Abstracts
CONTEXT:The incidence of hepatic hemangiomas ranges from 0.4% to 20% in the general population. Conventional ultrasound is usually the first diagnostic method to identify these hemangiomas, typically as an incidental finding. Ultrasonography with second generation contrast materials is being used in various areas of hepatology, yielding similar results to those obtained with computerized tomography and magnetic resonance imaging in the diagnosis of hepatic hemangiomas. OBJECTIVE: To evaluate the agreement between ultrasound with perflutrene contrast and magnetic resonance imaging in the diagnosis of hepatic hemangiomas. METHODS: A total of 37 patients were prospectively examined between January 2006 and August 2008. A total of 57 hepatic nodules were documented in this group as incidental findings on routine ultrasound exams. The 37 patients were administered perflutrene contrast without adverse reactions, and were all submitted to magnetic resonance exams. RESULTS: Conventional ultrasound identified 15 patients with nodules typical of hemangiomas and 22 patients with other nodules. In 35 patients, the contrast characteristics were consistent with hepatic hemangiomas. CONCLUSION: Agreement between the data obtained from ultrasound with contrast and magnetic resonance was 94.5%. In discordant cases, the magnetic resonance diagnosis prevailed. In the case which presented indeterminate findings on contrast ultrasonography, magnetic resonance was repeated after 3 months, confirming the diagnosis of a hepatic hemangioma. A biopsy was performed on the suspected malignant nodule which also confirmed the presence of a hepatic hemangioma. Ultrasonography with contrast has the advantages of being more accessible to the public at large and lower cost than magnetic resonance. The results of our study highlight the need for a new protocol in hepatic nodules incidentally identified on conventional ultrasonography. In the case of typical hemangiomas, conventional ultrasound is sufficient for diagnosis. However, for poorly defined nodules, ultrasonography with contrast is indicated. After confirming the presence of a hepatic hemangioma on contrast ultrasonography, no further exams are needed to finalize the diagnosis.
Hemangioma; Liver diseases; Ultrasonography; Contrast media; Magnetic resonance spectroscopy
CONTEXTO: O hemangioma hepático apresenta incidência entre 0,4% a 20% na população e a ultrassonografia convencional é geralmente o primeiro método diagnóstico a identificá-lo como achado incidental. A ultrassonografia com contrastes de segunda geração vem sendo utilizada em várias áreas da hepatologia, com resultados semelhantes à tomografia computadorizada e a ressonância magnética no diagnóstico dos hemangiomas hepáticos. OBJETIVO: Avaliar a concordância entre a ultrassonografia com o contraste perflutreno e a ressonância magnética no diagnóstico dos hemangiomas hepáticos. MÉTODOS: Foram analisados prospectivamente 37 pacientes entre janeiro de 2006 e agosto de 2008 e identificados 57 nódulos como achados incidentais de exame de ultrassom de rotina. Nos 37 pacientes, foi administrado o contraste perflutreno, sem reações adversas. Os 37 pacientes realizaram exames de ressonância magnética. RESULTADOS: A ultrassonografia convencional identificou em 15 pacientes nódulos com características típicas de hemangiomas e em 22 pacientes com nódulos com outras características Em 35 pacientes as características do contraste foram compatíveis com hemangiomas hepáticos. CONCLUSÕES: A concordância entre a ultrassonografia com contraste e a ressonância magnética foi de 94,5% e nos casos discordantes o diagnóstico foi realizado pela ressonância magnética. No caso indeterminado na ultrassonografia com contraste, a ressonância magnética foi repetida em 3 meses, confirmando o diagnostico de hemangioma hepático. No caso com nódulo sugestivo de malignidade na ultrassonografia com contraste, foi realizada biopsia do nódulo, com anatomopatológico de hemangioma hepático. A ultrassonografia com contraste apresenta vantagens de maior acesso a população e custos menores em relação à ressonância magnética. Os resultados deste trabalho sugerem novo protocolo para nódulos hepáticos identificados incidentalmente em exames de ultrassonografia convencional. Nos hemangiomas típicos, a ultrassonografia convencional seria suficiente. Nos casos com nódulos não definidos, a ultrassonografia com contraste a ser indicado, que ao confirmar o diagnóstico de hemangioma hepático, encerraria a instigação diagnóstica.
