Abstracts
CONTEXT: Failure of a colorectal anastomosis represents a life-threatening complication of colorectal surgery. Splenic flexure mobilization may contribute to reduce the occurrence of anastomotic complications due to technical flaws. There are no published reports measuring the impact of splenic flexure mobilization on the length of mobilized colon viable to construct a safe colorectal anastomosis. OBJECTIVE: The aim of the present study was to determine the effect of two techniques for splenic flexure mobilization on colon lengthening during open left-sided colon surgery using a cadaver model. DESIGN: Anatomical dissections for left colectomy and colorectal anastomosis at the sacral promontory level were conducted in 20 fresh cadavers by the same team of four surgeons. The effect of partial and full splenic flexure mobilization on the extent of mobilized left colon segment was determined. SETTING: University of Sao Paulo Medical School, Sao Paulo, SP, Brazil. Tertiary medical institution and university hospital. PARTICIPANTS: A team of four surgeons operated on 20 fresh cadavers. RESULTS: The length of resected left colon enabling a tension-free colorectal anastomosis at the level of sacral promontory achieved without mobilizing the splenic flexure was 46.3 (35-81) cm. After partial mobilization of the splenic flexure, an additionally mobilized colon segment measuring 10.7 (2-30) cm was obtained. After full mobilization of the distal transverse colon, a mean 28.3 (10-65) cm segment was achieved. CONCLUSION: Splenic flexure mobilization techniques are associated to effective left colon lengthening for colorectal anastomosis. This result may contribute to decision-making during rectal surgery and low colorectal and coloanal anastomosis.
Colectomy; Colon, transverse; Rectal neoplasms; Cadaver
CONTEXTO: A deiscência de uma anastomose colorretal representa uma complicação possivelmente fatal na cirurgia colorretal. A mobilização da flexura esplênica pode contribuir para reduzir a ocorrência de complicações da anastomose secundárias a falhas técnicas. Não há trabalhos publicados medindo o impacto da mobilização da flexura esplênica no comprimento do cólon mobilizado viável para a confecção de uma anastomose segura. OBJETIVO: determinar o efeito de duas técnicas de mobilização da flexura esplênica no aumento do comprimento do cólon durante colectomia esquerda aberta, utilizando modelo em cadáver. DESENHO: Dissecções anatômicas para a colectomia esquerda e anastomose colorretal ao nível do promontório sacral foram conduzidas em 20 cadáveres frescos pelo mesmo grupo de quatro cirurgiões. O efeito da mobilização da flexura esplênica parcial e total na extensão do segmento do cólon esquerdo mobilizado foi determinado. LOCAL: Centro Médico da Faculdade de Medicina, São Paulo (SP), Brasil. Instituição médica terciária e hospital universitário. PARTICIPANTES: Um time de quatro cirurgiões operando em 20 cadáveres frescos. RESULTADOS: O comprimento do cólon esquerdo dissecado permitindo uma anastomose sem tensão ao nível do promontório sacral sem a mobilização da flexura esplênica foi de 46,3 (35-81) cm. Após a mobilização parcial da flexura esplênica, um segmento adicional de cólon medindo 10,7 (2-30) cm foi obtido. Após a mobilização completa do cólon transverso distal, um segmento em média de 28,3 (10-65) cm foi obtido. CONCLUSÃO: Técnicas de mobilização da flexura esplênica estão associadas a um aumento efetivo no comprimento do cólon esquerdo para anastomoses colorretais. Esse resultado pode contribuir na tomada de decisões durante a cirurgia retal e anastomoses colorretais baixas e coloanais.
Colectomia; Cólon transverso; Neoplasias retais; Cadáver
ORIGINAL ARTICLES
Assessing the extent of colon lengthening due to splenic flexure mobilization techniques: a cadaver study
Impacto das técnicas de mobilização do ângulo esplênico sobre o alongamento do cólon esquerdo para a anastomose colorretal: estudo em cadáver
Sergio Eduardo Alonso Araujo; Victor Edmond Seid; Nam Jin Kim; Alexandre Bruno Bertoncini; Sergio Carlos Nahas; Ivan Cecconello
Disciplina de Cirurgia do Aparelho Digestivo e Coloproctologia, Departamento de Gastroenterologia, Faculdade de Medicina da Universidade de São Paulo, SP, Brasil
Correspondence Correspondence: Dr. Sergio Eduardo Alonso Araújo Avenida Enéas de Carvalho Aguiar, 255, room 9074 05403-900 - São Paulo, SP, Brazil. E-mail: sergioaraujo@colorretal.com.br
ABSTRACT
CONTEXT: Failure of a colorectal anastomosis represents a life-threatening complication of colorectal surgery. Splenic flexure mobilization may contribute to reduce the occurrence of anastomotic complications due to technical flaws. There are no published reports measuring the impact of splenic flexure mobilization on the length of mobilized colon viable to construct a safe colorectal anastomosis.
