ABSTRACT
BACKGROUND:
In the world, around 450,000 new cases of esophageal cancer are diagnosed each year.
OBJECTIVE:
To evaluate the trend of esophageal cancer mortality rates in Brazil between 1990-2017.
METHODS:
A time series study using data on mortality from esophageal cancer in residents ≥30 years in Brazil from 1990 to 2017. Data was estimated by the Global Burden of Disease (GBD) study and analyzed according to sex, age group and federal unit of Brazil. The standardized rates according to age were calculated by the direct method using the standard GBD world population. Annual average percentage change and 95% confidence interval (95% CI) were calculated for mortality by Joinpoint regression.
RESULTS:
The age-standardized mortality rate in males was 20.6 in 1990 and 17.6/100,000 in 2017, increasing according to age, being 62.4 (1990) and 54.7 (2017) for ≥70 years. In women, the age-standardized mortality rate was 5.9 in 1990 and 4.2/100,000 in 2017. There was a reduction in mortality rates in all age groups and both sexes with great variation among the states.
CONCLUSION:
Despite the high mortality rates for esophageal cancer in Brazil, the trend was decreasing, but with regional differences. Mortality was around four times higher in men.
HEADINGS:
Esophageal neoplasms; Global burden of disease; Mortality; Epidemiological studies
RESUMO
CONTEXTO
- No mundo, cerca de 450.000 novos casos de câncer de esôfago são diagnosticados a cada ano.
OBJETIVO:
Avaliar a tendência das taxas de mortalidade por câncer de esôfago no Brasil entre 1990-2017.
MÉTODOS:
Estudo de série temporal utilizando dados de mortalidade por câncer de esôfago em residentes ≥30 anos no Brasil de 1990 a 2017. Os dados foram estimados pelo estudo Global Burden of Disease (GBD) e analisados segundo sexo, faixa etária e unidade federal de Brasil. As taxas padronizadas de acordo com a idade foram calculadas pelo método direto usando a população mundial padrão do GBD. Mudança percentual média anual e intervalo de confiança de 95% (IC 95%) foram calculados para mortalidade por regressão de joinpoint.
RESULTADOS:
A taxa de mortalidade padronizada por idade no sexo masculino foi de 20,6 em 1990 e 17,6 / 100.000 em 2017, aumentando conforme a idade, sendo 62,4 (1990) e 54,7 (2017) para ≥70 anos. Nas mulheres, a taxa de mortalidade padronizada por idade foi de 5,9 em 1990 e de 4,2 / 100.000 em 2017. Houve redução das taxas de mortalidade em todas as faixas etárias e em ambos os sexos com grande variação entre os estados.
CONCLUSÃO:
Apesar das altas taxas de mortalidade por câncer de esôfago no Brasil, a tendência é decrescente, mas com diferenças regionais. A mortalidade foi cerca de quatro vezes maior nos homens.
DESCRITORES:
Neoplasias esofágicas; Carga global da doença; Mortalidade; Estudos epidemiológicos
INTRODUCTION
In the world, around 450,000 new cases of esophageal cancer are diagnosed every year11. Tatarian T, Palazzo F. Chapter 35 − Epidemiology, Risk Factors, and Clinical Manifestations of Esophageal Cancer. In: Yeo CJ, editor. Shackelford’s Surgery of the Alimentary Tract. 2 vol. 8th ed.. Philadelphia: Elsevier; 2019. p. 362-7. Available from: Available from: http://www.sciencedirect.com/science/article/pii/B9780323402323000352 . Accessed in 2020 (Jun 16).
http://www.sciencedirect.com/science/art...
. These incidences have been growing rapidly22. Simard EP, Ward EM, Siegel R, Jemal A. Cancers with increasing incidence trends in the United States: 1999 through 2008. CA Cancer J Clin. 2012;62:118-28. doi: 10.3322/caac.20141.
https://doi.org/10.3322/caac.20141...
,33. Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol. 2013;19:5598-606. doi: 10.3748/wjg.v19.i34.5598.
https://doi.org/10.3748/wjg.v19.i34.5598...
. The estimative for 2018 indicated that it is ranked number seven as the cancer with the most incidents and the sixth biggest cause of death by cancer in the world44. World Health Organization. International Agency of Research on Cancer. Global Cancer Observatory. Cancer Today. 2018. [Accessed 2020 June 16]. Available from: Available from: https://gco.iarc.fr/ .
https://gco.iarc.fr/...
. In Brazil, 11,405 new cases of esophageal cancer were registered and 9,761 deaths, of which 7,645 (78%) were men44. World Health Organization. International Agency of Research on Cancer. Global Cancer Observatory. Cancer Today. 2018. [Accessed 2020 June 16]. Available from: Available from: https://gco.iarc.fr/ .
https://gco.iarc.fr/...
