Abstracts
Hypoparathyroidism is a rare disorder that may be acquired or inherited. Postsurgical hypoparathyroidism is responsible for the majority of acquired hypoparathyroidism. Bone disease occurs in hypoparathyroidism due to markedly reduced bone remodeling due to the absence or low levels of parathyroid hormone. Chronically reduced bone turnover in patients with hypoparathyroidism typically leads to higher bone mass than in age- and sex-matched controls. Whether this increased bone density reduces fracture risk is less certain, because while increased bone mineralization may be associated with increased brittleness of bone, this does not appear to be the case in hypoparathyroidism. Treatment of hypoparathyroidism with recombinant parathyroid hormone may reduce bone mineral density but simultaneously strengthen the mechanical properties of bone.
Hypoparathyroidism; bone disease; bone mineral density; bone histomorphometry; fractures; skeleton
O hipoparatireoidismo é uma enfermidade rara que pode ser adquirida ou herdada. Dentre as causas adquiridas dessa doença, destaca-se como maior responsável o hipoparatireoidismo pós-cirúrgico. As manifestações ósseas dessa patologia decorrem devido a uma diminuição marcada no remodelamento ósseo causada pela diminuição ou ausência do hormônio da paratireoide. Esse remodelamento ósseo cronicamente reduzido leva a um aumento da massa óssea, evidenciado quando indivíduos com hipoparatireoidismo são comparados a controles de mesma idade e sexo. Entretanto, não se sabe se esse aumento de massa óssea reduz o risco de fratura. Apesar de o aumento da massa óssea estar associado a um aumento da fragilidade óssea em algumas situações, este não parece ser o caso no hipoparatireoidismo. O tratamento com hormônio recombinante da paratireoide pode reduzir a densidade mineral óssea ao mesmo tempo em que melhora as propriedades mecânicas do osso.
Hipoparatiroidismo; doença óssea; densidade mineral óssea; histomorfometria óssea; fraturas; esqueleto
INTRODUCTION
Hypoparathyroidism is a rare disorder characterized by the presence of decreased serum calcium and absent or inappropriately decreased serum parathyroid hormone (PTH). This condition is most often acquired, but may also be inherited (11 . Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391-403.). The acquired form is most often due to removal of, or damage to, the parathyroid glands or their blood supply at the time of neck surgery for thyroid disease, head and neck cancer, or parathyroid disease. Postsurgical hypoparathyroidism is responsible for about 75% of acquired cases (22 . Bilezikian JP, Khan A, Potts JT Jr, Brandi ML, Clarke BL, Shoback D, et al. Hypoparathyroidism in the adult: epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment, and challenges for future research. J Bone Miner Res. 2011;26(10):2317-37.). The next most common cause in adults is thought to be autoimmune disease, affecting either only the parathyroid glands, or the parathyroid glands in addition to multiple other endocrine organs. Remaining cases are due to a variety of rare infiltrative disorders, metastatic disease, iron or copper overload, ionizing radiation exposure, or rare genetic disorders.
This disorder is characterized by markedly reduced bone remodeling due to the absence or
markedly reduced presence of PTH (33 . Langdahl BL, Mortensen L, Vesterby A, Eriksen EF, Charles P. Bone
histomorphometry in hypoparathyroid patients treated with vitamin D. Bone.
1996;18(2):103-8.
4 . Kruse K, Kracht U, Wohlfart K, Kruse U. Biochemical markers of bone
turnover, intact serum parathyroid hormone and renal calcium excretion in patients with
pseudohypoparathyroidism and hypoparathyroidism before and during vitamin D treatment. Eur
J Pediatr. 1989;148(6):535-9.-55 . Mizunashi K, Furukawa Y, Miura R, Yumita S, Sohn HE, Yoshinaga K. Effects
of active vitamin D3 and parathyroid hormone on the serum osteocalcin in idiopathic
hypoparathyroidism and pseudohypoparathyroidism. J Clin Invest.
1988;82(3):861-5.). Chronically reduced bone turnover in patients with
hypoparathyroidism typically leads to increased bone mass compared to that in age- and
sex-matched controls (66 . Abugassa S, Nordenström J, Eriksson S, Sjödén G. Bone mineral density in
patients with chronic hypoparathyroidism. J Clin Endocrinol Metab.
1993;76(6):1617-21.
7 . Fujiyama K, Kiriyama T, Ito M, Nakata K, Yamashita S, Yokoyama N, et al.
Attenuation of postmenopausal high turnover bone loss in patients with hypoparathyroidism.
J Clin Endocrinol Metab. 1995;80(7):2135-8.
8 . Seeman E, Wahner HW, Offord KP, Kumar R, Johnson WJ, Riggs BL.
Differential effects of endocrine dysfunction on the axial and the appendicular skeleton.
J Clin Invest. 1982;69(6):1302-9.
9 . Touliatos JS, Sebes JI, Hinton A, McCommon D, Karas JG, Palmieri GM.
Hypoparathyroidism counteracts risk factors for osteoporosis. Am J Med Sci.
1995;310(2):56-60.
10 . Sikjaer T, Rejnmark L, Thomsen JS, Tietze A, Bruel A, Andersen G, et al.
Changes in 3-dimensional bone structure indices in hypoparathyroid patients treated with
PTH(1-84): a randomized controlled study. J Bone Miner Res.
