Abstracts
Background
The esophagus has a different response in relation to the characteristics of a swallowed bolus. Bolus viscosity and body position may affect esophageal contraction and transit.
Objectives
To investigate the effect of bolus viscosity and body position on esophageal contraction, transit and perception.
Methods
Esophageal contraction, transit and perception of transit were evaluated in 26 asymptomatic volunteers, 13 men and 13 women aged 18-60 years, mean: 33.6 (12.2) years. Esophageal contraction (manometry) and transit (impedance) were measured with a solid state catheter with sensors located 5, 10, 15, and 20 cm from the lower esophageal sphincter. Each volunteer swallowed in duplicate and in random sequence a 5 mL low viscous (LV) liquid bolus of an isotonic drink with pH 3.3, and a 5 mL high viscous (HV) paste bolus, which was prepared with 7.5 g of instant food thickener diluted in 50 mL of water (pH: 6.4).
Results
Total bolus transit time, in the sitting position, was longer with the HV bolus than with the LV bolus. Esophageal transit was longer in the supine position than in the sitting position. Bolus head advance time was longer with the HV bolus than with the LV bolus in both positions. Contraction esophageal amplitude was higher in the supine position than in the sitting position. The perception of bolus transit was more frequent with the HV bolus than with the LV bolus, without differences related to position.
Conclusions
The viscosity of the swallowed bolus and body position during swallows has an influence on esophageal contractions, transit and perception of transit.
Esophageal motility disorders; Peristalsis; Viscosity; Manometry; Electric impedance
Contexto
O esôfago tem resposta diferente relacionada às características do bolo deglutido. A viscosidade do bolo e a posição corporal podem afetar a contração do esôfago e o trânsito.
Objetivos
Investigar o efeito da viscosidade do bolo e da posição corporal sobre a contração do esôfago e no trânsito.
Métodos
A contração do esôfago, o trânsito e a percepção do trânsito foram avaliadas em 26 voluntários assintomáticos, 13 homens e 13 mulheres com idade entre 18 e 60 anos, média: 33,6 (12,2) anos. A contração do esôfago (manometria) e trânsito (impedância) foram medidas com um cateter de estado sólido com sensores localizados a 5, 10, 15 e 20 cm do esfíncter esofágico inferior. Cada voluntário deglutiu, em duplicata, 5 mL de bolo líquido (baixa viscosidade - BV, pH: 3,3) e 5 mL de bolo pastoso (alta viscosidade - AV, pH: 6,4).
Resultados
O tempo de trânsito total do bolo, na posição sentada, foi mais longo com o bolo AV do que com bolo BV. O trânsito pelo esôfago foi mais longo na posição supina do que na posição sentada. O tempo de avanço da cabeça do bolo foi mais longo com bolo AV do que com bolo BV, em ambas as posições. A amplitude da contração do esôfago foi maior na posição supina do que na posição sentada. A percepção do trânsito do bolo foi mais frequente com o bolo AV do que com o bolo BV, sem diferença relacionada com a posição.
Conclusões
A viscosidade do bolo deglutido e a posição do corpo durante a deglutição têm influência sobre as contrações esofágicas e no trânsito pelo esôfago.