. In 2015, it was the fifth largest cause of death in male patients55. Guerra MR, Bustamante-Teixeira MT, Corrêa CSL, et al. [Magnitude and variation of the burden of cancer mortality in Brazil and Federation Units, 1990 and 2015]. [Article in Portuguese, En]. Rev Bras Epidemiol. 2017;20(Suppl 1):102-15. doi: 10.1590/1980-5497201700050009.
https://doi.org/10.1590/1980-54972017000...
. Studies point to differences regarding the histological type66. Coleman HG, Xie SH, Lagergren J. The Epidemiology of Esophageal Adenocarcinoma. Gastroenterology. 2018;154:390-405. doi: 10.1053/j.gastro.2017.07.046.
https://doi.org/10.1053/j.gastro.2017.07...
7. Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of esophageal cancer by histological subtype in 2012. Gut. 2015;64:381-7. doi: 10.1136/gutjnl-2014-308124.
https://doi.org/10.1136/gutjnl-2014-3081...
-88. Huang FL, Yu SJ. Esophageal cancer: Risk factors, genetic association, and treatment. Asian J Surg. 2018;41:210-5. doi: 10.1016/j.asjsur.2016.10.005.
https://doi.org/10.1016/j.asjsur.2016.10...
, with squamous cell carcinoma being the most predominant, especially in South America and Asia99. No authors listed . Esophageal cancer: epidemiology, pathogenesis and prevention. Nat Clin Pract Gastroenterol Hepatol. 2008;5:517-26. doi: 10.1038/ncpgasthep1223.
https://doi.org/10.1038/ncpgasthep1223...
.
The literature indicates a predominance in males with a highest of incidence between the fifth and sixth decade of life11. Tatarian T, Palazzo F. Chapter 35 − Epidemiology, Risk Factors, and Clinical Manifestations of Esophageal Cancer. In: Yeo CJ, editor. Shackelford’s Surgery of the Alimentary Tract. 2 vol. 8th ed.. Philadelphia: Elsevier; 2019. p. 362-7. Available from: Available from: http://www.sciencedirect.com/science/article/pii/B9780323402323000352 . Accessed in 2020 (Jun 16).
http://www.sciencedirect.com/science/art...
,66. Coleman HG, Xie SH, Lagergren J. The Epidemiology of Esophageal Adenocarcinoma. Gastroenterology. 2018;154:390-405. doi: 10.1053/j.gastro.2017.07.046.
https://doi.org/10.1053/j.gastro.2017.07...
. Obesity is cited as a risk factor for esophageal cancer by predisposing to gastroesophageal reflux disease (GERD) and Barrett’s esophagus, a preceding condition to adenocarcinoma66. Coleman HG, Xie SH, Lagergren J. The Epidemiology of Esophageal Adenocarcinoma. Gastroenterology. 2018;154:390-405. doi: 10.1053/j.gastro.2017.07.046.
https://doi.org/10.1053/j.gastro.2017.07...
. Smoking is one of the most important risk factors for squamous cell carcinoma77. Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of esophageal cancer by histological subtype in 2012. Gut. 2015;64:381-7. doi: 10.1136/gutjnl-2014-308124.
https://doi.org/10.1136/gutjnl-2014-3081...
. Besides that, the consumption of alcohol, a high fat diet88. Huang FL, Yu SJ. Esophageal cancer: Risk factors, genetic association, and treatment. Asian J Surg. 2018;41:210-5. doi: 10.1016/j.asjsur.2016.10.005.
https://doi.org/10.1016/j.asjsur.2016.10...
, and the consumption of hot foods are associated with this type of cancer1010. Chen Y, Tong Y, Yang C, Gan Y, Sun H, Bi H, et al. Consumption of hot beverages and foods and the risk of esophageal cancer: a meta-analysis of observational studies. BMC Cancer. 2015;15:449. doi: 10.1186/s12885-015-1185-1.
https://doi.org/10.1186/s12885-015-1185-...
.
Patients with esophageal cancer have a reserved prognosis, in spite of the survival rate increase over the last five years that has been verified in studies, 5% in the 1960s and around 20% in the 2010s1111. Lagergren J, Smyth E, Cunningham D, Lagergren P. Oesophageal cancer. Lancet. 2017;390:2383-96. doi: 10.1016/S0140-6736(17)31462-9.
https://doi.org/10.1016/S0140-6736(17)31...
. In the cases in which the diagnostic is done in the initial phase and due to the advancement of the endoscopic treatment with the minimally invasive technique of resection called endoscopic dissection of the submucosa, the survival in five years reaches 95%1212. Arantes V, Espinoza-Ríos J. [Early esophageal squamous cell carcinoma management through endoscopic submucosal dissection]. [Article in En, Spanish]. Rev Gastroenterol Mex. 2018;83:259-67. doi: 10.1016/j.rgmxen.2018.05.004.
https://doi.org/10.1016/j.rgmxen.2018.05...