2012;27(4):781-8.-1111 . Takamura Y, Miyauchi A, Yabuta T, Kihara M, Ito Y, Miya A. Attenuation of
postmenopausal bone loss in patients with transient hypoparathyroidism after total
thyroidectomy. World J Surg. 2013;37(12):2860-5.). Whether this increased bone density reduces fracture risk is less
certain, because increased bone mineralization may be associated with increased brittleness
of bone, although this does not appear to be the case in hypoparathyroidism. Treatment of
hypoparathyroidism with recombinant parathyroid hormone may reduce bone mineral density
(BMD) but concomitantly strengthen bone.
BONE MINERAL DENSITY
Bone mineral density is usually upper-normal or increased in patients with chronic hypoparathyroidism. One of the first studies that showed this used single photon absorptiometry to measure skeletal mass in the proximal femur, lumbar spine, and distal radius in 19 females with hypoparathyroidism after surgery for either thyroid carcinoma or hyperparathyroidism (66 . Abugassa S, Nordenström J, Eriksson S, Sjödén G. Bone mineral density in patients with chronic hypoparathyroidism. J Clin Endocrinol Metab. 1993;76(6):1617-21.). Healthy subjects, as well as normocalcemic patients who had undergone the same surgical procedure without developing hypoparathyroidism, were used as controls. Skeletal mass was measured after a mean postoperative interval of 13 years in patients operated on for thyroid carcinoma, and 10 years in patients operated on for hyperparathyroidism. Bone mass was 10-32% greater in hypoparathyroid patients than in controls. In patients who retained parathyroid function after total thyroidectomy or surgical treatment of hyperparathyroidism, bone mass did not differ from that in age-matched healthy controls. Long term L-thyroxine treatment using doses that suppressed endogenous TSH production was not associated with decreased bone mass in this study, although other studies have not found this (1212 . Sugitani I, Fujimoto Y. Effect of postoperative thyrotropin suppressive therapy on bone mineral density in patients with papillary thyroid carcinoma: a prospective controlled study. Surgery. 2011;150(6):1250-7.,1313 . Biondi B, Cooper DS. Benefits of thyrotropin suppression versus the risks of adverse effects in differentiated thyroid cancer. Thyroid. 2010;20(2):135-46.). Reduced PTH production, vitamin D treatment, and calcium supplementation were all thought to have contributed to the increased bone mass found in the patients with postsurgical hypoparathyroidism.
Greater insight into the architectural basis of the increase in bone mass in hypoparathyroidism has been obtained by using peripheral quantitative computed tomography (pQCT). Using this technique, Chen and cols. (1414 . Chen Q, Kaji H, Iu MF, Nomura R, Sowa H, Yamauchi M, et al. Effects of an excess and a deficiency of endogenous parathyroid hormone on volumetric bone mineral density and bone geometry determined by peripheral quantitative computed tomography in female subjects. J Clin Endocrinol Metab. 2003;88(10):4655-8.) compared volumetric bone mineral density (vBMD) and geometry of the distal radius and mid-radius among postmenopausal women with postoperative or idiopathic hypoparathyroidism, primary hyperparathyroidism, and normal control individuals. At the 4% distal radius site, which is enriched in cancellous bone, trabecular vBMD was higher in the patients with hypoparathyroidism, lower in controls, and lowest in patients with primary hyperparathyroidism. At the 20% mid-radius site, cortical vBMD also was greater in hypoparathyroidism, lower in controls, and lowest in primary hyperparathyroidism. The BMD differences among these three groups could be explained by differences in bone geometry. At both radial sites, total bone area and both periosteal and endosteal surfaces were greater in primary hyperparathyroidism than in patients with hypoparathyroidism or controls, and cortical thickness and area were higher in patients with hypoparathyroidism compared to controls and patients with primary hyperparathyroidism. Increased cancellous bone volume has been shown by high-resolution pQCT, and increased bone mechanical strength has been suggested by microfinite element analysis (1515 . Cohen A, Dempster DW, Müller R, Guo XE, Nickolas TL, Liu XS, et al. Assessment of trabecular and cortical architecture and mechanical competence of bone by high-resolution peripheral computed tomography: comparison with transiliac bone biopsy. Osteoporos Int. 2010;21(2):263-73.).
Hypoparathyroidism has been reported to attenuate high-turnover bone loss seen in postmenopausal women. Takamura and cols. (1111 . Takamura Y, Miyauchi A, Yabuta T, Kihara M, Ito Y, Miya A. Attenuation of postmenopausal bone loss in patients with transient hypoparathyroidism after total thyroidectomy. World J Surg. 2013;37(12):2860-5.) hypothesized that patients with transient hypoparathyroidism might have altered BMD. This study evaluated 140 women who had undergone total thyroidectomy with BMD measurements of the lumbar spine, femoral neck, and radius three years after surgery. At the time of surgery, 99 patients were ≥ 50 years old, and 41 were < 50 years old. Patients were divided into three groups according to their postoperative parathyroid function, with 80 patients having normal parathyroid function, 54 having transient hypoparathyroidism, and 6 having permanent hypoparathyroidism. Among the 99 patients aged ≥ 50 years, 36 transient hypoparathyroid patients had median BMD Z-scores at all three sites that were significantly higher, by 1.083 at the lumbar spine, 0.533 at the femoral neck, and 1.047 at the radius, compared to the same sites in the 60 patients with normal parathyroid function aged ≥ 50 years. BMD in the three permanent hypoparathyroid patients ≥ 50 years was higher than those in the normal and transient hypoparathyroid patients, but the differences did not reach statistical significance, except at the femoral neck. Multivariate logistic regression analyses showed that Z-scores > 0 were associated significantly only with transient postoperative hypoparathyroidism. In the patients < 50 years, BMD values were not significantly different among the three groups except at the radius in permanent hypoparathyroid patients, which was significantly lower than those of the other patients. This study concluded that transient postsurgical hypoparathyroidism was associated with increased BMD in postmenopausal women, possibly due to attenuation of high-turnover bone loss in this group.
