ABSTRACT
We report a case of ocular sarcoidosis with positive immunoglobulin (Ig) M and IgG serology for toxoplasmosis. The patient was a young female with red painful eyes, bilateral eyelid edema, and panuveitis with periphlebitis. In laboratory testing, she was IgM and IgG positive for toxoplasmosis and anergic in the tuberculin test. Topical treatment for anterior uveitis and oral antibiotics for toxoplasmosis were started, without improvement. Orbit tomography showed increased lacrimal glands bilaterally, and chest X-ray radiographic findings were consistent with pulmonary sarcoidosis, which supported the presumed ocular sarcoidosis diagnosis. The patient was treated with oral prednisone and methotrexate without antibiotics. She showed clinical and vision improvement without recurrences during the 1-year follow-up. Ocular sarcoidosis is an important differential diagnosis requiring careful anamnesis and ophthalmological examinations. Ancillary tests, such as X-ray radiography, tomography, and clinical and laboratory evaluations may help rule out other causes. Treatment mainly consists of corticosteroids and immunosuppression.
Keywords:
Sarcoidosis; Toxoplasmosis, ocular; Uveitis, posterior; Eye diseases
RESUMO
Relatamos um caso de sarcoidose ocular com IgM e IgG positivos para toxoplasmose. Mulher jovem com quadro ocular bilateral de dor, vermelhidão, edema palpebral e panuveíte com periflebite. Os testes laboratoriais mostraram IgM e IgG positivos para toxoplasmose, teste tuberculínico anérgico. Realizou-se tratamento tópico da uveíte anterior e antibióticos orais para toxoplasmose, sem melhora. Tomografia de órbita mostrou aumento das glândulas lacrimais bilaterais e radiografia de tórax foi consistente com sarcoidose pulmonar, auxiliando no diagnóstico de sarcoidose ocular presumida. Iniciou-se prednisona e metotrexato orais, sem antibióticos, com melhora clínica e oftalmológica, sem recidivas em 1 ano de follow-up. Sarcoidose ocular é um importante diagnóstico diferencial que exige anamnese e exame oftalmológico cuidadosos. Exames complementares, como raio-X, tomografia computadorizada e avaliação clínica e laboratorial ajudam na avaliação e exclusão de outras causas. O tratamento consiste principalmente no uso de corticosteróide e imunossupressores.
Descritores:
Sarcoidose; Toxoplasmose ocular; Uveíte posterior; Oftalmopatias
INTRODUCTION
Sarcoidosis is a systemic inflammatory disease that mainly affects Afro-descendant women 20-50 years old. The lungs are the most damaged organs (90%), followed by the eyes, skin, and liver. Ocular involvement occurs in 25%-80% of patients. Although anterior uveitis is the most common ocular manifestation, 28% of patients present with posterior uveitis, especially with venous involvement(11 Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509-16. Review.
2 Spagnolo P. Sarcoidosis: a critical review of history and milestones. Clin Rev Allergy Immunol. 2015;49(1):1-5.
