ABSTRACT
BACKGROUND:
As age advances, a higher burden of comorbidities and less functional reserve are expected, however, the impact of aging in the surgical outcomes of gastric cancer (GC) patients is unknown.
OBJECTIVE:
The aim of this study is to evaluate surgical outcomes of GC patients according to their age group.
METHODS:
Patients submitted to gastrectomy with curative intent due to gastric adenocarcinoma were divided in quartiles. Each group had 150 patients and age limits were: ≤54.8, 54.9-63.7, 63.8-72, >72. The outcomes assessed were: postoperative complications (POC), 90-day postoperative mortality, disease-free survival (DFS) and overall survival (OS).
RESULTS:
Major surgical complications were 2.7% in the younger quartile vs 12% for the others (P=0.007). Major clinical complications raised according to the age quartile: 0.7% vs 4.7% vs 5.3% vs 7.3% (P<0.042). ASA score and age were independent risk factors for major POC. The 90-day mortality progressively increased according to the age quartile: 1.3% vs 6.0% vs 7.3% vs 14% (P<0.001). DFS was equivalent among quartile groups, while OS was significantly worse for those >72-year-old. D2 lymphadenectomy only improved OS in the three younger quartiles. Age >72 was an independent risk factor for worse OS (hazard ratio of 1.72).
CONCLUSION:
Patients <55-year-old have less surgical complications. As age progresses, clinical complications and 90-day mortality gradually rise. OS is worse for those above age 72, and D2 lymphadenectomy should be individualized after this age.
HEADINGS:
Stomach neoplasms; Aging; Survival; Postoperative complication; Gastrectomy
RESUMO
CONTEXTO:
Conforme a idade avança, se esperam mais morbidades e menor reserva funcional. Entretanto não está claro qual o impacto do envelhecimento nos resultados cirúrgicos do câncer gástrico (CaG).
OBJETIVO:
O intuito deste estudo é avaliar os resultados cirúrgicos de pacientes com CaG de acordo com o grupo etário.
MÉTODOS:
Pacientes submetidos a gastrectomia por adenocarcinoma gástrico com intuito curativo foram divididos em quartis. Cada grupo incluiu 150 indivíduos e os limites etários foram: ≤54,8; 54,9-63,7; 63,8-72; >72. Os resultados avaliados foram: complicações pós-operatórias (CPO), mortalidade em 90 dias, sobrevida livre de doença (SLD) e sobrevida global (SG).
RESULTADOS:
Complicações cirúrgicas maiores ocorreram em 2,7% dos pacientes no quartil mais jovem vs 12% para os demais (P=0,007). A incidência de complicações clínicas maiores aumentou conforme o quartil: 0,7% vs 4,7% vs 5,3% vs 7,3% (P<0,042). A pontuação ASA e a idade foram fatores de risco independentes para CPO maiores. A mortalidade em 90 dias aumentou progressivamente conforme o quartil etário: 1,3% vs 6,0% vs 7,3% vs 14% (P<0,001). A SLD foi equivalente entre os quartis, enquanto a SG foi significativamente pior para os >72 anos de idade. Linfadenectomia D2 aumentou a SG apenas para os 3 quartis mais jovens. Idade > 72 foi fator independente de risco para pior SG (razão de chances de 1,72)
CONCLUSÃO:
Pacientes < 55 anos tem menos complicações cirúrgicas. Conforme a idade avança, as complicações clínicas e a mortalidade em 90 dias aumenta gradualmente. A SG é pior se >72 anos e a indicação de linfadenectomia D2 deve ser individualizada a partir dessa idade.
DESCRITORES:
Neoplasias gástricas; Envelhecimento; Sobrevida; Complicações pós-operatórias; Gastrectomia
INTRODUCTION
Although the incidence of gastric cancer (GC) is slowly diminishing, it remains as one of the most common and lethal neoplasms in the world11. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2018;68:394-424. doi:10.3322/caac.21492
https://doi.org/10.3322/caac.21492...
. Surgical resection remains as the main treatment and it is a morbid procedure even in reference centers22. Ramos M, Pereira MA, Yagi OK, Dias AR, Charruf AZ, Oliveira RJ, et al. Surgical treatment of gastric cancer: a 10-year experience in a high-volume university hospital. Clinics (Sao Paulo, Brazil). 2018;73 (Suppl 1):e543s. doi:10.6061/clinics/2018/e543s
https://doi.org/10.6061/clinics/2018/e54...