Hemangioma; Hepatopatias; Ultrassonografia; Meios de contraste; Espectroscopia de ressonância magnética
ORIGINAL ARTICLE
Prospective study of ultrasound with perflutrene contrast compared to magnetic resonance imaging in the diagnosis of hepatic hemangiomas
Estudo prospectivo comparando a ultrassonografia com o contraste perflutreno e a ressonância magnética no diagnóstico de hemangiomas hepáticos
Joel SchmillevitchI; Luiz Arnaldo SzutanII; Fábio Gonçalves FerreiraII; Maria de Fátima SantosII; Ricardo MincisIII; Ana GorskiIV
IDepartment of Surgery, Faculty of Medical Sciences, Santa Casa of São Paulo (FCM - SCSP)
IILiver and Portal Hypertension Group of the Department of Surgery, FCM - SCSP
IIIFaculty of Medical Sciences of Santos, SP
IVDirector of the Schmillevitch Diagnostics Centre, São Paulo, SP, Brasil
Correspondence Correspondence: Dr. Joel Schmillevitch Rua Brasilio Machado, 444 Santa Cecília - 01230 010 São Paulo, SP, Brasil E-mail: joel@schmillevitch.com.br
ABSTRACT
CONTEXT:The incidence of hepatic hemangiomas ranges from 0.4% to 20% in the general population. Conventional
ultrasound is usually the first diagnostic method to identify these hemangiomas, typically as an incidental finding. Ultrasonography with second generation contrast materials is being used in various areas of hepatology, yielding similar results to those obtained with computerized tomography and magnetic resonance imaging in the diagnosis of hepatic hemangiomas.
OBJECTIVE: To evaluate the agreement between ultrasound with perflutrene contrast and magnetic resonance imaging in the diagnosis of hepatic hemangiomas.
METHODS: A total of 37 patients were prospectively examined between January 2006 and August 2008. A total of 57 hepatic nodules were documented in this group as incidental findings on routine ultrasound exams. The 37 patients were administered perflutrene contrast without adverse reactions, and were all submitted to magnetic resonance exams.
RESULTS: Conventional ultrasound identified 15 patients with nodules typical of hemangiomas and 22 patients with other nodules. In 35 patients, the contrast characteristics were consistent with hepatic hemangiomas.
CONCLUSION: Agreement between the data obtained from ultrasound with contrast and magnetic resonance was 94.5%. In discordant cases, the magnetic resonance diagnosis prevailed. In the case which presented indeterminate findings on contrast ultrasonography, magnetic resonance was repeated after 3 months, confirming the diagnosis of a hepatic hemangioma. A biopsy was performed on the suspected malignant nodule which also confirmed the presence of a hepatic hemangioma. Ultrasonography with contrast has the advantages of being more accessible to the public at large and lower cost than magnetic resonance. The results of our study highlight the need for a new protocol in hepatic nodules incidentally identified on conventional ultrasonography. In the case of typical hemangiomas, conventional ultrasound is sufficient for diagnosis. However, for poorly defined nodules, ultrasonography with contrast is indicated. After confirming the presence of a hepatic hemangioma on contrast ultrasonography, no further exams are needed to finalize the diagnosis.
Headings: Hemangioma. Liver diseases. Ultrasonography. Contrast media. Magnetic resonance spectroscopy.
RESUMO
CONTEXTO: O hemangioma hepático apresenta incidência entre 0,4% a 20% na população e a ultrassonografia convencional é geralmente o primeiro método diagnóstico a identificá-lo como achado incidental. A ultrassonografia com contrastes de segunda geração vem sendo utilizada em várias áreas da hepatologia, com resultados semelhantes à tomografia computadorizada e a ressonância magnética no diagnóstico dos hemangiomas hepáticos.
OBJETIVO: Avaliar a concordância entre a ultrassonografia com o contraste perflutreno e a ressonância magnética no diagnóstico dos hemangiomas hepáticos.
MÉTODOS: Foram analisados prospectivamente 37 pacientes entre janeiro de 2006 e agosto de 2008 e identificados 57 nódulos como achados incidentais de exame de ultrassom de rotina. Nos 37 pacientes, foi administrado o contraste perflutreno, sem reações adversas. Os 37 pacientes realizaram exames de ressonância magnética.
