Abstracts
Objective
To survey the prevalence of diabetes mellitus (DM) and pre-diabetes mellitus (PDM) in the Muslim population in northwest China, and discuss the risk factor.
Materials and methods
According to the income and the population, we randomly selected 3 villages with stratified and cluster sampling. The subjects were residents ≥ 20 years of age, and were from families which have been local for > 3 generations. The questionnaire and oral glucose tolerance test (OGTT) were completed and analyzed for 660 subjects.
Results
The prevalence of DM and PDM between the Han and Muslim populations were different (P = 0.041). And the prevalence were also different with respect to age in the Han (P < 0.001) and Muslim population (P < 0.001) respectively. Except for the 20-year-old age group the prevalence of DM and PDM within the Muslim population was higher than the Han (P = 0.013), we did not find any significant difference for other age groups (P > 0.05). The intake of salt (P < 0.001) and edible oil (P < 0.001) in the Muslim population was higher than the Han, while cigarette smoking (P < 0.001) and alcohol consumption (P < 0.001) was lower. BMI (P < 0.001), age (P = 0.025), and smoking cigarettes (P = 0.011) were risk factors for DM and PDM, but alcohol consumption (P < 0.001) was a protective factor.
Conclusions
In northwest China, the prevalence of DM was higher in the Muslim population, and it was special higher on the 20-year-old age compared to the Han. This might be explained by the potential genetic differences and poor dietary habits.
Risk factors; diabetes; Muslim population in China; northwest China
Objetivo
Avaliar a prevalência de diabetes melito (DM) e pré-diabetes melito (PDM) na população muçulmana no noroeste da China e discutir os fatores de risco.
Materiais e métodos
Selecionamos três vilarejos de acordo com a renda e a população, usando uma amostra estratificada e por cluster. Os sujeitos eram residentes com ≥ 20 anos de idade e de famílias que estavam no local há mais de três gerações. Foram feitos e analisados um questionário e o teste de tolerância oral à glicose (TTOG) para 660 sujeitos.
Resultados
A prevalência do DM e PDM entre as populações Han e muçulmana foi diferente (P = 0,041), e as prevalências também foram diferentes com relação à idade na população Han (P < 0,001) e muçulmana (P < 0,001), respectivamente. Exceto pela faixa etária de 20 anos de idade, a prevalência do DM e PDM na população muçulmana foi maior do que na população Han (P = 0,013), não havendo diferenças significativas para as outras faixas etárias (P > 0,05). A ingestão de sal (P < 0,001) e óleos comestíveis (P < 0,001) na população muçulmana foi mais alta do que na população Han, enquanto o tabagismo (P < 0,001) e consumo de álcool (P < 0,001) foram mais baixos. O IMC (P < 0,001), a idade (P = 0,025) e o tabagismo (P = 0,011) foram fatores de risco para o DM e PDM, mas o consumo de álcool (P < 0,001) foi um fator protetor.
Conclusões
No noroeste da China, a prevalência de DM é maior na população muçulmana e é especialmente mais alta na faixa etária de 20 anos de idade, quando comparada com a população Han. Isso pode ser explicado por diferenças genéticas potenciais e hábitos alimentares ruins.
Fatores de risco; diabetes; população muçulmana na China; noroeste da China
INTRODUCTION
Diabetes mellitus (DM) is one of the most common diseases worldwide and
may lead to micro- and macro-vascular complications. Common risk factors for the development
of DM include central obesity, family history, and dyslipidemia (11 Pan XR, Yang WY, Li GW, Liu J. Prevalence of diabetes and its risk factors
in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care.
1997;20(11):1664-9.,22 Yang ZJ, Liu J, Ge JP, Chen L, Zhao ZG, Yang WY; China National Diabetes
and Metabolic Disorders Study Group. Prevalence of cardiovascular disease risk factor in
the Chinese population: the 2007-2008 China National Diabetes and Metabolic Disorders
Study. Eur Heart J. 2012;33(2):213-20.). In many countries the
prevalence of DM has shown an upward trend in recent years, which is affected by some known
risk factors, such as dyslipidemia, obesity, poor dietary habits, and exercise (11 Pan XR, Yang WY, Li GW, Liu J. Prevalence of diabetes and its risk factors
in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care.
1997;20(11):1664-9.,33 Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and
exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT
and Diabetes Study. Diabetes Care. 1997;20(4):537-44.
4 Yang ZJ, Yang WY, Li GW; National Diabetes Prevention and Control
Cooperative Group. The distributive characteristics of impaired glucose metabolism
subcategories in Chinese adult population. Zhonghua Yi Xue Za Zhi.
2003;83(24):2128-31.
5 King H, Albert RE, Henman WH. Global burden of diabetes, 1995-2025:
prevalence, numerical estimates, and projections. Diabetes Care.
1998;21(9):1414-31.-66 Hu YH, Li GW, Pan XR. [Incidence of NIDDM in Daqing and forecasting of
NIDDM in China in 21st century]. Zhonghua Nei Ke Za Zhi.
