ABSTRACT
BACKGROUND:
Inflammatory bowel diseases (IBD) are chronic inflammatory affections of recurrent nature whose incidence and prevalence rates have increased, including in Brazil. In long term, they are responsible for structural damage that impacts quality of life, morbidity and mortality of patients.
OBJECTIVE:
To describe the profile of physicians who treat IBD patients as well as the characteristics of IBD care, unmet demands and difficulties.
METHODS:
A questionnaire containing 17 items was prepared and sent to 286 physicians from 101 Brazilian cities across 21 states and the Federal District, selected from the register of the State Commission of the “Study Group of Inflammatory Bowel Disease of Brazil” (GEDIIB).
RESULTS:
The majority of the physicians who answered the questionnaire were gastroenterologists and colorectal surgeons. More than 60% had up to 20 years of experience in the specialty and 53.14% worked at three or more locations. Difficulties in accessing or releasing medicines were evident in this questionnaire, as was referrals to allied healthy professionals working in IBD-related fields. More than 75% of physicians reported difficulties in performing double-balloon enteroscopy and capsule endoscopy, and 67.8% reported difficulties in measuring calprotectin. With regard to the number of patients seen by each physician, it was shown that patients do not concentrate under the responsibility of few doctors. Infliximab and adalimumab were the most commonly used biological medicines and there was a higher prescription of 5-ASA derivatives for ulcerative colitis than for Crohn’s disease. Steroids were prescribed to a smaller proportion of patients in both diseases. The topics “biological therapy failure” and “new drugs” were reported as those with higher priority for discussion in medical congresses. In relation to possible differences among the country’s regions, physicians from the North region reported greater difficulty in accessing complementary exams while those from the Northeast region indicated greater difficulty in accessing or releasing medicines.
CONCLUSION:
The data obtained through this study demonstrate the profile of specialized medical care in IBD and are a useful tool for the implementation of government policies and for the Brazilian society as a whole.
HEADINGS:
Inflammatory bowel diseases; Surveys and questionnaires; Professional practice location
RESUMO
CONTEXTO:
As doenças inflamatórias intestinais (DII) são afecções inflamatórias crônicas de caráter recorrente, cujas taxas de incidência e prevalência têm aumentado, inclusive no Brasil. A longo prazo, são responsáveis por danos estruturais que impactam na qualidade de vida, morbidade e mortalidade dos pacientes.
OBJETIVO:
Avaliar o perfil dos médicos que atendem pacientes com DII, assim como as características deste atendimento, demandas não atendidas e dificuldades.
MÉTODOS:
Um questionário contendo 17 variáveis foi elaborado e enviado para médicos, selecionados a partir do cadastro da Comissão das Estaduais do Grupo de Estudos da Doença Inflamatória Intestinal do Brasil (GEDIIB), totalizando 286 médicos de 101 cidades brasileiras distribuídas por 21 estados e Distrito Federal.
RESULTADOS:
A maioria dos médicos que respondeu o questionário foram Gastroenterologistas e Coloproctologistas. Mais de 60% tinham até 20 anos de atuação na especialidade e 53,14% trabalhavam em três locais ou mais. A dificuldade no acesso ou liberação de medicamentos ficou evidenciada neste questionário, assim como a dificuldade no encaminhamento para profissionais não médicos que atuam em DII. Mais de 75% dos médicos relataram dificuldades para realização de enteroscopia por duplo balão e cápsula endoscópica, e 67,8% para realização da calprotectina. Em relação ao número de pacientes atendidos por cada médico, foi evidenciado que não há uma concentração de pacientes sob a responsabilidade de poucos médicos. O infliximabe e o adalimumabe foram os biológicos mais utilizados e ficou evidenciada prescrição maior de derivados de 5-ASA para retocolite ulcerativa quando comparada à doença de Crohn. Os corticoides foram prescritos para uma parcela menor de pacientes em ambas doenças. Os temas “falha a terapia biológica” e “novas drogas” foram referidos como aqueles com maior prioridade para discussão em eventos científicos. Em relação às possíveis diferenças entre cada região e o restante do país, os médicos da região Norte relataram maior dificuldade no acesso a exames complementares e os médicos da região Nordeste, maior dificuldade no acesso ou liberação de medicamentos.
CONCLUSÃO:
Os dados obtidos por meio deste estudo mostram o perfil do atendimento médico especializado em DII e podem se constituir em ferramenta útil para para elaboração de políticas governamentais e para sociedade brasileira como um todo.
DESCRITORES:
Doenças inflamatórias intestinais; Inquéritos e questionários; Área de atuação profissional
INTRODUCTION
Inflammatory bowel diseases (IBD) are chronic recurrent inflammatory affections that mainly include Crohn’s disease (CD) and ulcerative colitis (UC). Although the etiology remains unknown, it is suggested that an inappropriate inflammatory response to intestinal microbiota occurs in genetically susceptible patients11. Gionchetti P, Dignass A, Danese S, Magro Dias FJ, Rogler G, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 2: Surgical management and special situations. J. Crohn’s Colitis. 2017;11:135-49.
2. Gomollón F, Dignass A, Annese V, Tilg H, Van Assche G, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 1: Diagnosis and medical management. J. Crohn’s Colitis . 2017;11:3-25.-33. Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: Definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J. Crohn’s Colitis . 2017;11:649-70..
The incidence and prevalence rates of IBD have increased, including in Brazil44. Kotze PG, Underwood FE, Damião AOMC, Ferraz JGP, Saad-Hossne R, et al. Progression of inflammatory bowel diseases throughout latin america and the caribbean: a systematic review. Clin Gastroenterol Hepatol. 2020;18:304-12.. In the long term, they are responsible for structural damage that compromises patients’ quality of life and have an impact on the morbidity and mortality of these patients55. Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140:1785-94.. Although therapeutic advances have resulted in lower rates of surgery in patients with CD, stenosis, fistulas and abscesses still frequently occur. The risk of surgical resection within 10 years is estimated to be 50%66. Frolkis AD, Dykeman J, Negrón ME, Debruyn J, Jette N, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013;145:996-1006.. The long-term complications of UC include stenosis in approximately 10% of cases, dysplasia and colorectal cancer77. De Dombal FT, Watts JM, Watkinson G, Goligher JC. Local complications of ulcerative colitis: stricture, pseudopolyposis, and carcinoma of colon and rectum. Br Med J. 1966;1:1442-7.. In a prospective study, the cumulative incidence of colorectal cancer was 2.5% after 20 years of illness and 7.6% after 30 years88. Rutter MD, Saunders BP, Wilkinson KH, Rumbles S, Schofield G, et al. Thirty-year analysis of a colonoscopic surveillance program for neoplasia in ulcerative colitis. Gastroenterology. 2006;130:1030-8..
In order to avoid complications, an appropriate approach aimed clinical and endoscopic remission of patients is fundamental99. Peyrin-Biroulet L, Sandborn W, Sands BE, Reinisch W, Bemelman W. Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE): determining Therapeutic Goals for Treat-to-Target. Am J Gastroenterol. 2015;110:1324-38.. To achieve this, it is necessary to not only have knowledge about IBD but also have a care structure that involves facilities, access to complementary exams, access to medicines and the possibility of multidisciplinary care.
This study aimed to evaluate the profile of physicians caring for patients with IBD as well as the characteristics of IBD care, unmet demands and difficulties regarding to attendance.