3. Baiocchi GL, Marrelli D, Verlato G, Morgagni P, Giacopuzzi S, Coniglio A, et al. Follow-up after gastrectomy for cancer: an appraisal of the Italian research group for gastric cancer. Ann Surg Oncol. 2014;21:2005-11. doi:10.1245/s10434-014-3534-8
https://doi.org/10.1245/s10434-014-3534-...
4. Nashimoto A, Akazawa K, Isobe Y, Miyashiro I, Katai H, Kodera Y, et al. Gastric cancer treated in 2002 in Japan: 2009 annual report of the JGCA nationwide registry. Gastric Cancer. 2013;16:1-27. doi:10.1007/s10120-012-0163-4
https://doi.org/10.1007/s10120-012-0163-...
-55. Norero E, Vega EA, Diaz C, Cavada G, Ceroni M, Martinez C, et al. Improvement in postoperative mortality in elective gastrectomy for gastric cancer: Analysis of predictive factors in 1066 patients from a single centre. Eur J Surg Oncol. 2017;43:1330-6. doi:10.1016/j.ejso.2017.01.004
https://doi.org/10.1016/j.ejso.2017.01.0...
. The disease is mostly diagnosed at late age (64 and above) and with life expectancy increasing globally, gastrectomy in elder patients is expected to grow. As age advances, a higher burden of comorbidities and less functional reserve are expected66. Ramos MFKP, Pereira MA, Dias AR, Yagi OK, Zaidan EP, Ribeiro-Júnior U, et al. Surgical outcomes of gastrectomy with D1 lymph node dissection performed for patients with unfavorable clinical conditions. Eur J Surg Oncol . 2019;45:460-5. doi:10.1016/j.ejso.2018.11.013
https://doi.org/10.1016/j.ejso.2018.11.0...
, however, the impact of aging in the surgical outcomes of gastric cancer patients is unknown. Is there an age-specific risk? An age limit where D2 lymphadenectomy should not be performed? Perhaps the clinical performance is more important than age itself.
The purpose of this paper was to evaluate how aging affects the surgical outcomes of GC patients submitted to gastrectomy with curative intent.
METHODS
This is a retrospective cohort study from a single institution. Data came from prospective database. All patients submitted to gastrectomy with curative intent (D1 or D2 lymphadenectomy) due to gastric adenocarcinoma between 2009 and 2019 were considered for inclusion. Those operated in urgency or with metastatic disease in the pathology report were excluded.
Patients were divided in quartiles, the 4 age groups were: young age (YA), lower intermediate (LI), higher intermediate (HI) and advanced age (AA). Their characteristics, laboratorial and radiologic exams, pathologic report and follow-up were revised. Pre-operative laboratory tests were considered. Comorbidities were classified with the Charlson Comorbidity Index (CCI)77. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-83. (GC was not considered in the score), American Society of Anesthesiologists Classification (ASA)88. Doyle DJ, Goyal A, Bansal P, Garmon EH (2017) American Society of Anesthesiologists Classification (ASA Class). In: StatPearls. StatPearls Publishing LLC., Treasure Island FL. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441940/
https://www.ncbi.nlm.nih.gov/books/NBK44...
was used for preoperative clinical performance assessment. Surgery and lymphadenectomy were performed according to the Japanese guidelines99. Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1-19. doi:10.1007/s10120-016-0622-4
https://doi.org/10.1007/s10120-016-0622-...
, the specimen was fixed in Carnoy’s solution1010. Dias AR, Pereira MA, Mello ES, Zilberstein B, Cecconello I, Ribeiro Junior U. Carnoy’s solution increases the number of examined lymph nodes following gastrectomy for adenocarcinoma: a randomized trial. Gastric Cancer. 2016;19:136-42. doi:10.1007/s10120-014-0443-2
https://doi.org/10.1007/s10120-014-0443-...
and the 8th edition of the TNM used for staging1111. Ajani JA, In H, Sano T, Gaspar LE, Erasmus JJ, Tang LH, et al. American Joint Committee on Cancer (AJCC). Cancer Staging Manual. 8th edition. Stomach. Springer. 2017;17:203-20..