BONE HISTOMORPHOMETRY
Although only two studies have evaluated bone histomorphometry in patients with hypoparathyroidism, the most comprehensive information on the effects of hypoparathyroidism on the skeleton has come from histomorphometric analysis of iliac crest bone biopsies.
In the first of these studies, Langdahl and cols. (33 . Langdahl BL, Mortensen L, Vesterby A, Eriksen EF, Charles P. Bone histomorphometry in hypoparathyroid patients treated with vitamin D. Bone. 1996;18(2):103-8.) obtained iliac crest bone biopsies from 4 men and 8 women with vitamin D-treated hypoparathyroidism and 13 age- and gender-matched control individuals. Nine of the subjects had postoperative hypoparathyroidism for 2 to 53 years duration, and 3 had idiopathic hypoparathyroidism for their entire lifetime. Ten of the patients were treated with 1-α-hydroxylated vitamin D (0.5 to 3.0 mcg/d), and two received calciferol oil (1600 to 3520 mcg/d). There was a nonsignificant trend toward an increase in cancellous bone volume in the hypoparathyroid subjects, but the structural indexes, marrow star volume, trabecular star volume, and trabecular thickness were not different from those in control individuals. Bone forming surface and bone-formation rate were reduced significantly by 58% and 80%, respectively, in the hypoparathyroid subjects, and remodeling activation frequency in the hypoparathyroid patients was reduced to 0.13 per year, compared with 0.6 per year in control individuals. Initial mineral apposition rate also was lower by a factor of 5 in the hypoparathyroid subjects, but this difference was not statistically significant. The total resorption period was prolonged from 26 to 80 days in the hypoparathyroid subjects, and the resorption depth was reduced. The reconstructed remodeling cycles derived from these data are shown in figure 1. The balance between the resorption depth and wall thickness of cancellous bone packets was slightly positive by approximately 5 mm in the hypoparathyroid subjects compared with the control individuals.
Reconstructed remodeling cycles in cancellous bone in hypoparathyroid (upper) and normal (lower) subjects. Note that all phases of the remodeling cycle are prolonged in hypoparathyroidism. Reproduced with permission from ref. 3.
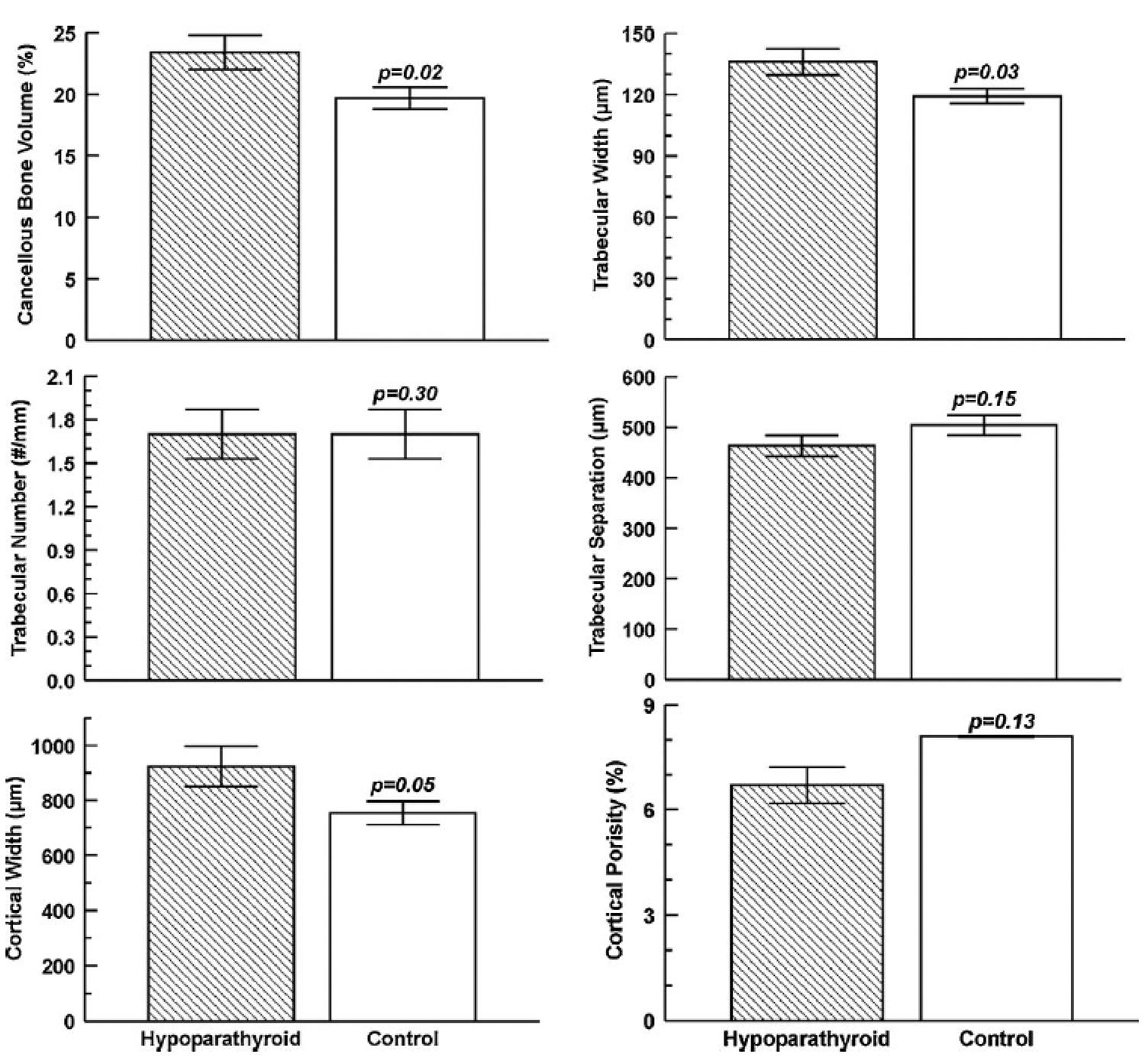
Rubin and cols. (1616 . Rubin MR, Dempster DW, Zhou H, Shane E, Nickolas T, Sliney J Jr, et al. Dynamic and structural properties of the skeleton in hypoparathyroidism. J Bone Miner Res. 2008;23(12):2018-24.) performed a more recent, larger histomorphometric study involving 24 women and 9 men with hypoparathyroidism treated with vitamin D and 33 age- and gender-matched control subjects. The etiologies of the hypoparathyroid state were post-thyroid surgery (n = 18), autoimmune (n = 13), and DiGeorge syndrome (n = 2), and the mean duration of their disease was 17 ± 13 (SD) years. Vitamin D intake varied between 400 and 100,000 IU/d, calcitriol intake between 0 and 3 mcg/day, and calcium supplementation between 0 and 9 g/d. Ten of the 33 hypoparathyroid subjects received thiazide diuretics. In contrast to the earlier smaller Langdahl study (33 . Langdahl BL, Mortensen L, Vesterby A, Eriksen EF, Charles P. Bone histomorphometry in hypoparathyroid patients treated with vitamin D. Bone. 1996;18(2):103-8.), cancellous