. However, more than 30% of patients develop metastasis, lowering the survival rate in five years to 4.5%11. Tatarian T, Palazzo F. Chapter 35 − Epidemiology, Risk Factors, and Clinical Manifestations of Esophageal Cancer. In: Yeo CJ, editor. Shackelford’s Surgery of the Alimentary Tract. 2 vol. 8th ed.. Philadelphia: Elsevier; 2019. p. 362-7. Available from: Available from: http://www.sciencedirect.com/science/article/pii/B9780323402323000352 . Accessed in 2020 (Jun 16).
http://www.sciencedirect.com/science/art...
. Differences in the outcome of treatment, in terms of survivability and recurrence, can be found according histological type, but it also depends on the state of the disease and the treatment done1313. Rustgi AK, El-Serag HB. Esophageal Carcinoma. N Engl J Med. 2014;371:2499-509. doi: 10.1056/NEJMra1314530.
https://doi.org/10.1056/NEJMra1314530...
,1414. Saigí M, Oliva M, Aliste L, Calvo M, Hormigo G, Serra Ò, et al. Clinical relevance of histologic subtypes in locally advanced esophageal carcinoma treated with pre-operative chemoradiotherapy: Experience of a monographic oncologic centre. PLoS One. 2017;12:e0184737. doi: 10.1371/journal.pone.0184737.
https://doi.org/10.1371/journal.pone.018...
.
In Brazil, a study evaluated the mortality of cancer from 1990 until 2015 and estimated a significant reduction of approximately 14% in mortality by esophageal cancer with similar patterns among the states, except for Ceará and Paraíba, both in the Northeast region, which had a significant increase in the last decades55. Guerra MR, Bustamante-Teixeira MT, Corrêa CSL, et al. [Magnitude and variation of the burden of cancer mortality in Brazil and Federation Units, 1990 and 2015]. [Article in Portuguese, En]. Rev Bras Epidemiol. 2017;20(Suppl 1):102-15. doi: 10.1590/1980-5497201700050009.
https://doi.org/10.1590/1980-54972017000...
. On the other hand, another study evaluated the temporal trends of esophageal cancer and reported an increase of incidence between 2005 and 2015, while the death rate remained the same1515. Amorim CA, De Souza LP, Moreira JP, Luiz RR, Carneiro AJV, De Souza HSP. Geographic distribution and time trends of esophageal cancer in Brazil from 2005 to 2015. Mol Clin Oncol. 2019;10:631-8. doi: 10.3892/mco.2019.1842.
https://doi.org/10.3892/mco.2019.1842...
.
Considering the few studies on the subject and the divergence in the data presented, which could be related to the failure in the registering of the cause of death into the information systems, it is expected that the use of estimates which have a data source that was corrected and treated to generate standardized information, as it was done all over the world by the Global Burden of Diseases (GBD) study, can elucidate the epidemiological situation of esophageal cancer in Brazil and in each state. Thus, the objective of this study was to estimate the mortality rate of esophageal cancer in Brazil and in the states of the country and evaluate the tendency between 1990 and 2017.
METHODS
This is a time series study that used data concerning mortality by esophageal cancer (the tenth revision of the International Classification of Diseases, ICD-10: C15) that occurred in residents starting at 30 years old in Brazil, between 1990 and 20171616. World Health Organization. International statistical classification of diseases and related health problems, 10th rev. [Internet]. [Accessed 2020 June 16]. World Health Organization. 1994. Available from: Available from: https://apps.who.int/iris/handle/10665/38450 .
https://apps.who.int/iris/handle/10665/3...
. To do this, applied corrections to the mortality data were done as a correction of death register and the redistribution of incorrectly defined and unspecific codes, i.e. garbage codes, with the purpose of obtaining estimates that are more coherent with the national reality. The estimates were done by the GBD study, coordinated by the Institute of Health Metrics and Evaluation (IHME)1717. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736-88. doi: 10.1016/S0140-6736(18)32203-7.
https://doi.org/10.1016/S0140-6736(18)32...
.
The data referent to the frequency of deaths by esophageal neoplasia was analyzed according to the year and the territory considered in a population that is 30 years old or older. The specific rates were calculated by (30 to 49 years old, 50 to 69 years, and 70 or older), and the standard rate by age (30 years old or older), according to sex and the 26 states of Brazil and the Federal District. The standardized rates according to age were calculated by the direct method using the standard GBD world population1717. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736-88. doi: 10.1016/S0140-6736(18)32203-7.
https://doi.org/10.1016/S0140-6736(18)32...
