender was associated with non-adherence in the univariate
analysis only (1414. Bonolo PF, César CC, Acúrcio FA, Ceccato MGB, Pádua CAM, Álvares J, et al.
Non-adherence among patients initiating antiretroviral therapy: A challenge for health professionals
in Brazil. AIDS. 2005;19Suppl 4:S5-13,
http://dx.doi.org/10.1097/01.aids.0000191484.84661.2b.
http://dx.doi.org/10.1097/01.aids.000019...
). However, an improved understanding of
gender differences in ART adherence may contribute to the development of more effective gender-based
interventions that can potentially reduce therapy failure during follow-up. Thus, the aim of this
study was to identify gender differences in factors associated with the first episode of
non-adherence in the 12 months following the first ARV prescription in AIDS public referral centers
in Brazil.
METHODS
This concurrent prospective analysis is part of the ATAR Project, a cohort study conducted during
2001-2002, for which the main objective was to determine the incidence and determinants of
non-adherence to ART among people living with HIV (PLHIV). Participants were adult (≥18 years old)
patients initiating treatment at two public AIDS referral centers in Belo Horizonte, Brazil, a large
urban area with approximately 2.5 million inhabitants (1414. Bonolo PF, César CC, Acúrcio FA, Ceccato MGB, Pádua CAM, Álvares J, et al.
Non-adherence among patients initiating antiretroviral therapy: A challenge for health professionals
in Brazil. AIDS. 2005;19Suppl 4:S5-13,
http://dx.doi.org/10.1097/01.aids.0000191484.84661.2b.
http://dx.doi.org/10.1097/01.aids.000019...
).
Participants were assessed immediately after receiving their first ARV drugs from the pharmacies at
each center (baseline interview) and in the first, fourth, and seventh months after initiating
therapy (follow-up visits). The maximum follow-up period was 12 months. This analysis aimed at
assessing the first episode of non-adherence among patients who returned for at least one follow-up
visit during the study period. Ethical approval and consent forms were obtained.
Baseline data included sociodemographic, clinical, and behavioral characteristics, whereas adherence to ART was evaluated at each follow-up visit. Additionally, quality of life and presence of anxiety and depression symptoms were assessed at baseline and at the second follow-up visit.
For the purposes of these analyses, the exposure variables have been grouped as follows: (i) sociodemographics (i.e., age, race, education, marital status, income, job schedule); (ii) behavioral factors (i.e., HIV status disclosure and alcohol, illicit drug, and tobacco use); (iii) health services-related variables (i.e., recruitment site, difficulty in searching for HIV service, use of more than one health service for HIV care, psychological support, and understanding of medical and pharmaceutical counseling related to ARV agents); and (iv) clinical and treatment-related factors (i.e., number of pills per day, self-reported difficulty of ART, clinical classification, TCD4+ lymphocyte count, adverse reactions, time between HIV test result or first medical visit to ARV prescription, self-perceived quality of life, and presence of anxiety and depression symptoms). The clinical and immunological data were extracted from medical charts, which were classified according to the Centers for Disease Control and Prevention definitions (1515. Centers for Disease Control and Prevention, 1993. Revised classification system for HIV infection and expanded surveillance case definitions for AIDS among adolescents and adults. MMWR Recomm Rep. 1992;41(RR-17):1-19.).
The patients' levels of comprehension of the ARV prescription were assessed using the following
six items: drug name, dosage, administration frequency, use precautions or situations demanding
special surveillance, side effects, and dietary guidance. Scores indicating the patients' levels of
comprehension of their ARV prescriptions were obtained using a latent trait model, estimated with
Item Response Theory (IRT) (1616. Zymowski MF, Muraki E, Misley RJ, Bock RD. BILOG-MG, multiple-grup IRT analysis
and test maintenance for binary items. Chicago: Scientific software, Inc.; 1996.), based on the concordance
between each patient's answer and the previously published written prescription (1717. Ceccato MGB, Acurcio FA, Cesar CC,Bonolo PF, Guimarães MDC. Compreensão da
terapia anti-retroviral: uma aplicação do modelo de traço latente. Cad.SaúdePública.
2008;24(7)1689-99, http://dx.doi.org/10.1590/S0102-311X2008000700023.
http://dx.doi.org/10.1590/S0102-311X2008...
). For this analysis, each score was categorized as sufficient or
insufficient, based on the median of participant scores. An understanding of medical or
pharmaceutical orientation was self-reported and categorized as follows: sufficient (high or
complete), insufficient (median, low or none), or did not receive orientation.
The duration between the initial HIV test and the first ARV prescription and the time between the
first medical visit and ARV prescription were categorized using the median points. Age was assessed
as a continuous variable. Adverse reactions were defined as any effects or undesirable symptoms
reported by the patients over the study period that were attributed to the ARV drug. Symptoms of
anxiety and depression were evaluated at baseline using the Hospital Anxiety and Depression Scale
(HADS) (1818. Zigmond AS, Snaith RP. The hospital anxiety and depression scale.