METHODS
A questionnaire was prepared by the executive board of the Study Group of Inflammatory Bowel Disease of Brazil (GEDIIB) and forwarded in the form of a quiz to the coordinators of the State Commission of this medical association. The coordinators were responsible for distributing the quiz among physicians who were known to be a reference in IBD care in cities of each state or macroregion. Seventeen variables were analyzed (city where the physician works, state, time since graduation, medical specialty, years of experience in the specialty, workplace, difficulty in accessing and releasing medicines for patients with CD, difficulty in accessing and releasing medicines for patients with UC, difficulty in referring patients to other IBD specialists, difficulty in performing complementary exams, number of patients with CD, number of patients with UC, number of patients with CD using each class of drug, number of patients with UC using each class of drug, number of patients who used each biological medicine as the first-choice drug to treat CD, number of patients who used each biological medicine as the first-choice drug to treat UC and topics on IBD management that he/she would like to discuss). Responses were accepted from April to October 2019. The variables related to the number of patients were divided into intervals and, therefore, classified as semi-quantitative. Descriptive analysis was performed and the results of the quantitative, semi-quantitative and qualitative variables were presented as absolute numbers and percentages. The quantitative variables were analyzed in terms of distribution using the Kolmogorov-Smirnov test. Relationships among qualitative variables were assessed using the chi-square test, and Fisher’s exact test was used when there were cells with a value lower than 5. Relationships among quantitative variables were studied using the Kruskal-Wallis test. The significance level was set at P<0.05.
RESULTS
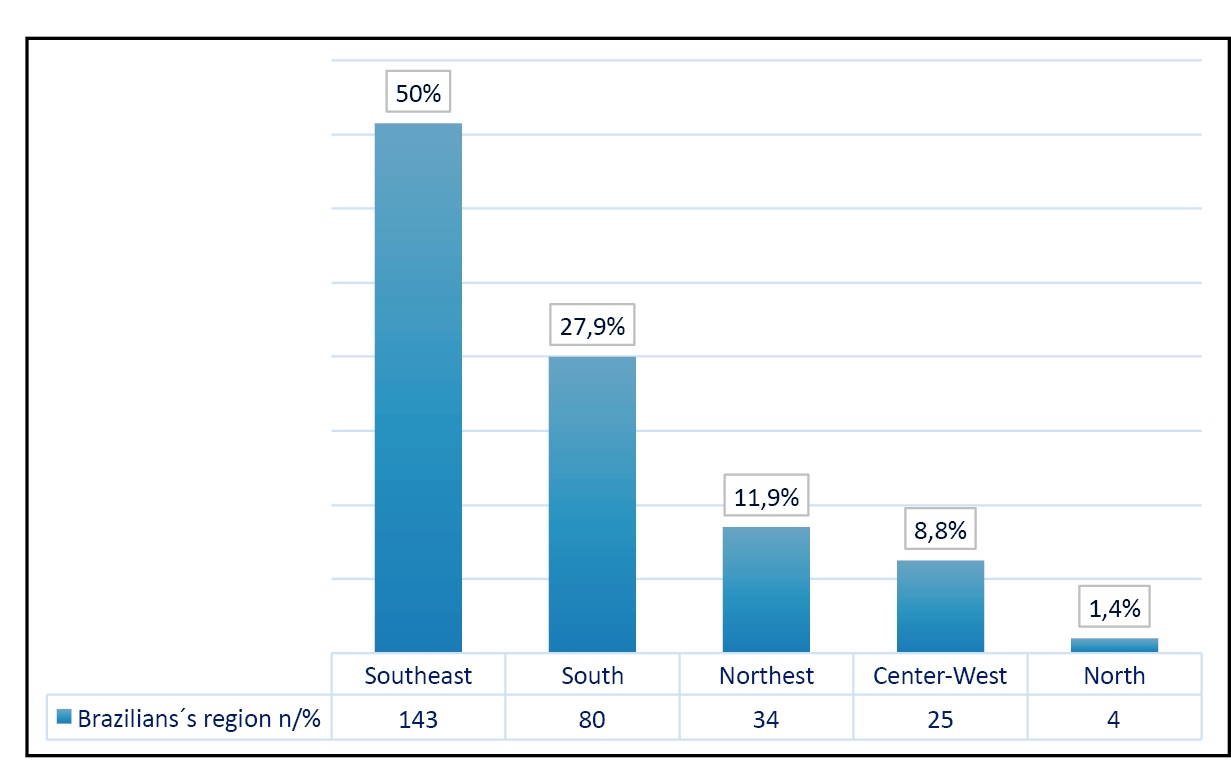
A total of 286 physicians working in 101 Brazilian cities across 21 of 26 states and the Federal District participated in the survey. The state of São Paulo contributed with the highest number of respondents (66), which was equivalent to 23% of the total. The state of Rio Grande do Sul contributed with 36 (12.6%) respondents, Minas Gerais with 32 (11.2%), Paraná with 28 (9.8%) and Rio de Janeiro with 23 (8%), making up the five states with the highest number of respondents. With regard to the number of respondents per region, the Southeast contributed with 143 (50% of the total), the South with 80 (28%), the Northeast with 34 (11.9%), the Center-West with 25 (8.7%) and the North with 4 (1.4%) (Figure 1).
Distribution of the number of responses to the questionnaire by geographic region of Brazil.
The median time since graduation of the medical professionals was 17 years (3-55 years) and the median years of experience in the specialty was 13 years (1-51 years). When the median time since graduation variable was divided into time periods, 60 physicians (21.1%) had between 1 and 10 years of graduation and 107 (38.5%) had between 11 and 20 years of training. These two intervals accounted for 60.1% of the valid responses. Similarly, when the variable years of experience in the specialty was divided into time periods, 119 (42.5%) physicians had between 1 and 10 years of experience and 90 (32.1%) physicians had between 11 and 20 years of experience. This indicates that 74.6% had a maximum of 20 years of experience in the specialty. The specialty that contributed most to the survey was Gastroenterology, with 140 responses (49% of the total), followed by Coloproctology with 104 (36.4% of the total). Figure 2 shows the number of responses from each specialty.
Distribution of the absolute number of responses by medical specialty. Gastroent: Gastroenterology; Coloproct: Coloproctology; Gastroint sur: Gastrointestinal surgery; Endosc: Digestive Endoscopy; GastroPed: Pediatric Gastroenterology; General surg: General surgery.
With regard to the workplace, 58 (20.27%) physicians answered that they worked at one location, including an office, a private clinic, an outpatient clinic or a public hospital. Another 76 (26.57%) physicians worked at two locations and 152 (53.14%) physicians worked at three or more locations. Most physicians (255) worked in clinics or private offices, which corresponded to almost 90% of the sample population. Figure 3 shows the distribution of the physicians’ workplaces.
The difficulty in accessing or releasing medicines was clearly evident in this questionnaire, especially related to biological therapy. The number of physicians that reported this was 201 (70.4%) regarding the treatment of patients with CD and 272 (95.1%) regarding the treatment of UC. Moreover, 207 (72.3%) and 148 (57.74%) physicians reported having difficulty in accessing or releasing the other drug classes (5-ASA derivatives, corticosteroids and immunosuppressants) used in the management of CD and UC patients, respectively. Figure 4 shows the difficulties in numbers for each drug class for each of these diseases.
Frequency of difficulty in accessing or releasing medicines for CD and UC patients in absolute numbers and percentages. CD: Crohn’s disease; UC: ulcerative colitis; 6-MP: 6 mercaptopurine; MTX: methotrexate. The use of methotrexate was not evaluated in the management of patients with UC.
With respect to interdisciplinarity, 192 (67.1%) physicians answered that they had difficulty in referring patients to allied healthy IBD specialists. The greatest difficulties were associated with professionals in the fields of nutrition, psychology and nursing (39.9%, 23.4% and 18.2%, respectively). Figure 5 shows the frequency of difficulty in referral to each field of professionals.
Frequency of difficulty in referring patients to each field of professionals in absolute numbers and percentages. Psichol: Psichologist; Nutricion: Nutricionist; GastroPed: Pediatric Gastroenterologist; Pathol: Pathologist; Gastroent: Gastroenterologist.
The difficulty in performing complementary exams was also assessed. More than half of the physicians reported difficulty in performing double-balloon enteroscopy (77.6%), capsule endoscopy (75.9%), fecal calprotectin testing (67.8%) and MRI enterography (50.7%). More than one-third reported difficulty in requesting screening tests for tuberculosis, either the tuberculin test (purified protein derivative [PPD]) or the interferon-γ release assay (IGRA). However, only four (1.45%) physicians reported difficulty in performing routine laboratory tests (complete blood count, electrolytes, glucose, and kidney, liver and thyroid function) and serological screening tests for hepatitis B, hepatitis C and HIV. Figure 6 shows the exams that were included in the questionnaire and frequency of difficulty in performing them.