Postoperative complications were classified as minor and major (>II)1212. Dindo D, Demartines N, Clavien P-A. Classification of Surgical Complications. Ann Surg. 2004;240:205-13. doi:10.1097/01.sla.0000133083.54934.ae
https://doi.org/10.1097/01.sla.000013308...
and divided in surgical (directly related to the surgical procedure) or clinical (indirectly related, e.g.: myocardial infarction, pneumonia, thrombosis). The outcomes assessed were postoperative complications (POC), postoperative surgical mortality (during hospital stay or until 30 days from surgery), 90-day mortality, disease-free survival and overall survival. The 90-day mortality was the chosen parameter to analyze more completely the short-term surgical results1313. Damhuis RA, Wijnhoven BP, Plaisier PW, Kirkels WJ, Kranse R, van Lanschot JJ. Comparison of 30-day, 90-day and in-hospital postoperative mortality for eight different cancer types. Br J Surg. 2012; 99 (8):1149-1154. doi:10.1002/bjs.8813
https://doi.org/10.1002/bjs.8813...
.
Adjuvant or perioperative chemotherapy (CMT) was performed (capecitabine and oxaliplatin/cisplatin or cisplatin and irinotecan or 5-fluorouracil and oxaliplatin) for T3-4 and N+ disease or at the oncologist’s discretion.
This study was approved by the Hospital Ethics Committee and is registered online (www.plataformabrasil.com; CAAE: 30308620.1.0000.0068).
Statistical analysis
For statistical analysis, nominal data will be presented in frequencies with percentages and numerical data in mean with standard deviation. The t test and squared-chi test were used for continuous and categorical variables, respectively.
The association of clinical and surgical variables with the occurrence of 90-day mortality and POC were analyzed by binary logistic regression, and odds ratios (ORs) with 95% confidence interval (95% CI) were calculated.
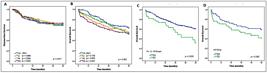
Survival curves were calculated for each quartile group starting at the day of the gastrectomy and estimated with the Kaplan-Meier method. Log-rank test was used to analyze the difference between the curves. Overall survival (OS) was considered from the date of the surgery until death or last follow-up and Disease-free survival (DFS) until disease recurrence or last follow-up.
Cox regression analysis was performed to evaluate prognostic factors associated with survival. A P-value ≤0.05 was considered statistically significant (P-values are two-tailed). Analyses were performed with SPSS version 20.0 (Inc, Chicago, IL, USA).
RESULTS
Among 1,157 patients undergoing surgical treatment for GC, 600 fulfilled the inclusion criteria. The mean age was 62.8 years (range 22.7 to 94.5), 58.7% were male. Subtotal gastrectomy and D2 lymphadenectomy were performed in 64.8% and 83% of cases, respectively. Major POC occurred in 14% of the patients and postoperative mortality was 5.3%.
According to the quartiles, the following age groups were obtained: YA≤54.8, LI=54.9-63.7, HI=63.8-72, AA>72. Table 1 presents the groups characteristics; 150 patients were included in each group. Female patients were more common in the YA group and the frequency of patients with lower hemoglobin and albumin rates increased with age. The groups HI and AA had higher burden of comorbidities and higher ASA score. In relation to surgery, D2 lymphadenectomy and laparoscopic surgery were more frequent in younger groups (YA and LI), while D1 was more frequent in the AA group.
Regarding pathological characteristics (Table 2), Lauren’s diffuse tumors and poorly differentiated histology were more common in the YA group, while intestinal type was predominant in the AA patients. There was no significant difference in pT, pN and pTNM status between groups.
Short-term outcomes
Postoperative outcomes are presented in Table 3. Major complications raised progressively according to the age group. The frequency of major clinical complications according to the age quartile group was: 0.7% vs 4.7% vs 5.3% vs 7.3% (P<0.042). Surgical complications were less frequent in the YA group. Postoperative mortality (Clavien V) increased as age progressed (0.7% vs 4% vs 7.3% vs 9.3%, P=0.005) and the same occurred with 90-day mortality (1.3% vs 6.0% vs 7.3% vs 14%, P<0.001).