ActaPsychiatricaScandinavica. 1983;67(6):361-70.). Quality of life was evaluated using the brief
version of the World Health Organization Quality of Life instrument (WHOQOL-bref) (1919. Development of the World Health Organization WHOQOL-BREF quality of life
assessment. The WHOQOL Group. Psychol Med. 1998;28(3):551-8.). We used a global perception of quality of life that classified
the participants' quality of life into the following five categories: ‘very poor’, ‘poor’, ‘neither
poor nor good’, ‘good’, and ‘very good’. For the purposes of analysis, the data were dichotomized
into two categories, including those who classified their quality of life as ‘very poor’, ‘poor’,
and ‘neither poor nor good’, compared to those who reported a ‘good’ or ‘very good’ quality of life
(2020. Campos LN, Guimarães MDC, Remien RH. Anxiety and depression symptoms as risk
factors for non-adherence to antiretroviral therapy in Brazil. AIDS Behav. 2010;14(2):289-99,
http://dx.doi.org/10.1007/s10461-008-9435-8.
http://dx.doi.org/10.1007/s10461-008-943...
).
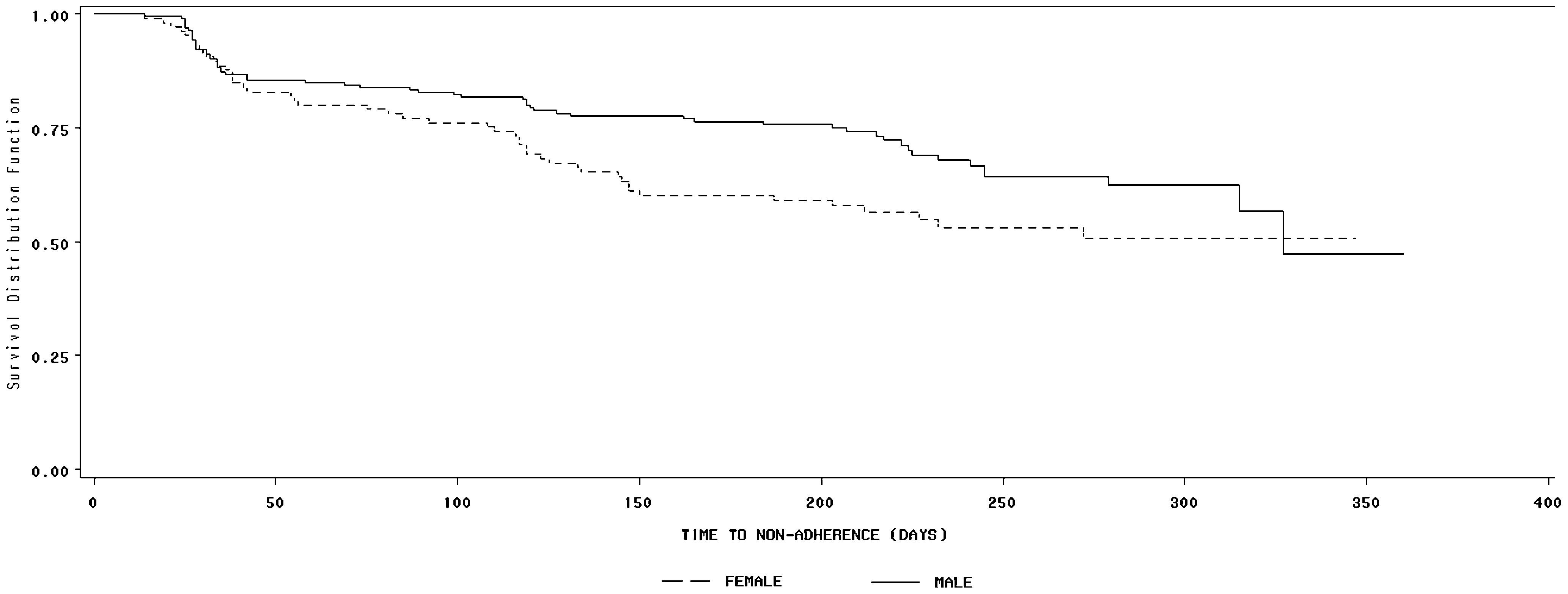
The self-reported measurement of adherence was defined as the number of prescribed doses of each ARV drug taken during the three days prior to each follow-up visit. Only the first occurrence of non-adherence was assessed, and it was defined as the intake of less than 95% of the prescribed number of doses. All analyses were stratified by gender, and the times to non-adherence were estimated using the Kaplan-Meier method and the Log-rank test.
The strength of association between selected exposure variables and the first episode of non-adherence was estimated by the relative hazard (RH) with 95% confidence interval, obtained from Cox's proportional hazard model for both univariate and multivariate gender-stratified analyses. Variables with p-values equal to or less than 0.20 were included in the final multivariate model with a subsequent sequential deletion. The level of significance required for inclusion in the final model was 0.05 to better ascertain potential confounders. A likelihood ratio test was used to compare all models, and the proportional hazard assumption was assessed by checking the parallelism of the log-log survival curves and the Schoenfeld test.