. The crude and standardized rates of mortality was calculated for 100,000 inhabitants. The average annual percentage of change (AAPC) and the respective 95% confidence intervals (95% CI) were estimated to evaluate the trends of mortality during 1990 and 2017 by use of the Joinpoint Regression Program software1818. National Cancer Institute. Joinpoint Regression Program - Surveillance Research Program. Joinpoint Trend Analysis Software. Statistical methodology and applications branch, Surveillance Research Program. 2019. [Internet]. [Accessed in 2020 June 16]. Available from: Available from: https://surveillance.cancer.gov/joinpoint/ .
https://surveillance.cancer.gov/joinpoin...
, version 4.7.0.0. The AAPC is the weighted average of the angular coefficients of the linear regression, with weights equal to lengths to each segment of the whole interval. An increase or decrease in the trend is statistically significant when different from 0 (P<0.05) and stable when equal to 0 (P>0.05).
This study respected the ethical preconceptions of research and specific Brazilian resolutions. Data was used in an aggregated manner without identifying individuals and causing any damage to them. The GBD study is compliant with the Guidelines for Accurate and Transparent Health Estimates Reporting statement. This study was approved by the Research Ethics Committee of Universidade Federal de Minas Gerais (CAAE no. 62803316.7.0000.5149).
RESULTS
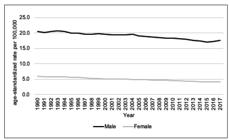
In Brazil, between 1990 and 2017, the highest esophageal cancer mortality rates were ascribed to males (Figure 1). The mortality rates increased with age, thus the largest rates were found for people who were 70 years old or older for both sexes (Figure 2).
Temporal trends in esophageal cancer mortality, according to sex, in Brazil, in the period 1990-2017.
Temporal trends in esophageal cancer mortality, according to sex and age group, in Brazil, in the period 1990-2017.
Among men in Brazil, the mortality rate between 30 and 49 years old (per 100,000 men) was 3.3 in 1990 and 3.0 in 2017, with a reduction of −0.3% per year; between 50 and 69 years old, the rate was 30.9 (1990) and 27.2 (2017) with a reduction of −0.4% per year. The standardized mortality rate according to age (30 years old or older) was 20.6 and 17.6 per 100,000 inhabitants in 1990 and 2017, respectively (Table 1).
The age group between 30 and 49 years old in 11 states, generally located in the Northeast region of Brazil, presented a trend of increase, while four states presented a trend of reduction. Between the ages of 50 and 69, eight states presented an increase and six other states showed a trend of decrease, and were generally located in the South and Southeast regions. Among men 70 years old or older, nine states had a trend of increase and six states had a reduction. To the standardized rate per age (30 years old or older), there was a trend of increase in seven states and a trend of decrease in nine states (Table 1). The increase trend is notable in Rio Grande do Norte and Bahia, among all age groups, as well as the reduction in the state of São Paulo. The trend of increase was verified, in general, in the Northeast region, and the reduction was verified in the states of the South and Southeast regions.
Among women, in Brazil, the mortality rate between 30 and 49 years old (per 100,000 women) was 0.7 in 1990, and 0.6 in 2017, with a reduction of −0.7% per year; in the age group between 50 and 69 years old, the rate was 7.0 (1990) and 5.2 (2017), with a decrease of −1.1% per year; and among 70 years old or older, the rate was 24.0 (1990) and 17.7 (2017), with a decrease of −1.1% per year. The standardized mortality rate by age group was of 5.9 and 4.2 per 100,000 women in 1990 and 2017, respectively (Table 2).
In the age group of 30 and 49 years, 12 states presented a trend of decrease in mortality rate among women. The 50 to 69 years old group in two states in the Northeast region presented an increase, and 17 other states presented a decrease. Among those 70 years old or older, there was an increase trend (in Ceará, in the Northeast region) and 16 states had a reduction trend. At last, the standardized rate according to age (30 years old or older) presented an increase trend in one state (Ceará) and a trend of decrease in 20 states (Table 2).
DISCUSSION
The results of this study point to a reduction in the esophageal cancer rate throughout the country for all age groups, considering that the mortality rates observed of males was approximately four times bigger than females. The reduction of esophageal cancer is in accordance with the findings in rural China and also in some of the countries of Europe, such as France, Switzerland and Denmark, in similar periods1919. Gao X, Wang Z, Kong C, Yang F, Wang Y, Tan X. Trends of Esophageal Cancer Mortality in Rural China from 1989 to 2013: An Age-Period-Cohort Analysis. Int J Environ Res Public Health. 2017;14:218. doi: 10.3390/ijerph14030218.
https://doi.org/10.3390/ijerph14030218...
,2020. Gupta B, Kumar N. Worldwide incidence, mortality and time trends for cancer of the oesophagus. Eur J Cancer Prev. 2017;26:107-18. doi: 10.1097/CEJ.0000000000000249.
https://doi.org/10.1097/CEJ.000000000000...
.