1993;32(3):173-5.). However, few studies have focused on the prevalence of
DM in different races in the same geographic area. In China, the Han population is the
largest majority group. It represents 92% of the inhabitants of China. Currently, the
existing many studies have described the social-demographic characteristics and the
prevalence of DM in China, such as The Da Qing IGT and Diabetes Study (33 Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and
exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT
and Diabetes Study. Diabetes Care. 1997;20(4):537-44.). A recent study conducted in 2010 reported the age-standardized
prevalence of total DM and pre-diabetes mellitus (PDM) were 9.7% and 15.5%
respectively in China (77 Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. Prevalence of diabetes
among men and women in China. N Engl J Med. 2010;362(12):1090-101.,88 Yang ZJ, Yang WY, Xiao JZ, Li GW, Wang Y. [Impact of lowering the
cut-point for impaired fasting glucose on the distribution of impaired glucose regulation
subcategories in Chinese adult population]. Zhonghua Yi Xue Za Zhi.
2004;84(21):1773-6.). These findings supported that Han population can represent the
findings of the Chinese population in general and can be used as a control group in relation
to the findings in Han population. The Han population is thus better characterized and can
be easier for the comparison of the findings in the other ethnicity populations. On the
other hand, owing to the special characteristics of dietary habits, the Muslim population in
China, one of the largest minority groups, has clear differences in the characteristics from
other Chinese groups. Residents in the Ningxia Hui Autonomous Region, a major place of
habitation for Chinese Muslims, make up > 40% of the Muslim population in China. Guyuan
city, which is located in the southern mountain area of the Ningxia Hui Autonomous Region,
is a small town in the northern route of Silk Road and inhabited by a traditional Muslim
population (Hui). According to the 2008 demographic statistics, population in Guyuan is 1.53
million, among them Muslim population are 0.65 million which is accounted for 44.1 percent
of total population. The Muslim population in Guyuan city, whose ancestors were Muslim
merchants of Persia and Arab, are different from other local Chinese ancient Muslims, such
as residents in Uygur, Kazak, and Kirgiz. Although Muslims live together with Han,
intermarriage is uncommon due to economic backwardness. Moreover, most residents lived in
the same area for more than three generations, and mobile populations are uncommon. There
are no policies to control the Muslim population, so multiple pregnancies are common, which
also leads to distinctive demographic characteristics. In addition to demographic
characteristics, diet in the Muslim population is different from the Han population. The Han
population subsists mainly on pork; however, beef and mutton are the main meats consumed by
the Muslim population. In the winter, preserved food is the main non-staple food because
there are almost no fresh vegetables, which leads to high salt intake for people.
We have reviewed many papers which have addressed DM in the Muslim population. Most of the studies have focused on glycemic trends during Ramadan in fasting subjects with DM or the treatment of DM (99 Ahmadani MY, Riaz M, Fawwad A, Hydrie MZ, Hakeem R, Basit A. Glycaemic trend during Ramadan in fasting diabetic subjects: a study from Pakistan. Pak J Biol Sci. 2008;11(16):2044-7.,1010 Fernández Miró M, Goday A, Cano JF. [Treatment of diabetes mellitus during Ramadan]. Med Clin (Barc). 2007;129(8):303-8.). Few studies regarding the prevalence of DM and PDM or risk factors in the Muslim population have been reported, especially comparisons with other non-Muslims in the same geographic areas (1111 Dowse GK, Gareeboo H, Zimmet PZ, Alberti KG, Tuomilehto J, Fareed D, et al. High prevalence of NIDDM and impaired glucose tolerance in Indian, Creole, and Chinese Mauritians. Mauritius Noncommunicable Disease Study Group. Diabetes. 1990;39(3):390-6.,1212 King H, Rewers M. Global estimates for prevalence of diabetes mellitus and impaired glucose tolerance in adults. WHO Ad Hoc Diabetes Reporting Group. Diabetes Care. 1993;16(1):157-77.). Within the same geographic environment, whether or not the distinctive demographic characteristics and special eating habits are the intrinsic factors which result in some diseases, such as DM, is always our main concern. Our previous study showed that glucose metabolic disorders in Guyuan city, which was based on the subjects in the permanent population surrounding the rural area, was higher than other cities in Ningxia, China (1313 Liu WF, Yin XL, Wang DK, Dai XW, Song HL, Liu W, et al. Screening analysis of type 2 diabetes in Ningxia Guyuan city. Clinical Focus. 2011;26(10):870-2.). It is necessary to perform further investigation and research of the population in this region, especially the Muslim population, because there are significant difference between Han and Muslim populations, according to our previous study (1313 Liu WF, Yin XL, Wang DK, Dai XW, Song HL, Liu W, et al. Screening analysis of type 2 diabetes in Ningxia Guyuan city. Clinical Focus. 2011;26(10):870-2.).