bone volume was increased in the hypoparathyroid patients (Figures 2 and 3). The structural basis for the higher cancellous bone volume in hypoparathyroidism was increased trabecular width, with trabecular number and trabecular spacing both similar to those in control subjects. Cortical width also was significantly greater in the hypoparathyroid subjects, and cortical porosity was 17% lower than in control subjects, but this difference was not statistically significant. Remodeling activity was assessed separately on the cancellous, endocortical, and intracortical skeletal envelopes. Osteoid surface and width were reduced in the hypoparathyroid subjects on all three envelopes. Tetracycline-based bone formation rate was significantly lower on all three envelopes in the hypoparathyroid subjects, with the most profound reduction (more than five-fold) seen on the cancellous envelope (Figure 4). The reduction in bone formation rate was due to significant decreases in both mineralized surface and mineral apposition rate on all three envelopes. Eroded surface did not differ between the hypoparathyroid and normal subjects, but the bone resorption rate was significantly lower in the hypoparathyroid subjects on all three envelopes. As in the earlier Langdahl study (33 . Langdahl BL, Mortensen L, Vesterby A, Eriksen EF, Charles P. Bone histomorphometry in hypoparathyroid patients treated with vitamin D. Bone. 1996;18(2):103-8.), these findings are indicative of a profound reduction in the bone turnover rate in hypoparathyroidism, accompanied by an increase in bone mass in both cancellous and cortical compartments.
Low-magnification view of iliac crest bone biopsies obtained from a normal control subject (left) and a hypoparathyroid patient (right). Biopsies were stained with Goldner-Masson trichrome stain. Note that cancellous bone volume and cortical thickness are increased in the hypoparathyroid patient. Reproduced with permission from ref. 16.
Cancellous and cortical bone measurements obtained by bone histomorphometry in patients with hypoparathyroidism (hatched bars) and normal controls (open bars). Values are mean ± SD. Drawn from data from Rubin and cols. Reproduced with permission from ref. 2.
High-power magnification views of tetracycline labels in a hypoparathyroid patient (left) and normal control subject (right). Note that tetracycline labelling was markedly reduced in the patient with hypoparathyroidism, reflecting low bone turnover. Reproduced with permission from ref. 16.
The effects of PTH deficiency on cancellous and cortical bone mass, which were observed initially by noninvasive imaging and by 2D histomorphometry, were confirmed recently by the 3D analytical capability afforded by micro-computed tomography. Results from the study by Rubin and cols. (1717 . Rubin MR, Dempster DW, Kohler T, Stauber M, Zhou H, Shane E, et al. Three dimensional cancellous bone structure in hypoparathyroidism. Bone. 2010;46(1):190-5.) confirmed the increase in cancellous bone volume and trabecular thickness in hypoparathyroid subjects, and demonstrated higher trabecular number and trabecular connectivity in comparison with matched control subjects. In addition, the structural model index was lower in hypoparathyroidism, indicating that the trabecular structure was more platelike than rodlike (Figure 5).
