Abstracts
The authors report a recent complication during the postoperative period of cataract surgery. A patient was submitted to cataract surgery in both eyes with IOL implantation (Sensar®) inside the capsular bag. The postoperative period of right eye was uneventful, however, in the left eye the patient noted a dark shadow at the temporal visual field at the first postoperative week. This diagnosis was confirmed with the presence of a temporal scotoma revealed by the computerized visual field (first reported in this study) and also reducing the pupil area with miotic drops. The treatment of this complication was performed by using brimonidine tartrate and after 6 months this symptom completely disappeared as confirmed by the computerized visual field. The treatment should be based on reducing the pupil area with miotic drops and we also recommend to observe these cases until the 6th postoperative month before indicating an IOL exchange since the capsular edge that overlaps the IOL may opacify creating an optical barrier reducing or eliminating negative dysphotopsia.
Cataract extraction; Lens implantation, intraocular; Vision disorders; Perimetry; Case reports
Os autores relatam uma complicação no período pós-operatório relativamente recente na cirurgia de catarata. Trata-se de paciente que foi submetido à cirurgia de catarata bilateral não simultânea com implante sacular da lente intra-ocular (Sensar®). O pós-operatório do olho direito evoluiu sem nenhuma queixa, entretanto, no olho esquerdo o paciente referiu a presença de uma sombra em campo visual temporal na primeira semana de pós-operatório sendo diagnosticado disfotopsia negativa após exclusão de outras causas oculares, principalmente retinianas. Este diagnóstico foi confirmado com a presença de um escotoma temporal na campimetria visual computadorizada (relatado na literatura pela primeira vez neste estudo) e também com a redução medicamentosa do tamanho da pupila. Seu tratamento foi realizado com a administração de tartarato de brimonidina e após 6 meses o sintoma desapareceu sendo também documentado com o campo visual (ausência de escotoma). A disfotopsia negativa deve ser tratada visando reduzir a área pupilar e observar por pelo menos 6 meses antes de indicar a troca do lente intra-ocular, uma vez que a cápsula anterior que cobre a LIO pode opacificar criando uma barreira óptica reduzindo ou eliminando esta complicação.
Extração de catarata; Implante de lente intra-ocular; Transtornos da visão; Perimetria; Relatos de casos
RELATOS DE CASOS
Unilateral dysphotopsia after bilateral intraocular lens implantation using the AR40e IOL model: case report
Disfotopsia unilateral após implante bilateral de lente intra-ocular modelo AR40e: relato de caso
Frederico França MarquesI; Daniela Meira Villano MarquesII
IChefe do Setor de Catarata do Complexo Hospitalar Padre Bento de Guarulhos - Guarulhos (SP) - Brasil; Ex-fellow do setor de Catarata do Cincinnati Eye Institute - Ohio - USA; Mestre em Administração na área oftalmológica - MBA e Pós-graduando nível Doutorado pela Universidade Federal de São Paulo - UNIFESP - São Paulo (SP) - Brasil
IIMédica do Setor de Catarata do Departamento de Oftalmologia do Complexo Hospitalar Padre Bento de Guarulhos - Guarulhos (SP) - Brasil; Ex-fellow do setor de Catarata do Cincinnati Eye Institute - Ohio - USA; Mestre em Administração na área oftalmológica - MBA; Pós-graduanda nível Doutorado pela UNIFESP - São Paulo (SP) - Brasil
Endereço para correspondência Endereço para correspondência: Frederico França Marques Rua Arapá, 28 - Apto. 31 São Paulo (SP) CEP 04363-060 E-mail: fredani2010@terra.com.br
ABSTRACT
The authors report a recent complication during the postoperative period of cataract surgery. A patient was submitted to cataract surgery in both eyes with IOL implantation (Sensar®) inside the capsular bag. The postoperative period of right eye was uneventful, however, in the left eye the patient noted a dark shadow at the temporal visual field at the first postoperative week. This diagnosis was confirmed with the presence of a temporal scotoma revealed by the computerized visual field (first reported in this study) and also reducing the pupil area with miotic drops. The treatment of this complication was performed by using brimonidine tartrate and after 6 months this symptom completely disappeared as confirmed by the computerized visual field. The treatment should be based on reducing the pupil area with miotic drops and we also recommend to observe these cases until the 6th postoperative month before indicating an IOL exchange since the capsular edge that overlaps the IOL may opacify creating an optical barrier reducing or eliminating negative dysphotopsia.