In the current study we determined the prevalence of DM and PDM in the Muslim population in China and determined the special risk factors in their race.
MATERIALS AND METHODS
Participants
A total of 1,963 villagers were studied between January 2009 and February 2011. In our study, we selected the two-stage sampling procedure to collect samples. In the first stage, consider different income levels might affect the diet habits which can further affect the incidence of DM and PDM, we thus performed the population stratification based on the income levels (high level [> 1500 Renminbi {RMB}, middle level [1000 - 1500 RMB], and low level [< 1000 RMB]) per capita per year (1414 Fu C, Chen Y, Wang F, Wang X, Song J, Jiang Q. High prevalence of hyperglycemia and the impact of high household income in transforming rural China. BMC Public Health. 2011;11:862.,1515 Chang JX, Sun L. The national salary difference in the rural labors: a research from Guyuan, Ningxia Hui autonomous region [J]. Management World (Monthly). 2008(3):81-5.). For each income level, we sampled one countryside from those countrysides around Guyuan city with the same income levels. After performing the stratified sampling, three countrysides were selected. In the second stage, consider the population size and the economical situation of each subordinate village from the corresponding countryside is similar; we thus adopted the cluster sampling to extract one village from the selected each countryside in the first stage. Finally, a total of 1,963 villagers from three villages were selected. After excluding those samples with greater missing information, 660 participants ≥ 20 y of age (mean age = 45.79 ± 14.65 y; 288 males and 372 females) and residence in the village for ≥ 20 years of Guyuan, Ningxia were included in the study. The sample population was limited to families that had been local for greater than three generations. The current research planned to collect 800 responses. Participation in the survey was voluntary. If subjects declined to participate, the investigators attempted to survey the neighbor. This process continued until the targeted number of surveys was reached. All of the participants signed informed consent. The study was approved by the Ethics Committee of Ningxia Teachers’ University.
Methods
The level of fasting blood glucose (FBG; fasting for at least 8 h), and 2-h postprandial blood glucose (PBG2h; after a normal meal) were measured for all of the research subjects using Roche’s superior blood glucose meter, which has an error < ± 15% compared with venous blood. With a fasting blood glucose cut-off of < 5.6 mmol/L, the diagnosis of IFG can significantly improve the sensitivity of fasting glucose in predicting DM (55 King H, Albert RE, Henman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21(9):1414-31.,66 Hu YH, Li GW, Pan XR. [Incidence of NIDDM in Daqing and forecasting of NIDDM in China in 21st century]. Zhonghua Nei Ke Za Zhi. 1993;32(3):173-5.); thus, we chose a fasting plasma glucose level ≥ 5.6 mmol/L as the oral glucose tolerance test (OGTT) screening cut-off level. In participants who had a FBG ≥ 5.60 mmol/L (105 mg/dL) and a PBG2h ≥ 7.8 mmol/L (140 mg/dL), an extra 75 g oral glucose tolerance test was performed (OGTT; Beckman-Unicel Dxc800 biochemistry analyzer; Beckman Ltd., Suzhou, Jiangsu, China) (1616 Yang WY, Xing XY, Yang CJ, et al. Exploring the diagnostic level of fasting plasma glucose in Chinese diabetic population [J]. Chin J Endocrinol Metab. 1988;14(1):3-7.). The diagnosis was based on the results of the 75 g OGTT and World Health Organization criteria. Among all of the research subjects, those with a normal FBG (normal range, 4.4-6.1 mmol/L) and a PBG2h (normal range, 4.4-7.8 mmol/L) were diagnosed as normal glucose tolerance (NGT), and others who had a normal FBG and elevated PBG2h (> 7.8 and < 11.1 mmol/L) were diagnosed with impaired glucose tolerance (IGT). The research subjects with a normal PBG2h and an elevated FBG (> 6.1 and < 7.0 mmol/L) were diagnosed with impaired fasting glucose (IFG). The research subjects with an elevated FBG (> 7.0 mmol/L) and an elevated PBG2h (> 11.1 mmol/L) were diagnosed with DM. The research subjects with a FBG > 7.0 mmol/L and a PBG2h < 11.1 mmol/L or a FBG < 7.0 mmol/L and a PBG2h > 11.1 mmol/L, the OGTT was measured repeatedly.
Questionnaires for the DM epidemiologic study were based on the Chinese Academy of Preventive Medicine, and consisted of ethnic, health status, medical history, family history, physical work, income, cigarette smoking and alcohol consumption habits, intake of oil and salt, and status of the subject’s awareness. During the survey, 836 questionnaires were used. Of the 836 questionnaires, 50 had missing information (e.g., oil and salt intake was not captured as well as information on pregnancy and childbirth) and 126 only completed the questionnaire and did not have the intact blood glucose indicator because no OGTT was performed after the rapid finger-blood glucose procedure. The remaining 660 subjects who had matched completed questionnaire and intact blood glucose results were included in the statistical analysis.