RESULTADOS: A ultrassonografia convencional identificou em 15 pacientes nódulos com características típicas de hemangiomas e em 22 pacientes com nódulos com outras características Em 35 pacientes as características do contraste foram compatíveis com hemangiomas hepáticos.
CONCLUSÕES: A concordância entre a ultrassonografia com contraste e a ressonância magnética foi de 94,5% e nos casos discordantes o diagnóstico foi realizado pela ressonância magnética. No caso indeterminado na ultrassonografia com contraste, a ressonância magnética foi repetida em 3 meses, confirmando o diagnostico de hemangioma hepático. No caso com nódulo sugestivo de malignidade na ultrassonografia com contraste, foi realizada biopsia do nódulo, com anatomopatológico de hemangioma hepático. A ultrassonografia com contraste apresenta vantagens de maior acesso a população e custos menores em relação à ressonância magnética. Os resultados deste trabalho sugerem novo protocolo para nódulos hepáticos identificados incidentalmente em exames de ultrassonografia convencional. Nos hemangiomas típicos, a ultrassonografia convencional seria suficiente. Nos casos com nódulos não definidos, a ultrassonografia com contraste a ser indicado, que ao confirmar o diagnóstico de hemangioma hepático, encerraria a instigação diagnóstica.
Descritores: Hemangioma. Hepatopatias. Ultrassonografia. Meios de contraste. Espectroscopia de ressonância magnética.
INTRODUCTION
Hemangiomas are the most common benign congenital tumor of the liver with an incidence ranging from 0.4% to 20% at autopsy(8, 9) and are more frequent in women. It is classified as a congenital vascular malformation or hamartoma.
Conventional ultrasonography (US) is the imaging method routinely used for abdominal examinations given its lack of side effects, low cost and general availability (Figure 1). The identification of hepatic nodules as an incidental finding is common (incidentalomas)(5). This method has low specificity in the differential diagnosis of hepatic nodules, while colored Doppler does not detect vascularization in the majority of hepatic hemangiomas(11).
Computerized tomography (CT) and magnetic resonance (MR) are the imaging methods used to diagnose hepatic hemangiomas, both of which entail the use of contrast agents(2, 4, 7).
Contrasts for use in ultrasonography have been undergoing development since 1968 and the latest contrasts, considered second generation, are used in more than 60 countries(15, 16).
The color Doppler ultrasound (US) first used in US exams with contrast yielded unsatisfactory results due to artifacts in the images and the fact that balls of dye disappeared rapidly.
The pulse inverted harmonics and low mechanical index employed in today's US technologies allow for real-time characterization of mediums in contrast without colored Doppler(15, 22).
US exams using contrast produce mild side effects in a small number of patients(17, 19). The diagnostic concordance between contrast US and magnetic resonance MR is over 90% in the diagnosis of hepatic hemangiomas(4).
In spite of numerous studies, the true value of contrast ultrasound has not yet been clearly defined in our milieu.The aim of this study was to evaluate the concordance between contrast ultrasound and magnetic resonance MR in the diagnosis of hepatic hemangiomas.
METHODS
A total of 37 patients were prospectively analyzed between January 2006 and August 2008. Twelve of these patients were seen at the Hospital Irmandade da Santa Casa de Misericórdia de São Paulo, SP, Brazil and the remainder (25) at the Schmillevitch Diagnostics Centre, São Paulo, SP. Of the 37 patients, 28 (75.67%) subjects were women and 9 (24.33%) men, with a mean age of 42.3 years.
Patients were recruited by the Irmandade da Santa Casa de Misericórdia de São Paulo Hospital and the Schmillevitch Diagnostics Center and included cases with hepatic nodules as an incidental finding on conventional abdominal ultrasound exams.
Fifty seven nodules were documented as incidental findings on routine ultrasound exam in patients without cancer or chronic hepatopathy. Nodules measured between 0.8 cm and 22 cm across.
The diagnostic criteria for a typical hemangioma on conventional US were: solitary, circumscribed, hyperechoic nodule, with both dimensions less than 4 cm(14). The 37 patients first underwent US with contrast followed by MR in a double-blind study design.
US with perflutrene contrast was performed using equipment from Medison (South Korea) model SA 9900 with inverse pulse harmonics and low mechanical index (0.04 to 0.1) and a 3.5 MHz transducer.
Contrast was given by intravenous bolus injection of 0.5 mL of dye into a peripheral arm vein in all patients, followed by 10 mL of 0.9% saline solution.