Frequency of difficulty in performing complementary exams in absolute numbers and percentages. DB entero: double balloon enteroscopy; Cap endos: capsule endoscopy; Calpr: calprotectin; EnteroMRI: Entero magnetic resonance image; EnteroCT: Enterocomptuted tomography; ST for TB: screening test for tuberculosis; Colon: Colonoscopy; UGIE: upper gastorintestinal endoscopy; AP: anatomopathological; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; Viral Serol: viral serology; Routin: routine.
The following question regarding the number of patients attended to in the various services was included in the questionnaire: “How many patients with a diagnosis of inflammatory bowel diseases are you currently treating?” and the answer options were semi-quantitative (1-10, 11-50, 51-100, 101-200, 201-500 and >500 patients). For both CD and UC, the most common interval was between 11 and 50 patients (115 and 117 doctors, respectively). Figure 7 shows the frequency distribution of each interval for both diseases.
Frequency distribution of the number of physicians by number of patients (in intervals) diagnosed with CD and UC.
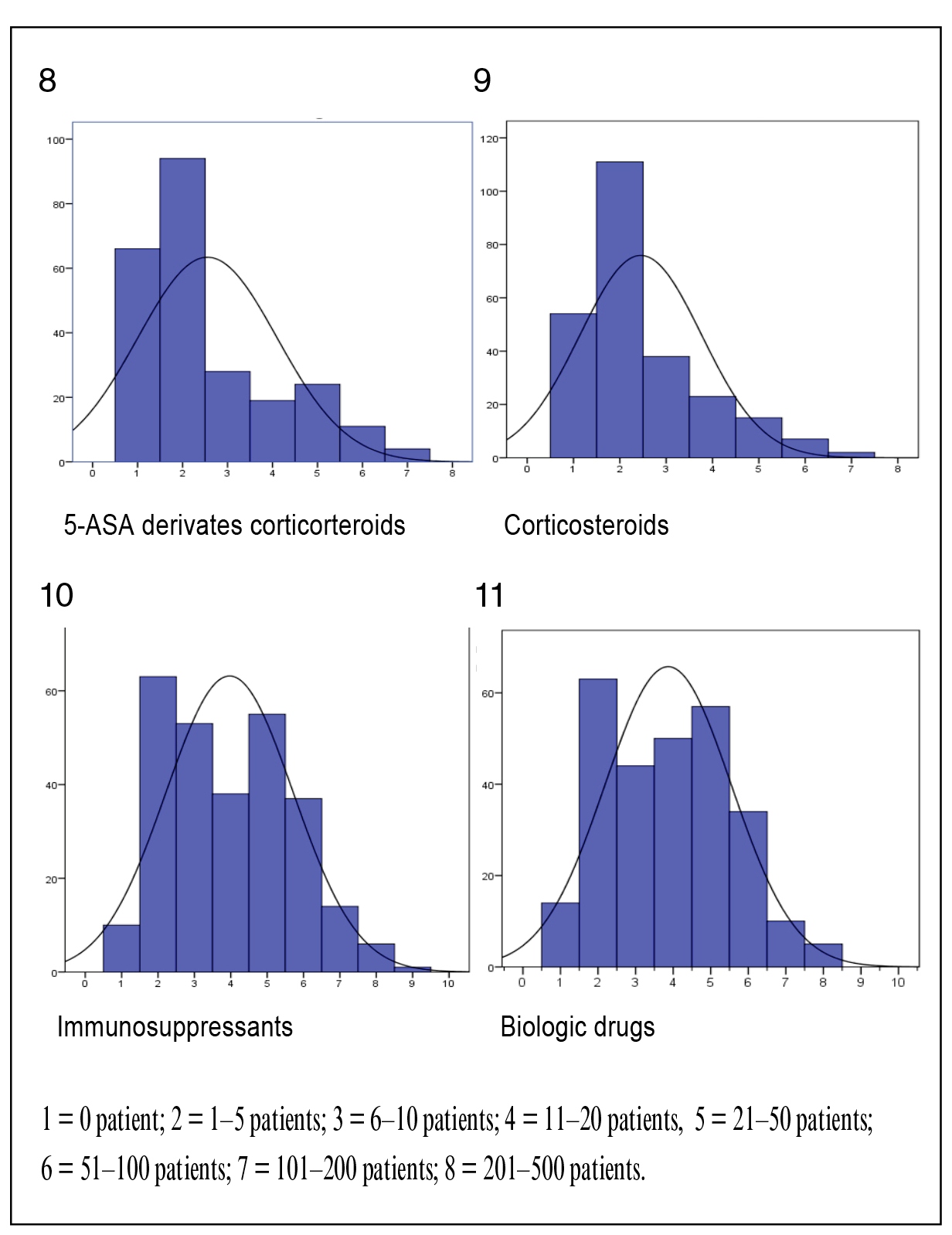
With regard to treatment, using also semi-quantitative data, the following graphs show the frequency of prescription of 5-ASA derivatives, steroids, immunosuppressants and biological medicines for the management of CD among the physicians who answered the questionnaire. The vast majority of physicians responded that they either did not have patients using 5-ASA derivatives or had up to five patients using this drug class. The same response pattern was observed in relation to steroid use. There was no normality of distribution regarding the prescription of both drug classes in the histogram. The distribution of the prescription of immunosuppressants and biological drugs tended to be homogeneous, with higher prescription frequencies around the median. These observations suggest that the frequency of prescribing immunosuppressants and biological drugs tends to be higher than the frequency of prescribing 5-ASA derivatives and steroids for patients with CD. (Figure 8, 9, 10 and 11).
Distribution of frequency of prescription of each drug class to patients with CD (number of patients using each drug class [x] × number of physicians [y]).
A different trend was observed regarding the prescription of the different drug classes to patients with UC. A higher number of physicians had a higher number of prescriptions of 5-ASA derivatives for UC than for CD, and the opposite occurred regarding the prescription of biological medicines, i.e., there was a concentration in the ranges that corresponded to the lowest numbers of physicians and prescriptions. The pattern of corticosteroid and immunosuppressant prescriptions for UC was very similar to that observed for CD. (Figure 12, 13, 14, and 15).
Distribution of frequency of prescription of each drug class to patients with UC (number of patients using each drug class [x] × number of physicians [y]).
The safety in prescribing biological medicines was also evaluated and 44 (15.4%) physicians stated that they did not feel safe to use them. The main reasons were need for discussion with a more experienced team, possibility of exchange of biological drugs and dose optimization.
The following question addressed which biological drug was the physician’s first choice: “How many patients did you assign to each biological medicine of the list below as the first choice drug to manage CD and UC?” For CD, the following options were included: adalimumab, certolizumab, infliximab, ustekinumab and vedolizumab; and for UC, the options were adalimumab, golimumab, infliximab and vedolizumab.
Figure 16, 17, 18, 19 and 20 show the results of responses for CD, and Figure 21, 22, 23 and 24 show those for UC. The X-axis represents the number of prescriptions, and the Y-axis represents the number of physicians. Most physicians did not use certolizumab as the first-choice drug to treat Crohn’s patients. Similarly, but less pronounced, most physicians did not use ustekinumab and vedolizumab as the first-choice drug. The graphs for adalimumab and infliximab demonstrate that they were the most prescribed biological medicines and the behavior of prescription distribution was similar for both, with a higher number of prescriptions of infliximab as the first-choice drug for Crohn’s patients.
Distribution of frequency of prescription of each biological medicine as the first-choice drug in the management of patients with CD.
. Frequency of prescription of each biological medicine as the firstchoice drug in the management of patients with UC.