Keywords: Cataract extraction/adverse effects; Lens implantation, intraocular/adverse effects; Vision disorders/etiology; Perimetry; Case reports [Publication type]
RESUMO
Os autores relatam uma complicação no período pós-operatório relativamente recente na cirurgia de catarata. Trata-se de paciente que foi submetido à cirurgia de catarata bilateral não simultânea com implante sacular da lente intra-ocular (Sensar®). O pós-operatório do olho direito evoluiu sem nenhuma queixa, entretanto, no olho esquerdo o paciente referiu a presença de uma sombra em campo visual temporal na primeira semana de pós-operatório sendo diagnosticado disfotopsia negativa após exclusão de outras causas oculares, principalmente retinianas. Este diagnóstico foi confirmado com a presença de um escotoma temporal na campimetria visual computadorizada (relatado na literatura pela primeira vez neste estudo) e também com a redução medicamentosa do tamanho da pupila. Seu tratamento foi realizado com a administração de tartarato de brimonidina e após 6 meses o sintoma desapareceu sendo também documentado com o campo visual (ausência de escotoma). A disfotopsia negativa deve ser tratada visando reduzir a área pupilar e observar por pelo menos 6 meses antes de indicar a troca do lente intra-ocular, uma vez que a cápsula anterior que cobre a LIO pode opacificar criando uma barreira óptica reduzindo ou eliminando esta complicação.
Descritores: Extração de catarata/efeitos adversos; Implante de lente intra-ocular/efeitos adversos; Transtornos da visão/etiologia; Perimetria; Relatos de casos [Tipo de publicação]
INTRODUCTION
The intraocular lens (IOL) has been subject of many studies recently in order to provide a better visual acuity for the patient as well as lower incidence of postoperative complications such as posterior capsule opacification. One of these studies concluded that the vertical edge design of the IOL optic zone acts at a mechanical barrier to lenticular cell migration reducing the incidence of posterior capsule opacification when compared with the round edge design(1).
As a consequence of these changes, new postoperative complications related to the image formation at the retina emerged and were named dysphotopsia which can be positive, represented by halos and glare; or negative, with a dark shadow in the temporal visual field. The positive are justified by the reflection of the light at the vertical edge, acting like a mirror creating an irregular and unwanted image; by contrast, the negative are still unknown(2).
This study reports a case of unilateral negative dysphotopsia after uneventful bilateral cataract surgery using the same acrylic IOL with a modified edge (Sensar® AR40e) in both eyes as documented with the help of Humphrey visual field perimetry.
CASE REPORT
A 46 year-old policeman, from São Paulo, presented at this service with the main complaint of blurred vision for the last 6 months in both eyes, also reporting that it got worse when exposed to an environment of bright lights. As ocular past history, he underwent refractive surgery (Lasik) OU four years ago to correct myopic astigmatism (OD = pl 3.25 cyl 15° / OS = pl 2.25 cyl 180°).
Best-corrected visual acuity (BCVA) was 20/30 OD and 20/25 OS. Biomicroscopy of the anterior segment revealed clear corneas with well-positioned flaps, quiet anterior chambers and subcapsular cataracts located at the visual axis 3+/4 OD and 2+/4 OS. During "flash light test" his BCVA was reduced to 20/50 OD and 20/40 OS. Intraocular pressure and indirect ophthalmoscopy were unremarkable OU.
After careful calculation of the keratometry using the history method, ultrasonic biometry was performed using the SRK/T formula with the refraction error planned for emmetropia. The used IOL was Sensar® - AR40e model (AMO) and the power, 19.00 D OD e 20.00 D OS. Both surgeries were performed with an interval of three months starting with OD.
Surgical technique
After a 3.0 mm near clear cornea superior incision, a 1.0 mm paracentesis was performed two clock hours apart. The anterior chamber was refilled with dispersive viscoelastic and a continuous circular capsulotomy was performed with an Utrata forceps. Hydrodissection and hydrodelineation was performed in multiple meridians to free the nucleus and epinucleus. Phacoemusification of the nucleus was done uneventfully using the one-handed technique. After irrigation/aspiration of the cortex, the posterior capsule was cleaned and polished. The IOL was implanted using the Emerald System Injector, and after confirming its centration, with the CCC covering its edge 360 degrees, the viscoelastic was aspirated, stromal edema was performed in the incisions and the watertightness of them was confirmed with a negative Seidel test. During the surgery of the right eye, a positive pressure was noted leading to an iris prolapse during phacoemulsification resulting in a mild focal iris atrophy.