Micro-CT images of cancellous bone from a patient with hypoparathyroidism (left) and a normal control subject (right). The cancellous bone in the patient with hypoparathyroidism appears heavier and denser. Reproduced with permission from ref. 17.
Christen and cols. (1818 . Christen P, Ito K, Müller R, Rubin MR, Dempster DW, Bilezikian JP, et al. Patient-specific bone modelling and remodelling simulation of hypoparathyroidism based on human iliac crest biopsies. J Biomech. 2012;45(14):2411-6.) reported on the material composition of the bone matrix in hypoparathyroidism. Using backscatter electron imaging, they found that the mean mineralization density in iliac bone from subjects with hypoparathyroidism was similar to that of control subjects, although there was greater interindividual variation in mineralization parameters in the hypoparathyroidism subjects than in the control subjects. This result was surprising because one might have expected that mineralization density would be enhanced in hypoparathyroidism owing to the low turnover and attendant increase in mineralization as the bone becomes more mature. These findings suggest that mineralization density is controlled by other factors, in addition to the degree of secondary mineralization, and indicates that the higher BMD by densitometry in hypoparathyroidism is due in large part to the increase in bone tissue volume rather than an increase in the amount of mineral within the tissue.
MARKERS OF BONE TURNOVER
Previous studies have shown that markers of bone turnover are lower in patients with hypoparathyroidism than in healthy age- and sex-matched controls. Markers of bone formation are decreased relative to those in healthy controls, and markers of bone resorption are similarly decreased. These findings generally confirm the bone histomorphometry findings reported in the preceding section, with specific results discussed in treatment trials discussed in the following section on response to treatment with PTH.
FRACTURES
The mechanism behind PTH activation of bone remodeling is intimately dependent on the time of exposure of bone cells to parathyroid hormone levels. Sustained high PTH levels trigger catabolism, while transitory elevations induce anabolism. Mendonça and cols. (1919 . Mendonça ML, Pereira FA, Nogueira-Barbosa MH, Monsignore LM, Teixeira SR, Watanabe PC, et al. Increased vertebral morphometric fracture in patients with postsurgical hypoparathyroidism despite normal bone mineral density. BMC Endocr Disord. 2013;13:1.) recently performed a small study assessing the impact of hypoparathyroidism on BMD, frequency of subclinical vertebral fracture, and mandible morphometry. This study evaluated 33 postmenopausal women, 16 of whom had hypoparathyroidism, and 17 of whom were healthy controls matched for age, weight and height. BMD of the lumbar spine, total hip, and 1/3 distal radius, radiographic evaluation of vertebral morphometry, panoramic radiography of the mandible, and biochemical evaluation of mineral metabolism and bone remodeling were assessed in both groups. There were no significant differences in lumbar spine or total hip BMD between the groups. There was marked heterogeneity of lumbar spine BMD in the hypoparathyroid patients, with increased BMD in four, normal BMD in nine, osteopenia in one, and osteoporosis in two patients. BMD was decreased in the 1/3 distal radius in the hypoparathyroid patients (P < 0.005). The hypoparathyroid group had increased morphometric vertebral fractures and decreased mandible cortical thickness. The study concluded that vertebral fragility fractures occurred in hypoparathyroid patients despite normal or increased BMD.
Underbjerg and cols. (2020 . Underbjerg L, Sikjaer T, Mosekilde L, Rejnmark L. Post-surgical hypoparathyroidism - risk of fractures, psychiatric diseases, cancer, cataract, and infections. J Bone Miner Res. 2014 May 7 [Epub ahead of print].) recently showed that post-surgical hypoparathyroidism was associated with decreased upper extremity fracture risk. The study evaluated data on fractures and other outcomes in patients with postsurgical hypoparathyroidism due to nonmalignant causes in the Danish National Patient Registry, with information confirmed by review of individual hospital records. Individual cases were matched with three age- (± 2 years) and gender-matched controls from the general background population. Compared to controls, patients did not have increased risk of any fracture, whereas risk of fracture of the upper extremities was significantly decreased. The authors concluded that postsurgical hypoparathyroidism is associated with protection against upper extremity fractures. Whether these findings apply to patients with hypoparathyroidism due to other causes is not yet clear. No other published studies to date have formally assessed fracture incidence in patients with hypoparathyroidism.
RESPONSE TO TREATMENT WITH PTH
Regardless of the cause of hypoparathyroidism, the effects of chronic PTH deficiency on the human skeleton are profound. In normal adults, bone mass is regulated by a delicate balance between bone resorption and formation in a tightly regulated process termed remodeling. PTH is one of the key regulators of the rate of bone remodeling. A reduction or absence of circulating PTH leads initially to a decrease in bone resorption and then to a coupled reduction in bone formation. However, the balance between resorption and formation favors the latter because, over time, bone mass increases in patients with hypoparathyroidism. This effect is seen in both cancellous and cortical bone compartments (66 . Abugassa S, Nordenström J, Eriksson S, Sjödén G. Bone mineral density in patients with chronic hypoparathyroidism. J Clin Endocrinol Metab. 1993;76(6):1617-21.,77 . Fujiyama K, Kiriyama T, Ito M, Nakata K, Yamashita S, Yokoyama N, et al. Attenuation of postmenopausal high turnover bone loss in patients with hypoparathyroidism. J Clin Endocrinol Metab. 1995;80(7):2135-8.,1414 . Chen Q, Kaji H, Iu MF, Nomura R, Sowa H, Yamauchi M, et al. Effects of an excess and a deficiency of endogenous parathyroid hormone on volumetric bone mineral density and bone geometry determined by peripheral quantitative computed tomography in female subjects. J Clin Endocrinol Metab. 2003;88(10):4655-8.,1616 . Rubin MR, Dempster DW, Zhou H, Shane E, Nickolas T, Sliney J Jr, et al. Dynamic and structural properties of the skeleton in hypoparathyroidism. J Bone Miner Res. 2008;23(12):2018-24.,2121 . Duan Y, De Luca V, Seeman E. Parathyroid hormone deficiency and excess: similar effects on trabecular bone but differing effects on cortical bone. J Clin Endocrinol Metab. 1999;84(2):718-22.).