An additional dose of contrast was used in two patients with four and five nodules, respectively.
No adverse contrast reactions were seen in any of the patients.
The contrast US exam was split into three phases for analysis:
a) arterial phase of approximately 10 to 30 seconds;
b) portal phase of approximately 30 to 90 seconds;
c) late phase of approximately 90 to 120 seconds.
The exam was photographed and recorded on digital video discs, and lasted between 10 to 15 minutes.
Of the 37 patients, 24 underwent ultrasound exam with contrast immediately after US, and 13 patients from 3 to 10 days after US.
The author acquired the contrast and all exams were performed free of charge.
MR imaging exams were done on 1.0 or 1.5 Tesla devices, within 2 to 32 days of the conventional US exam. The protocol for diagnosis of hepatic hemangioma included T1 and T2 weighted analysis, and administration of extracellular gadolinium with and without fat saturation(6).
All patients signed an informed consent and the study was approved by the Research Ethics Committee of the Hospital Irmandade da Santa Casa de Misericórdia de São Paulo, SP, Brazil (protocol no. 500/07).
RESULTS
Conventional US identified 23 patients with solitary nodules and 14 patients with multiple nodules. Of these 57 nodules, 27 were hyperechoic and 30 were hypoechoic.
Fifteen patients had nodules with typical characteristics of hepatic hemangiomas, while 22 had atypical nodules(10).
All of the 30 hypoechoic nodules had correlation with varying degrees of diffuse hepatic steatosis (Figure 2).
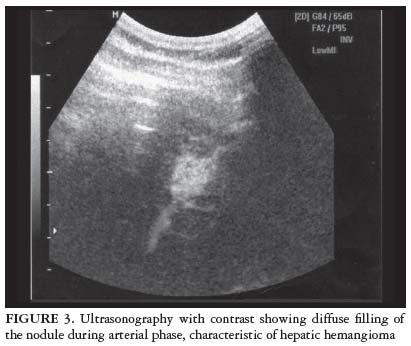
After the administration of perflutrene contrast, within a few seconds, peripheral enhancement of the hepatic nodules revealed progressive centripetal filling in the arterial phase. In nodules less than 2 cm in size, filling by contrast was diffuse (Figure 3).
In the venous and late phases, filling by contrast of nodules greater than 2 cm, was partial or total whereas for nodules measuring less than 2 cm, the filling pattern remained diffuse or unaltered (Figure 4).
Findings for US with contrast in 35 patients were consistent with hepatic hemangiomas (Table 1).
One patient with a single nodule presented no contrast enhancement for all the three phases of the exam (indeterminate).
In one patient with a solitary nodule measuring 5.2 cm by 4.0 cm, leakage of contrast was observed in the venous and late phases (washout), characteristic of a malignant tumor.
The exam was painless and there were no adverse reactions in any of the 37 patients.
A total of 60 nodules were detected on MR, 3 of which measured less than 1 cm across and were not detected by US.
The 60 nodules were all hypointense in T1 and hyperintense in T2 (Figure 5). After gadolinium administration, there was a centripetal enhancement with partial filling in 18 patients and impregnation centripetally with total filling in a further 9 patients (Figure 6).
All of the 37 patients were diagnosed with hepatic hemangiomas by MR.
DISCUSSION
Incidentalomas or incidental findings on abdominal US of hepatic nodules are frequent. A significant proportion of these cases require other imaging methods to confirm the diagnosis.
Medical conduct in the event of a typical hemangioma nodule on conventional US is diverse. Typically, the conventional exam is repeated after 3 to 6 months, and no other imaging exams are done. Some authors recommend a CT or MR in all cases of nodules greater than 1 mm(13, 14).
Use of contrast in US has brought new perspectives to the method, and this approach is gradually becoming adopted in hepatology for the differential diagnosis of hepatic nodules, detection of primary carcinomas, transplant assessment, among others(12).
Technical advances in US equipment such as pulse inverted harmonics and low mechanical index, allied with a second generation of contrast media, were fundamental in the development of the new method.
Characteristics of enhancement by perflutrene contrast in this study demonstrated similar results to those reported by other authors. Diffuse staining in nodules less than 2 cm and peripheral staining in nodules greater than 2 cm with centripetal filling is partial or total. This pattern of contrast capture in hepatic hemangiomas is not seen in other benign or malignant liver nodules(3).