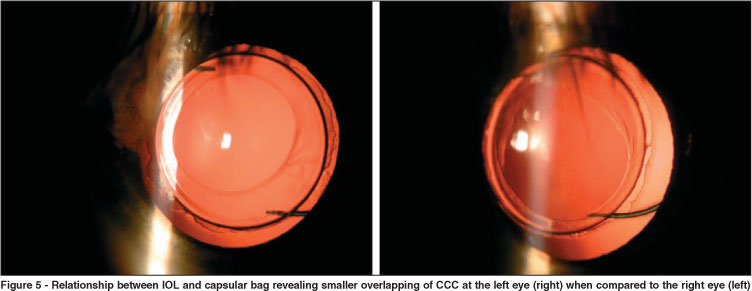
At the immediate postoperative period, the patient was satisfied with uncorrected visual acuity of 20/20 OU. The right eye had an uneventful evolution on the postoperative visits, by contrast, in the left eye, the patient reported on the first postoperative month visit a dark shadow in the temporal visual field, well-characterized by him, although the uncorrected visual acuity remained 20/20 and the IOL was well-positioned with the CCC overlapping its edge 360 degrees (Figure 1).
After excluding corneal flap problems due to the previous refractive surgery and retinal detachment, a negative dysphotopsia was suspected since the implanted IOL had a vertical edge component in its design. In order to confirm the diagnosis, a Humphrey visual field perimetry to document the described dark shadow in the temporal visual field was requested followed by miotic instillation (2% pilocarpine) to reduce the incidence of oblique light rays at the IOL periphery.
The patient returned after one week with the visual field perimetry revealing an absolute scotoma in the superior temporal visual field justifying the patient's symptom (Figure 2); moreover, he also referred an eighty percent (80%) improvement with the miotic therapy.
Once we had all these data, diagnosis of negative dysphotopsia was confirmed and the clinical (miotic) and surgical therapy (IOL exchange) was explained to the patient. Then, we preferred to observe only until the third postoperative month of evolution and the miotic medication was changed after the first week to 0.2% brimonidine tartrate once a day (6:00 PM) since it is well-known to decrease the pupil size under scotopic situations, and it is also well-tolerated when compared with the collateral effects of pilocarpine(3-4).
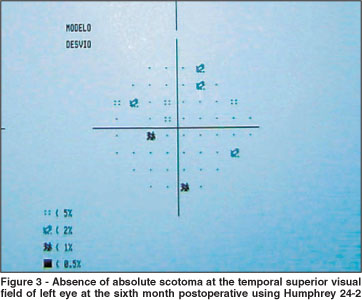
At the third postoperative month, the patient referred a significant improvement with reduction of the dark shadow in the temporal visual field, which improved even more at the 6th month postoperative visit confirmed by visual field perimetry (Figure 3). Biomicroscopy of the anterior segment revealed an increased density at the remaining anterior capsule overlapping the IOL edge. At this point, the patient reported that he spontaneously discontinued the medication. Then, regarding this controlled situation the patient was requested to return every 6 months for control postoperative examinations.
DISCUSSION
The IOL had many improvements since its first implantation performed by Harold Ridley in 1949. Nowadays the intraocular lens has not only the goal to reestablish visual function but also, to avoid postoperative complications such as posterior capsule opacification(1).
After introducing the intraocular lens with square edge the incidence of posterior capsule opacification had a significant reduction due to its new design which led to a mechanical barrier against the lens epithelial cell migration toward the central posterior capsule(1). However, the square edge originated new complications such as unwanted images named dysphotopsia which can be positive, represented by halos and glare, or negative, represented by a dark shadow in the temporal visual field(2).
Problems related to unwanted images at the retina and square edges have been reported a decade ago with the insertion of holes at the optic zone periphery to facilitate its manipulation during implantation(5). These images were described in the investigative phase of CeeOn 911® (Pharmacia Corporation) and also during the use of SA30AL® and SA60AT® (Alcon)(6-9).
These images are due the oblique incidence of light rays that reflects on the square edge of the IOL, similar to a "mirror" effect, creating part of the image at the retina periphery with loss of quality with halos and glare, besides a dark shadow in the temporal visual field, although the mechanism of this last symptom is not well known(10).