To assess effects of PTH therapy on 3-dimensional bone structure, Sikjaer and cols. (2222 . Sikjaer T, Rejnmark L, Thomsen JS, Tietze A, Brüel A, Andersen G, et al. Changes in 3-dimensional bone structure indices in hypoparathyroid patients treated with PTH(1-84): a randomized controlled study. J Bone Miner Res. 2012;27(4):781-8.) randomized 62 patients with hypoparathyroidism to 24 weeks of treatment with either PTH(11 . Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391-403.-84) 100 µg/day subcutaneously or similar placebo as add-on therapy to calcium and vitamin D supplementation. Microcomputed tomography was performed on 44 iliac crest bone biopsies, with 23 biopsies taken from patients on PTH treatment, obtained after 24 weeks of treatment. Compared with placebo, PTH treatment caused a 27% lower trabecular thickness (p < 0.01) and 4% lower trabecular bone tissue density (p < 0.01), whereas connectivity density was 34% higher (p < 0.05). Trabecular tunneling was evident in 11 (48%) of the biopsies from the PTH treatment group. Patients with tunneling had significantly higher levels of biochemical markers of bone resorption and formation. In cortical bone, the number of Haversian canals per area was 139% higher (p = 0.01) in the PTH treatment group, causing a trend toward increased cortical porosity (p = 0.09). At different subregions of the hip, areal BMD (aBMD) and volumetric BMD (vBMD), as assessed by dual-energy X-ray absorptiometry (DXA) and quantitative computed tomography (QCT), decreased significantly by 1% to 4% in the PTH treatment group. However, at the lumbar spine, aBMD decreased by 1.8% (p < 0.05), whereas vBMD increased by 12.8% (p = 0.02) in the PTH treatment group compared with the placebo group.
Rubin and cols. (2323 . Rubin MR, Dempster DW, Sliney J Jr, Zhou H, Nickolas TL, Stein EM, et al. PTH(1-84) administration reverses abnormal bone-remodeling dynamics and structure in hypoparathyroidism. J Bone Miner Res. 2011;26(11):2727-36.) hypothesized that parathyroid hormone(11 . Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391-403.-84) [PTH(1-84)] treatment would restore skeletal properties toward normal in hypoparathyroidism. This study included 64 subjects with hypoparathyroidism who were treated with PTH(11 . Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391-403.-84) for 2 years. All subjects underwent histomorphometric assessment with percutaneous iliac crest bone biopsies at baseline and at 1 or 2 years. Another group of subjects had a single biopsy at 3 months, having received tetracycline before beginning PTH(11 . Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391-403.-84) and prior to the biopsy, using a quadruple-label protocol. Biochemical bone turnover markers were measured. Structural changes after PTH(11 . Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391-403.-84) treatment for two years included reduced trabecular width (144 ± 34 µm to 128 ± 34 µm, p = 0.03) and increased trabecular number (1.74 ± 0.34/mm to 2.07 ± 0.50/mm, p = 0.02). Cortical porosity increased after two years of treatment from 7.4% ± 3.2% to 9.2% ± 2.4% (p = 0.03). Histomorphometrically measured dynamic parameters, including mineralizing surface, increased significantly at three months, peaked at one year (0.7% ± 0.6% to 7.1% ± 6.0%, p = 0.001), and persisted at two years. Biochemical measurements of bone turnover increased significantly, peaking after five to nine months of therapy, and persisting for 24 months. The study concluded that PTH(11 . Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391-403.-84) treatment of hypoparathyroidism is associated with increases in histomorphometric and biochemical indices of skeletal dynamics. Structural changes were felt to be consistent with an increased remodeling rate in both trabecular and cortical compartments, with tunneling resorption in cortical bone. These changes were interpreted as suggesting that PTH(11 . Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391-403.-84) improves abnormal skeletal properties in hypoparathyroidism, and restores bone metabolism toward normal euparathyroid levels.