In relation to UC, only two physicians prescribed golimumab as the first-choice biological medicine. Seventy-three physicians prescribed vedolizumab as the first-choice to 1-5 patients, 20 prescribed it to 6-10 patients, 8 prescribed it to 11-20 patients and 3 prescribed it to >20 patients. The numbers for the use of adalimumab and infliximab are more robust, and, as was observed in the management of CD, there was a higher number of prescriptions of infliximab as the first-choice drug for UC, too.
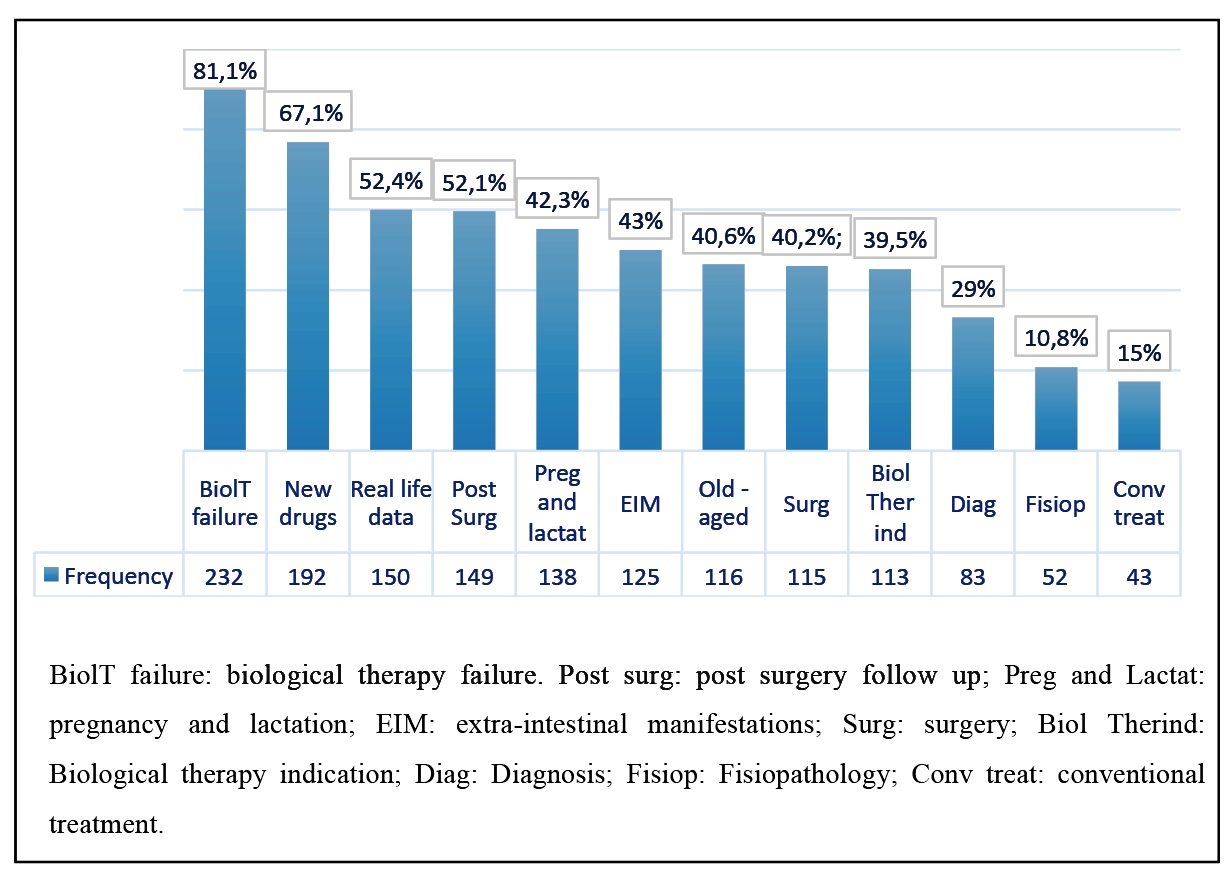
Finally, the physicians were asked which topics related to IBD management they would like to discuss. “Biological therapy failure” and “new drugs” were the topics most frequently indicated by the physicians, with 81.1% and 67.1% of the responses, respectively. Figure 25 shows the topics and the frequency with which each was indicated.
Distribution of frequency of the topics that physicians would like to be discussed further.
To evaluate differences between regions, a comparative analysis was performed between each region and the other regions. The following variables were analyzed: graduation time, years of experience in the specialty, number of specialists, workplace, difficulty in accessing or releasing medicines used in the treatment of IBD, difficulty in referral to other specialists who manage IBD, difficulty in accessing exams and topics they would like to discuss.
Table 1 presents the results related to time since graduation, years of experience in the specialty, medical specialties and workplace. There was no difference in time since graduation and years of experience in the specialty between each region and the other regions of Brazil. However, the analysis of the variable “medical specialties” showed that there were proportionally more gastroenterologists and colorectal surgeons in the Southeast region than in the other regions (P=0.011), whereas there were proportionally more gastroenterologists than colorectal surgeons, general surgeons and gastroenterologists in the Northeast region (P=0.034). This indicates that IBD care was more concentrated in those two specialties in the Southeast region and more concentrated in gastroenterology in the Northeast region. The workplaces were very similar among the regions, with the exception of the location “clinic or private office specialized in IBD care.” Proportionally, there were five times more physicians working in this location in the Northeast region than in the other regions (P=0.003). Another noteworthy result was that in the Center-West region, 38.8% of physicians worked in a “private hospital,” while in the other regions, this rate was 49.8%, which was trend to significance (P=0.057).
With regard to difficulties in accessing and releasing medicines for patients with CD, some differences were observed among the regions. Physicians from the Northeast region reported greater difficulty in the use of 6-mercaptopurine (61.9% vs 27.8%; P=0.034) and methotrexate (70% vs 11.5%; P=0.000). In this region, a statistical trend was observed (9.6% vs 2%, P=0.057), despite P>0.05, toward a greater difficulty in the use of steroids, too. Physicians from the South region reported greater difficulty in accessing or releasing biological medicines (81.25% vs 66%; P=0.014). Nevertheless, in this region, there was a statistical trend for easier access to or release of 6-mercaptopurine and methotrexate (16.25 vs 26.21%, P=0.087; 7.5% vs 16.5%, P=0.057). The results obtained for the other regions were similar to those of the rest of the country. Table 2 shows the results of the statistical analyses based on P-values.
For the management of UC, physicians from the Northeast, South and Center-West regions reported some differences compared with the other regions. There was greater difficulty on the part of physicians from the Northeast region in accessing or releasing steroids (6.5% vs 0.8%; P=0.013) and 6-mercaptopurine (38.2% vs 15.5%; P=0.003). Physicians from the South region reported more difficulty regarding biological medicines. Although the difficulty in accessing or releasing these drugs was evident throughout the country, all 80 physicians in the South region reported some difficulty (100% vs 93.2%; P=0.013). With regard to azathioprine, there was a significant trend toward lower difficulty in accessing and releasing this drug (7.5% vs 16.5%; P=0.057) in South region. In the Center-West region, although the number of affirmative responses regarding difficulty in accessing and releasing biological medicines was also high, there was a statistically difference between the responses (80% vs 96.5%; P=0.04), as shown in Table 3.
The responses related to the difficulty in referring patients to other specialists/professionals working in IBD presented the same behavior in each region and the rest of the country, with the exception of the Northeast region, where it was more difficult to gain access to a surgeon (29.4% vs 14.3%, P=0.03;) and where there was a statistical trend toward difficulty in referral to nursing professionals (35.3% vs 21.8%; P=0.088). (Table 4).