The length of hospital stay was higher for older patients; Chemotherapy (perioperative or adjuvant) was administered less frequently as age progressed (p<0.001). Recurrence rate was similar among groups (P=0.588)
Analysis of potential risk factors for POC and 90-day mortality is shown in Table 4. Age groups and ASA were independent risk factors for major POC, while advanced age group and ASA >II were independent risk factors for 90-day mortality.
Survival analysis
In a median follow-up of 31.1 months (mean of 36.9 months), 208 patients died and 129 had disease recurrence. The OS and DFS rates for the entire cohort were 57.2% and 71.4%, respectively.
Among the 129 patients who had recurrence (YA: 37, LI: 34, HI: 30, AA: 29), there was no difference concerning the site of relapse among groups (regional vs peritoneal vs distant). YA patients had one site of relapse in 94.6% of the times vs 73.5% (LI), 70% (HI) and 64.3% (AA) (P=0.019).
DFS was equivalent among quartiles (p=0.91) (Figure 1). Considering OS, the AA group had significantly worse survival compared to the YA (P=0.007); LI and HI patients had similar OS compared to the YA group (P=0.179 and P=0.08, respectively).
OS was studied according to the extent of the lymphadenectomy (Figure 1). Analyzing the 3 younger quartiles together, D2 patients had better survival compared to D1 (P=0.005). In the AA group, there was no significant improvement in OS for patients who underwent D2 lymphadenectomy compared to D1 (P=0.065).
Disease-free survival and overall survival of gastric adenocarcinoma patients operated with curative intent according to their age groups and the extension of the lymphadenectomy.
Univariate and multivariate analysis are showed in Table 5. The type of gastrectomy, histologic type, pT, pN and CMT were factors associated with DFS at the multivariate analysis. For OS, advanced age, ASA III/IV, total gastrectomy, pT3-4 and pN+ were independent risk factors related with worse survival. The hazard ratio for AA group was 1.72 (95%CI 1.15-2.57, P=0.008).
DISCUSSION
The incidence of malignant neoplasms (GC included) increases as age advances. DNA damage and cell exposition to carcinogens accumulate over time1414. Arai T, Takubo K. Clinicopathological and molecular characteristics of gastric and colorectal carcinomas in the elderly. Pathol Int. 2007;57:303-14. doi:10.1111/j.1440-1827.2007.02101.x
https://doi.org/10.1111/j.1440-1827.2007...
. Besides, age-related changes to the DNA repair, immune and endocrine systems may promote or facilitate carcinogenesis1515. Anisimov VN. Carcinogenesis and aging. Adv Cancer Res. 1983;40:365-424. doi:10.1016/s0065-230x(08)60684-3
https://doi.org/10.1016/s0065-230x(08)60...
. With aging comorbidities raise and performance deteriorates. So, theoretically outcomes of a morbid procedure, such as gastrectomy, worsen as age progresses. However, the impact of aging in the results of gastrectomy for GC is poorly addressed in the literature1616. Saito H, Osaki T, Murakami D, Sakamoto T, Kanaji S, Tatebe S, Tsujitani S, Ikeguchi M. Effect of age on prognosis in patients with gastric cancer. ANZ J Surg. 2006;76:458-61. doi:10.1111/j.1445-2197.2006.03756.x
https://doi.org/10.1111/j.1445-2197.2006...
. Two studies from a vast database suggest that older age associates with worse prognosis, however important limitations and bias are observed: information concerning margin status, resections with curative intent, and lymphadenectomy performed are all missing; also lymph node count was very low1717. Song P, Wu L, Jiang B, Liu Z, Cao K, Guan W. Age-specific effects on the prognosis after surgery for gastric cancer: A SEER population-based analysis. Oncotarget. 2016;7:48614-24. doi:10.18632/oncotarget.9548
https://doi.org/10.18632/oncotarget.9548...
,1818. Chen J, Xu Y, Long Z, Zhou Y, Zhu H, Wang Y, Shi Y. Impact of Age on the Prognosis of Operable Gastric Cancer Patients: An Analysis Based on SEER Database. Medicine (Baltimore). 2016;95:e3944. doi:10.1097/MD.0000000000003944
https://doi.org/10.1097/MD.0000000000003...