3 Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357(21):2153-65.-44 Birnbaum AD, Rifkin LM. Sarcoidosis: sex-dependet variations in presentation and management. J Ophthalmol. 2014;2014:236905.).
We present a case of a patient who had bilateral posterior uveitis with vasculitis due to sarcoidosis and who was IgM positive for toxoplasmosis, which made early diagnosis difficult.
CASE REPORT
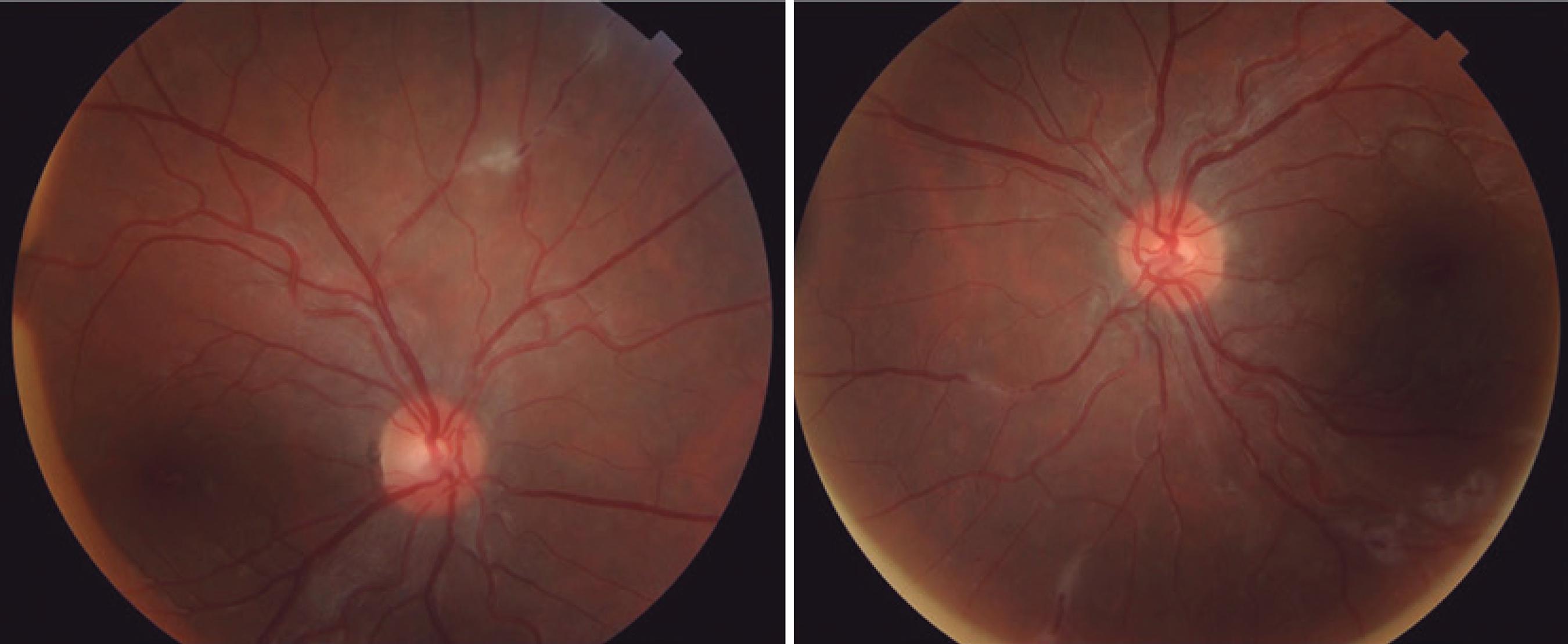
A 27-year-old Afro-descendant woman complained of headache, asthenia, night fever, and bilateral painful upper eyelid edema for 2 months. She also had bilateral ocular pain for 7 days. Her personal and familial past histories were unremarkable. Her best-corrected visual acuity (BCVA) was 20/20 in both eyes (OU). She presented with bilateral superior temporal eyelid edema, and anterior biomicroscopy revealed conjunctival injection and anterior chamber cells 3+(11 Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509-16. Review.), without other alterations in OU. The intraocular pressure was normal in OU, and fundoscopy showed vascular sheathing, mainly venous, with candle wax drippings sign in OU, and intraretinal hemorrhages in the left eye (OS) (Figure 1). Testing showed positive serology for to xoplasmosis detected by immunoenzymatic enzyme-linked immunosorbent assay (IgG >650 and IgM= 2.78), anergic PPD, but no other laboratory abnormalities. Fluorescein angiography showed perivascular hyperfluorescence by leakage (Figure 2).
Retinography showing areas of venous vascular sheathing and candle wax drippings sign in both eyes. OD in the right and OS in the left.
Fluorescein angiography showing hyperfluorescence areas through leakage and capillaritis in both eyes. OD in the right and OS in the left.
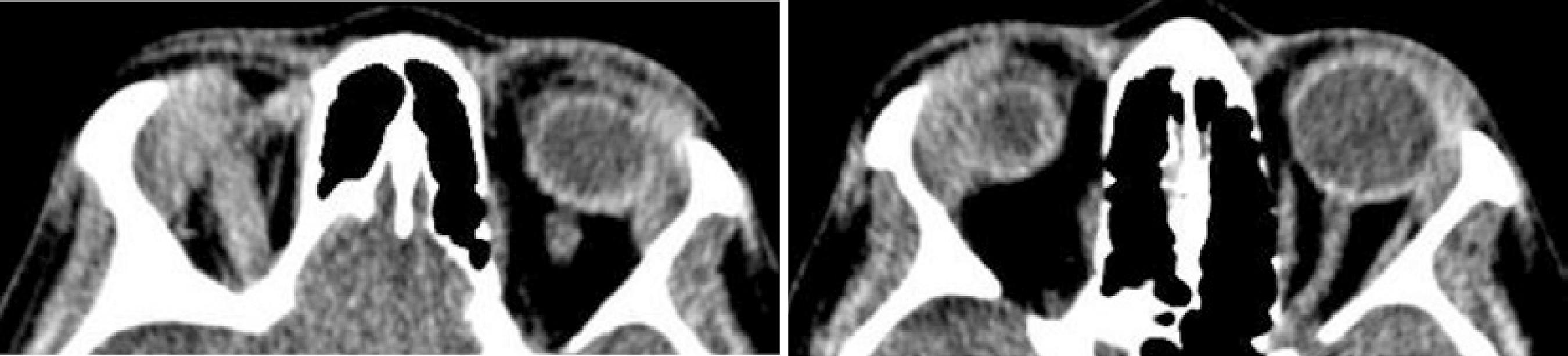
Empirical treatment for ocular toxoplasmosis was started (oral sulfamethoxazole + trimethoprim 800/160 mg 1 pill twice a day and oral prednisone 1 mg/kg/day in regression 20 mg every 3 days) as well as topical treatment with prednisolone acetate 1% and tropicamide 1% drops in OU. After 3 weeks, the patient returned with improvement of systemic symptoms and bipalpebral edema but with worsening of retinal vasculitis in OU. Computed tomography (CT) of the orbit showed a bilateral increase in lacrimal glands (Figure 3), and chest X-ray radiography showed increased hilar lymph nodes and some pulmonary infiltrates, signs that were consistent with the diagnosis of pulmonary sarcoidosis stage II. The diagnosis of presumed ocular sarcoidosis was made. Antibiotics were discontinued and slowly regressive oral prednisone 1 mg kg-1day-1 and methotrexate were started. The patient showed clinical improvement, and after 1 year of follow-up, she presented without systemic or ocular complaints, with a BCVA of 20/20 in OU. Ocular examinations subsequently showed that she continued to exhibit sporadic small areas of vasculitis in OU, without other complications.