Moreover, the round edges have a better light ray distribution over the retina through a significant area leading to a decrease of contrast when compared with square-edge IOLs. Thus, the round edge IOL decreases the intensity of glare of the reflected image reducing the potential for unwanted optic images. By contrast, the square-edge IOLs create a homogeneous image and internally focused through a smaller retina area explaining why the patient does not tolerate it(11).
An increased incidence of this phenomenon in the square-edge IOLs compared to round-edge IOLs was reported(12). When using Acrysof IOL (MA60BM), the incidence of these symptoms in the first postoperative week were 60% to 70% with gradual reduction on the next postoperative visits, however, a small part of these patients remained with this complaint after one month of surgery(13).
In order to reduce these symptoms, new IOL designs were created, such as the "frozen square-edge" proposed by the Acrysof IOL second generation (Alcon) and the "three angulations square-edge" also named Optiedge proposed by Sensar IOL (AMO), which has three different angulations, the anterior is round, the posterior is vertical, and the intermediate is built at 45 degrees between them (Figure 4). By these modifications, a significant loss of light ray reflex at the square edge occurs, resulting in less discomfort for the patient.
After studying all these above described modifications, regarding the effects of the light rays on square-edge IOL, the authors found a three times increased incidence of dysphotopsia in IOLs with frozen edge as compared to IOLs with optiedge(14). However, when comparing the visual discomfort due to glare there was no difference between both groups(15).
Due these adjustments at the IOL edges, the incidence of dysphotopsias decreased, but they were not eliminated being a important cause of IOL exchange, especially in cases where the IOL optic zone is not overlapped by the anterior rim of the capsulorhexis(13).
Aiming to perform a correct diagnosis, it is important to exclude other factors that can modify the correct incidence of the light rays on the retina, such as corneal flap displacement in patients with previous refractive surgery(16), IOL dislocation(17-18), and retina detachment. Once these diagnosis were ruled out, miosis should be attempted since it reduces the oblique incidence of light rays improving the patient's symptom besides confirming the dysphotopsia diagnosis.
In this case, Humphrey visual field perimetry was efficient to establish the diagnosis as well as to follow-up the improvement of the symptom reported by the patient revealing the absolute scotoma in the superior temporal visual field and its regression during the postoperative period.
Regarding the treatment of dysphotopsia, the use of miotic eyedrops (2% pilocarpine) presents limited results due its collateral effects such as myopic shift and cystoid macular edema, however the use of 0.2% brimonidine tartrate helps to inhibit the physiologic mydriasis leading to a smaller pupil area being a very useful medication in this case(3-4). Another recommended alternative in cases where capsulotomy overlaps the IOL optic edge is to wait since the development of fibrosis and its adherence to the anterior capsule, create an optical barrier reducing the incidence of oblique light rays on the IOL edge(13-14).
In our case, although the same IOL model was implanted in the capsular bag in both eyes with good centration and consequently a good uncorrected visual acuity, these symptoms were referred only in OS. The reason of the exact formation of the negative dysphotopsia (dark shadow in the temporal visual field) in some patients with square-edge IOL remains still unknown, although we know that the incidence of oblique light rays plays an important role in its development, as well as it is the main cause of the positive dysphotopsia. However, the use of the visual field perimetry in this case (Humphrey 24-2) which analyzes 24° in the temporal visual field demonstrated that this scotoma at the retina is not so peripheral.
Our hypothesis to explain the unilateral manifestation in this case is the presence of a subtle difference in the CCC size which is larger in OS, and as a result, leading to a larger area of the IOL square edge being exposed to the oblique light rays (Figure 5). The use of a miotic to confirm the diagnosis and an observational management were very useful in this case since the opacification of the anterior capsule created by the fibrosis generated an optic barrier with gradual improvement of the symptom reported by the patient.
CONCLUSION
In the presence of square-edge IOLs, the dysphotopsias were incorporated in the group of cataract surgery postoperative complications, specially, the negative ones with a dark shadow in the temporal visual field. Thus, it is crucial that the cataract surgeon recognizes its symptoms, and knows how to make the diagnosis and to treat it. The use of visual field perimetry demonstrated to be efficient not only to confirm the diagnosis but also to follow-up its regression during the postoperative period.
The treatment can be performed with miotics to reduce the pupil area associated with an observational or surgical management with an IOL exchange for one with a round edge. When the CCC overlaps the IOL optic zone, it is prudent to observe between 3 and 6 months, since an optical barrier has an increased chance to be created by the fibrosis reducing or eliminating the patient's discomfort.