. Other study included 448 patients and observed that age was an independent risk factor for gastric cancer-specific mortality (GCSM), with age 70-79 being associated with increased GCSM for stages I and II. Patients with stage IV disease, who underwent palliative treatment, and who received support care alone were included. Margins and lymphadenectomy performed and not reported1919. Lee JG, Kim SA, Eun CS, Han DS, Kim YS, Choi BY, et al. Impact of age on stage-specific mortality in patients with gastric cancer: A long-term prospective cohort study. PLoS One. 2019;14:e0220660. doi:10.1371/journal.pone.0220660
https://doi.org/10.1371/journal.pone.022...
.
In our cohort, aging significantly increased complications and shortened OS. Patients in the younger quartile (≤54.8) showed fewer major surgical complications, probably because they are more fit and with superior performance. Major clinical complications, postoperative and 90-day mortalities gradually raised as age quartile increased.
The independent risk factors that related to major POC were ASA score >II (OR: 1.88) and aging; the risk increased progressively according to the age quartile (OR: 4.67 vs 5.08 vs 5.77). The two independent risk factors for 90-day mortality were ASA >II and being in the advanced age quartile. The difference in 90-day mortality between the youngest and eldest was colossal (1.3% vs 14%) and demonstrates the importance of aging in the short-term results. It also indicates that after 72-year-old indication for surgery should be individualized. The 30-day mortality is commonly used to access the surgical risk, we considered the death rate until 90 days to have a better understanding of the surgical and oncological short-term results2020. Damhuis RA, Wijnhoven BP, Plaisier PW, Kirkels WJ, Kranse R, van Lanschot JJ. Comparison of 30-day, 90-day and in-hospital postoperative mortality for eight different cancer types. Br J Surg . 2012;99:1149-54. doi: 10.1002/bjs.8813.
https://doi.org/10.1002/bjs.8813...
.
When we consider the long-term, DFS was not impacted by aging, but OS was worse for those with advanced age. These findings are with agreement with available data2121. Xu Y, Wang Y, Xi C, Ye N, Xu X. Is it safe to perform gastrectomy in gastric cancer patients aged 80 or older?: A meta-analysis and systematic review. Medicine (Baltimore). 2019;98:e16092. doi:10.1097/MD.0000000000016092
https://doi.org/10.1097/MD.0000000000016...
. They also suggest that elders may not live long enough to show oncological benefit after radical procedure. At this moment, few countries in the world have life expectancy above 80-year-old. So, submitting elders who are at their final years to a morbid procedure is a difficult decision, especially when we consider that with aging complications increase and life expectancy shortens. D2 was less performed as age increased demonstrating the concern to limit surgical aggressiveness in elders. Advanced age was an independent risk factor for worse OS and the benefit of D2 lymphadenectomy in this quartile failed to achieve the statistical significance observed in the younger quartiles.
Despite being more aggressive, total gastrectomy did not correlate with major POC or 90-day mortality. However, it was associated with worse DFS and OS. Possible explanations are that compared to subtotal gastrectomy, recovery and nutritional status are more impaired and larger lesions, that have a worse prognosis per se, require total gastrectomy more frequently.
Our study has other interesting findings. As expected, the frequency of diffuse tumors was greater in younger patients2222. Arai T, Esaki Y, Inoshita N, Sawabe M, Kasahara I, Kuroiwa K, Honma N, Takubo K. Pathologic characteristics of gastric cancer in the elderly: a retrospective study of 994 surgical patients. Gastric Cancer. 2004;7:154-9. doi:10.1007/s10120-004-0285-4
https://doi.org/10.1007/s10120-004-0285-...
. Neutrophil lymphocyte ratio (NLR), a prognostic maker in GC, increased with aging suggesting less specific immunological response as age advances2323. Szor DJ, Dias AR, Pereira MA, Ramos MFKP, Zilberstein B, Cecconello I, Ribeiro-Júnior U. Prognostic Role of Neutrophil/Lymphocyte Ratio in Resected Gastric Cancer: A Systematic Review and Meta-analysis. Clinics (Sao Paulo). 2018;73:e360. doi:10.6061/clinics/2018/e360
https://doi.org/10.6061/clinics/2018/e36...