RESULTS
Among 306 participants, 199 (65.0%) were male, and 107 were female. Descriptive characteristics are presented in Table 1). Higher proportions of women reported only basic levels of schooling (41.1%) and unemployment (53.3%) compared to men (19.7% and 26.6%, respectively), whereas men reported a higher proportion of lifetime illicit drug use (38.0%) compared to women (9.0%). There were no marked differences between genders with regard to health service characteristics. However, clinical characteristics indicated that women exhibited a longer duration between the HIV test and the first ART prescription and between the first medical visit and the first ART prescription. Furthermore, women reported less positive self-perceived quality of life (49.5%) than men (62.7%) and higher baseline anxiety (47.0%) and depression symptoms (i.e., moderate-severe) (34.0%) compared to men (29.5% and 15.5%, respectively). The cumulative incidence of non-adherence was 34.6% (95% CI=29.5%-40.1%), including 29.7% (95% CI=23.6%-36.3%) among men and 43.9% (95% CI=34.8%-53.4%) among women (p=0.01). A significant difference in non-adherence survival Kaplan-Meier curves was identified between men and women (Log-Rank Test: p=0.038) (Figure 1). The median time to the first episode of non-adherence was a shorter duration for women (272 days) than men (327 days).
For men, univariate analyses (Table 2) indicated that non-adherence was associated (p<0.05) with the following factors: alcohol use in the month prior to the baseline interview, lifetime injection drug use, lifetime illicit drug use, self-reported difficulty with ART, baseline TCD4+ lymphocyte count <200/mm3, five or more adverse reactions reported, a longer duration between the HIV test and the first ART prescription, a longer time between the first medical visit and the first ART prescription, poorer self-perceived quality of life, and the presence of moderate/severe symptoms of anxiety or depression. For women, univariate analyses indicated associations (p<0.05) with alcohol use in the month prior to the baseline interview, current tobacco use, and lifetime illicit drug use.
The final multivariate model is shown in Table 3). The results indicated that self-reported difficulty of ART (p=0.002), five or more adverse reactions reported (p=0.007), and a longer duration between the HIV test and the first ART prescription (p=0.002) were independently associated with increased risk of non-adherence among male participants. In contrast, being married or in a stable union (p=0.022), alcohol use in the month prior to the baseline interview (p=0.046), current tobacco use (p=0.005), and a longer duration between the HIV test and the first ART prescription (p=0.028) were associated with increased risk of non-adherence among female participants.
Relative hazard with 95% confidence interval obtained from multivariate analysis of the first episode of ART non-adherence among 306 participants (199 men and 107 women), Belo Horizonte (MG), 2001-2002.
DISCUSSION
In this analysis, the high incidence of non-adherence was 1.5 times greater among women compared
to men. This finding is consistent with studies reporting poorer adherence among women that have
significant differences identified between genders (22. Fielden SJ, Rusch ML, Yip B, Wood E, Shannon K, Levy AR, et al. Nonadherence
increases the risk of hospitalization among HIV-infected antiretroviral naïve patients started on
HAART. J IntAssoc Physicians AIDS Care. 2008;7(5):238-44,
http://dx.doi.org/10.1177/1545109708323132.
http://dx.doi.org/10.1177/15451097083231...
,2121. Kyser M, Buchacz K, Bush TJ, Conley LJ, Hammer J, Henry K, et al. Factors
associated with nonadherence to antiretroviral therapy in the SUN study. AIDS Care.
2011;23(5):601-11, http://dx.doi.org/10.1080/09540121.2010.525603.
http://dx.doi.org/10.1080/09540121.2010....
-2222. Kuyper LM, Wood E, Montaner JSG, Yip B, O'Connell JM, Hogg RS. Gender
differences in HIV-1 RNA rebound attributed to incomplete antiretroviral adherence among
HIV-infected patients in a population- based cohort. J Acquir Immune DeficSyndr. 2004;37(4):1470-6,
http://dx.doi.org/10.1097/01.qai.0000138379.39317.62.
http://dx.doi.org/10.1097/01.qai.0000138...
). However, other
studies have failed to find a significant association between gender and ARV adherence (1111. Berg KM, Demas AP, Howard AA, Schoenbaum EE, Gourevitc MN, Arnsten JH. Gender
differences in Factors Associated with Adherence to Antiretroviral Therapy. J Gen Intern Med.
2004;19(11):1111-7, http://dx.doi.org/10.1111/j.1525-1497.2004.30445.x.
http://dx.doi.org/10.1111/j.1525-1497.20...
-1212. Applebaum AJ, Richardson MA, Brady SM, Brief DJ, keane TM. Gender and Other
psychosocial factors as predictors of adherence to HAART in adults with comorbid HIV/aids,
psychiatric and substance related disorder. Aids Behav. 2009;13(1):60-5,
http://dx.doi.org/10.1007/s10461-008-9441-x.
http://dx.doi.org/10.1007/s10461-008-944...
,2323. Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a
peer support intervention targeting antiretroviral medication adherence and depressive
symptomatology in HIV positive men and women. Health Psychol. 2007;22(6):488-95,
http://dx.doi.org/10.1037/0278-6133.26.4.488.
http://dx.doi.org/10.1037/0278-6133.26.4...