The Muslim and Han populations are differentiated by inheritance and identity. In this observation, the Muslim or Han population was identified when they were in an ethnic group for greater than three generations. In this area, because of tradition, inter-ethnic marriages do not occur. The few intermarriage couples migrated to other regions. The question regarding intermarriage was asked when the questionnaire was developed. People with an intermarriage history were excluded. The researchers searched three generations of the subjects to verify their ethnicity as Muslim (believing in the religion) or Han (who can have or not).
The questionnaire regarding edible oil and salt intake was designed as follows: how many people ≥ 20 years of age are in your family? What is the consumption of salt and edible oil monthly? Then, the salt and edible oil intake per person was estimated. Because there were local customs, such as preserved salted food for the winter in some seasons and preparing plenty of fried food for festivals, the edible oil and salt intake was not calculated monthly, but yearly. Dietary guidelines advocate that the daily salt intake should be < 6 grams per person per day, thus the annual salt intake should be 2190 g (2.19 kg/year). Beijing is a city with a high daily salt intake, which reaches 15 grams (5.47 kg/year). Based on the records, we determined whether or not the salt intake was excessive in the Muslim population.
The body mass index (BMI), waist and hip circumference, and blood pressure were measured and recorded. The researcher inquired about a history of hypertension and medication use and noted “hypertension”, when indicated. Those who did not have a history of hypertension were examined in the seated position after 3 minutes for blood pressure measurement (both left and right. Researchers picked the arm with the highest blood pressure reading, and obtained 3 blood pressure readings every 2 minutes. The average of the three measurements was used to confirm a diagnosis of hypertension. If the systolic pressure was > 140 mmHg or the diastolic pressure was > 90 mmHg, the villager would be suspected to have hypertension and would re-visit to measure the blood pressure. If the result was the same, the diagnosis of hypertension was confirmed. If the result was different, the blood pressure was measured for a third time and the diagnosis was based on the third result.
Gravidas were excluded from this study because pregnancy, parturition times, and macrosomia were recorded in the medical history, and capillary glucose measurements and OGTT tests were performed. Macrosomia is defined as a fetus with a birth weight ≥ 8 kilograms.
This research was conducted by teachers and students in the Department of Medicine at Ningxia Teachers’ University and the staff in the Centers for Disease Control and Prevention of Yuanzhou District in Guyuan City. They received proper training before the project began. The training included a physical examination (height, weight, and waist circumference), blood pressure and glucose measurement, pre-survey preparation before the procedures, the content and structure of the questionnaire, and surveys prompting and completion of skills. Quality control was performed during the entire survey, and included the study design, survey staff training, field survey, data collection, data entry, summarization, statistics, and analysis. The quality control in the field survey was especially important and the supervisor in each team randomly examined 2% of the questionnaires and blood pressure as well as glucose by a second visit. This limited potential errors.
Statistical analysis
Data were analyzed using SPSS (version 17.0 for Windows; SPSS Inc., Chicago, IL, USA). The quantitative characteristics of the Han and Muslim population in China were expressed as the mean ± standard deviation, and were compared using a two-sample t-test. Chi-square tests were used to compare the categorical data and to determine the difference in prevalence in two race groups and in different age groups. Also, we used binary-logistic regression to detect potential risk factors of all the clinical characteristics on different OGTT results. P values < 0.05 were considered significant.
RESULTS
Race-specific characteristics of the Han and Muslim population in China
The two-sample t-tests and chi-square tests were used to compare the quantitative and categorical characteristics of the Han and Muslim populations in China. No significant difference was detected with respect to gender, age, BMI, WHR, SBP, and history of coronary heart disease between the Han and Muslim population (P > 0.05); however, there was a significant difference with respect to the DBP and history of hypertension between the two races. In summary, except the prevalence of “history of hypertension” is higher (P = 0.007) and the DBP is lower (P = 0.037) in Han population, there were no significant difference between two races for other clinical characteristics (P > 0.05; Table 1).