Transtornos da motilidade esofágica; Viscosidade; Viscosidade; Manometria; Impedância elétrica
INTRODUCTION
The esophagus has a different response in relation to the characteristics of a swallowed bolus. Swallowing a solid bolus causes an increase in amplitude of contractions and a longer bolus transit through the esophageal body compared to swallows of a liquid bolus( 55. Dalmazo J, Aprile LRO, Dantas RO. Esophageal contractions, bolus transit and perception of transit after swallows of liquid and solid boluses in normal subjects. Arq Gastroenterol. 2012;49:250-4. , 1010. Johnston BT, Colins JS, McFarland RJ, Blakwell JN, Love AH. A comparison of esophageal motility in response to bread swallows and water swallows. Am J Gastroenterol. 1993;88:351-5. , 1111. Keren S, Argaman E, Golan M. Solid swallowing versus water swallowing: manometric study of dysphagia. Dig Dis Sci. 1992;37:603-8. , 1818. Zhang X, Xiang X, Tu L, Xie X, Hou X. Esophageal motility in the supine and upright positions for liquid and solid swallows through high-resolution manometry. J Neurogastroenterol Motil. 2013;19:467-72. ). An increase in bolus viscosity causes a slowing of peristaltic contraction propagation( 88. Dooley CP, Schlossmacher B, Valenzuela JE. Effects of alterations in bolus viscosity on esophageal peristalsis in humans. Am J Physiol. 1988;254:G8-11. ), a longer bolus transit( 1616. Wise JL, Murray JA, Conklin JL. Regional differences in oesophageal motor function. Neurogastroenterol Motil. 2004;16:31-7. ) and an increase in contraction duration( 88. Dooley CP, Schlossmacher B, Valenzuela JE. Effects of alterations in bolus viscosity on esophageal peristalsis in humans. Am J Physiol. 1988;254:G8-11. , 99. Gravesen F, Behan N, Drewes A, Gregersen H. Viscosity of food boluses affects the axial force in the esophagus. World J Gastroenterol. 2011;17:1982-8. ), without alteration of contraction amplitude( 99. Gravesen F, Behan N, Drewes A, Gregersen H. Viscosity of food boluses affects the axial force in the esophagus. World J Gastroenterol. 2011;17:1982-8. ). Another investigation described that contraction amplitude is lower with a viscous bolus than a non viscous bolus, that the influence of the viscosity of the bolus has regional differences and that position (supine or upright) has influence on swallows of a non viscous bolus but not on swallows of a viscous bolus( 1616. Wise JL, Murray JA, Conklin JL. Regional differences in oesophageal motor function. Neurogastroenterol Motil. 2004;16:31-7. ). However, investigations with solid and liquid bolus found that peristaltic wave amplitudes and durations are greater in the supine than in the upright position( 1414. Sears VW Jr, Castell JA, Castell DO. Comparison of effects of upright versus supine body position and liquid versus solid bolus on esophageal pressure in normal humans. Dig Dis Sci. 1990;35:857-64. , 1818. Zhang X, Xiang X, Tu L, Xie X, Hou X. Esophageal motility in the supine and upright positions for liquid and solid swallows through high-resolution manometry. J Neurogastroenterol Motil. 2013;19:467-72. ).
There is no correlation between objective measurements of swallowing function and the perception of the bolus esophageal transit( 44. Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJPM. Sensation of stasis is poorly correlated with impaired esophageal bolus transport. Neurogastroenterol Motil. 2014;26:538-45. , 55. Dalmazo J, Aprile LRO, Dantas RO. Esophageal contractions, bolus transit and perception of transit after swallows of liquid and solid boluses in normal subjects. Arq Gastroenterol. 2012;49:250-4. , 1212. Lazarescu A, Karamanolis G, Aprile L, Oliveira RB, Dantas R, Sifrim D. Perception of dysphagia: lack of correlation with objective measurements of esophageal function. Neurogastroenterol Motil. 2010;22:1292-7. , 1717. Xiao Y, Kahrilas PJ, Nicodème F, Lin Z, Roman S, Pandolfino JE. Lack of correlation between HRM metrics and symptoms during the manometric protocol. Am J Gastroenterol. 2014;109:521-6. ), but the perception is more frequent during viscous or solid swallows than during liquid swallows( 55. Dalmazo J, Aprile LRO, Dantas RO. Esophageal contractions, bolus transit and perception of transit after swallows of liquid and solid boluses in normal subjects. Arq Gastroenterol. 2012;49:250-4. , 1717. Xiao Y, Kahrilas PJ, Nicodème F, Lin Z, Roman S, Pandolfino JE. Lack of correlation between HRM metrics and symptoms during the manometric protocol. Am J Gastroenterol. 2014;109:521-6. ).
Our aim in this investigation was to evaluate, in healthy subjects, the esophageal contractions, esophageal bolus transit, and perception of esophageal transit of a low viscous liquid bolus (LV) and a high viscous paste bolus (HV) swallowed in the supine and in the sitting positions. Our hypothesis was that bolus viscosity and position have influence in esophageal contractions, transit and perception of transit.
METHOD
Esophageal contraction, transit and perception of transit were evaluated in 26 asymptomatic volunteers, 13 men and 13 women aged 18-60 years, mean 33.6 (12.2) years. Volunteers were asymptomatic, did not have digestive, pulmonary or neurologic disease, nor swallowing problems, heartburn or regurgitation. They were recruited by advertisement inside the hospital. The investigation was approved by the Human Research Committee of the University Hospital of Ribeirão Preto. All volunteers gave written informed consent to participate in the investigation.