DISCUSSION
Sarcoidosis presents with non-caseating granulomas with epithelioid cells in various tissues, but the etiology is unknown. The estimated incidence is approximately 15-21 per 100,000 habitants, and the prevalence is 1-40 per 100,000 habitants. The disease usually, affects people between 20 and 50 years of age, with a slight predominance in Afro-descendants and women. The course and manifestations of the disease vary depending on age, sex, race, and the affected organs. The disease can affect the entire body, mainly the lungs (90%) but also the eyes, skin, liver, spleen, central nervous system, cardiovascular system, kidneys, bones, and ligaments(22 Spagnolo P. Sarcoidosis: a critical review of history and milestones. Clin Rev Allergy Immunol. 2015;49(1):1-5.
3 Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357(21):2153-65.
4 Birnbaum AD, Rifkin LM. Sarcoidosis: sex-dependet variations in presentation and management. J Ophthalmol. 2014;2014:236905.-55 Jamilloux Y, Kodjikian L, Broussolle C, Sève P. Sarcoidosis and uveitis. Autoimmun Rev. 2014;13(8):840-9.).
Ocular sarcoidosis occurs in up to 50% of patients and affects the lacrimal glands, orbit, eyelids, conjunctiva, cornea, sclera, retina, choroids, and optic nerve. Sarcoidosis is the cause of 2%-15% of all uveitis and is characterized by bilateral involvement (80%-90%) and a symmetrical clinical course. Anterior uveitis is the most common presentation (41%-75%), with classically chronic, bilateral, granuloma tous keratic precipitates, iris nodules, and anterior and posterior synechia. However, non-granulomatous uveitis is two times more common than the granulomatous type. Posterior uveitis is observed in 28% of cases, usually with extensive venous vascular sheathing (periphle bitis) and perivenous infiltrates (candle wax drippings sign), which can cause branch retinal venous occlusion and retinal ischemia and lead to neovascularization and vitreous hemorrhage. Other ocular complications include band keratopathy, glaucoma, and cataracts. Intermediate uveitis (6%-10%) and panuveitis (9%-33%) may occur(55 Jamilloux Y, Kodjikian L, Broussolle C, Sève P. Sarcoidosis and uveitis. Autoimmun Rev. 2014;13(8):840-9.). There also may be orbital and annexes involvement, mainly in women and the elderly. The lacrimal gland is affected in 42% of patients and manifests as gland increase and dry-eye symptoms, and orbital invol vement presents with proptosis, diplopia, ophthalmoparesis and decreased vision(55 Jamilloux Y, Kodjikian L, Broussolle C, Sève P. Sarcoidosis and uveitis. Autoimmun Rev. 2014;13(8):840-9.,66 Prabhakaran VC, Saeed P, Esmaeli B, Sullivan TJ, McNab A, Davis G, et al. Orbital and adnexal sarcoidosis. Arch Ophthalmol. 2007;125(12):1657-62.).