The conduct of the referring doctor for a patient whose liver nodule had malignant characteristics on US exam, was to order a biopsy of the nodule, which resulted in a pathological diagnosis of hepatic hemangioma. There were no complications during the biopsy.
In the case presenting an indeterminate nodule on contrast US, the requesting physician requested a repeat MR after 3 months, based on a presumptive diagnosis of hepatic hemangioma.
The agreement between contrast US and MR in the diagnosis of hepatic hemangioma has been described as ranging from 88% to 96%(1). In our study, agreement was found in 35 of the 37 cases (94.5%) and the two discordant cases were given the MR diagnosis.
Cases of error with contrast US most likely stem from histological changes in the nodules. False-positives and negatives occur on CT and MR for the same reasons(20, 21).
Piscaglia et al.(17), in a 2006 study of 23.188 ultrasonography exams with contrast, found side effects in 27 cases (0.0086%), the most common being nausea, vomiting, and hypotension. In 2008, an analysis of 66.164 US exams using perflutrene contrast detected mild adverse reactions in 0.006%.
These contrast agents are not nephrotoxic or cardiotoxic and may be used in patients with renal insufficiency. In our study sample, the exam was painless in all 37 patients and no adverse reactions were observed.
Romanini et al.(18), in 2007, showed correlation between US with contrast and MR in the diagnosis of 575 hepatic tumors which were confirmed by biopsy. These authors found sensitivity of 98.1% and specificity of 95.7%, concluding that conventional US associated with contrast US reduced the cost of diagnosing hepatic nodules for hospitals and the public health service.
An US with contrast has several disadvantages over MR, given the former's partial images of the liver and the fact that the exam is operator dependent.
However, US with contrast has broader availability to the general public as the costs of the equipment of the exam itself are lower. It is also a painless exam, with rare side effects. A contrast US can be performed immediately after conventional US reducing time to reach diagnosis and stress and anxiety of the patient.
The results of this study suggest the need for a new protocol for the diagnosis of hepatic nodules found incidentally on routine US exams. In patients with nodules detected on conventional US which are deemed typical of hepatic hemangiomas, follow-up using conventional US should suffice(13). However, in patients with undefined nodules on conventional US, an US with contrast should be the second imaging method indicated. If hepatic hemangioma is subsequently diagnosed, no further investigations are needed.
REFERENCES
Received 22/6/2010.
Accepted 19/11/2010
Study conducted by the Surgery Department of the Faculty of Medical Sciences, Santa Casa of São Paulo and the Schmillevitch Diagnostics Centre, São Paulo, SP, Brasil.
- 1. Bauer A, Solbiati L. Ultrasound contrast agents. In: Solbiati L, Martegani A, Leen E, Correas JM, Burns PN, Becker D, editors. Contrast-enhanced ultrasound of liver diseases. Milan: Springer; 2003. p.21-6.
- 2. Charboneau JW. There is a hyperechoic mass in the liver: what does that mean? In: Cooperberg PL, editor. Categorical course in diagnostic radiology: findings at US - what do they mean? Chicago: RSNA; 2002. p.73-8.
- 3. Claudon M, Cosgrove D, Albrecht T, Bolondi L, Bosio M, Calliada F, Correas JM, Darge K, Dietrich C, D'Onofrio M, Evans DH, Filice C, Greiner L, Jäger K, Jong N, Leen E, Lencioni R, Lindsell D, Martegani A, Meairs S, Nolsøe C, Piscaglia F, Ricci P, Seidel G, Skjoldbye B, Solbiati L, Thorelius L, Tranquart F, Weskott HP, Whittingham T. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) - update 2008. Ultraschall Med. 2008;29:28-44.
- 4. Coumbaras M, Wedum D, Monnier-Cholley L, Dahan H, Tubiana JM, Arrivé L. CT and MR imaging features of pathologically proven atypical hemangiomas of the liver. AJR Am J Roentgenol. 2002;179:1457-63.
- 5. Gallix B, Aufort S. [Incidentalomas]. J Radiol. 2007;88:1048-60.
- 6. Goshima S, Kanematsu M, Kondo H, Yokoyama R, Kajita K, Tsuge Y, Watanabe H, Shiratori Y, Onozuka M, Moriyama N. Diffusion-weighted imaging of the liver: optimizing b value for the detection and characterization of benign and malignant hepatic lesions. J Magn Reson Imaging. 2008;28:691-7.