The predominance of males was observed in a global study with ratios varying between 3.3:1 and 7:111. Tatarian T, Palazzo F. Chapter 35 − Epidemiology, Risk Factors, and Clinical Manifestations of Esophageal Cancer. In: Yeo CJ, editor. Shackelford’s Surgery of the Alimentary Tract. 2 vol. 8th ed.. Philadelphia: Elsevier; 2019. p. 362-7. Available from: Available from: http://www.sciencedirect.com/science/article/pii/B9780323402323000352 . Accessed in 2020 (Jun 16).
http://www.sciencedirect.com/science/art...
,2121. Wong MCS, Hamilton W, Whiteman DC, Jiang JY, Qiao Y, Fung FDH, et al. Global Incidence and mortality of oesophageal cancer and their correlation with socioeconomic indicators temporal patterns and trends in 41 countries. Sci Rep. 2018;8:4522. doi: 10.1038/s41598-018-19819-8.
https://doi.org/10.1038/s41598-018-19819...
,2222. Queiroga RC, Pernambuco AP. [Esophageal Cancer: Epidemiology, Diagnosis, and Treatment]. [Internet]. [Accessed in 2020 June 16]. [Article in Portuguese]. Revista Brasileira de Cancerologia. 2006;52:173-8. Available from: https://rbc.inca.gov.br/site/arquivos/n_52/v02/pdf/revisao3.pdf.
https://rbc.inca.gov.br/site/arquivos/n_...
. While the reasons for this predominance may not be entirely known, the greater exposure of men is one of the main risk factors, such as smoking and alcohol consumption2323. West R. Tobacco smoking: Health impact, prevalence, correlates and interventions. Psychol Health. 2017;32:1018-36. doi: 10.1080/08870446.2017.1325890.
https://doi.org/10.1080/08870446.2017.13...
,2424. Abnet CC, Arnold M, Wei WQ. Epidemiology of Esophageal Squamous Cell Carcinoma. Gastroenterology. 2018;154:360-73. doi: 10.1053/j.gastro.2017.08.023.
https://doi.org/10.1053/j.gastro.2017.08...
, which contribute to it. Furthermore, the role of androgen receptors in the pathogenesis of the disease have been studied in order to clarify the predominance of males2525. Sukocheva OA, Li B, Due SL, Hussey DJ, Watson DI. Androgens and esophageal cancer: What do we know?. World J Gastroenterol . 2015;21:6146-56. doi: 10.3748/wjg.v21.i20.6146.
https://doi.org/10.3748/wjg.v21.i20.6146...
. Besides the lower rates, females had the biggest reduction in mortality when compared to males. Such data could be related to the better general health condition of women, considering that women traditionally seek health attention more frequently2626. Malta DC, Bernal RTI, Lima MG, Araújo SSC, Silva MMA, Freitas MIF, et al. [Noncommunicable diseases and the use of health services: analysis of the National Health Survey in Brazil]. [Article in En, Portuguese]. Rev Saude Publica. 2017;51(Suppl 1):4s. doi: 10.1590/s1518-8787.2017051000090.
https://doi.org/10.1590/s1518-8787.20170...
. In spite of the increase of patients seeking health care throughout the years, this increase is bigger among women2727. Nunes BP, Flores TR, Garcia LP, Chiavegatto Filho ADP, Thumé E, Facchini LA. [Time trend of lack of access to health services in Brazil, 1998-2013]. [Article in En, Portuguese]. Epidemiol Serv Saude. 2016;25:777-87. doi: 10.5123/S1679-49742016000400011.
https://doi.org/10.5123/S1679-4974201600...
.
The highest mortality in a given age group was after 70 years of age, as observed in the United States between 2009 and 20132828. Noone AM, Cronin KA, Altekruse SF, Howlader N, Lewis DR, Petkov VI, Penberthy L. Cancer incidence and survival trends by subtype using data from the Surveillance Epidemiology and End Results Program, 1992-2013. Cancer Epidemiol Biomarkers Prev. 2017;26:632-41. doi: 10.1158/1055-9965.EPI-16-0520.
https://doi.org/10.1158/1055-9965.EPI-16...
. This could be related to the cumulative character of the exposure to carcinogenic factors, especially being exposed to smoke in the past. Even though the mortality rate is regressing in this age group, this population is growing significantly with the phenomenon of population aging. It is estimated that in 1980, the population over 60 years old represented about 6% of the total population in Brazil, and that in 2010 this number was close to 11%2929. Miranda GMD, Mendes ACG, Silva ALA da. O envelhecimento populacional brasileiro: desafios e consequências sociais atuais e futuras [Population aging in Brazil: current and future social challenges and consequences]. Rev Bras Geriatr Gerontol. 2016;19:507-19. doi: 10.1590/1809-98232016019.150140.
https://doi.org/10.1590/1809-98232016019...