. As age progressed, laparoscopic access and D1 were less frequent, the postoperative length of stay longer, and chemotherapy less used. The two main factors that influenced DFS were pN and pT status; while pN, pT, and advanced age had the greatest impact in OS.
Although data collection was prospective, our study has the limitations of its retrospective nature. Another limitation is the fact that, as expected, older patients received CMT less frequently. On the other hand, it is the first time that aging is correlated with the short-term outcomes, and that only patients submitted to potential curative resection were included in the cohort. Also, perioperative care and surgical technique changed significantly over the last decades, we considered a recent time frame from a unique center to make the cohort more uniform.
CONCLUSION
Patients younger than age 55 have less surgical complications. As age progresses clinical complications and 90-day mortality gradually rise. DFS is not impacted by aging, while OS is worse for those above age 72. Also, D2 dissection should be indicated with caution for those older than 72 years.
REFERENCES
-
1Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2018;68:394-424. doi:10.3322/caac.21492
» https://doi.org/10.3322/caac.21492 -
2Ramos M, Pereira MA, Yagi OK, Dias AR, Charruf AZ, Oliveira RJ, et al. Surgical treatment of gastric cancer: a 10-year experience in a high-volume university hospital. Clinics (Sao Paulo, Brazil). 2018;73 (Suppl 1):e543s. doi:10.6061/clinics/2018/e543s
» https://doi.org/10.6061/clinics/2018/e543s -
3Baiocchi GL, Marrelli D, Verlato G, Morgagni P, Giacopuzzi S, Coniglio A, et al. Follow-up after gastrectomy for cancer: an appraisal of the Italian research group for gastric cancer. Ann Surg Oncol. 2014;21:2005-11. doi:10.1245/s10434-014-3534-8
» https://doi.org/10.1245/s10434-014-3534-8 -
4Nashimoto A, Akazawa K, Isobe Y, Miyashiro I, Katai H, Kodera Y, et al. Gastric cancer treated in 2002 in Japan: 2009 annual report of the JGCA nationwide registry. Gastric Cancer. 2013;16:1-27. doi:10.1007/s10120-012-0163-4
» https://doi.org/10.1007/s10120-012-0163-4 -
5Norero E, Vega EA, Diaz C, Cavada G, Ceroni M, Martinez C, et al. Improvement in postoperative mortality in elective gastrectomy for gastric cancer: Analysis of predictive factors in 1066 patients from a single centre. Eur J Surg Oncol. 2017;43:1330-6. doi:10.1016/j.ejso.2017.01.004
» https://doi.org/10.1016/j.ejso.2017.01.004 -
6Ramos MFKP, Pereira MA, Dias AR, Yagi OK, Zaidan EP, Ribeiro-Júnior U, et al. Surgical outcomes of gastrectomy with D1 lymph node dissection performed for patients with unfavorable clinical conditions. Eur J Surg Oncol . 2019;45:460-5. doi:10.1016/j.ejso.2018.11.013
» https://doi.org/10.1016/j.ejso.2018.11.013 -
7Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-83.
-
8Doyle DJ, Goyal A, Bansal P, Garmon EH (2017) American Society of Anesthesiologists Classification (ASA Class). In: StatPearls. StatPearls Publishing LLC., Treasure Island FL. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441940/
» https://www.ncbi.nlm.nih.gov/books/NBK441940/ -
9Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1-19. doi:10.1007/s10120-016-0622-4
» https://doi.org/10.1007/s10120-016-0622-4 -
10Dias AR, Pereira MA, Mello ES, Zilberstein B, Cecconello I, Ribeiro Junior U. Carnoy’s solution increases the number of examined lymph nodes following gastrectomy for adenocarcinoma: a randomized trial. Gastric Cancer. 2016;19:136-42. doi:10.1007/s10120-014-0443-2
» https://doi.org/10.1007/s10120-014-0443-2 -
11Ajani JA, In H, Sano T, Gaspar LE, Erasmus JJ, Tang LH, et al. American Joint Committee on Cancer (AJCC). Cancer Staging Manual. 8th edition. Stomach. Springer. 2017;17:203-20.