The analysis of the variable “difficulty in performing complementary exams” showed that the situation in the North region is different from that in the rest of the country. However, the number of responses from this region was small44. Kotze PG, Underwood FE, Damião AOMC, Ferraz JGP, Saad-Hossne R, et al. Progression of inflammatory bowel diseases throughout latin america and the caribbean: a systematic review. Clin Gastroenterol Hepatol. 2020;18:304-12.. Physicians from the North region found it more difficult to perform routine laboratory tests (25% vs 0.35%; P=0.028), serum markers of inflammation (25% vs 2.1%; P=0.021), computed tomography enterography (100% vs 38.7%; P=0.024), colonoscopy (75% vs 18.8%; P=0.025) and anatopathological exams (50% vs 4.6%; P=0.015). The responses of the physicians from the Center-West region showed a trend toward greater difficulty in performing screening tests for tuberculosis (48% vs 29.8%; P=0.073), and, instead, lower difficulty in performing MRI enterography (47% vs 52.5%; P=0.06). In the Southeast region, there was trend toward lower difficulty in performing screening tests for tuberculosis (25.9% vs 37%; P=0.056). The responses of physicians from the South and Northeast regions regarding complementary exams were not significantly different from that of the rest of the country. (Table 5).
When the variable “preferred subjects or topics to be further discussed” was analyzed, the pattern of responses of the specialists from the Center-West region reflected a higher demand for the discussion of topics compared with the rest of Brazil, namely the topics “Pregnancy and Lactation” and “Extraintestinal manifestations” (72% vs 46.15%, P=0.020; 68% vs 41.4%, P=0.012). The responses also indicated a trend toward a greater demand for discussion of the topics “Biological treatment-indication”, “Biological treatment-failure” and “Elderly” (60% vs 39.8%, P=0.058; 96% vs 79.7%, P=0.058; 605 vs 38.7%, P=0.054, respectively). The responses from the Southeast region showed a lower demand for the topic “Biological treatment-indication” (34.9% vs 48.2%, P=0.031), and a similar result was observed in the South region, where there was less demand for the topics “pregnancy and lactation” and “elderly” (31.25% vs 55.12%, P=0.000; 30% vs 44.6%, P=0.031, respectively). The responses from the Northeast and North regions did not indicate different demands compared with the rest of the country for each topic. (Table 6).
DISCUSSION
This study was developed based on a questionnaire that was customized by the executive board of GEDIIB and answered by physicians working in 21 of the 26 Brazilian states and in the Federal District. Physicians from states of Tocantins in the Center-West region and states of Acre, Amapá, Rondônia and Roraima in the North region did not participate in the study. The highest concentration of responses was in the Southeast region, accounting for 50% of the total, which possibly reflects the higher number of practicing physicians in these regions1010. Demografia Médica: Brasil possui médicos ativos com CRM em quantidade suficiente para atender demandas da população. Conselho Federal de Medicina, Brasília, 26 de Novembro de 2018. Disponível em: Disponível em: https://amb.org.br/wp-content/uploads/2018/03/DEMOGRAFIA-M%C3%89DICA.pdf . Acesso em 21 de fevereiro de 2020.
https://amb.org.br/wp-content/uploads/20...
. The Southest is the region with highest ratio of doctors per 1.000 inhabitants (2.81), while North region has the lowest, 1.16/1.000 inhabitants1010. Demografia Médica: Brasil possui médicos ativos com CRM em quantidade suficiente para atender demandas da população. Conselho Federal de Medicina, Brasília, 26 de Novembro de 2018. Disponível em: Disponível em: https://amb.org.br/wp-content/uploads/2018/03/DEMOGRAFIA-M%C3%89DICA.pdf . Acesso em 21 de fevereiro de 2020.
https://amb.org.br/wp-content/uploads/20...
.
This same trend of distribution of responses was observed when data referring to the states were evaluated. Thus, states such as Amazonas and Pará in the North region contributed with two responses each and states such as Alagoas, Paraíba, Rio Grande do Norte and Sergipe in the Northeast region contributed with only one response each. The five states with the highest number of responses also have a higher number of physicians actively registered in the Federal Council of Medicine (CFM) - 287.271 of 451.777 registered physicians in Brazil in 20171010. Demografia Médica: Brasil possui médicos ativos com CRM em quantidade suficiente para atender demandas da população. Conselho Federal de Medicina, Brasília, 26 de Novembro de 2018. Disponível em: Disponível em: https://amb.org.br/wp-content/uploads/2018/03/DEMOGRAFIA-M%C3%89DICA.pdf . Acesso em 21 de fevereiro de 2020.
https://amb.org.br/wp-content/uploads/20...
.
Most physicians who answered the questionnaire (60.1%) had up to 20 years of professional experience, and almost 75% of them also had up to 20 years of experience as specialists. The concentration of responses in this range of years of professional experience also reflects the medical demographic data published by the CFM, which indicated the young age of physicians in Brazil1010. Demografia Médica: Brasil possui médicos ativos com CRM em quantidade suficiente para atender demandas da população. Conselho Federal de Medicina, Brasília, 26 de Novembro de 2018. Disponível em: Disponível em: https://amb.org.br/wp-content/uploads/2018/03/DEMOGRAFIA-M%C3%89DICA.pdf . Acesso em 21 de fevereiro de 2020.
https://amb.org.br/wp-content/uploads/20...
. The average age of doctors working in the country is 45.4 years. The CFM states that this is a result of the increase in new physicians as a result of the opening of new medical courses. However, it is not possible to rule out the growing interest of younger physicians for the subject and the increasing number of vacancies in medical residency programs1111. Recorte Demográfico da Residência Médica Brasileira em 2019. Revista Consensus, Brasília, Edição 32; 2019. [Internet]. [Access 2020 February 21]. Available from: Available from: http://www.conass.org.br/consensus/recorte-demografico-da-residencia-medica-brasileira-em-2019/ .
http://www.conass.org.br/consensus/recor...
.
Gastroenterology and Coloproctology were the most represented specialties (85.4% of the total). This is explained by the fact that these specialists have the most affinity and interest for the topic. Currently, the GEDIIB has 612 associated physicians, of which 226 are gastroenterologists and 171 are colorectal surgeons, which accounts for 65% of the total. On the other hand, only one physician specializing in Internal Medicine answered the questionnaire. The number of respondent Pediatric Gastroenterologists was also noteworthy, with only eight answering the questionnaire (three from Rio Grande do Sul, two from Maranhão and one each from Santa Catarina, São Paulo and Pernambuco). It is likely that the questionnaire was not sent to a large number of Pediatric Gastroenterologists. Currently, the GEDIIB has 36 Pediatric Gastroenterologists.
With regard to the workplace, the responses represented a phenomenon observed in Brazil since the 1980s, i.e., multiple employment caused by reduction in physicians’ wages1212. Maciel Filho R, Pierantoni CR. O médico e o mercado de trabalho em saúde no Brasil: revendo conceitos e mudanças. Observatório de Recursos Humanos em Saúde no Brasil. Estudos e Análises - Volume 2. 2013;139-62.. Only 58 (20.37%) physicians work at a single location, while 152 (53.14%) work at three or more locations, although they are specialists. Almost 90% of the sample (255 doctors) work in a clinic or private office.
Another problem in the analysis of this questionnaire was the difficulty in accessing or releasing medicines, particularly those associated with biological therapy. However, the responses related to the other drug classes indicate that the situation is much more complicated. For CD, 70.4% of physicians responded that they have difficulty in accessing or releasing biological medicines and 72.3% responded that this is also the case with the other drug classes used in the treatment of the disease. The numbers for this variable regarding biological therapy for UC were higher (95.1%) and 57.74% answered that they have difficulties with other drugs. These results are attributable to several reasons. The distribution of these drugs in the Brazilian Unified Health System (SUS) follows the Clinical Protocol and Therapeutic Guidelines (PCDT) of the Federal Government. For CD, the first PCDT dates from 2002 and included the following drugs: sulfasalazine, mesalazine, metronidazole, ciprofloxacin, hydrocortisone, prednisone, azathioprine, 6-mercaptopurine, methotrexate, cyclosporine, infliximab, and thalidomide1313. Protocolo Clínico e Diretrizes Terapêuticas - Doença de Crohn. Portaria nº 858 de 12 de novembro de 2002. [Internet]. [Access 2020 February 21]. Available from: https://portalarquivos2.saude.gov.br/images/pdf/2014/abril/02/pcdt-doenca-de-crohn-2010.pdf.
https://portalarquivos2.saude.gov.br/ima...