. In 2017, it was 14.6%3030. Instituto Brasileiro de Geografia e Estatísticas − IBGE. Pesquisa Nacional por Amostra de Domicílios Contínua − PNAD Contínua. Características gerais dos domicílios e dos moradores. 2018. Available from: https://www.ibge.gov.br/estatisticas/sociais/trabalho/17270-pnad-continua.html?edicao=24437&t=resultados. Accessed in 2020 (Jun 16).
https://www.ibge.gov.br/estatisticas/soc...
. Considering this piece of data, the social impact of esophageal cancer tends to increase.
The variability of the incidence rates and esophageal cancer mortality, even in small geographical areas, is described in the literature as an epidemiological characteristic of the disease3131. Soares EO, Mattos IE, Monteiro GTR. Tendência da mortalidade por câncer de esôfago em capitais brasileiras, 1980-2002. Escola Nacional de Saúde Pública Sérgio Arouca (ENSP). 2008. Available from: Available from: http://www6.ensp.fiocruz.br/repositorio/resource/363454 . Accessed in 2020 (Jun 16).
http://www6.ensp.fiocruz.br/repositorio/...
. In this study, the states were analyzed individually and a great disparity in the results was verified, with rates of higher magnitude located in the South of the country and an emphasis in Rio Grande do Sul, which is also the number one state in tobacco consumption3232. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise em Saúde e Vigilância de Doenças não Transmissíveis. Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico, Vigitel 2018. Brasília: Ministério da Saúde; 2019. [Accessed 2020 June 16]. Available from: Available from: http://bvsms.saude.gov.br/bvs/publicacoes/vigitel_brasil_2018_vigilancia_fatores_risco.pdf .
http://bvsms.saude.gov.br/bvs/publicacoe...
. Considering that the consumption of hot drinks is associated with a higher risk of esophageal cancer1010. Chen Y, Tong Y, Yang C, Gan Y, Sun H, Bi H, et al. Consumption of hot beverages and foods and the risk of esophageal cancer: a meta-analysis of observational studies. BMC Cancer. 2015;15:449. doi: 10.1186/s12885-015-1185-1.
https://doi.org/10.1186/s12885-015-1185-...
, another variable that contributes to the high rates of mortality in Rio Grande do Sul is a drink called chimarrão, which is a type of hot herbal tea that is highly consumed in this region.
The mortality rates decreased in the states with a higher development index, which are concentrated in the South and Southeast regions of the country, while less developed states, mainly located in the Northeast region, had an increase in rates. Such facts could be the result of a probable predominance in the carcinoma histological subtype of squamous cells, which have a relationship that is inversely proportional to the human development index2121. Wong MCS, Hamilton W, Whiteman DC, Jiang JY, Qiao Y, Fung FDH, et al. Global Incidence and mortality of oesophageal cancer and their correlation with socioeconomic indicators temporal patterns and trends in 41 countries. Sci Rep. 2018;8:4522. doi: 10.1038/s41598-018-19819-8.
https://doi.org/10.1038/s41598-018-19819...
. Besides that, this type of cancer has demonstrated better survival rates and a lower rate of relapse in comparison to adenocarcinomas1414. Saigí M, Oliva M, Aliste L, Calvo M, Hormigo G, Serra Ò, et al. Clinical relevance of histologic subtypes in locally advanced esophageal carcinoma treated with pre-operative chemoradiotherapy: Experience of a monographic oncologic centre. PLoS One. 2017;12:e0184737. doi: 10.1371/journal.pone.0184737.
https://doi.org/10.1371/journal.pone.018...
. Inequality in the country persists, even though enhancements were verified in the last years2727. Nunes BP, Flores TR, Garcia LP, Chiavegatto Filho ADP, Thumé E, Facchini LA. [Time trend of lack of access to health services in Brazil, 1998-2013]. [Article in En, Portuguese]. Epidemiol Serv Saude. 2016;25:777-87. doi: 10.5123/S1679-49742016000400011.
https://doi.org/10.5123/S1679-4974201600...
. The more developed regions are also those that have better access to quality health services to diagnose and provide the proper treatment to the disease. Additionally, the growing mortality rates in the less developed states agree with studies that show a higher incidence of esophageal cancer in urban and developed areas of the country1515. Amorim CA, De Souza LP, Moreira JP, Luiz RR, Carneiro AJV, De Souza HSP. Geographic distribution and time trends of esophageal cancer in Brazil from 2005 to 2015. Mol Clin Oncol. 2019;10:631-8. doi: 10.3892/mco.2019.1842.
https://doi.org/10.3892/mco.2019.1842...
.
The decrease of mortality in Brazil could be related to the reduction of incidence of the disease, which is related to the decrease of the prevalence of smokers of both sexes in the last decades. The prevalence of smokers 18 years old or older decreased from 43.3% in 1989 to 13.2% in 2017 for men, and 27% to 7.5% for women, in the same period3333. Instituto Nacional do Câncer. Dados e números da prevalência do tabagismo. INCA − Instituto Nacional de Câncer. Observatório da Política Nacional de Controle do Tabaco. 2018. [Accessed 2020 June 16]. Available from: https://www.inca.gov.br/observatorio-da-politica-nacional-de-controle-do-tabaco/dados-e-numeros-prevalencia-tabagismo.
https://www.inca.gov.br/observatorio-da-...