Esophageal contraction and transit were measured with a catheter of the Sandhill Scientific Manometry System (Highlands Ranch, CO - USA) that incorporates five pressure- (two circumferential and three unidirectional) and four impedance-measuring segments( 1515. Tutuian R, Vela MF, Shay SS, Castell DO. Multichannel intraluminal impedance in esophageal function testing and gastroesophageal reflux monitoring. J Clin Gastroenterol. 2003;37:206-15. ). The solid state pressure transducers were placed 5 cm apart, and the impedance-measuring segment consisted of pairs of metal rings placed 2 cm apart, centered at the pressure transducers, thus straddling the four proximal pressure transducers. The signal from the catheter was transferred to an amplifying and digitalizing interface (Sensor PAC-Z, Sandhill Scientific Inc) and recorded and stored using the dedicated software Insight Acquisition (Sandhill Scientific Inc) and Bio-View Analysis (Sandhill Scientific Inc). The amplitude, duration and area under the curve (AUC) of the contractions, and the time of propagation of peristaltic contractions from 20 cm to 5 cm from the lower esophageal sphincter (LES) were analyzed on the manometric tracings and the total bolus transit time (TBTT), bolus head advance time (BHAT), bolus presence time (BPT) and segment transit time (STT) were analyzed on the impedance tracings, as previously described( 1515. Tutuian R, Vela MF, Shay SS, Castell DO. Multichannel intraluminal impedance in esophageal function testing and gastroesophageal reflux monitoring. J Clin Gastroenterol. 2003;37:206-15. ).
The volunteers were studied initially sitting on a chair. The catheter was introduced through the nose until the distal circumferential pressure sensor registered the LES pressure. The others pressure sensor registered the pressures at 5, 10, 15, and 20 cm from the LES. The impedance values were registered at 5, 10, 15, and 20 cm from the LES. After 5 minutes of stabilization of the recording, each volunteer swallowed twice in a random sequence, in the sitting and supine positions, 5 mL of a liquid bolus (Gatorade, AMBEV, Jaquariúna SP, Brazil), an isotonic drink with pH 3.3 which was offered in a syringe, and 5 mL of a paste bolus, which was prepared with 7.5 g of instant food thickner Nutilis (Nutricia, Cuyk BV, Netherlands) diluted in 50 mL of water (pH: 6.4), offered in a spoon of 5 mL, both at room temperature. After the completion of each swallow they were asked about their perception of the bolus passage using a scoring system( 1212. Lazarescu A, Karamanolis G, Aprile L, Oliveira RB, Dantas R, Sifrim D. Perception of dysphagia: lack of correlation with objective measurements of esophageal function. Neurogastroenterol Motil. 2010;22:1292-7. ): 1 - bolus passage without perception of transit; 2 - slow transit; 3 - partial blockage; 4 - complete blockage. The subjects performed 104 swallows of liquid bolus and 104 swallows of paste bolus, 52 swallows in each position for each bolus.
The viscosity of the liquid and paste boluses was measured with a rheometer (Brookfield Engineering Laboratories, Massachusetts, USA) with the spindles LV-2 (liquid) and LV-3 (paste). The liquid bolus had a pH of 3.3 and a density of 1.04 g/cm3. The paste bolus had a pH of 6.4 and a density of 1.05 g/cm3. The measurement of viscosity at 26º C found for the paste bolus, with spindle rotation from 15 to 75 RPM, a range of values from 1585 cp to 3249 cp (high viscous - HV), and for the liquid bolus, with spindle rotation from 110 to 200 RPM, a range of values from 40 cp to 55 cp (low viscous - LV).
Statistical analysis was done by the Center of Quantitative Analysis of the Medical School of Ribeirão Preto USP (CEMEQ) using a linear model with mixed effects( 1313. Schall R. Estimation in generalized linear models with random effects. Biometrika. 1991;78:719-27. ). The model was adjusted using the Proc Mixed feature of the SAS software package version. The results are reported as mean and standard deviation (SD), unless otherwise stated. The differences were considered significant when P≤0.05 in a two-tailed statistical analysis.
RESULTS
The impedance registered, in the sitting position, a complete bolus transit in 58% of swallows of HV and LV boluses and, in the supine position, 62% of HV bolus swallows and 77% of LV swallows (P>0.05). The total bolus transit time, in the sitting position, was longer with the HV bolus [7.5 (2.6) s] than with LV bolus [6.1(1.6) s] (P<0.01). In the supine position there was no difference between HV [8.1(2.5) s] and LV [7.6 (2.2) s] (P>0.05). The transit was longer in the supine position than in sitting position (P<0.05).