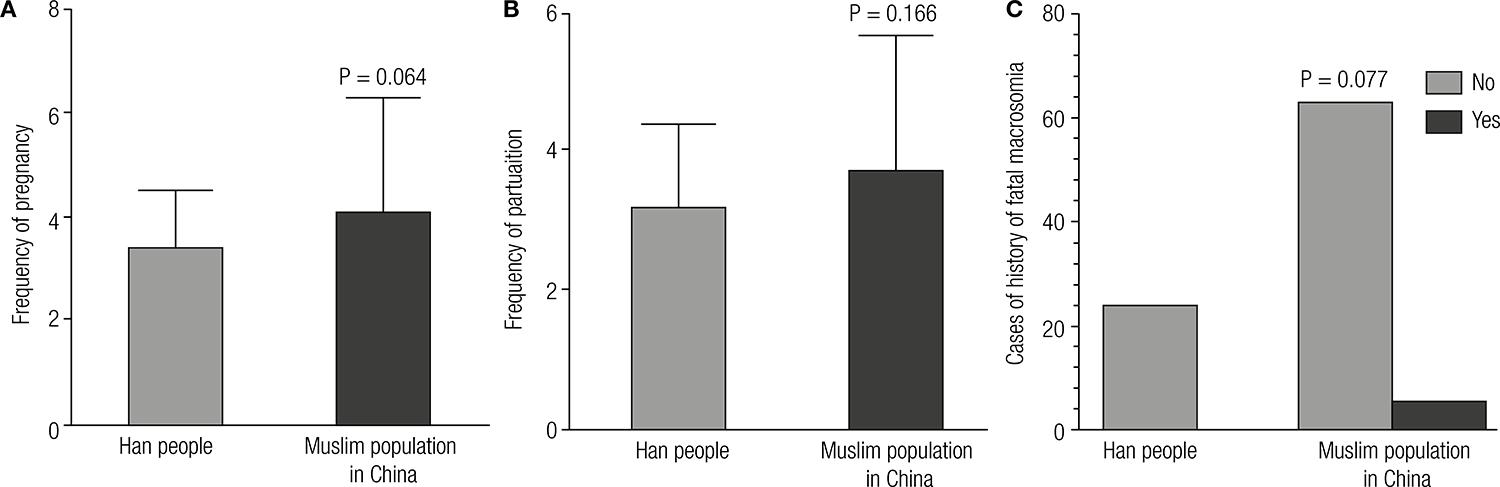
Based on the data elicited in the questionnaires, the intake of oil and salt, cigarette smoking, and drinking alcohol in the Muslim population were significantly different from the Han people (P < 0.001; Figure 1). No significant differences in the frequency of pregnancy (3.72 ± 1.71; P > 0.05) and frequency of parturition (3.34 ± 1.57; P > 0.05) existed between the Han and Muslim population. In addition, no significant difference in fetal macrosomia existed between the Han and Muslim population in China (P > 0.05; Figure 2), and the level of awareness of DM, PDM, and NGT was not significantly different between the Han and Muslim population using LR χ2 test (P = 0.152; Figure 3).
Comparison of the differences in intake of oil (A) and salt (B), cigarette smoking (C), and alcohol consumption (D) between the Han and Muslim population in China.
Comparison of the differences in frequency of pregnancy (A) and parturition (B), and cases with a history of fetal macrosomia (C) between the Han and Muslim population in China.
Awareness of diabetes and pre-diabetes, NGT (under) in the Han people and Muslim population in China (above).
Race-specific prevalence of DM and PDM among rustics
An age-adjusted Cochran–Mantel–Haenszel (CMH) test was used to analyze the differences in prevalence between the two race groups. Consider the most important demographic change to DM prevalence across the world appears to be the increase in the proportion of people ≥ 65 years of age, we therefore performed the age stratification (< 65y and ≥ 65y). The results showed that there was a significant difference in the prevalence of DM and PDM between the Han and Muslim populations in China after adjusting the age (P = 0.041). In the Muslim population, the prevalence of DM (5.8%), IGT (10.3%) were higher than the Han people, IFG (4.3%), and IFG + IGT (5.2%) were lower than the Han people (Table 2).
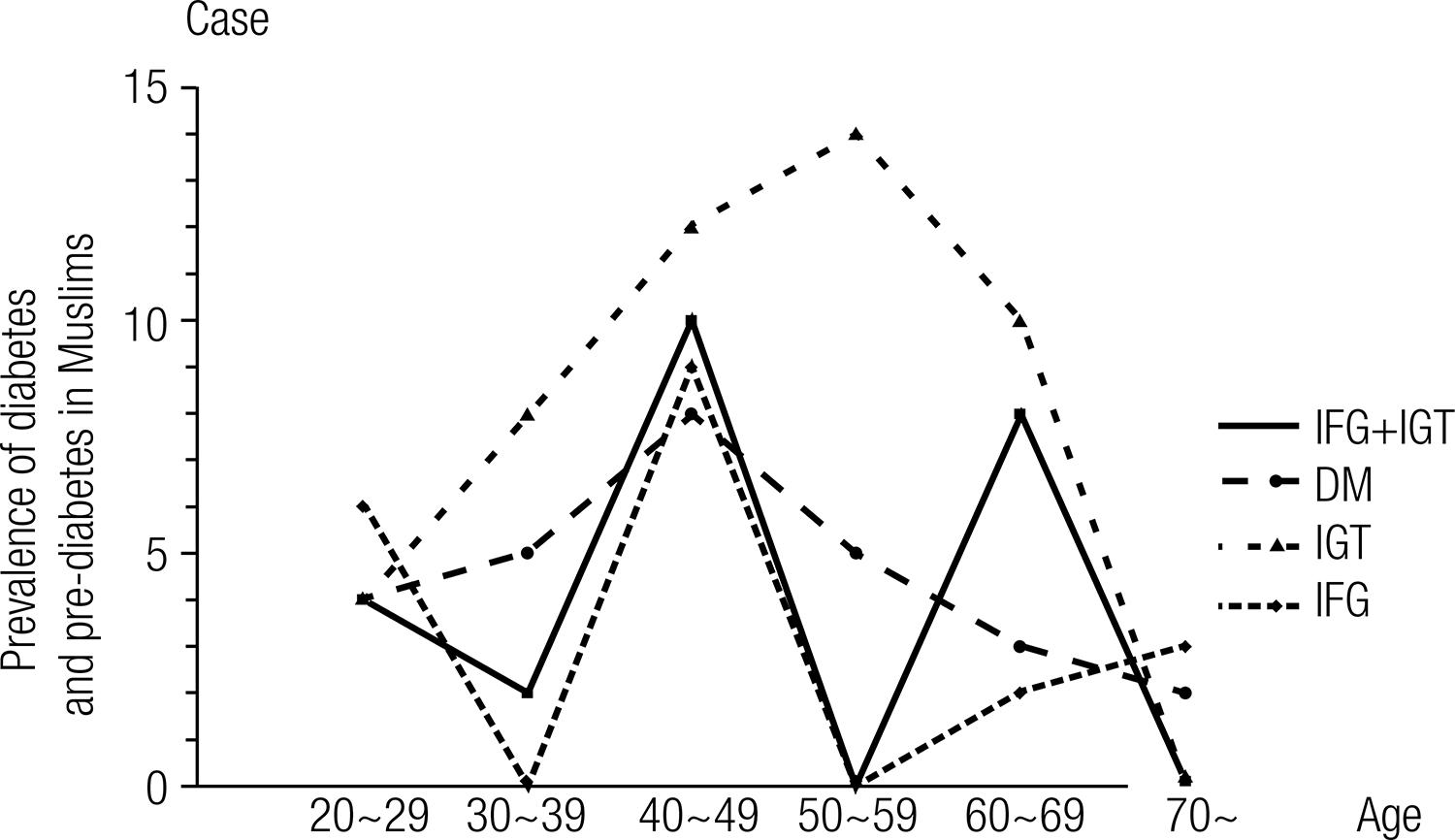
Prevalence of DM and PDM in the Muslim population in China and the risk factors
The prevalence of DM and PDM was significantly different among different age groups in the Muslim population in China using the Pearson χ2 test (P < 0.001). The IGT increased in those < 50-59 years of age and decreased in those > 50-59 years of age. DM increased in those < 40-49 years of and decreased in those > 40-49 years of age. The IFG + IGT had different upward trends in those 30-39 to 40-49 years and 50-59 to 