Because of its different clinical manifestations, the diagnosis of ocular sarcoidosis is difficult and made by exclusion. Chest radiogra phy is altered in 90% of cases and is considered the best initial exami nation. Classically, ocular sarcoidosis presents with bilateral hilar lymphadenopathy but can also demonstrate parenchymal opacities or pleural involvement. Chest CT is indicated in cases of negative radiography and high suspicion of the disease. Laboratory tests, such as angiotensin-converting enzyme, lysozyme, and calcium metabolism, may be used but are not specific and are often normal. The tuberculin skin test (purified protein derivative skin test) is usually anergic. Definitive diagnosis is made by histopathological analyses showing non-ca seating epithelioid granuloma in the biopsy of affected organs (lung, mediastinal lymph nodes, skin, liver, conjunctiva, salivary, or lacrimal glands). The International Ocular Sarcoidosis Workshop graduates the sarcoidosis diagnosis as definitive (biopsy result), presumed (typical ocular findings associated with hilar lymphadenopathy), probable (ocular signs and compatible laboratory tests without hilar adenopathy), and possible (eye and laboratory findings compatible but negative biopsy)(33 Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357(21):2153-65.,55 Jamilloux Y, Kodjikian L, Broussolle C, Sève P. Sarcoidosis and uveitis. Autoimmun Rev. 2014;13(8):840-9.,77 Heinle R, Chand C. Diagnostic criteria for sarcoidosis. Autoimmun Rev. 2014;13(4-5): 383-7.,88 Read RW. Intraocular inflammation and uveitis. Basic and Clinical Science Course: section 9. American Academy of Ophthalmology; 2014. p.172-7. Available from: http://ebooks.aao.org/product/20152016-basic-clinical-science-course-section-09-intraocular-inflammation-uveitis-ebook-print
http://ebooks.aao.org/product/20152016-b...
).
Our case is interesting because the patient had clinical features consistent with sarcoidosis (young Afro-descendent woman with bilateral ocular periphlebitis and lacrimal gland involvement) but also had positive serology for toxoplasmosis (IgG and IgM). Since Brazil is an endemic country for toxoplasmosis, we decided to start empirical treatment of this infection, despite the suspicion of sarcoidosis. However, the patient did not show improvement in all of her signs, so we decided to continue the clinical investigation. The diagnosis of presumed ocular sarcoidosis was supported by imaging tests and pulmonologist evaluation.
Treatment for ocular sarcoidosis currently involves administration of systemic corticosteroids. Topical therapy (corticosteroids and mydriatics) is administered in addition to systemic corticosteroids in cases of anterior uveitis. Intravitreal corticosteroids may also be used in posterior uveitis with oral therapy intolerance. Immunosuppressive agents can be added to minimize steroid use and control inflammation, with methotrexate being the preferred choice. Approximately 10% of cases lead to blindness, especially because of development of cystoid macular edema and retinal neovascularization(55 Jamilloux Y, Kodjikian L, Broussolle C, Sève P. Sarcoidosis and uveitis. Autoimmun Rev. 2014;13(8):840-9.,88 Read RW. Intraocular inflammation and uveitis. Basic and Clinical Science Course: section 9. American Academy of Ophthalmology; 2014. p.172-7. Available from: http://ebooks.aao.org/product/20152016-basic-clinical-science-course-section-09-intraocular-inflammation-uveitis-ebook-print
http://ebooks.aao.org/product/20152016-b...
).
CONCLUSION
Although ocular sarcoidosis is a difficult diagnosis, the disease should always be considered in patients with uveitis. Because of its wide diversity of clinical signs and symptoms, the disease requires careful anamnesis and ophthalmological examination. Ancillary tests, such as X-ray radiography, chest and orbital CT, and clinical and laboratory evaluation help in ruling out other causes. Despite the importance of these ancillary tests, clinical evaluation remains imperative, as demonstrated in our case. The treatment consists mainly of oral corticosteroids and immunosuppression.
-
Funding: No specific financial support was available for this study.
REFERENCES
-
1Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509-16. Review.
-
2Spagnolo P. Sarcoidosis: a critical review of history and milestones. Clin Rev Allergy Immunol. 2015;49(1):1-5.
-
3Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357(21):2153-65.
-
4Birnbaum AD, Rifkin LM. Sarcoidosis: sex-dependet variations in presentation and management. J Ophthalmol. 2014;2014:236905.
-
5Jamilloux Y, Kodjikian L, Broussolle C, Sève P. Sarcoidosis and uveitis. Autoimmun Rev. 2014;13(8):840-9.
-
6Prabhakaran VC, Saeed P, Esmaeli B, Sullivan TJ, McNab A, Davis G, et al. Orbital and adnexal sarcoidosis. Arch Ophthalmol. 2007;125(12):1657-62.
-
7Heinle R, Chand C. Diagnostic criteria for sarcoidosis. Autoimmun Rev. 2014;13(4-5): 383-7.
-
8Read RW. Intraocular inflammation and uveitis. Basic and Clinical Science Course: section 9. American Academy of Ophthalmology; 2014. p.172-7. Available from: http://ebooks.aao.org/product/20152016-basic-clinical-science-course-section-09-intraocular-inflammation-uveitis-ebook-print
» http://ebooks.aao.org/product/20152016-basic-clinical-science-course-section-09-intraocular-inflammation-uveitis-ebook-print
Publication Dates
-
Publication in this collection
Mar-Apr 2017
History
-
Received
26 Aug 2016 -
Accepted
18 Nov 2016