OBJECTIVE: The aim of the present study was to determine the effect of two techniques for splenic flexure mobilization on colon lengthening during open left-sided colon surgery using a cadaver model.
DESIGN: Anatomical dissections for left colectomy and colorectal anastomosis at the sacral promontory level were conducted in 20 fresh cadavers by the same team of four surgeons. The effect of partial and full splenic flexure mobilization on the extent of mobilized left colon segment was determined.
SETTING: University of Sao Paulo Medical School, Sao Paulo, SP, Brazil. Tertiary medical institution and university hospital.
PARTICIPANTS: A team of four surgeons operated on 20 fresh cadavers.
RESULTS: The length of resected left colon enabling a tension-free colorectal anastomosis at the level of sacral promontory achieved without mobilizing the splenic flexure was 46.3 (35-81) cm. After partial mobilization of the splenic flexure, an additionally mobilized colon segment measuring 10.7 (2-30) cm was obtained. After full mobilization of the distal transverse colon, a mean 28.3 (10-65) cm segment was achieved.
CONCLUSION: Splenic flexure mobilization techniques are associated to effective left colon lengthening for colorectal anastomosis. This result may contribute to decision-making during rectal surgery and low colorectal and coloanal anastomosis.
Headings: Colectomy. Colon, transverse. Rectal neoplasms. Cadaver.
RESUMO
CONTEXTO: A deiscência de uma anastomose colorretal representa uma complicação possivelmente fatal na cirurgia colorretal. A mobilização da flexura esplênica pode contribuir para reduzir a ocorrência de complicações da anastomose secundárias a falhas técnicas. Não há trabalhos publicados medindo o impacto da mobilização da flexura esplênica no comprimento do cólon mobilizado viável para a confecção de uma anastomose segura.
OBJETIVO: determinar o efeito de duas técnicas de mobilização da flexura esplênica no aumento do comprimento do cólon durante colectomia esquerda aberta, utilizando modelo em cadáver.
DESENHO: Dissecções anatômicas para a colectomia esquerda e anastomose colorretal ao nível do promontório sacral foram conduzidas em 20 cadáveres frescos pelo mesmo grupo de quatro cirurgiões. O efeito da mobilização da flexura esplênica parcial e total na extensão do segmento do cólon esquerdo mobilizado foi determinado.
LOCAL: Centro Médico da Faculdade de Medicina, São Paulo (SP), Brasil. Instituição médica terciária e hospital universitário.
PARTICIPANTES: Um time de quatro cirurgiões operando em 20 cadáveres frescos.
RESULTADOS: O comprimento do cólon esquerdo dissecado permitindo uma anastomose sem tensão ao nível do promontório sacral sem a mobilização da flexura esplênica foi de 46,3 (35-81) cm. Após a mobilização parcial da flexura esplênica, um segmento adicional de cólon medindo 10,7 (2-30) cm foi obtido. Após a mobilização completa do cólon transverso distal, um segmento em média de 28,3 (10-65) cm foi obtido.
CONCLUSÃO: Técnicas de mobilização da flexura esplênica estão associadas a um aumento efetivo no comprimento do cólon esquerdo para anastomoses colorretais. Esse resultado pode contribuir na tomada de decisões durante a cirurgia retal e anastomoses colorretais baixas e coloanais.
Descritores: Colectomia. Cólon transverso. Neoplasias retais. Cadáver.