. These results express many regulatory policies that were adopted in the country, such as the ratification, in 2006, of the Framework Convention on Tobacco Control of the World Health Organization3434. Brasil. Presidência da República. Casa Civil. Decreto no 5.658, de 2 de janeiro de 2006. [Accessed 2020 June 16]. Available from: http://www.planalto.gov.br/ccivil_03/_Ato2004-2006/2006/Decreto/D5658.htm.
http://www.planalto.gov.br/ccivil_03/_At...
. Among these implemented policies, the monitoring of the use of tobacco, the increase of taxes in these products, the prohibition of advertisement of tobacco products are highlighted; the law n. 12.546 in 2011 instituted places free of tobacco3535. Brasil. Presidência da República. Casa Civil. Subchefia para Assuntos Jurídicos. Lei nº 12.546, de 14 de dezembro de 2011. [Accessed 2020 June 16]. Available from: http://www.planalto.gov.br/CCIVIL_03/_Ato2011-2014/2011/Lei/L12546.htm.
http://www.planalto.gov.br/CCIVIL_03/_At...
; the decree nº 8.262 in 20143636. Brasil. Presidência da República. Casa Civil. Decreto no 8.262, de 31 de maio de 2014. Altera o Decreto no 2.018, de 1o de outubro de 1996, que regulamenta a Lei no 9.294, de 15 de julho de 1996. [Accessed 2020 June 16]. Available from: http://presrepublica.jusbrasil.com.br/legislacao/121697845/decreto-8262-14.
http://presrepublica.jusbrasil.com.br/le...
, which regulated these ambiances and determined an increase of places with warnings3737. Malta DC, Silva AG, Machado ÍE, De Sá ACMGN, Dos Santos FM, Prates EJS, Cristo EB. Trends in smoking prevalence in all Brazilian capitals between 2006 and 2017. J Bras Pneumol. 2019;45. doi: 10.1590/1806-3713/e20180384.
https://doi.org/10.1590/1806-3713/e20180...
.
Besides the verified advancements in the Brazilian health system, specifically the access to these health services2727. Nunes BP, Flores TR, Garcia LP, Chiavegatto Filho ADP, Thumé E, Facchini LA. [Time trend of lack of access to health services in Brazil, 1998-2013]. [Article in En, Portuguese]. Epidemiol Serv Saude. 2016;25:777-87. doi: 10.5123/S1679-49742016000400011.
https://doi.org/10.5123/S1679-4974201600...
, another factor potentially related to the reduction of mortality is the advancement of medicine regarding the diagnosis and treatment of cancer, such as the target therapy and endoscopic resection of the injury in the initial stages of the disease1212. Arantes V, Espinoza-Ríos J. [Early esophageal squamous cell carcinoma management through endoscopic submucosal dissection]. [Article in En, Spanish]. Rev Gastroenterol Mex. 2018;83:259-67. doi: 10.1016/j.rgmxen.2018.05.004.
https://doi.org/10.1016/j.rgmxen.2018.05...
,3838. Parakh S, Gan HK, Parslow AC, Burvenich IJG, Burgess AW, Scott AM. Evolution of anti-HER2 therapies for cancer treatment. Cancer Treat Rev. 2017;59:1-21. PMID: 28715775; doi: 10.1016/j.ctrv.2017.06.005.
https://doi.org/10.1016/j.ctrv.2017.06.0...
. However, the early diagnosis of esophageal cancer is a challenge in Brazil and in Western countries which lack tracking policies, even in high-risk patients3939. Arantes V, Forero Piñeros EA, Yoshimura K, Toyonaga T. [Advances in the management of early esophageal carcinoma]. Rev Col Bras Cir. 2012;39:534-43. doi: 10.1590/S0100-69912012000600015.
https://doi.org/10.1590/S0100-6991201200...
.
The Global Burden of Disease (GBD) study dealt with the systems databases to obtain more adequate quality data. Among the corrections are those of the underreporting of deaths and redistribution of unspecified causes. This treatment makes available a standardized comparison between places and periods in which the quality indices are heterogeneous. In Brazil, that is not different and this is very useful, considering that the states present diversified situations related to the quality of mortality data. On the other hand, this applied analytic methodology done by the GBD studies have many modeling stages in which it presupposes and coefficient estimates must be elaborated, which results in different data of directly estimates from the national Vital Registration System. In this way, the data analysis done by GBD could be considered limited by the fact that it must accept premises and world inferences which could not be the most adequate to the reality in Brazil, since it did not use crude data registered in information system. However, it is important to note that the GBD study has been amply shared and used by researchers in different themes, bringing to the study the potential of allowing mortality comparisons between different states and regions in Brazil, as well as in other countries.