- 7. Herman P, Costa ML, Machado MA, Pugliese V, D'Albuquerque LA, Machado MC, Gama-Rodrigues JJ, Saad WA. Management of hepatic hemangiomas: a 14-year experience. J Gastrointest Surg. 2005;9:853-9.
- 8. Ishak KG. Benign tumors and pseudotumors of the liver. Appl Pathol. 1988;6:82-104.
- 9. Ishak KG, Goodman Z, Stocker JT. Atlas of tumor pathology: tumors of the liver and intrahepatic bile ducts. Washington: Armed Forces Institute of Pathology; 2001.
- 10. Jang HJ, Kim TK, Lim HK, Park SJ, Sim JS, Kim HY, Lee JH. Hepatic hemangioma: atypical appearances on CT, MR imaging, and sonography. AJR Am J Roentegerol. 2003;180:35-141.
- 11. Kudo M, Tochio H, Zhou P. Differentiation of hepatic tumors by color Doppler imaging: role of the maximum velocity and the pulsatility index of the intratumoral blood flow signal. Intervirology. 2004;47:154-61.
- 12. Lanka B, Jang HJ, Kim TK, Burns PN, Wilson SR. Impact of contrast-enhanced ultrasonography in a tertiary clinical practice. J Ultrasound Med. 2007;26:1703-14.
- 13. Leifer DM, Middleton WD, Teefey SA, Menias CO, Leahy JR. Follow-up of patients at low risk for hepatic malignancy with a characteristic hemangioma at US. Radiology. 2000;214:167-72.
- 14. Machado MM, Rosa ACF, Lemes MS, Mota OM, da Silva OQ, Campoli PMO, Santana Filho JB, Barreto PA, Nunes RA, Barreto MC, Milhomem PM, Milhomem LM, Oliveira GB, Oliveira FB, Castro FCF, Brito AM, Barros N, Cerri GG. Hemangiomas hepáticos: aspectos ultra-sonográficos e clínicos. Radiol Bras. 2006;39:441-6.
- 15. Maruyama H, Matsutani S, Saisho H, Mine Y, Yuki H, Miyata K. Different behaviors of microbubbles in the liver: time-related quantitative analysis of two ultrasound contrast agents, Levovist and Definity. Ultrasound Med Biol. 2004;30:1035-40.
- 16. Maruyama H, Matsutani S, Saisho H, Mine Y, Kamiyama N, Hirata T, Sassamata M. Real time blood-pool images of contrast-enhanced ultrasound with definity in the detection of tumor nodules in the liver. Br J Radiol. 2005;78:512-8.
- 17. Piscaglia F, Bolondi L. The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol. 2006;32:1369-75.
- 18. Romanini L, Passamonti M, Aiani L, Cabassa P, Raieli G, Montermini I, Martegani A, Grazioli L, Calliada F. Economic assessment of contrast-enhanced ultrasonography for evaluation of focal liver lesions: a multicentre Italian experience. Eur Radiol. 2007;17:F99-106.
- 19. Schmillevitch J. Ultra-sonografia com contraste para o estudo de nódulos hepáticos. In: Mincis M, editor. Gastroenterologia e hepatologia. 4a ed. São Paulo: Leitura Médica; 2008. p.75-8.
- 20. Van den Bos IC, Hussain SM, de Man RA, Zondervan PE, Ijzermans JN, Preda A, Krestin GP. Magnetic resonance imaging of liver lesions: exceptions and atypical lesions. Curr Probl Radiol. 2008;37:95-103.
- 21. Vossen JA, Buijs M, Liapi E, Eng J, Bluemke DA, Kamel IR. Receiver operating characteristic analysis of diffusion-weighted magnetic resonance imaging in differentiating hepatic hemangioma from other hypervascular liver lesions. J Comput Assist Tomogr. 2008;32:750-6.
- 22. Wilson SR, Burns PN. Liver mass evaluation with ultrasound: the impact of microbubble contrast agents and pulse inversion imaging. Semin Liver Dis. 2001;21:147-59.
Correspondence:
Publication Dates
-
Publication in this collection
17 June 2011 -
Date of issue
June 2011
History
-
Accepted
19 Nov 2010 -
Received
22 June 2010