), and yet another study reported higher adherence rates among women (1313. Hawkins C, Chalamilla G, Okuma J, Spiegelman D, Hertzmark E, Aris E, et al. Sex
differencs in antiretroviral treatment outcomes among HIV-infected adults in an urban Tanzanian
setting. AIDS. 2011;25(9):1189-97, http://dx.doi.org/10.1097/QAD.0b013e3283471deb.
http://dx.doi.org/10.1097/QAD.0b013e3283...
). These discordant results may be due to methodological
distinctions, sample differences, or sociocultural divergence.
A literature review conducted on the adherence to ART in developed countries and spanning from
2000-2011 was conducted to determine whether the prevalence of non-adherence varied by gender (2424. Puskas CM, Forrest JI, Parashar S, Salters KA, Cescon AM, Kaida A, et al. Women
and vulnerability to HAART non-adherence: A literature review of treatment adherence by Gender from
2000 to 2011. Curr HIV/AIDS Rep. 2011;8(4)277-87,
http://dx.doi.org/10.1007/s11904-011-0098-0.
http://dx.doi.org/10.1007/s11904-011-009...
). The authors found that, when using higher cutoff points (100%
and 95%), women exhibited a lower mean proportional adherence than men across all measurements. In
contrast, lower cutoff points (90% and 80%) indicated that women reported a higher mean proportional
adherence across the majority of measurements. Although the authors concluded that these findings
suggested that female gender status often predicts lower adherence, they emphasized that differences
in methodology may account for these contradictory results.
Distinct gender differences were observed in our results. The only variable represented in the multivariate model for both men and women was the association of non-adherence with a longer duration between the HIV test result and the first ARV prescription. This delay in treatment initiation is concerning and can be the result of either the patient's difficulty in accepting the diagnosis and beginning treatment or a reduced perception of the necessity of treatment due to a lack of symptoms. The follow-up protocol for individuals living with HIV requires that they return to the health service for medical consultations every six months on average. Moreover, HIV referral services tend to be overloaded with patients, and priority is usually given to those with symptoms or more severe clinical conditions (2525. Arici C, Ripamonti D, Maggiolo F, Rizzi M, Finazzi MG, Pezzotti P, et al. Factors associated with the failure of HIV-positive persons to return for scheduled medical visits. HIV Clin Trials. 2002;3(1):52-7.).
However, people living with HIV who are asymptomatic tend to have less awareness of the disease and may not perceive the seriousness of the AIDS threat (2626. Duran S, Spire B, Raffi F, Walter V, Bouchour D, Journot V, et al. Self-reported symptoms after initiation of a protease inhibitor in HIV-infected patients and their impact on adherence to HAART. HIV Clin Trials.2001;2(1):38-45.). This perception potentially results in poor and delayed searches for care, despite the established capabilities and significant investments made by the Brazilian Health System to help diagnose, treat, and care for people living with HIV and AIDS. We emphasize the need to implement counseling and create alternative facilities for ambulatory care and treatment (2727. Gómez EJ. Pursuing Centralization amidst decentralization: the politics of Brasil's innovative response to HIV/AIDS. Journal of Politics in Latin America. 2011;3(3):95-126.).
Among men, self-reported difficulty with ART was a predictor of non-adherence. To acquire a behavior, such as adherence to ARV therapy, an individual needs to believe that benefits of the behavior compensate for the potential difficulties (2828. Guimarães MDC, Rocha GM, Campos LN, Freitas FMT, Gualberto FAZ, Teixeira RAR, et al. Difficulties reported by HIV-infected patients using antiretroviral therapy in Brazil. Clinics. 2008;63(2):165-72.).
Consistent with the literature, our results indicated that clinical factors such as adverse
reactions have been consistently associated with non-adherence (55. Ortego C, Huedo-Medina TB, Llorca LS, Santos P, Rodríguez E, Warre MR, et al.
Adherence to Highly Active Antiretroviral Therapy (HAART): A Meta-Analysis. AIDS Behav.
2011;15(7):1381-96, http://dx.doi.org/10.1007/s10461-011-9942-x.
http://dx.doi.org/10.1007/s10461-011-994...
). Adverse reactions are common with ARV therapy, especially among patients initiating
treatment (33. Kalichman SC, Cherry C, Amaral CM, Swetzes C, Eaton L, Macy R, et al. Adherence
to antiretroviral therapy and HIV transmission risks: implications for test-and-treat approaches to
HIV prevention. AIDS Patient Care STDS. 2010;24(5):271-7,
http://dx.doi.org/10.1089/apc.2009.0309.
http://dx.doi.org/10.1089/apc.2009.0309...
,1010. Mirjam-Colette K, Pisu M, Dumcheva A, Westfall AO, Kilby M, Saag MS. Gender
Differences in Discontinuation of Antiretroviral Treatment. J Acquir Immune DeficSyndr.
2009;52(3):336-41.
11. Berg KM, Demas AP, Howard AA, Schoenbaum EE, Gourevitc MN, Arnsten JH. Gender
differences in Factors Associated with Adherence to Antiretroviral Therapy. J Gen Intern Med.