Bolus presence time was longer at 5 cm from LES for LV bolus compared with HV bolus, in the sitting and supine positions (P<0.03, Table 1). The bolus head advance time was longer with the HV bolus than with the LV bolus (P<0.04, Table 2), except for the distal esophageal body in the supine position, when there was no difference. For the segment transit time, it was longer for HV bolus in the middle esophagus in the sitting position, and for LV bolus in the distal esophagus in supine position (P<0.02, Table 2).
Esophageal contractions were similar for LV bolus and HV bolus (Table 3), except in the proximal esophagus with the subjects sitting, where the amplitude and the AUC of contractions were higher with the HV bolus compared with LV bolus (P<0.05). There was no difference between HV bolus and LV bolus in the propagation of esophageal contraction [sitting: HV - 3.4 (1.5) s, LV - 5.3 (5.3) s; supine: HV - 3.6 (3.4) s, LV - 3.3 (2.6) s, P>0.05]. The results for amplitude and AUC were higher in the supine position than in sitting position (P<0.03, Table 3). All contractions during LV and HV swallows were peristaltic.
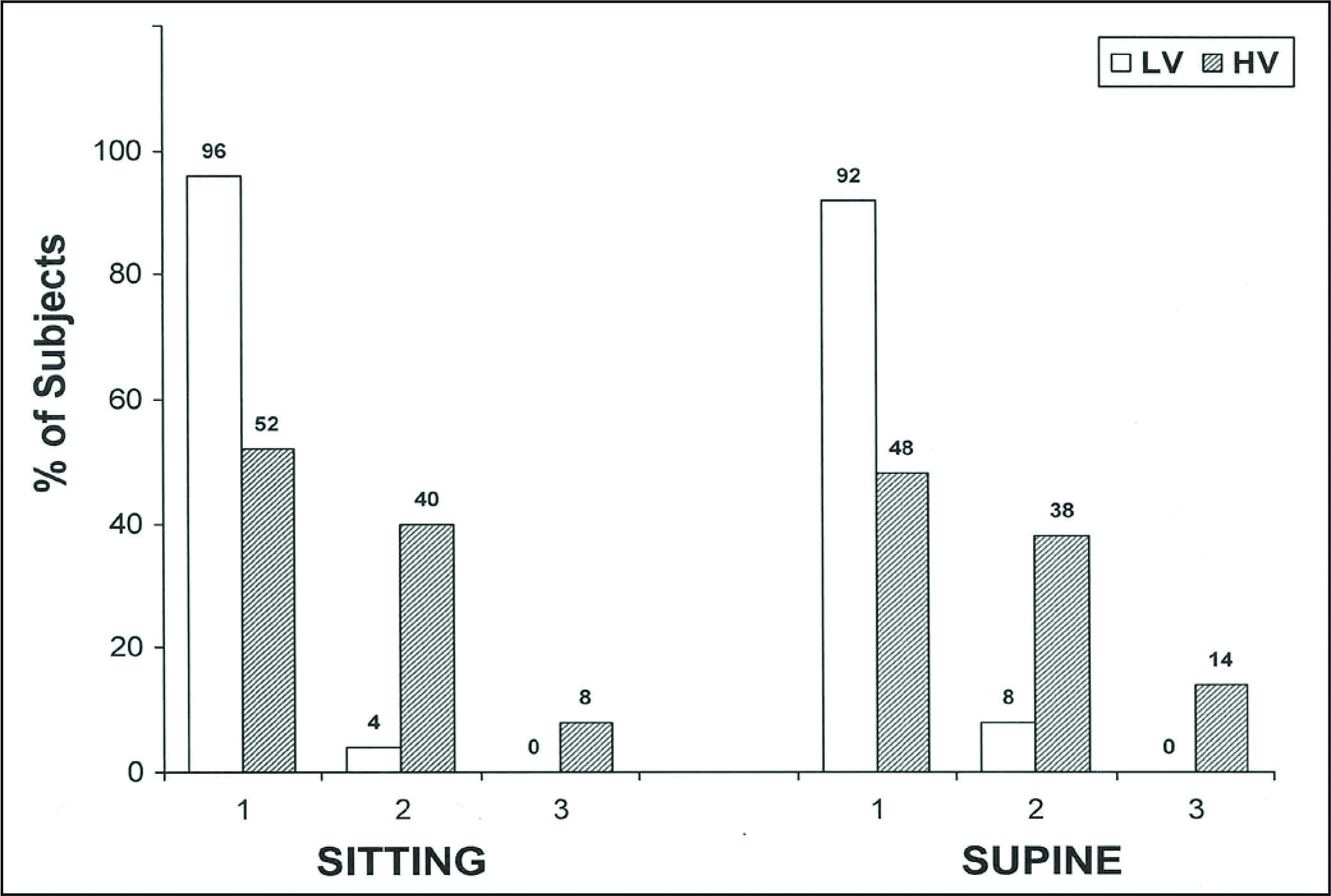
The perception of bolus transit was more frequent with the HV bolus than with the LV bolus (P<0.05), without differences related with the position (Figure 1). There was perception of transit (grades 2 and 3) in the sitting position in 48% of swallows of the HV bolus and 4% of swallows of the LV bolus, and in the supine position there was perception of 52% of swallows of the HV bolus and 8% of the LV bolus. None of the subjects had grade 4 of the scoring system.