Gafni and cols. (2424 . Gafni RI, Brahim JS, Andreopoulou P, Bhattacharyya N, Kelly MH, Brillante BA, et al. Daily parathyroid hormone 1-34 replacement therapy for hypoparathyroidism induces marked changes in bone turnover and structure. J Bone Miner Res. 2012;27(8):1811-20.) discontinued calcitriol therapy and treated 2 adult and 3 adolescent hypoparathyroid patients with synthetic human PTH 1-34 (hPTH 1-34), injected two to three times daily for 18 months, with doses individualized to maintain serum calcium at 1.9 to 2.25 mmol/L. Biochemical markers and BMD were assessed every 6 months, and iliac crest biopsies performed before and after one year of treatment. hPTH 1-34 therapy significantly increased bone markers to supranormal levels. Bone histomorphometry revealed that treatment dramatically increased cancellous bone volume and trabecular number, and decreased trabecular separation. Changes in trabecular width were variable, suggesting that the increase in trabecular number was due to the observed intratrabecular tunneling. Cortical width remained unchanged, but hPTH 1-34 treatment increased cortical porosity. Cancellous bone remodeling was also stimulated, inducing significant changes in osteoid, mineralizing surface, and bone formation rate. Similar changes were seen in endocortical and intracortical remodeling. BMD Z-scores were unchanged at the spine and femoral neck. Total hip Z-scores increased, but total body BMD Z-scores decreased during the first 6 months of treatment and then stabilized, remaining significantly decreased compared to baseline. Radial Z-scores also decreased with treatment, and this was most pronounced in the growing adolescent patient. Daily hPTH 1-34 therapy for hypoparathyroidism stimulated bone turnover, increased bone volume, and altered bone structure in the iliac crest. These findings were interpreted as suggesting that treatment with hPTH 1-34 in hypoparathyroid adults and adolescents has varying effects in the different skeletal compartments, leading to an increase in trabecular bone and an apparent trabecularization of cortical bone.
Neer and cols. (2525 . Rubin MR, Sliney J Jr, McMahon DJ, Silverberg SJ, Bilezikian JP. Therapy of hypoparathyroidism with intact parathyroid hormone. Osteoporos Int. 2010;32:1927-34.) showed that compared with baseline in postmenopausal osteoporotic women, BMD increased at the lumbar spine by 2.9% ± 4% (p < 0.05) from 1.24 ± 0.3 to 1.27 ± 0.3 g/cm(22 . Bilezikian JP, Khan A, Potts JT Jr, Brandi ML, Clarke BL, Shoback D, et al. Hypoparathyroidism in the adult: epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment, and challenges for future research. J Bone Miner Res. 2011;26(10):2317-37.) (T-score 1.7 ± 2.0 to 1.9 ± 2.0) after treatment with teriparatide (PTH 1-34) over 21 months. The lumbar spine is a site that is enriched in cancellous bone. Because PTH is known to be anabolic for cancellous bone, this observation was interpreted to indicate that new, younger bone was being formed as a result of PTH treatment. A more detailed examination of skeletal features using high resolution imaging or bone biopsy will be necessary to elucidate which changes in microarchitectural parameters contribute to the increase in trabecular BMD. Such results also would be of great interest in terms of a comparison between the effects of PTH(1–84) as a therapy for osteoporosis or as replacement therapy for hypoparathyroidism. Along with the increase in lumbar spine BMD, a decrease in the distal 1/3 radius, a site enriched in cortical bone, was observed, decreasing by 2.4% ± 4.0% (p < 0.05) from 0.73 ± 0.1 to 0.70 ± 0.1 g/cm(2) (T-score, -0.03 ± 2.0 to -0.26 ± 1.0). These results suggest that teriparatide causes endosteal resorption. These data do not imply that bone is weakened because salutary effects on microarchitecture and bone size could well provide biomechanical advantages despite the reduction in BMD. More detailed skeletal assessment will be required to answer this question. Overall, these changes in trabecular and cortical skeletal compartments recall the pattern seen with PTH treatment of osteoporosis in individuals who do not have hypoparathyroidism (26).
Taken together, these studies suggest that treatment of patients with hypoparathyroidism with PTH of different forms reduces BMD toward normal and improves bone microarchitecture, resulting in improved bone strength. These changes should also lead to reduced fracture risk, but prospective randomized controlled trials have not yet been conducted to demonstrate this.
CONCLUSION
Bone disease occurs in hypoparathyroidism due to the absence or relative deficiency of parathyroid hormone. Lack of parathyroid hormone results in low bone turnover and increased bone mineral density with associated increased bone mineralization. Whether these changes affect risk of fracture is not yet clear. Nevertheless, treatment with parathyroid hormone appears to improve the structural quality of bone.
REFERENCES
-
1Shoback D. Clinical practice. Hypoparathyroidism. N Engl J Med. 2008;359:391-403.
-
2Bilezikian JP, Khan A, Potts JT Jr, Brandi ML, Clarke BL, Shoback D, et al. Hypoparathyroidism in the adult: epidemiology, diagnosis, pathophysiology, target-organ involvement, treatment, and challenges for future research. J Bone Miner Res. 2011;26(10):2317-37.
-
3Langdahl BL, Mortensen L, Vesterby A, Eriksen EF, Charles P. Bone histomorphometry in hypoparathyroid patients treated with vitamin D. Bone. 1996;18(2):103-8.
-
4Kruse K, Kracht U, Wohlfart K, Kruse U. Biochemical markers of bone turnover, intact serum parathyroid hormone and renal calcium excretion in patients with pseudohypoparathyroidism and hypoparathyroidism before and during vitamin D treatment. Eur J Pediatr. 1989;148(6):535-9.
-
5Mizunashi K, Furukawa Y, Miura R, Yumita S, Sohn HE, Yoshinaga K. Effects of active vitamin D3 and parathyroid hormone on the serum osteocalcin in idiopathic hypoparathyroidism and pseudohypoparathyroidism. J Clin Invest. 1988;82(3):861-5.