60-69 years of age. Decreasing trends were found in those aged 20-29 to 30-39 years, 40-49 to 50-59 years, and 60-69 to > 70 years of age. The IFG increased in those 30-39 to 40-49 years and 50-59 to > 70 years of age. Decreasing trends existed in those 20-29 to 30-39 years and 40-49 to 50-59 years of age. The prevalence of DM and PDM in the 20-year-old age group within the Muslim population was higher than the Han (P = 0.013), we did not find any significant difference between the Han and Muslim population for other age groups (P > 0.05; Figure 4 and Table 3).
We used binary-logistic regression to detect the traditional risk factors for DM and PDM, and the results showed that BMI, age, cigarette smoking, and alcohol consumption were related to the prevalence of DM and PDM. The risk of DM and PDM increased the prevalence 2.196-fold (P < 0.001) and 1.186-fold (P = 0.025) when BMI and age increased, respectively. Cigarette smoking increased the risk of DM and PDM 3.41-fold over no-smoking (P = 0.011), while alcohol consumption was a protective factor (P < 0.001) (Table 4).
DISCUSSION
Guyuan City is located in the southern Ningxia Hui Autonomous Region, an economically underdeveloped region in northwest China. Because the Muslim population accounts for 44.1% of the total residents and most represent greater than three generations, the local population is different from other regions with distinct geographic and demographic characteristics. In a previous stratified cluster random sampling study of the Muslim population in this region we found that the prevalence of diabetes was higher than the Ningxia Lingwu region (3.16% in a 2008 survey) and Yinchuan (5.0% in a 2009 survey), in which the resident population was dominated by Han. The prevalence of IGT was higher than the Lingwu area (IGT standardized prevalence rate = 7.32%); the prevalence of IFG was close to Yinchuan (IFG prevalence rate = 4.0%), while there was a significant difference in the prevalence of IFG, IGT, DM, and IFG + IGT between the Han and Muslim population (P = 0.002) (1313 Liu WF, Yin XL, Wang DK, Dai XW, Song HL, Liu W, et al. Screening analysis of type 2 diabetes in Ningxia Guyuan city. Clinical Focus. 2011;26(10):870-2.). These results suggest that in Guyuan City (based on surrounding rural residents), the Muslim population has a high prevalence of glucose metabolism disturbance, thus it is necessary to perform further research in the Muslim population in the region.