INTRODUCTION
Failure of a colorectal anastomosis adds not only morbidity and mortality to patients undergoing rectal surgery but also increases the risk of local recurrence when cancer is considered(9). Main technical flaws resulting in a leak from a low colorectal or coloanal anastomosis are inadequate blood supply and tension on the suture line. Adequate blood supply is dependent on an unimpaired marginal artery. Lack of tension is achieved by gaining added length from the left colon. Several maneuvers may be used to allow progressive release of the left colon to provide a tension-free anastomosis to the low rectum(13). One such maneuver, splenic flexure (SF) mobilization, is considered to be an important technical component of anterior rectal resection and low colorectal anastomosis(4).
The main outcome expected from SF mobilization is to achieve a safe and tension-free low colorectal or coloanal anastomosis. Besides, some authors consider that mobilizing SF is also important to provide an adequate oncologic resection(12).
However, SF mobilization is laborious and time-consuming because of the requirement for an extensive retroperitoneal dissection(1). Therefore, it should be carried out using thorough operative technique avoiding lesion to peritoneal (spleen) and retroperitoneal structures such as the ureter and tail of pancreas(6), while preserving vascular supply for future anastomosis. Moreover, a study with colorectal surgeons revealed that they scored the highest difficulty degrees for laparoscopic colorectal procedures requiring SF mobilization(7). Since SF mobilization might also be associated to specific morbidity, manifold approaches for SF mobilization have been used by surgeons to minimize its complications while preserving the benefit of anastomotic safety(13). However, the real effect on left colon lengthening derived from different techniques for SF mobilization remains largely unknown.
We hypothesized that different techniques of SF mobilization may lead to distinct lengths of mobilized left colon. In the present study, we aimed to measure the effect of two techniques for SF mobilization on colon lengthening for colorectal anastomosis during open left-sided colon surgery using a cadaver model.
Literature
There are currently no published clinical or anatomical reports on the length of mobilized colon viable to construct a safe colorectal anastomosis after SF mobilization.
This is the first prospective study concerning the length of left colon segment after SF mobilization. The results reported herein may help surgeons to reach the most adequate decision as to how to proceed regarding the operative strategy on benign and malignant rectal diseases.
MATERIAL
Twenty fresh cadavers with no colonic disease included in its diagnosis, dissected between April and June 2010.
Of the 20 studied cadavers, 12 (60%) were female. Mean age was 63.4 years (35 to 81). Means for weight and height were 66.3 kg (55 to 75) and 1.73 m (1.60 to 1.84), respectively.
Method
An Institutional Review Board at University of São Paulo Medical Center approved this research.
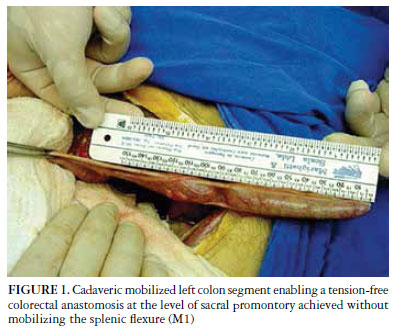
Twenty fresh cadavers were dissected by the same team of four surgeons. In all cadavers, the same procedure was performed. Three measurements were obtained - M1: length (cm) of resected left colon necessary for a tension-free colorectal anastomosis at the level of sacral promontory achieved without mobilizing the splenic flexure; M2: length (cm) of mobilized left colon segment after mobilization of the splenic flexure, and M3: length (cm) of mobilized left colon segment achieved after full mobilization of the distal transverse colon.
Surgical method
All operations were conducted by the same colorectal surgeon (SEAA). Surgical procedure was initiated by performing a full midline incision from the xyphoid process to the pubic symphysis. After retractor placement, peritoneal cavity inspection was accomplished. First, the left colon was fully mobilized through incising the left colic gutter from the splenic flexure to the left peritoneal reflection. After appropriate ureter identification, through careful dissection, the retroperitoneal fascia overlying left kidney, ureter and gonadal vessels was kept intact. The dissection entered the retro-rectal space only to the sacral promontory level. The superior limit for this mobilization was always the inferior pancreatic border at its body and tail; the medial limit was the left aortic aspect; and the inferior dissection limit was the sacral promontory. After completion of left colon mobilization as described, the inferior mesenteric vein (IMV) was divided and ligated right to the inferior pancreatic border. The inferior mesenteric artery was divided and ligated close to the aorta. After completion of vascular control, the rectum was transected at the promontory level. The proximal resection level at the descending colon was such as enabling the construction of a tension-free colorectal anastomosis at the promontory level. To do so, an incision at the mesocolon free edge in a position just cranial to the IMV stump was performed aiming the colon mesenteric border in an upright manner. After dividing the descending colon and the rectum as depicted, the resected colon segment was measured (M1) (Figure 1).