. In its previous review in 2017, adalimumab, certolizumab and allopurinol were also included1414. Portaria Conjunta Nº 14, de 28 de Novembro De 2017. Protocolo Clínico de Diretrizes Terapêuticas - Doença De Crohn. [Internet]. [Access 2020 February 22]. Available from: http://conitec.gov.br/images/Protocolos/Portaria_Conjunta_14_PCDT_Doenca_de_Crohn_28_11_2017.pdf.
http://conitec.gov.br/images/Protocolos/...
. Therefore, although vedolizumab has been registered by the National Health Surveillance Agency (Anvisa) since 2015, it was not part of this protocol1515. Consultas - Anvisa - Agência Nacional de Vigilância Sanitária. Vedolizumabe. [Internet]. [Access 2020 February 22]. Available from: https://consultas.anvisa.gov.br/#/medicamentos/25351596045201401/?substancia=25770.
https://consultas.anvisa.gov.br/#/medica...
. In 2018, ustekinumab was officially registered by ANVISA for the treatment of CD, thus, it was not included in the more recent protocol of the government1616. Consultas - Anvisa - Agência Nacional de Vigilância Sanitária. Ustequinumabe. [Internet]. [Access 2020 February 22]. Available from: https://consultas.anvisa.gov.br/#/medicamentos/25351630200200806/?substancia=25220.
https://consultas.anvisa.gov.br/#/medica...
. Hence, two biologics used in the treatment of patients with CD were not yet included in the last PCDT. Concomitantly, investment in public healthcare in Brazil has been decreasing annually. Thus, government pharmacies have not been supplied as they should, including medicines used in the conventional treatment of IBD. This portrays the situation in relation to the approach to CD in the public system. In the private healthcare system, biological therapy for CD was incorporated into the list of procedures of the National Health Agency (ANS) in 2017, and there was no specific mention of the types of biological medicines1717. Nota Técnica nº 196/2017; Nota Técnica nº 204/2017; Revisão do Rol de Procedimentos e Eventos em Saúde - 2018 Processo nº 33902.440494/2016-22. [Internet]. [Access 2020 February 22]. Available from: http://www.ans.gov.br/images/stories/ Particitacao_da_sociedade/consultas_publicas/cp61/cp61_relatorio_nota_tecnica_ 204_2017.pdf.
http://www.ans.gov.br/images/stories/ Pa...
. Medicines used in the conventional treatment of CD are not included in the ANS procedures list. The situation is even worse in terms of UC management, because in the period during which the questionnaire was available (between April and October 2019), the current PCDT for UC dated from 20021818. Protocolo Clinico e Diretrizes Terapêuticas - Retocolite ulcerativa. Portaria SAS/MS nº 861, [Internet]. [Access 2002 November 4]. Available from: Available from: http://bvsms.saude.gov.br/bvs/publicacoes/protocolo_clinico_diretrizes_terapeuticas_retocolite_ulcerativa.pdf . Acesso em 22 de fevereiro de 2020.
http://bvsms.saude.gov.br/bvs/publicacoe...
. In this PCDT there was no mention of biological therapy. In November 2019, the recommendation report of the Ministry of Health was published, in which the first and only existing protocol (of 2002) was reviewed. It added biological therapy (infliximab) to treat moderate to severe UC refractory to conventional treatment, including in the pediatric population. However, the first option for treating severe acute colitis was cyclosporine. Furthermore, adalimumab, golimumab, ustekinumab and tofacitinib were not included. This report was available for public consultation recently and was approved by the government, but there is no infliximab to treat UC patients, yet. In the private system, no biological medicine has been included in the ANS list to date1818. Protocolo Clinico e Diretrizes Terapêuticas - Retocolite ulcerativa. Portaria SAS/MS nº 861, [Internet]. [Access 2002 November 4]. Available from: Available from: http://bvsms.saude.gov.br/bvs/publicacoes/protocolo_clinico_diretrizes_terapeuticas_retocolite_ulcerativa.pdf . Acesso em 22 de fevereiro de 2020.
http://bvsms.saude.gov.br/bvs/publicacoe...
. In this context, there have been increasing legal actions regarding the access and release of these medicines, not only against the government but also against health operators.
IBD often require a multidisciplinary team for a comprehensive approach. In this context, the questionnaire showed that the professionals in the fields of nutrition, psychology and nursing were the most difficult to refer patients to and/or engage (40.2%, 39.9%, and 23.4%, respectively). Unlike what happens with Medicine, through medical residency programs, which have been regulated by the Federal Government since 1977 and through which important part of specialists are trained, multiprofessional residency programs in health were only created in 2005, with still few programs available, and the number of vacancies is still reduced1919. Residência multiprofissional. [Internet]. [Access 2020 February 22]. Available from: http://portal.mec.gov.br/residencias-em-residencia-multiprofissional.
http://portal.mec.gov.br/residencias-em-...
. These programs do not focus on specific subareas such as IBD. Thus, there is a significant lack of non-medical health professionals either working in or with affinity for IBD.
Another fundamental issue for the correct management of patients with IBD is access to complementary exams. More complex endoscopic exams, although less used, such as double-balloon enteroscopy and capsule endoscopy were the most frequently cited, i.e., physicians reported having greater difficulty in performing these exams. These are procedures that, despite being available in some centers in Brazil, are not covered by the SUS and are also not included in the ANS procedures list1717. Nota Técnica nº 196/2017; Nota Técnica nº 204/2017; Revisão do Rol de Procedimentos e Eventos em Saúde - 2018 Processo nº 33902.440494/2016-22. [Internet]. [Access 2020 February 22]. Available from: http://www.ans.gov.br/images/stories/ Particitacao_da_sociedade/consultas_publicas/cp61/cp61_relatorio_nota_tecnica_ 204_2017.pdf.
http://www.ans.gov.br/images/stories/ Pa...
. With regard to the most routinely used endoscopic exams in IBD care, less than one-fifth of the specialists reported difficulty in performing colonoscopy and only 7% reported difficultly in performing upper gastrointestinal endoscopy. In relation to calprotectin testing, it is still difficult to perform because it is a test that is unavailable both in the SUS and in the ANS procedures list, as is the case with the previous two endoscopic exams1717. Nota Técnica nº 196/2017; Nota Técnica nº 204/2017; Revisão do Rol de Procedimentos e Eventos em Saúde - 2018 Processo nº 33902.440494/2016-22. [Internet]. [Access 2020 February 22]. Available from: http://www.ans.gov.br/images/stories/ Particitacao_da_sociedade/consultas_publicas/cp61/cp61_relatorio_nota_tecnica_ 204_2017.pdf.
http://www.ans.gov.br/images/stories/ Pa...
. So patients, have to pay by themselves. MRI enterography and CT enterography were difficult to perform for 50.7% and 39.5% of the physicians; both are listed in the ANS procedures list but are not available in the SUS1717. Nota Técnica nº 196/2017; Nota Técnica nº 204/2017; Revisão do Rol de Procedimentos e Eventos em Saúde - 2018 Processo nº 33902.440494/2016-22. [Internet]. [Access 2020 February 22]. Available from: http://www.ans.gov.br/images/stories/ Particitacao_da_sociedade/consultas_publicas/cp61/cp61_relatorio_nota_tecnica_ 204_2017.pdf.
http://www.ans.gov.br/images/stories/ Pa...
.
Notably, more than one-third of the physicians reported difficulty in requesting the PPD test or IGRA. The PPD test was in short supply in Brazil, and this situation was duly documented by the GEDIIB together with the Brazilian Society of Rheumatology and the Brazilian Society of Dermatology2020. Nota conjunta sobre indisponibilidade temporária do PPD. São Paulo, 06 de fevereiro de 2020. [Internet]. [Access 2020 February 23]. Available from: Available from: https://www.reumatologia.org.br/site/wp-content/uploads/2020/02/Nota-Tecnica.-Assinada-PPD.03.fev2020.pdf .
https://www.reumatologia.org.br/site/wp-...