2004;19(11):1111-7, http://dx.doi.org/10.1111/j.1525-1497.2004.30445.x.
http://dx.doi.org/10.1111/j.1525-1497.20...
-1212. Applebaum AJ, Richardson MA, Brady SM, Brief DJ, keane TM. Gender and Other
psychosocial factors as predictors of adherence to HAART in adults with comorbid HIV/aids,
psychiatric and substance related disorder. Aids Behav. 2009;13(1):60-5,
http://dx.doi.org/10.1007/s10461-008-9441-x.
http://dx.doi.org/10.1007/s10461-008-944...
,2222. Kuyper LM, Wood E, Montaner JSG, Yip B, O'Connell JM, Hogg RS. Gender
differences in HIV-1 RNA rebound attributed to incomplete antiretroviral adherence among
HIV-infected patients in a population- based cohort. J Acquir Immune DeficSyndr. 2004;37(4):1470-6,
http://dx.doi.org/10.1097/01.qai.0000138379.39317.62.
http://dx.doi.org/10.1097/01.qai.0000138...
,2929. Pádua CA, César CC, Bonolo PF, Acurcio FA, Guimarães MD. Self-reported adverse
reactions among patients initiating antiretroviral therapy in Brazil. Braz J Infect Dis.
2007;11(1):20-6.-3030. Floridia M, Giuliano M, Palmisano L, Vella S. Gender differences in the
treatment of HIV infection. Pharmacological Research. 2008;58(3-4):173-182,
http://dx.doi.org/10.1016/j.phrs.2008.07.007.
http://dx.doi.org/10.1016/j.phrs.2008.07...
).
Among female participants, we determined that marital status, including being married or in a
stable union, was associated with poor adherence. Potential explanations for this finding include
differences in health service attendance given the responsibility to manage one's home and children
(3030. Floridia M, Giuliano M, Palmisano L, Vella S. Gender differences in the
treatment of HIV infection. Pharmacological Research. 2008;58(3-4):173-182,
http://dx.doi.org/10.1016/j.phrs.2008.07.007.
http://dx.doi.org/10.1016/j.phrs.2008.07...
). Health professionals from HIV referral services must
understand and involve the family and nurture social relationships, with the aim of achieving and
maintaining high levels of adherence to ART for this particular population (3131. Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of
alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care
utilization. Drug Alcohol Depend. 2010;112(3):178-93,
http://dx.doi.org/10.1016/j.drugalcdep.2010.06.014.
http://dx.doi.org/10.1016/j.drugalcdep.2...
). In addition to biological differences, women with HIV often balance multiple
roles, have limited access to healthcare, report less household income, and express other concerns
that are not typically shared by HIV-positive men (3232. Vosv M, Martin LA, Smith NG, Jenkins SR. Gender Differences in HIV-Related
Coping and Depression. AIDS Behav. 2010;14(2):390-400.).
Finally, our results emphasized that the behavioral characteristics that can be modified after
the initiation of ART may be critical for the early adoption of adherent behavior. The analysis
indicated that, among women, alcohol use was significantly associated with non-adherence. These
findings are consistent with the literature (1111. Berg KM, Demas AP, Howard AA, Schoenbaum EE, Gourevitc MN, Arnsten JH. Gender
differences in Factors Associated with Adherence to Antiretroviral Therapy. J Gen Intern Med.
2004;19(11):1111-7, http://dx.doi.org/10.1111/j.1525-1497.2004.30445.x.
http://dx.doi.org/10.1111/j.1525-1497.20...
-1212. Applebaum AJ, Richardson MA, Brady SM, Brief DJ, keane TM. Gender and Other
psychosocial factors as predictors of adherence to HAART in adults with comorbid HIV/aids,
psychiatric and substance related disorder. Aids Behav. 2009;13(1):60-5,
http://dx.doi.org/10.1007/s10461-008-9441-x.
http://dx.doi.org/10.1007/s10461-008-944...
), thereby suggesting that alcohol use may disproportionately
impact ARV adherence in women. Furthermore, alcohol use is highly prevalent among individuals with
HIV/AIDS (2121. Kyser M, Buchacz K, Bush TJ, Conley LJ, Hammer J, Henry K, et al. Factors
associated with nonadherence to antiretroviral therapy in the SUN study. AIDS Care.
2011;23(5):601-11, http://dx.doi.org/10.1080/09540121.2010.525603.
http://dx.doi.org/10.1080/09540121.2010....
,3131. Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of
alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care
utilization. Drug Alcohol Depend. 2010;112(3):178-93,
http://dx.doi.org/10.1016/j.drugalcdep.2010.06.014.
http://dx.doi.org/10.1016/j.drugalcdep.2...
). A
systematic review of the literature indicated that, among individuals with HIV/AIDS, alcohol use
disorders are related to decreased ART adherence and to poorer HIV treatment outcomes (3131. Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of
alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care
utilization. Drug Alcohol Depend. 2010;112(3):178-93,
http://dx.doi.org/10.1016/j.drugalcdep.2010.06.014.
http://dx.doi.org/10.1016/j.drugalcdep.2...