Further, the dissection for SF mobilization was accomplished. The splenocolic ligament was divided and the greater omentum was removed from the SF. After division of the splenocolic ligament and detachment of the omentum for the distal transverse colon, the extent of mobilized left colon that could be resected to ensure a well-constructed colorectal anastomosis was measured (M2).
The last step in the cadaver's surgery was the full separation of the distal transverse mesocolon from its retroperitoneal attachments at the anterior pancreatic border. This detachment is accomplished medially to the level of the left branch of the middle colic artery. As result, the distal transverse colon was completely mobile and used for further descent and colorectal anastomosis. The extent of mobilized left colon that could be resected to ensure a well-constructed colorectal anastomosis after full mobilization of the distal transverse colon was measured (M3) (Figure 2).
RESULTS
In this cadaver model experimental study, the length of resected left colon enabling a tension-free colorectal anastomosis at the level of sacral promontory achieved without mobilizing the SF was 46.3 (35-81) cm. The results in Table 1 demonstrate that a mobilized colonic segment measuring 10.7 (2-30) cm was obtained after partial mobilization of the splenic flexure. In addition, a mean 28.3 (10-65) cm mobilized colon segment was achieved after full mobilization of the distal transverse colon.
DISCUSSION
Clinical anastomotic leakage remains a life-threatening complication after anterior or low anterior rectal resection. The ability to perform a safe resection and reconstruction is an essential part of rectal surgery. When performing a large or small bowel anastomosis, using a hand-sewn or stapling device, the principles that ensure a successful outcome are that the apposed bowel segments are viable, the repair is tension-free, and there is no distal obstruction(13). It is generally accepted that good exposure with adequate mobilization of the colon, often required in the region of the SF, is the key to performing a safe colorectal anastomosis.
Splenic flexure mobilization is considered to be an essential component of anterior resection for rectal cancer. However, routine SF mobilization extends operative time and may be technically challenging in a unpredictable way. Therefore, different degrees of colon detachment may result form different techniques of SF mobilization. As result, selective SF mobilization is currently adopted by many surgeons worldwide(4). We sought to measure the effect of two different techniques for SF mobilization on colon lengthening for colorectal anastomosis using an open surgery cadaver model. We found that an additional 10 to 28 cm-long colon segment might be obtained if SF mobilization is carried out with or without distal transverse colon mobilization. Although not directly assessed in this study, it is plausible to speculate that extending the colon segment available for colorectal anastomosis after SF mobilization would reduce tension, preserve blood flow to the anastomosis and ultimately improve surgical outcomes. This is corroborated by a previous report in which SF mobilization was shown to reduce complications of colorectal anastomosis(8).
The management of rectal diseases through a laparoscopic approach has added some challenges to colorectal surgeons. In laparoscopic low anterior rectal resection, the need to perform a complete total mesorectal excision coupled with low transection of the rectum make the whole operation technically demanding(7). Moreover, the construction of a low colorectal anastomosis after SF mobilization allowing free descent of the left colon into the pelvis adds complexity to the procedure(2, 3, 10) and risk of iatrogenic injuries to spleen and retroperitoneal structures(14). In the study conducted by Jamali et al.(7), a mail-survey of 35 experienced laparoscopic colorectal surgeons revealed that all colorectal procedures requiring SF mobilization scored high difficulty ratings. However, SF mobilization remains utilized by most surgeons involved in laparoscopic total mesorectal excision for rectal cancer(5).
Several interventions may alter the safety of a colorectal anastomosis. Protective stoma, epiploonplasty, use of fibrin glue, and suture reinforcement are procedures frequently used by surgeons, but not in a standardized manner. Moreover, surgeon's experience might play an important role(8). Regarding SF mobilization, it is currently accepted that it may not be performed for patients with a lengthy or redundant sigmoid colon. In these cases, by preserving the superior rectal artery, the blood supply to the distal colon remains intact. Hence, some authors have hypothesized that SF mobilization might be selectively undertaken for rectal cancer surgery(4, 11). Thus, since there is currently no consensus regarding the role of routine SF mobilization for rectal resection, our results providing an estimate about the extent of mobilized left colon derived from partial or full SF mobilization may contribute to solve some controversy.