We have shown that the prevalence of DM and IGT in the stratified sampling of rural residents around Guyuan city were higher in the Muslim population than the Han population and also higher than the general prevalence in the area, and the prevalence of IFG and IFG + IGT was lower than the Han population and the general prevalence in the area (P = 0.002) (1313 Liu WF, Yin XL, Wang DK, Dai XW, Song HL, Liu W, et al. Screening analysis of type 2 diabetes in Ningxia Guyuan city. Clinical Focus. 2011;26(10):870-2.,1717 Yang ZG, Liu L, Liu XY, Ma ZM, Li ZZ. The analysis of diabetic prevalence and the possible risk factors in the residents of community in Yinchuan city [J]. Ningxia Medical Journal. 2009;31(5):38-42.). Based on an analysis of the questionnaires for the DM epidemiologic study, we showed that characteristics, such as gender (F/M), age, BMI, and WHR, were similar in the different race groups, which indicated that there was no significant difference in demographic characteristics, although the Han and Muslim population belonged to different races with different living habits. Thus, the differences in demographic characteristics were not the reason for the differences in prevalence in DM and PDM. Ethnic and genetic differences may be an important reason for the high prevalence of DM and PDM.
Previous studies have shown that overweight and obese residents are uncommon in rural population in China. Risk factors for DM are mainly central obesity, family history, and dyslipidemia, rather than an elevated BMI. In our previous study we found that overweight subjects (28 > BMI ≥ 24 kg/m2) accounted for 27.7% of the population, which was greater than the average prevalence of overweight subjects in rural areas (25.85% according to the Zhengzhou University School of Public Health [2007], China) (1313 Liu WF, Yin XL, Wang DK, Dai XW, Song HL, Liu W, et al. Screening analysis of type 2 diabetes in Ningxia Guyuan city. Clinical Focus. 2011;26(10):870-2.). The BMI and WHR were not statistically different between the Muslim and Han populations in the region. BMI was a risk factor for glucose metabolism disturbance in the Muslim population; for each 1 kg/m2 increase in BMI, the prevalence risk increased 2.196-fold and WHR is not a major factor. Thus, with improved living standards and reducing the urban-rural divide, the Muslim rural population of overweight and obese subjects increased and glucose metabolism disturbance and DM risk factors have changed.
Based on the analysis of the questionnaire survey for the DM epidemiologic study, we found that there were ethnic differences in blood pressure, oil and salt consumption, cigarette smoking, and drinking alcohol appetites. Oil and salt intake in the Muslim population of the survey was significantly higher than the Han, but the prevalence rate of hypertension was significantly lower than the Han; cigarette smoking and drinking alcohol in the Muslim population were significantly less than the Han. The amount of cigarette smoking as a risk factor and alcohol consumption as a protective factor for glucose metabolism disturbance were statistically significant in the Muslim population. All these characteristics, and whether or not the characteristics are related with genes in the Muslim population, are worth further study in the future (1818 Cullmann M, Hilding A, Östenson CG. Alcohol consumption and risk of pre-diabetes and type 2 diabetes development in a Swedish population. Diabet Med. 2012;29(4):441-52.,1919 Engler PA, Ramsey SE. Diabetes and alcohol use: detecting at-risk drinking. J Fam Pract. 2011;60(12):E1-6.).
We also found that most females in the area had many pregnancies and deliveries, but there were no significant differences in the Han and Muslim population. A history of fetal macrosomia is often considered a risk factor for DM, which was similar in the different race groups. When we estimated the risk for DM and PDM in the Muslim population, the frequency of pregnancy and parturition, and a history of fetal macrosomia were not risk or protective factors. Thus, the differences in the frequency of pregnancy, parturition, and fetal macrosomia were not affected the prevalence of DM and PDM in the Muslim population.
In epidemiologic studies, awareness is an important indicator of the disease detection rate and severity of disease-related complications. In this study we found that awareness (only 25.34%) in the Muslim population was slightly higher than the Han nationality, and NGT was slightly higher than glucose metabolism disturbance, but the difference was not significant. Due to remoteness, ethnic minorities, rural areas, and economic backwardness in the region, the level of education was generally low and the relative isolation with the outside world, and the overall awareness of the disease was actually low. DM-related literacy work in this area is still important.
The study also found that there were significant differences in the prevalence of DM and PDM in the age distribution of Muslim and Han population. The prevalence of DM and PDM in the 20-year-old age group in the Muslim population were higher than the Han. Whether or not the genetic and dietary habits of the Muslim population and this characteristic were relevant is worthy of further study.
Due to limited conditions we were unable to observe more subjects in the study. The standard OGTT test was not carried out on the normal finger blood glucose (fasting and postprandial 2 hours). The differences in genetics between Muslim and Han populations were not studied in depth. For these unresolved issues, we will continue to conduct in-depth research in the future.