). Other studies support the correlation with alcohol dependence
in women, which is thought to partially reflect the relative behavior frequency in relation to male
participants (1111. Berg KM, Demas AP, Howard AA, Schoenbaum EE, Gourevitc MN, Arnsten JH. Gender
differences in Factors Associated with Adherence to Antiretroviral Therapy. J Gen Intern Med.
2004;19(11):1111-7, http://dx.doi.org/10.1111/j.1525-1497.2004.30445.x.
http://dx.doi.org/10.1111/j.1525-1497.20...
-1212. Applebaum AJ, Richardson MA, Brady SM, Brief DJ, keane TM. Gender and Other
psychosocial factors as predictors of adherence to HAART in adults with comorbid HIV/aids,
psychiatric and substance related disorder. Aids Behav. 2009;13(1):60-5,
http://dx.doi.org/10.1007/s10461-008-9441-x.
http://dx.doi.org/10.1007/s10461-008-944...
).
A separate study conducted between 1999 and 2004 using two cohorts of women also indicated that
alcohol use (including binging and heavy and low consumption) reduced adherence (3333. Lazo M, Gange SJ, Wilson TE, Anastos K, Ostrow DG, Witt MD, et al. Patterns and
predictors of changes in adherence to highly active antiretroviral therapy: longitudinal study of
men and women. Clin Infect Dis. 2007;45(10):1377-85,
http://dx.doi.org/10.1086/522762.
http://dx.doi.org/10.1086/522762...
).
Our findings also indicated that tobacco use among women was associated with non-adherence. This
result is corroborated by the literature, which has highlighted that increased tobacco consumption
soon after initiation of ART was related with subsequent non-adherence (3434. Webb MS, Vanable PA, Carey MP, Blair DC. Medication adherence in HIV-infected
smokers: the mediating role of depressive symptoms. AIDS Educ Prev. 2009;21(3 Suppl):94-105,
http://dx.doi.org/10.1521/aeap.2009.21.3_supp.94.
http://dx.doi.org/10.1521/aeap.2009.21.3...
). Similarly, nicotine dependence appears to be related to non-adherence in the
context of other substance use behavior, and depression may, in part, mediate the relationship
between tobacco use and ART non-adherence (3434. Webb MS, Vanable PA, Carey MP, Blair DC. Medication adherence in HIV-infected
smokers: the mediating role of depressive symptoms. AIDS Educ Prev. 2009;21(3 Suppl):94-105,
http://dx.doi.org/10.1521/aeap.2009.21.3_supp.94.
http://dx.doi.org/10.1521/aeap.2009.21.3...
-3535. Tapp C, Milloy MJ, Zhang R, Guillemi S, Hogg RS, Montaner J, et al. Female
gender predicts lower access and adherence to antiretroviral therapy in a setting of free
healthcare. BMC Infections Diseases. 2011;11:86,
http://dx.doi.org/10.1186/1471-2334-11-86.
http://dx.doi.org/10.1186/1471-2334-11-8...
). Thus, in addition to other health implications due to tobacco
use, particularly in women, more interventional studies are needed to focus on smoking and
non-adherence.
In conclusion, this gender analysis indicated that social, behavioral, clinical, and health service characteristics associated with non-adherence at the beginning of ART are potentially different among women and men. Whereas among men, these factors directly related to the treatment per se, i.e., adverse reactions and self-reported difficulty, the non-adherence among women was more clearly explained by demographic (i.e., marital status) and behavioral characteristics (i.e., alcohol, tobacco use). We should also note that the time to reported non-adherence among women was significantly shorter than that of men, thereby emphasizing the need for immediate action as ART treatment begins. Early intervention strategies to improve adherence should focus on these differences and on an integrated assessment of clinical, counseling, social, and work support, while facilitating access to health services. However, despite the evidence we have presented, additional studies are required to better ascertain the gender differences in non-adherence so that effective measures can be incorporated into the care of individuals living with HIV who use public services in Brazil. Despite the evidence provided by this analysis, further studies are still needed to address these gaps in knowledge and to better conceptualize gender differences in factors associated with non-adherence in AIDS public referral centers, with the ultimate aim of improving care and reducing the barriers to strong treatment adherence.
This study is part of the ATAR Project (Adherence to Antiretrovirals) developed by the Research Group in Epidemiology and Health Evaluation, Faculty of Medicine, Federal University of Minas Gerais, Belo Horizonte, MG, Brazil. Sponsorship: This research received financial support from the Pan-American Health Organization (OPAS/WHO) and the Brazilian National AIDS/STD/Hepatitis Department, UNESCO, Ministry of Health.
REFERENCES
-
1Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21-30.
-
2Fielden SJ, Rusch ML, Yip B, Wood E, Shannon K, Levy AR, et al. Nonadherence increases the risk of hospitalization among HIV-infected antiretroviral naïve patients started on HAART. J IntAssoc Physicians AIDS Care. 2008;7(5):238-44, http://dx.doi.org/10.1177/1545109708323132.
» http://dx.doi.org/10.1177/1545109708323132 -
3Kalichman SC, Cherry C, Amaral CM, Swetzes C, Eaton L, Macy R, et al. Adherence to antiretroviral therapy and HIV transmission risks: implications for test-and-treat approaches to HIV prevention. AIDS Patient Care STDS. 2010;24(5):271-7, http://dx.doi.org/10.1089/apc.2009.0309.