. According to the Ministry of Health, the unavailability of the PPD test resulted from problems in the acquisition of it and issues that involved registration by Anvisa2020. Nota conjunta sobre indisponibilidade temporária do PPD. São Paulo, 06 de fevereiro de 2020. [Internet]. [Access 2020 February 23]. Available from: Available from: https://www.reumatologia.org.br/site/wp-content/uploads/2020/02/Nota-Tecnica.-Assinada-PPD.03.fev2020.pdf .
https://www.reumatologia.org.br/site/wp-...
. IGRA is not included in the ANS procedures list and is also not available in the SUS.
With regard to routine laboratory tests, viral serology, inflammatory serum markers and chest X-ray, the number of respondents reporting difficulty did not exceed 3%. These tests are available in the SUS and are also included in the ANS procedures list. Similarly, routine anatomopathological examinations are available in both the public and private health systems, which is why only 5.2% of physicians found it difficult to use them1818. Protocolo Clinico e Diretrizes Terapêuticas - Retocolite ulcerativa. Portaria SAS/MS nº 861, [Internet]. [Access 2002 November 4]. Available from: Available from: http://bvsms.saude.gov.br/bvs/publicacoes/protocolo_clinico_diretrizes_terapeuticas_retocolite_ulcerativa.pdf . Acesso em 22 de fevereiro de 2020.
http://bvsms.saude.gov.br/bvs/publicacoe...
.
Most physicians treated between 1 and 10 and between 11 and 50 patients with CD and UC, respectively; of these, approximately two-thirds reported that they cared for 11 to 50 patients diagnosed with each disease. This shows that there is no concentration of patients under the responsibility of a limited number of doctors. Physicians who answered “more than 500 patients,” both for CD and UC (5 and 4, respectively), were mostly professionals who worked in reference centers within public universities.
Graphs depicting the prescription of each drug class to patients with CD show that the frequency of prescribing immunosuppressants and biological drugs was higher than that of prescribing 5-ASA derivatives and steroids. It is known that steroids should not be used to maintain remission in these patients and that 5-ASA derivatives are of little use in maintaining CD remission, except when the colon is affected2121. Burger D, Travis S. Conventional Medical Management of Inflammatory Bowel Disease. Gastroenterology. 2011;140:1827-37.. With regard to UC management, the trend regarding the prescription of 5-ASA derivatives was different, exhibiting the same distribution as that of the prescription of immunosuppressants and biological medicines for CD and of immunosuppressants for UC. This happened, possibly, because this drug class is used to maintain UC remission2121. Burger D, Travis S. Conventional Medical Management of Inflammatory Bowel Disease. Gastroenterology. 2011;140:1827-37.. The distribution of prescription of biologics was similar to that of steroids, i.e., most physicians had few patients using these drug classes. The result obtained for biological therapy is most likely associated with the difficulty in its access or release, as mentioned above.
With regard to the safety of prescribing biologics, 15.4% of physicians reported that they still felt unsafe to use them and that this insecurity was related to the lack of discussion with more experienced staff, the risk of exchange of biologics and dose optimization. The authors believe that such data will be useful for promoting future actions related to a continuing education program.
Among the available biological medicines, infliximab and adalimumab were the most used as the first-choice drug for both CD and UC. These drugs have been available for longer in Brazil, and this may be one of the reasons for these results.
To collect data for the elaboration of continuing education programs, the questionnaire also aimed to evaluate the topics of IBD management the specialists wanted to discuss. The topics related to advanced therapy were the most demanded (biological therapy failure and new drugs; 81.1% and 67.1%, respectively). Only 15% of physicians said that they wanted to discuss conventional treatment. This can be interpreted in two ways: one is related to the acquired knowledge about this treatment; on the other hand, it is a fact that the recycling and updating of topics in medicine is always desirable, so the fact that 85% of physicians did not wish to discuss a particular topic warrants consideration.
In addition, a comparison was made in this study between each region and the rest of Brazil. In relation to time since graduation and years of experience in the specialty, the medians were the same. With regard to medical specialties, IBD care was more concentrated among gastroenterologists and colorectal surgeons in the Southeast region and among gastroenterologists in the Northeast region than in the rest of the country. The higher number of specialists acting in the Southeast region probably facilitates the population’s access to these specialties1010. Demografia Médica: Brasil possui médicos ativos com CRM em quantidade suficiente para atender demandas da população. Conselho Federal de Medicina, Brasília, 26 de Novembro de 2018. Disponível em: Disponível em: https://amb.org.br/wp-content/uploads/2018/03/DEMOGRAFIA-M%C3%89DICA.pdf . Acesso em 21 de fevereiro de 2020.
https://amb.org.br/wp-content/uploads/20...
. The data relative to the Northeast region shows that few specialists from other areas answered the questionnaire. This may act as a bias in the interpretation of the results, because the concentration of care among gastroenterologists does not necessarily mean greater accessibility to them, but rather difficulties in accessing other specialists who manage IBD.
The data obtained about the physicians’ workplace were very similar between each region and the overall results of Brazil. However, it was evident that physicians in the Northeast region worked proportionally more in IBD clinics or private offices, and that the number of physicians working in private hospitals was lower in the Center-West region than in other regions. These results put in evidence specific characteristics that are difficult to interpret. However, they will certainly be useful for future comparisons.
As already discussed, the difficulty in accessing or releasing medicines was a serious problem detected through this questionnaire. When comparing each region with the rest of the country, significant differences were observed, both regarding the approach to CD and UC. With regard to CD, physicians from the Northeast reported greater difficulty in accessing or releasing 6-mercaptopurine and methotrexate, while physicians from the South region reported greater difficulty in accessing or releasing biologics. The known regional differences are mainly due to the availability of medicines in the State Health Departments (SES), which in turn depends on the financial situation of each state. In addition, there was a statistical trend toward greater difficulty in accessing or releasing steroids in the Northeast. Unlike immunosuppressants and biological therapy, steroids are available in pharmacies of basic health units and their distribution is made by the Federal Government. Therefore, theoretically, this difference should not exist. This can be considered a region-specific problem. Also in the South region, there was a statistical trend toward lower difficulty in the access and release of 6-mercaptopurine and methotrexate, which may reflect a better functioning of the SESs in the states of this region, specifically with regard to these medications.
With regard to UC care, the response behavior from the Center-West region showed differences, as did that from the Northeast and South regions. Physicians from the Center-West region reported less difficulty in accessing or releasing biologics, although the percentage was yet high (80%). No difference was found in the policy of biologics supply, either in the SUS or in the private system, that could justify this difference. Differences between medical coverage may help explain this difference. The physicians from the Northeast region reported difficulty in accessing or releasing immunosuppressants and steroids, and the physicians from the South region reported difficulty in accessing or releasing biological medicines (100%). The motives were the same as those mentioned in the previous paragraph.
In terms of interdisciplinarity, the Northeast behaved differently from the rest of the country, because the reports show greater difficulty in referring patients to surgical and nursing professionals. Different social contexts may explain the results.
The analysis of the variable “difficulty in accessing complementary exams” showed that physicians from the North region had greater difficulty in performing routine laboratory tests, serum markers of inflammation, CT enterography, colonoscopy and anatomopathological examinations. Although the number of replies was small44. Kotze PG, Underwood FE, Damião AOMC, Ferraz JGP, Saad-Hossne R, et al. Progression of inflammatory bowel diseases throughout latin america and the caribbean: a systematic review. Clin Gastroenterol Hepatol. 2020;18:304-12., this probably shows an important regional inequality in this regard. Other more subtle differences among regions were also detected, including a statistical trend toward lower difficulty in using screening tests for tuberculosis in the Southeast region and a statistical trend toward greater difficulty in performing tuberculosis tests and lower difficulty in performing MRI enterography in the Center-West region. Such differences should be treated as anedoctal results. Regarding the PPD test, only a few regions may have felt more intensely the unavailability of this exam in the country. The lower difficulty in performing MRI enterography may be related to a higher number of patients with health insurance plans; however, it was not an aim of the study to make this assessment.