Recebido para publicação em 15.03.2006
Última versão recebida em 28.08.2006
Aprovação em 06.09.2006
Nota Editorial: Depois de concluída a análise do artigo sob sigilo editorial e com a anuência do Dr. Francisco Porfírio Neto Jr. sobre a divulgação de seu nome como revisor, agradecemos sua participação neste processo.
Trabalho realizada no Departamento de Oftalmologia da Universidade Federal de São Paulo - UNIFESP - São Paulo (SP) - Brasil.
- 1. Nishi O, Nishi K. Preventing posterior capsule opacification by creating a discontinuous sharp bend in the capsule. J Cataract Refract Surg. 1999;25(4):521-6.
- 2. Davison JA. Positive and negative dysphotopsia in patients with acrylic intraocular lenses. J Cataract Refract Surg. 2000;26(9):1346-55.
- 3. McDonald JE 2nd, El-Moatassem Kotb AM, Decker BB. Effect of brimonidine tartrate ophthalmic solution 0.2% on pupil size in normal eyes under different luminance conditions. J Cataract Refract Surg. 2001;27(4):560-4.
- 4. Poinoosawmy D, Nagasubramanian S, Brown NA. Effect of pilocarpine on visual acuity and on the dimensions of the cornea and anterior chamber. Br J Ophthalmol. 1976;60(10):676-9.
- 5. Waller S, Steinert RF. Symptomatic intraocular reflections from oval intraocular lens implants. Am J Ophthalmol. 1993;116(3):374-6.
- 6. Masket S. Truncated edge design, dysphotopsia, and inhibition of posterior capsule opacification. J Cataract Refract Surg. 2000;26(1):145-7.
- 7. Davison JA. Clinical performance of Alcon SA30AL and SA60AT single-piece acrylic intraocular lenses. J Cataract Refract Surg. 2002;28(7):1112-23.
- 8. Davison JA. Explanting the AcrySof single-piece IOL. EyeWorld. 2001;6:67.
- 9. Izak AM, Werner L, Pandey SK, Apple DJ, Vargas LG, Davison JA. Single-piece hydrophobic acrylic intraocular lens explanted within the capsular bag: case report with clinicopathological correlation. J Cataract Refract Surg. 2004; 30(6):1356-61.
- 10. Coroneo MT, Pham T, Kwok LS. Off-axis edge glare in pseudophakic dysphotopsia. J Cataract Refract Surg. 2003;29(10):1969-73.
- 11. Holladay JT, Lang A, Portney V. Analysis of edge glare phenomena in intraocular lens edge designs. J Cataract Refract Surg. 1999;25(6):748-52.
- 12. Tester R, Pace NL, Samore M, Olson RJ. Dysphotopsia in phakic and pseudophakic patients: incidence and relation to intraocular lens type(2). J Cataract Refract Surg. 2000;26(6):810-6.
- 13. Dewey SH. Square-edge IOLs Part II: Dysphotopsia. Cataract Refract Surg Today [serial on the Internet]. 2002 [cited 2005 Jun 6]; (April):[about 5 p.]. Available from: http://www.crstodayarchive.com/03_archive/0402/crst0402_06.html
- 14. Franchini A, Gallarati BZ, Vaccari E. Analysis of stray-light effects related to intraocular lens edge design. J Cataract Refract Surg. 2004;30(7):1531-6.
- 15. Hayashi K, Hayashi H. Effect of a modified optic edge design on visual function: textured-edge versus round-anterior, slope-side edge. J Cataract Refract Surg. 2004;30(8):1668-74.
- 16. Pande M, Hillman JS. Optical zone centration in keratorefractive surgery. Entrance pupil center, visual axis, coaxially sighted corneal reflex, or geometric corneal center? Ophthalmology. 1993;100(8):1230-7.
- 17. Mamalis N, Spencer TS. Complications of foldable intraocular lenses requiring explantation or secondary intervention - 2000 survey update. J Cataract Refract Surg. 2001;27(8):1310-7.
- 18. Birchall W, Brahma AK. Eccentric capsulorhexis and postoperative dysphotopsia following phacoemulsification. J Cataract Refract Surg. 2004;30(6):1378-81.
Endereço para correspondência:
Publication Dates
-
Publication in this collection
19 June 2007 -
Date of issue
Mar 2007
History
-
Reviewed
28 Aug 2006 -
Received
15 Mar 2006 -
Accepted
06 Sept 2006