» http://dx.doi.org/10.1089/apc.2009.0309 -
4Mannheimer SB, Matts J, Telzak E, Chesney M, Child C, Wu AW, et al. Quality of life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS Care. 2005;17(1):10-22, http://dx.doi.org/10.1080/09540120412331305098.
» http://dx.doi.org/10.1080/09540120412331305098 -
5Ortego C, Huedo-Medina TB, Llorca LS, Santos P, Rodríguez E, Warre MR, et al. Adherence to Highly Active Antiretroviral Therapy (HAART): A Meta-Analysis. AIDS Behav. 2011;15(7):1381-96, http://dx.doi.org/10.1007/s10461-011-9942-x.
» http://dx.doi.org/10.1007/s10461-011-9942-x -
6Mocroft A, Gill MJ, Davidson W, Phillips AN. Are There Gender Differences in Starting Protease Inhibitors, HAART, and Disease Progression Despite Equal Access to Care? J Acquir Immune Defic Syndr. 2000;24(5):475-82.
-
7Moore DM, Zhang W, Genebat M, et al. Non-medically supervised treatment interruptions among participants in a universally accessible antiretroviral therapy programme. HIV Med. 2010;11(5):299-307, http://dx.doi.org/10.1111/j.1468-1293.2009.00779.x.
» http://dx.doi.org/10.1111/j.1468-1293.2009.00779.x -
8Currier JS, Spino C, Grimes J, Wosfy CB, Katzenstein DA, Hughes MD, et al. Differences between women and men in adverse events and CD4+ responses to nucleoside analogue therapy for HIV infection. J Acquir Immune DeficSyndr. 2000;24(4):316-24.
-
9Lima V, Harrigan R, Bangsberg DR, Hogg RS, Gross R, Yip B, Montaner JSG. The combined effect of modern highly active antiretroviral therapy regimens and adherence on mortality over time. J Acquir Immune DeficSyndr. 2009;50(5):529-36, http://dx.doi.org/10.1097/QAI.0b013e31819675e9.
» http://dx.doi.org/10.1097/QAI.0b013e31819675e9 -
10Mirjam-Colette K, Pisu M, Dumcheva A, Westfall AO, Kilby M, Saag MS. Gender Differences in Discontinuation of Antiretroviral Treatment. J Acquir Immune DeficSyndr. 2009;52(3):336-41.
-
11Berg KM, Demas AP, Howard AA, Schoenbaum EE, Gourevitc MN, Arnsten JH. Gender differences in Factors Associated with Adherence to Antiretroviral Therapy. J Gen Intern Med. 2004;19(11):1111-7, http://dx.doi.org/10.1111/j.1525-1497.2004.30445.x.
» http://dx.doi.org/10.1111/j.1525-1497.2004.30445.x -
12Applebaum AJ, Richardson MA, Brady SM, Brief DJ, keane TM. Gender and Other psychosocial factors as predictors of adherence to HAART in adults with comorbid HIV/aids, psychiatric and substance related disorder. Aids Behav. 2009;13(1):60-5, http://dx.doi.org/10.1007/s10461-008-9441-x.
» http://dx.doi.org/10.1007/s10461-008-9441-x -
13Hawkins C, Chalamilla G, Okuma J, Spiegelman D, Hertzmark E, Aris E, et al. Sex differencs in antiretroviral treatment outcomes among HIV-infected adults in an urban Tanzanian setting. AIDS. 2011;25(9):1189-97, http://dx.doi.org/10.1097/QAD.0b013e3283471deb.
» http://dx.doi.org/10.1097/QAD.0b013e3283471deb -
14Bonolo PF, César CC, Acúrcio FA, Ceccato MGB, Pádua CAM, Álvares J, et al. Non-adherence among patients initiating antiretroviral therapy: A challenge for health professionals in Brazil. AIDS. 2005;19Suppl 4:S5-13, http://dx.doi.org/10.1097/01.aids.0000191484.84661.2b.
» http://dx.doi.org/10.1097/01.aids.0000191484.84661.2b -
15Centers for Disease Control and Prevention, 1993. Revised classification system for HIV infection and expanded surveillance case definitions for AIDS among adolescents and adults. MMWR Recomm Rep. 1992;41(RR-17):1-19.
-
16Zymowski MF, Muraki E, Misley RJ, Bock RD. BILOG-MG, multiple-grup IRT analysis and test maintenance for binary items. Chicago: Scientific software, Inc.; 1996.
-
17Ceccato MGB, Acurcio FA, Cesar CC,Bonolo PF, Guimarães MDC. Compreensão da terapia anti-retroviral: uma aplicação do modelo de traço latente. Cad.SaúdePública. 2008;24(7)1689-99, http://dx.doi.org/10.1590/S0102-311X2008000700023.
» http://dx.doi.org/10.1590/S0102-311X2008000700023 -
18Zigmond AS, Snaith RP. The hospital anxiety and depression scale. ActaPsychiatricaScandinavica. 1983;67(6):361-70.