We must acknowledge some limitations to our study. Firstly, the study was conducted on cadavers and secondly only a reduced number of them were available. However, it is highly unlikely that the results obtained with surgical technique employed would differ significantly in vivo.
There remains no doubt that the experienced surgeon will choose to mobilize the SF if not already done so, once have observed tension in a colorectal anastomosis. However, tension evaluation may be associated to subjectivity. The controversy over the routine use of SF mobilization derives from the fact that there are no randomized trials on this issue. In the meantime, our results may contribute to the decision making process especially after total mesorectal excision and when reconstruction through colonic pouch-anal anastomosis is considered.
This is the first report of a prospective study dedicated to measure the length of left colon segment that can be obtained after SF mobilization. We also quantified the influence of partial and full SF mobilization on left colon lengthening. The results may have important implications in the decision-making during rectal surgery of benign and malignant rectal diseases.
Received 30/1/2012
Accepted 16/5/2012
Declared conflict of interest of all authors: none.
- 1. Akiyoshi T, Kuroyanagi H, Oya M, Ueno M, Fujimoto Y, Konishi T, Yamaguchi T. Factors affecting difficulty of laparoscopic surgery for left-sided colon cancer. Surg Endosc. 2010;24:2749-54.
- 2. Anthuber M, Fuerst A, Elser F, Berger R, Jauch KW. Outcome of laparoscopic surgery for rectal cancer in 101 patients. Dis Colon Rectum. 2003;46:1047-53.
- 3. Bärlehner E, Benhidjeb T, Anders S, Schicke B. Laparoscopic resection for rectal cancer: outcomes in 194 patients and review of the literature. Surg Endosc. 2005;19:757-66.
- 4. Brennan DJ, Moynagh M, Brannigan AE, Gleeson F, Rowland M, O'Connell PR. Routine mobilization of the splenic flexure is not necessary during anterior resection for rectal cancer. Dis Colon Rectum. 2007;50:302-7.
- 5. Cheung YM, Lange MM, Buunen M, Lange JF. Current technique of laparoscopic total mesorectal excision (TME): an international questionnaire among 368 surgeons. Surg Endosc. 2009;23:2796-801.
- 6. Ignjatovic D, Djuric B, Zivanovic V. Is splenic lobe/segment dearterialization feasible for inferior pole trauma during left hemicolectomy? Tech Coloproctol. 2001;5:23-5.
- 7. Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescaux J. Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg. 2008;143:762-7; discussion 8.
- 8. Karanjia ND, Corder AP, Bearn P, Heald RJ. Leakage from stapled low anastomosis after total mesorectal excision for carcinoma of the rectum. Br J Surg. 1994;81:1224-6.
- 9. Konishi T, Watanabe T, Kishimoto J, Nagawa H. Risk factors for anastomotic leakage after surgery for colorectal cancer: results of prospective surveillance. J Am Coll Surg. 2006;202:439-44.
- 10. Morino M, Allaix ME, Giraudo G, Corno F, Garrone C. Laparoscopic versus open surgery for extraperitoneal rectal cancer: a prospective comparative study. Surg Endosc. 2005;19:1460-7.
- 11. Park JS, Kang SB, Kim DW, Lee KH, Kim YH. Laparoscopic versus open resection without splenic flexure mobilization for the treatment of rectum and sigmoid cancer: a study from a single institution that selectively used splenic flexure mobilization. Surg Laparosc Endosc Percutan Tech. 2009;19:62-8.
- 12. Rafferty JF. Obtaining adequate bowel length for colorectal anastomosis. Clin Colon Rectal Surg. 2001;14:25-31.
- 13. Sugarbaker PH. Progressive release of the left colon for a tension-free colorectal or coloanal anastomosis. Cancer Treat Res. 1996;82:255-61.
- 14. Wang JK, Holubar SD, Wolff BG, Follestad B, O'Byrne MM, Qin R. Risk factors for splenic injury during colectomy: a matched case-control study. World J Surg. 2011;35:1123-9.
Correspondence:
Publication Dates
-
Publication in this collection
21 Sept 2012 -
Date of issue
Sept 2012
History
-
Received
30 Jan 2012 -
Accepted
16 May 2012