In relation to data for the variable “preferred subjects or topics to be further discussed” allow concluding that the demand for discussion was greater among physicians in the Center-West region, that physicians in the Southeast region demand less to discuss the topic “Biological treatment-indication, and that the demand to discuss the topics “Pregnancy and Lactation” and “Elderly” is lower among physicians from the South region.
In conclusion, some results should be interpreted with caution considering the design of the study. In addition, certain data may not have specific explanations other than those related to regional differences per se. The objective of this questionnaire was to describe the care of patients with IBD in Brazil and to assess the demands of physicians, without using any government official data. The medical perspective should be valued, because these professionals face obstacles and difficulties in their daily practice of medicine in Brazil. These results may also be useful for the adoption of measures by the government and non-governmental associations to improve this scenario. Several problems were reported, but perhaps the most important one was related to the difficulty in accessing or releasing medicines. High difficulty rates were not solely related to biological therapy. This was a serious problem reported by physicians, which compromises the quality of patient treatment. Moreover, regional differences were expected, which were confirmed by some results, especially through the responses of physicians from the North and Northeast regions.
Finally, the data obtained through this study should be compared with future data. Initiatives such as the present study are useful not only for other medical associations and the government but also for the Brazilian society as a whole.
REFERENCES
-
1Gionchetti P, Dignass A, Danese S, Magro Dias FJ, Rogler G, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 2: Surgical management and special situations. J. Crohn’s Colitis. 2017;11:135-49.
-
2Gomollón F, Dignass A, Annese V, Tilg H, Van Assche G, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 1: Diagnosis and medical management. J. Crohn’s Colitis . 2017;11:3-25.
-
3Magro F, Gionchetti P, Eliakim R, Ardizzone S, Armuzzi A, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: Definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J. Crohn’s Colitis . 2017;11:649-70.
-
4Kotze PG, Underwood FE, Damião AOMC, Ferraz JGP, Saad-Hossne R, et al. Progression of inflammatory bowel diseases throughout latin america and the caribbean: a systematic review. Clin Gastroenterol Hepatol. 2020;18:304-12.
-
5Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140:1785-94.
-
6Frolkis AD, Dykeman J, Negrón ME, Debruyn J, Jette N, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013;145:996-1006.
-
7De Dombal FT, Watts JM, Watkinson G, Goligher JC. Local complications of ulcerative colitis: stricture, pseudopolyposis, and carcinoma of colon and rectum. Br Med J. 1966;1:1442-7.
-
8Rutter MD, Saunders BP, Wilkinson KH, Rumbles S, Schofield G, et al. Thirty-year analysis of a colonoscopic surveillance program for neoplasia in ulcerative colitis. Gastroenterology. 2006;130:1030-8.
-
9Peyrin-Biroulet L, Sandborn W, Sands BE, Reinisch W, Bemelman W. Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE): determining Therapeutic Goals for Treat-to-Target. Am J Gastroenterol. 2015;110:1324-38.
-
10Demografia Médica: Brasil possui médicos ativos com CRM em quantidade suficiente para atender demandas da população. Conselho Federal de Medicina, Brasília, 26 de Novembro de 2018. Disponível em: Disponível em: https://amb.org.br/wp-content/uploads/2018/03/DEMOGRAFIA-M%C3%89DICA.pdf Acesso em 21 de fevereiro de 2020.
» https://amb.org.br/wp-content/uploads/2018/03/DEMOGRAFIA-M%C3%89DICA.pdf -
11Recorte Demográfico da Residência Médica Brasileira em 2019. Revista Consensus, Brasília, Edição 32; 2019. [Internet]. [Access 2020 February 21]. Available from: Available from: http://www.conass.org.br/consensus/recorte-demografico-da-residencia-medica-brasileira-em-2019/
» http://www.conass.org.br/consensus/recorte-demografico-da-residencia-medica-brasileira-em-2019/ -
12Maciel Filho R, Pierantoni CR. O médico e o mercado de trabalho em saúde no Brasil: revendo conceitos e mudanças. Observatório de Recursos Humanos em Saúde no Brasil. Estudos e Análises - Volume 2. 2013;139-62.
-
13Protocolo Clínico e Diretrizes Terapêuticas - Doença de Crohn. Portaria nº 858 de 12 de novembro de 2002. [Internet]. [Access 2020 February 21]. Available from: https://portalarquivos2.saude.gov.br/images/pdf/2014/abril/02/pcdt-doenca-de-crohn-2010.pdf
» https://portalarquivos2.saude.gov.br/images/pdf/2014/abril/02/pcdt-doenca-de-crohn-2010.pdf -
14Portaria Conjunta Nº 14, de 28 de Novembro De 2017. Protocolo Clínico de Diretrizes Terapêuticas - Doença De Crohn. [Internet]. [Access 2020 February 22]. Available from: http://conitec.gov.br/images/Protocolos/Portaria_Conjunta_14_PCDT_Doenca_de_Crohn_28_11_2017.pdf
» http://conitec.gov.br/images/Protocolos/Portaria_Conjunta_14_PCDT_Doenca_de_Crohn_28_11_2017.pdf -
15Consultas - Anvisa - Agência Nacional de Vigilância Sanitária. Vedolizumabe. [Internet]. [Access 2020 February 22]. Available from: https://consultas.anvisa.gov.br/#/medicamentos/25351596045201401/?substancia=25770
» https://consultas.anvisa.gov.br/#/medicamentos/25351596045201401/?substancia=25770 -
16Consultas - Anvisa - Agência Nacional de Vigilância Sanitária. Ustequinumabe. [Internet]. [Access 2020 February 22]. Available from: https://consultas.anvisa.gov.br/#/medicamentos/25351630200200806/?substancia=25220
» https://consultas.anvisa.gov.br/#/medicamentos/25351630200200806/?substancia=25220 -
17Nota Técnica nº 196/2017; Nota Técnica nº 204/2017; Revisão do Rol de Procedimentos e Eventos em Saúde - 2018 Processo nº 33902.440494/2016-22. [Internet]. [Access 2020 February 22]. Available from: http://www.ans.gov.br/images/stories/ Particitacao_da_sociedade/consultas_publicas/cp61/cp61_relatorio_nota_tecnica_ 204_2017.pdf
» http://www.ans.gov.br/images/stories/ Particitacao_da_sociedade/consultas_publicas/cp61/cp61_relatorio_nota_tecnica_ 204_2017.pdf -
18Protocolo Clinico e Diretrizes Terapêuticas - Retocolite ulcerativa. Portaria SAS/MS nº 861, [Internet]. [Access 2002 November 4]. Available from: Available from: http://bvsms.saude.gov.br/bvs/publicacoes/protocolo_clinico_diretrizes_terapeuticas_retocolite_ulcerativa.pdf Acesso em 22 de fevereiro de 2020.
» http://bvsms.saude.gov.br/bvs/publicacoes/protocolo_clinico_diretrizes_terapeuticas_retocolite_ulcerativa.pdf -
19Residência multiprofissional. [Internet]. [Access 2020 February 22]. Available from: http://portal.mec.gov.br/residencias-em-residencia-multiprofissional
» http://portal.mec.gov.br/residencias-em-residencia-multiprofissional -
20Nota conjunta sobre indisponibilidade temporária do PPD. São Paulo, 06 de fevereiro de 2020. [Internet]. [Access 2020 February 23]. Available from: Available from: https://www.reumatologia.org.br/site/wp-content/uploads/2020/02/Nota-Tecnica.-Assinada-PPD.03.fev2020.pdf
» https://www.reumatologia.org.br/site/wp-content/uploads/2020/02/Nota-Tecnica.-Assinada-PPD.03.fev2020.pdf -
21Burger D, Travis S. Conventional Medical Management of Inflammatory Bowel Disease. Gastroenterology. 2011;140:1827-37.
-
Disclosure of funding: no funding received
Publication Dates
-
Publication in this collection
11 Dec 2020 -
Date of issue
Oct-Dec 2020
History
-
Received
25 Apr 2020 -
Accepted
11 June 2020