Frequency of perception of esophageal transit (% of subjects), in the sitting and supine positions, after swallows of a low viscous bolus (LV) and high viscous bolus (HV). 1 - Bolus passage without perception of transit; 2 - Slow transit; 3 - Partial blockage. None of the subjects had grade 4 of the scoring system. Perception of transit (grades 2 and 3) with HV bolus was more frequent than with LV bolus (P<0.05).
DISCUSSION
Intraluminal impedance associated with manometry is a good method to detect abnormalities of esophageal motility. Nowadays high resolution manometry is considered the best way to perform esophageal motility evaluation( 1717. Xiao Y, Kahrilas PJ, Nicodème F, Lin Z, Roman S, Pandolfino JE. Lack of correlation between HRM metrics and symptoms during the manometric protocol. Am J Gastroenterol. 2014;109:521-6. , 1818. Zhang X, Xiang X, Tu L, Xie X, Hou X. Esophageal motility in the supine and upright positions for liquid and solid swallows through high-resolution manometry. J Neurogastroenterol Motil. 2013;19:467-72. ), although solid state manometry has a high sensitivity to register esophageal contractions and impedance is able to measure esophageal transit. A viscous bolus detects more manometric abnormalities than a liquid bolus, but impedance diagnosis has a greater similarity for both liquid and viscous solutions( 33. Blonski W, Hila A, Jain V, Freeman J, Vela M, Castell DO. Impedance manometry with viscous test solution increases detection of esophageal function defects compared with liquid swallows. Scand J Gastroenterol. 2007;42:917-22. ).
The results we found, a longer BPT with LV than with HV boluses in distal esophagus, in the sitting and supine positions, the BHAT longer with HV bolus than with LV bolus, the contraction amplitude and AUC in the proximal esophagus higher with HV bolus than with LV bolus, in the sitting position, and contraction amplitude and AUC higher in the supine than in the sitting position, are similar to previous ones when measuring the same variables( 1616. Wise JL, Murray JA, Conklin JL. Regional differences in oesophageal motor function. Neurogastroenterol Motil. 2004;16:31-7. ).
The STT in the supine position and the BPT in both positions were longer with the LV bolus at the distal esophageal body. This transit alteration is likely caused by the low pH of the liquid bolus. An acidic bolus has a slower transit through the distal esophageal body than a neutral bolus( 11. Alves LMT, Fabio SRC, Dantas RO. Effect of bolus taste on the esophageal transit of patients with stroke. Dis Esophagus. 2012;26:305-10. , 22. Alves LMT, Secaf M, Dantas RO. Oral, pharyngeal, and esophageal transit of an acidic bolus in healthy subjects. Esophagus. 2013;10:217-22. ), a response of the distal esophageal body that justifies the advice to patients with gastroesophageal reflux disease to not drink acidic liquids.