-
12Dindo D, Demartines N, Clavien P-A. Classification of Surgical Complications. Ann Surg. 2004;240:205-13. doi:10.1097/01.sla.0000133083.54934.ae
» https://doi.org/10.1097/01.sla.0000133083.54934.ae -
13Damhuis RA, Wijnhoven BP, Plaisier PW, Kirkels WJ, Kranse R, van Lanschot JJ. Comparison of 30-day, 90-day and in-hospital postoperative mortality for eight different cancer types. Br J Surg. 2012; 99 (8):1149-1154. doi:10.1002/bjs.8813
» https://doi.org/10.1002/bjs.8813 -
14Arai T, Takubo K. Clinicopathological and molecular characteristics of gastric and colorectal carcinomas in the elderly. Pathol Int. 2007;57:303-14. doi:10.1111/j.1440-1827.2007.02101.x
» https://doi.org/10.1111/j.1440-1827.2007.02101.x -
15Anisimov VN. Carcinogenesis and aging. Adv Cancer Res. 1983;40:365-424. doi:10.1016/s0065-230x(08)60684-3
» https://doi.org/10.1016/s0065-230x(08)60684-3 -
16Saito H, Osaki T, Murakami D, Sakamoto T, Kanaji S, Tatebe S, Tsujitani S, Ikeguchi M. Effect of age on prognosis in patients with gastric cancer. ANZ J Surg. 2006;76:458-61. doi:10.1111/j.1445-2197.2006.03756.x
» https://doi.org/10.1111/j.1445-2197.2006.03756.x -
17Song P, Wu L, Jiang B, Liu Z, Cao K, Guan W. Age-specific effects on the prognosis after surgery for gastric cancer: A SEER population-based analysis. Oncotarget. 2016;7:48614-24. doi:10.18632/oncotarget.9548
» https://doi.org/10.18632/oncotarget.9548 -
18Chen J, Xu Y, Long Z, Zhou Y, Zhu H, Wang Y, Shi Y. Impact of Age on the Prognosis of Operable Gastric Cancer Patients: An Analysis Based on SEER Database. Medicine (Baltimore). 2016;95:e3944. doi:10.1097/MD.0000000000003944
» https://doi.org/10.1097/MD.0000000000003944 -
19Lee JG, Kim SA, Eun CS, Han DS, Kim YS, Choi BY, et al. Impact of age on stage-specific mortality in patients with gastric cancer: A long-term prospective cohort study. PLoS One. 2019;14:e0220660. doi:10.1371/journal.pone.0220660
» https://doi.org/10.1371/journal.pone.0220660 -
20Damhuis RA, Wijnhoven BP, Plaisier PW, Kirkels WJ, Kranse R, van Lanschot JJ. Comparison of 30-day, 90-day and in-hospital postoperative mortality for eight different cancer types. Br J Surg . 2012;99:1149-54. doi: 10.1002/bjs.8813.
» https://doi.org/10.1002/bjs.8813 -
21Xu Y, Wang Y, Xi C, Ye N, Xu X. Is it safe to perform gastrectomy in gastric cancer patients aged 80 or older?: A meta-analysis and systematic review. Medicine (Baltimore). 2019;98:e16092. doi:10.1097/MD.0000000000016092
» https://doi.org/10.1097/MD.0000000000016092 -
22Arai T, Esaki Y, Inoshita N, Sawabe M, Kasahara I, Kuroiwa K, Honma N, Takubo K. Pathologic characteristics of gastric cancer in the elderly: a retrospective study of 994 surgical patients. Gastric Cancer. 2004;7:154-9. doi:10.1007/s10120-004-0285-4
» https://doi.org/10.1007/s10120-004-0285-4 -
23Szor DJ, Dias AR, Pereira MA, Ramos MFKP, Zilberstein B, Cecconello I, Ribeiro-Júnior U. Prognostic Role of Neutrophil/Lymphocyte Ratio in Resected Gastric Cancer: A Systematic Review and Meta-analysis. Clinics (Sao Paulo). 2018;73:e360. doi:10.6061/clinics/2018/e360
» https://doi.org/10.6061/clinics/2018/e360
-
Disclosure of funding: no funding received
Publication Dates
-
Publication in this collection
23 Apr 2021 -
Date of issue
Jan-Mar 2021
History
-
Received
11 Sept 2020 -
Accepted
27 Oct 2020