-
19Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28(3):551-8.
-
20Campos LN, Guimarães MDC, Remien RH. Anxiety and depression symptoms as risk factors for non-adherence to antiretroviral therapy in Brazil. AIDS Behav. 2010;14(2):289-99, http://dx.doi.org/10.1007/s10461-008-9435-8.
» http://dx.doi.org/10.1007/s10461-008-9435-8 -
21Kyser M, Buchacz K, Bush TJ, Conley LJ, Hammer J, Henry K, et al. Factors associated with nonadherence to antiretroviral therapy in the SUN study. AIDS Care. 2011;23(5):601-11, http://dx.doi.org/10.1080/09540121.2010.525603.
» http://dx.doi.org/10.1080/09540121.2010.525603 -
22Kuyper LM, Wood E, Montaner JSG, Yip B, O'Connell JM, Hogg RS. Gender differences in HIV-1 RNA rebound attributed to incomplete antiretroviral adherence among HIV-infected patients in a population- based cohort. J Acquir Immune DeficSyndr. 2004;37(4):1470-6, http://dx.doi.org/10.1097/01.qai.0000138379.39317.62.
» http://dx.doi.org/10.1097/01.qai.0000138379.39317.62 -
23Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomatology in HIV positive men and women. Health Psychol. 2007;22(6):488-95, http://dx.doi.org/10.1037/0278-6133.26.4.488.
» http://dx.doi.org/10.1037/0278-6133.26.4.488 -
24Puskas CM, Forrest JI, Parashar S, Salters KA, Cescon AM, Kaida A, et al. Women and vulnerability to HAART non-adherence: A literature review of treatment adherence by Gender from 2000 to 2011. Curr HIV/AIDS Rep. 2011;8(4)277-87, http://dx.doi.org/10.1007/s11904-011-0098-0.
» http://dx.doi.org/10.1007/s11904-011-0098-0 -
25Arici C, Ripamonti D, Maggiolo F, Rizzi M, Finazzi MG, Pezzotti P, et al. Factors associated with the failure of HIV-positive persons to return for scheduled medical visits. HIV Clin Trials. 2002;3(1):52-7.
-
26Duran S, Spire B, Raffi F, Walter V, Bouchour D, Journot V, et al. Self-reported symptoms after initiation of a protease inhibitor in HIV-infected patients and their impact on adherence to HAART. HIV Clin Trials.2001;2(1):38-45.
-
27Gómez EJ. Pursuing Centralization amidst decentralization: the politics of Brasil's innovative response to HIV/AIDS. Journal of Politics in Latin America. 2011;3(3):95-126.
-
28Guimarães MDC, Rocha GM, Campos LN, Freitas FMT, Gualberto FAZ, Teixeira RAR, et al. Difficulties reported by HIV-infected patients using antiretroviral therapy in Brazil. Clinics. 2008;63(2):165-72.
-
29Pádua CA, César CC, Bonolo PF, Acurcio FA, Guimarães MD. Self-reported adverse reactions among patients initiating antiretroviral therapy in Brazil. Braz J Infect Dis. 2007;11(1):20-6.
-
30Floridia M, Giuliano M, Palmisano L, Vella S. Gender differences in the treatment of HIV infection. Pharmacological Research. 2008;58(3-4):173-182, http://dx.doi.org/10.1016/j.phrs.2008.07.007.
» http://dx.doi.org/10.1016/j.phrs.2008.07.007 -
31Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112(3):178-93, http://dx.doi.org/10.1016/j.drugalcdep.2010.06.014.
» http://dx.doi.org/10.1016/j.drugalcdep.2010.06.014 -
32Vosv M, Martin LA, Smith NG, Jenkins SR. Gender Differences in HIV-Related Coping and Depression. AIDS Behav. 2010;14(2):390-400.
-
33Lazo M, Gange SJ, Wilson TE, Anastos K, Ostrow DG, Witt MD, et al. Patterns and predictors of changes in adherence to highly active antiretroviral therapy: longitudinal study of men and women. Clin Infect Dis. 2007;45(10):1377-85, http://dx.doi.org/10.1086/522762.
» http://dx.doi.org/10.1086/522762 -
34Webb MS, Vanable PA, Carey MP, Blair DC. Medication adherence in HIV-infected smokers: the mediating role of depressive symptoms. AIDS Educ Prev. 2009;21(3 Suppl):94-105, http://dx.doi.org/10.1521/aeap.2009.21.3_supp.94.
» http://dx.doi.org/10.1521/aeap.2009.21.3_supp.94 -
35Tapp C, Milloy MJ, Zhang R, Guillemi S, Hogg RS, Montaner J, et al. Female gender predicts lower access and adherence to antiretroviral therapy in a setting of free healthcare. BMC Infections Diseases. 2011;11:86, http://dx.doi.org/10.1186/1471-2334-11-86.
» http://dx.doi.org/10.1186/1471-2334-11-86
-
No potential conflict of interest was reported.
Publication Dates
-
Publication in this collection
May 2013
History
-
Received
3 Sept 2012 -
Reviewed
19 Nov 2012 -
Accepted
3 Jan 2013