Bolus transit and bolus head advanced time was longer for the HV bolus than for the LV bolus, consequence of the more difficult transit through the esophagus of a viscous bolus than a non viscous bolus. The response to this slower transit was an increase in esophageal contraction amplitude only in the proximal esophagus, when the swallow was performed in the sitting position, which creates a pressure gradient between proximal and distal esophagus and facilitates the bolus flow. Evaluation of esophageal motility in the supine position described that esophageal pressure amplitude did not increase with the bolus viscosity nor with the bolus volume( 99. Gravesen F, Behan N, Drewes A, Gregersen H. Viscosity of food boluses affects the axial force in the esophagus. World J Gastroenterol. 2011;17:1982-8. ). In supine position, a more intense contraction is needed than in the sitting position to create a pressure gradient between proximal and distal esophagus( 1414. Sears VW Jr, Castell JA, Castell DO. Comparison of effects of upright versus supine body position and liquid versus solid bolus on esophageal pressure in normal humans. Dig Dis Sci. 1990;35:857-64. , 1818. Zhang X, Xiang X, Tu L, Xie X, Hou X. Esophageal motility in the supine and upright positions for liquid and solid swallows through high-resolution manometry. J Neurogastroenterol Motil. 2013;19:467-72. ), thus an increase in esophageal contractions was seen for HV and LV bolus. All the observed variations should be adaptations of the normal function to the characteristic of the bolus and to body position. The clinical implication of the results is that people with ineffective esophageal motility, particularly old subjects, must not eat in the supine position and should avoid the swallow of a high viscous bolus.
The results of the present investigation showed that position has no influence in perception but swallows of a viscous bolus may be associated with transit perception in about half of the swallows performed. The swallows of a viscous bolus need adaptation of esophageal motility, which may explain the more frequent perception of bolus transit with the HV bolus. Esophageal perception of a solid bolus transit through the esophagus is associated with a loss of adaptation to bolus characteristics. In patients without perception of transit a solid bolus causes an increase in the contraction amplitude of the esophageal body, what was not seen in patients with perception( 55. Dalmazo J, Aprile LRO, Dantas RO. Esophageal contractions, bolus transit and perception of transit after swallows of liquid and solid boluses in normal subjects. Arq Gastroenterol. 2012;49:250-4. ).
The esophageal perception of bolus transit is not always associated with esophageal contraction alterations, esophageal transit abnormalities or esophageal stasis( 44. Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJPM. Sensation of stasis is poorly correlated with impaired esophageal bolus transport. Neurogastroenterol Motil. 2014;26:538-45. , 1212. Lazarescu A, Karamanolis G, Aprile L, Oliveira RB, Dantas R, Sifrim D. Perception of dysphagia: lack of correlation with objective measurements of esophageal function. Neurogastroenterol Motil. 2010;22:1292-7. , 1717. Xiao Y, Kahrilas PJ, Nicodème F, Lin Z, Roman S, Pandolfino JE. Lack of correlation between HRM metrics and symptoms during the manometric protocol. Am J Gastroenterol. 2014;109:521-6. ). Even with normal esophageal motility, it is possible to have the perception of the bolus crossing the esophageal body( 44. Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJPM. Sensation of stasis is poorly correlated with impaired esophageal bolus transport. Neurogastroenterol Motil. 2014;26:538-45. , 1212. Lazarescu A, Karamanolis G, Aprile L, Oliveira RB, Dantas R, Sifrim D. Perception of dysphagia: lack of correlation with objective measurements of esophageal function. Neurogastroenterol Motil. 2010;22:1292-7. ). One possibility to explain the perception of HV bolus transit is that during the test the subjects were more alert to the paste bolus than to the liquid bolus, increasing their sensitivity to perceive the bolus transit.
In the pharyngeal phase of swallowing, an increase in bolus viscosity causes a delay in bolus transit and an increase in the duration of pharyngeal peristaltic waves( 77. Dantas RO, Kern MK, Massey BT, Dodds WJ, Kahrilas PJ, Brasseur JG, Cook IJ, Lang IM. Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing. Am J Physiol. 1990;258:G675-81. ). Bolus viscosity does not cause alteration of the amplitude of the oropharyngeal and hypopharyngeal peristaltic pressure complex( 66. Dantas RO, Dodds WJ. Influência da viscosidade do bolo alimentar deglutido na motilidade da faringe. Arq Gastroenterol. 1990;27:164-8. , 77. Dantas RO, Kern MK, Massey BT, Dodds WJ, Kahrilas PJ, Brasseur JG, Cook IJ, Lang IM. Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing. Am J Physiol. 1990;258:G675-81. ), which suggests that there is a similarity between the effect of a HV bolus in the pharynx and esophagus.