Additional information: Liu W wrote the manuscript, contributed to the discussion, researched data, and reviewed/edited the manuscript. Hua L researched data, and contributed to the discussion. Liu WF, Song HL, and Dai XW researched data and contributed to the discussion. Yang JK reviewed the manuscript.
Ackonwledgements
Dr. Liu W (Department of Endocrinology, Beijing Tongren Hospital, Capital Medical University), Dr. Hua L (Biomedical Engineering Institute, Capital Medical University), and Dr. Liu WF (Department of Medicine, Ningxia Teachers’ University), are the guarantors of this work, had full access to all of the data, and take full responsibility for the integrity of the data and the accuracy of the data analysis. This work was partially supported by the Beijing Natural Science Foundation (Grant Nos. 7142015) and the Science Technology Development Project of Beijing Municipal Commission of Education (SQKM201210025008) and the Science and Technology Research Project of Ningxia Higher School ([2010] 297). We give special thanks to Liu WF and to his memory with this paper.
REFERENCES
-
1Pan XR, Yang WY, Li GW, Liu J. Prevalence of diabetes and its risk factors in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care. 1997;20(11):1664-9.
-
2Yang ZJ, Liu J, Ge JP, Chen L, Zhao ZG, Yang WY; China National Diabetes and Metabolic Disorders Study Group. Prevalence of cardiovascular disease risk factor in the Chinese population: the 2007-2008 China National Diabetes and Metabolic Disorders Study. Eur Heart J. 2012;33(2):213-20.
-
3Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20(4):537-44.
-
4Yang ZJ, Yang WY, Li GW; National Diabetes Prevention and Control Cooperative Group. The distributive characteristics of impaired glucose metabolism subcategories in Chinese adult population. Zhonghua Yi Xue Za Zhi. 2003;83(24):2128-31.
-
5King H, Albert RE, Henman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21(9):1414-31.
-
6Hu YH, Li GW, Pan XR. [Incidence of NIDDM in Daqing and forecasting of NIDDM in China in 21st century]. Zhonghua Nei Ke Za Zhi. 1993;32(3):173-5.
-
7Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362(12):1090-101.
-
8Yang ZJ, Yang WY, Xiao JZ, Li GW, Wang Y. [Impact of lowering the cut-point for impaired fasting glucose on the distribution of impaired glucose regulation subcategories in Chinese adult population]. Zhonghua Yi Xue Za Zhi. 2004;84(21):1773-6.
-
9Ahmadani MY, Riaz M, Fawwad A, Hydrie MZ, Hakeem R, Basit A. Glycaemic trend during Ramadan in fasting diabetic subjects: a study from Pakistan. Pak J Biol Sci. 2008;11(16):2044-7.
-
10Fernández Miró M, Goday A, Cano JF. [Treatment of diabetes mellitus during Ramadan]. Med Clin (Barc). 2007;129(8):303-8.
-
11Dowse GK, Gareeboo H, Zimmet PZ, Alberti KG, Tuomilehto J, Fareed D, et al. High prevalence of NIDDM and impaired glucose tolerance in Indian, Creole, and Chinese Mauritians. Mauritius Noncommunicable Disease Study Group. Diabetes. 1990;39(3):390-6.
-
12King H, Rewers M. Global estimates for prevalence of diabetes mellitus and impaired glucose tolerance in adults. WHO Ad Hoc Diabetes Reporting Group. Diabetes Care. 1993;16(1):157-77.
-
13Liu WF, Yin XL, Wang DK, Dai XW, Song HL, Liu W, et al. Screening analysis of type 2 diabetes in Ningxia Guyuan city. Clinical Focus. 2011;26(10):870-2.
-
14Fu C, Chen Y, Wang F, Wang X, Song J, Jiang Q. High prevalence of hyperglycemia and the impact of high household income in transforming rural China. BMC Public Health. 2011;11:862.
-
15Chang JX, Sun L. The national salary difference in the rural labors: a research from Guyuan, Ningxia Hui autonomous region [J]. Management World (Monthly). 2008(3):81-5.
-
16Yang WY, Xing XY, Yang CJ, et al. Exploring the diagnostic level of fasting plasma glucose in Chinese diabetic population [J]. Chin J Endocrinol Metab. 1988;14(1):3-7.
-
17Yang ZG, Liu L, Liu XY, Ma ZM, Li ZZ. The analysis of diabetic prevalence and the possible risk factors in the residents of community in Yinchuan city [J]. Ningxia Medical Journal. 2009;31(5):38-42.
-
18Cullmann M, Hilding A, Östenson CG. Alcohol consumption and risk of pre-diabetes and type 2 diabetes development in a Swedish population. Diabet Med. 2012;29(4):441-52.
-
19Engler PA, Ramsey SE. Diabetes and alcohol use: detecting at-risk drinking. J Fam Pract. 2011;60(12):E1-6.
Publication Dates
-
Publication in this collection
Oct 2014
History
-
Received
14 Feb 2014 -
Accepted
11 July 2014