-
6Abugassa S, Nordenström J, Eriksson S, Sjödén G. Bone mineral density in patients with chronic hypoparathyroidism. J Clin Endocrinol Metab. 1993;76(6):1617-21.
-
7Fujiyama K, Kiriyama T, Ito M, Nakata K, Yamashita S, Yokoyama N, et al. Attenuation of postmenopausal high turnover bone loss in patients with hypoparathyroidism. J Clin Endocrinol Metab. 1995;80(7):2135-8.
-
8Seeman E, Wahner HW, Offord KP, Kumar R, Johnson WJ, Riggs BL. Differential effects of endocrine dysfunction on the axial and the appendicular skeleton. J Clin Invest. 1982;69(6):1302-9.
-
9Touliatos JS, Sebes JI, Hinton A, McCommon D, Karas JG, Palmieri GM. Hypoparathyroidism counteracts risk factors for osteoporosis. Am J Med Sci. 1995;310(2):56-60.
-
10Sikjaer T, Rejnmark L, Thomsen JS, Tietze A, Bruel A, Andersen G, et al. Changes in 3-dimensional bone structure indices in hypoparathyroid patients treated with PTH(1-84): a randomized controlled study. J Bone Miner Res. 2012;27(4):781-8.
-
11Takamura Y, Miyauchi A, Yabuta T, Kihara M, Ito Y, Miya A. Attenuation of postmenopausal bone loss in patients with transient hypoparathyroidism after total thyroidectomy. World J Surg. 2013;37(12):2860-5.
-
12Sugitani I, Fujimoto Y. Effect of postoperative thyrotropin suppressive therapy on bone mineral density in patients with papillary thyroid carcinoma: a prospective controlled study. Surgery. 2011;150(6):1250-7.
-
13Biondi B, Cooper DS. Benefits of thyrotropin suppression versus the risks of adverse effects in differentiated thyroid cancer. Thyroid. 2010;20(2):135-46.
-
14Chen Q, Kaji H, Iu MF, Nomura R, Sowa H, Yamauchi M, et al. Effects of an excess and a deficiency of endogenous parathyroid hormone on volumetric bone mineral density and bone geometry determined by peripheral quantitative computed tomography in female subjects. J Clin Endocrinol Metab. 2003;88(10):4655-8.
-
15Cohen A, Dempster DW, Müller R, Guo XE, Nickolas TL, Liu XS, et al. Assessment of trabecular and cortical architecture and mechanical competence of bone by high-resolution peripheral computed tomography: comparison with transiliac bone biopsy. Osteoporos Int. 2010;21(2):263-73.
-
16Rubin MR, Dempster DW, Zhou H, Shane E, Nickolas T, Sliney J Jr, et al. Dynamic and structural properties of the skeleton in hypoparathyroidism. J Bone Miner Res. 2008;23(12):2018-24.
-
17Rubin MR, Dempster DW, Kohler T, Stauber M, Zhou H, Shane E, et al. Three dimensional cancellous bone structure in hypoparathyroidism. Bone. 2010;46(1):190-5.
-
18Christen P, Ito K, Müller R, Rubin MR, Dempster DW, Bilezikian JP, et al. Patient-specific bone modelling and remodelling simulation of hypoparathyroidism based on human iliac crest biopsies. J Biomech. 2012;45(14):2411-6.
-
19Mendonça ML, Pereira FA, Nogueira-Barbosa MH, Monsignore LM, Teixeira SR, Watanabe PC, et al. Increased vertebral morphometric fracture in patients with postsurgical hypoparathyroidism despite normal bone mineral density. BMC Endocr Disord. 2013;13:1.
-
20Underbjerg L, Sikjaer T, Mosekilde L, Rejnmark L. Post-surgical hypoparathyroidism - risk of fractures, psychiatric diseases, cancer, cataract, and infections. J Bone Miner Res. 2014 May 7 [Epub ahead of print].
-
21Duan Y, De Luca V, Seeman E. Parathyroid hormone deficiency and excess: similar effects on trabecular bone but differing effects on cortical bone. J Clin Endocrinol Metab. 1999;84(2):718-22.
-
22Sikjaer T, Rejnmark L, Thomsen JS, Tietze A, Brüel A, Andersen G, et al. Changes in 3-dimensional bone structure indices in hypoparathyroid patients treated with PTH(1-84): a randomized controlled study. J Bone Miner Res. 2012;27(4):781-8.
-
23Rubin MR, Dempster DW, Sliney J Jr, Zhou H, Nickolas TL, Stein EM, et al. PTH(1-84) administration reverses abnormal bone-remodeling dynamics and structure in hypoparathyroidism. J Bone Miner Res. 2011;26(11):2727-36.
-
24Gafni RI, Brahim JS, Andreopoulou P, Bhattacharyya N, Kelly MH, Brillante BA, et al. Daily parathyroid hormone 1-34 replacement therapy for hypoparathyroidism induces marked changes in bone turnover and structure. J Bone Miner Res. 2012;27(8):1811-20.
-
25Rubin MR, Sliney J Jr, McMahon DJ, Silverberg SJ, Bilezikian JP. Therapy of hypoparathyroidism with intact parathyroid hormone. Osteoporos Int. 2010;32:1927-34.
-
Financial support: none.
Publication Dates
-
Publication in this collection
July 2014
History
-
Received
3 Apr 2014 -
Accepted
14 May 2014