In conclusion, swallows performed in the supine position have higher esophageal contraction amplitude than swallows performed in the sitting position, which may be an adaptation to the longer bolus transit through esophagus in supine position. A higher viscous bolus has a longer bolus head advanced time than a lower viscous bolus, but in distal esophagus the bolus presence time was longer with the lower viscous bolus we used than with a higher viscous bolus, perhaps consequence of the lower pH of the LV bolus compared with the pH of the HV bolus. The perception of bolus transit was more frequently observed with the high viscous bolus than with the low viscous bolus, without influence of the body position.
Author contribution
Dalmazo J, Aprile LRO and Dantas RO, who had participation in the investigation and in the preparation of the manuscript.
REFERENCES
-
1Alves LMT, Fabio SRC, Dantas RO. Effect of bolus taste on the esophageal transit of patients with stroke. Dis Esophagus. 2012;26:305-10.
-
2Alves LMT, Secaf M, Dantas RO. Oral, pharyngeal, and esophageal transit of an acidic bolus in healthy subjects. Esophagus. 2013;10:217-22.
-
3Blonski W, Hila A, Jain V, Freeman J, Vela M, Castell DO. Impedance manometry with viscous test solution increases detection of esophageal function defects compared with liquid swallows. Scand J Gastroenterol. 2007;42:917-22.
-
4Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJPM. Sensation of stasis is poorly correlated with impaired esophageal bolus transport. Neurogastroenterol Motil. 2014;26:538-45.
-
5Dalmazo J, Aprile LRO, Dantas RO. Esophageal contractions, bolus transit and perception of transit after swallows of liquid and solid boluses in normal subjects. Arq Gastroenterol. 2012;49:250-4.
-
6Dantas RO, Dodds WJ. Influência da viscosidade do bolo alimentar deglutido na motilidade da faringe. Arq Gastroenterol. 1990;27:164-8.
-
7Dantas RO, Kern MK, Massey BT, Dodds WJ, Kahrilas PJ, Brasseur JG, Cook IJ, Lang IM. Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing. Am J Physiol. 1990;258:G675-81.
-
8Dooley CP, Schlossmacher B, Valenzuela JE. Effects of alterations in bolus viscosity on esophageal peristalsis in humans. Am J Physiol. 1988;254:G8-11.
-
9Gravesen F, Behan N, Drewes A, Gregersen H. Viscosity of food boluses affects the axial force in the esophagus. World J Gastroenterol. 2011;17:1982-8.
-
10Johnston BT, Colins JS, McFarland RJ, Blakwell JN, Love AH. A comparison of esophageal motility in response to bread swallows and water swallows. Am J Gastroenterol. 1993;88:351-5.
-
11Keren S, Argaman E, Golan M. Solid swallowing versus water swallowing: manometric study of dysphagia. Dig Dis Sci. 1992;37:603-8.
-
12Lazarescu A, Karamanolis G, Aprile L, Oliveira RB, Dantas R, Sifrim D. Perception of dysphagia: lack of correlation with objective measurements of esophageal function. Neurogastroenterol Motil. 2010;22:1292-7.
-
13Schall R. Estimation in generalized linear models with random effects. Biometrika. 1991;78:719-27.
-
14Sears VW Jr, Castell JA, Castell DO. Comparison of effects of upright versus supine body position and liquid versus solid bolus on esophageal pressure in normal humans. Dig Dis Sci. 1990;35:857-64.
-
15Tutuian R, Vela MF, Shay SS, Castell DO. Multichannel intraluminal impedance in esophageal function testing and gastroesophageal reflux monitoring. J Clin Gastroenterol. 2003;37:206-15.
-
16Wise JL, Murray JA, Conklin JL. Regional differences in oesophageal motor function. Neurogastroenterol Motil. 2004;16:31-7.
-
17Xiao Y, Kahrilas PJ, Nicodème F, Lin Z, Roman S, Pandolfino JE. Lack of correlation between HRM metrics and symptoms during the manometric protocol. Am J Gastroenterol. 2014;109:521-6.
-
18Zhang X, Xiang X, Tu L, Xie X, Hou X. Esophageal motility in the supine and upright positions for liquid and solid swallows through high-resolution manometry. J Neurogastroenterol Motil. 2013;19:467-72.
-
Disclosure of funding: no funding received
Publication Dates
-
Publication in this collection
Jan-Mar 2015
History
-
Received
3 Mar 2014 -
Accepted
29 May 2014