CONCLUSION
As expected, the esophageal cancer mortality rates increase with age, being higher in the ≥70 years old group. There was a trend to decrease the mortality rate in Brazil during the presented period in every age group and in both sexes, even though differences were identified among the states. In spite of the reduction in mortality rates throughout a significant part of the Brazilian states, these are still elevated when compared to the rest of the world. The expectation is that, with the increase of new therapies and early diagnosis, the impact of the disease will be minimized and the prognostic of the patients improved.
REFERENCES
-
1Tatarian T, Palazzo F. Chapter 35 − Epidemiology, Risk Factors, and Clinical Manifestations of Esophageal Cancer. In: Yeo CJ, editor. Shackelford’s Surgery of the Alimentary Tract. 2 vol. 8th ed.. Philadelphia: Elsevier; 2019. p. 362-7. Available from: Available from: http://www.sciencedirect.com/science/article/pii/B9780323402323000352 Accessed in 2020 (Jun 16).
» http://www.sciencedirect.com/science/article/pii/B9780323402323000352 -
2Simard EP, Ward EM, Siegel R, Jemal A. Cancers with increasing incidence trends in the United States: 1999 through 2008. CA Cancer J Clin. 2012;62:118-28. doi: 10.3322/caac.20141.
» https://doi.org/10.3322/caac.20141 -
3Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol. 2013;19:5598-606. doi: 10.3748/wjg.v19.i34.5598.
» https://doi.org/10.3748/wjg.v19.i34.5598 -
4World Health Organization. International Agency of Research on Cancer. Global Cancer Observatory. Cancer Today. 2018. [Accessed 2020 June 16]. Available from: Available from: https://gco.iarc.fr/
» https://gco.iarc.fr/ -
5Guerra MR, Bustamante-Teixeira MT, Corrêa CSL, et al. [Magnitude and variation of the burden of cancer mortality in Brazil and Federation Units, 1990 and 2015]. [Article in Portuguese, En]. Rev Bras Epidemiol. 2017;20(Suppl 1):102-15. doi: 10.1590/1980-5497201700050009.
» https://doi.org/10.1590/1980-5497201700050009 -
6Coleman HG, Xie SH, Lagergren J. The Epidemiology of Esophageal Adenocarcinoma. Gastroenterology. 2018;154:390-405. doi: 10.1053/j.gastro.2017.07.046.
» https://doi.org/10.1053/j.gastro.2017.07.046 -
7Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of esophageal cancer by histological subtype in 2012. Gut. 2015;64:381-7. doi: 10.1136/gutjnl-2014-308124.
» https://doi.org/10.1136/gutjnl-2014-308124 -
8Huang FL, Yu SJ. Esophageal cancer: Risk factors, genetic association, and treatment. Asian J Surg. 2018;41:210-5. doi: 10.1016/j.asjsur.2016.10.005.
» https://doi.org/10.1016/j.asjsur.2016.10.005 -
9No authors listed . Esophageal cancer: epidemiology, pathogenesis and prevention. Nat Clin Pract Gastroenterol Hepatol. 2008;5:517-26. doi: 10.1038/ncpgasthep1223.
» https://doi.org/10.1038/ncpgasthep1223 -
10Chen Y, Tong Y, Yang C, Gan Y, Sun H, Bi H, et al. Consumption of hot beverages and foods and the risk of esophageal cancer: a meta-analysis of observational studies. BMC Cancer. 2015;15:449. doi: 10.1186/s12885-015-1185-1.
» https://doi.org/10.1186/s12885-015-1185-1 -
11Lagergren J, Smyth E, Cunningham D, Lagergren P. Oesophageal cancer. Lancet. 2017;390:2383-96. doi: 10.1016/S0140-6736(17)31462-9.
» https://doi.org/10.1016/S0140-6736(17)31462-9 -
12Arantes V, Espinoza-Ríos J. [Early esophageal squamous cell carcinoma management through endoscopic submucosal dissection]. [Article in En, Spanish]. Rev Gastroenterol Mex. 2018;83:259-67. doi: 10.1016/j.rgmxen.2018.05.004.
» https://doi.org/10.1016/j.rgmxen.2018.05.004 -
13Rustgi AK, El-Serag HB. Esophageal Carcinoma. N Engl J Med. 2014;371:2499-509. doi: 10.1056/NEJMra1314530.
» https://doi.org/10.1056/NEJMra1314530 -
14Saigí M, Oliva M, Aliste L, Calvo M, Hormigo G, Serra Ò, et al. Clinical relevance of histologic subtypes in locally advanced esophageal carcinoma treated with pre-operative chemoradiotherapy: Experience of a monographic oncologic centre. PLoS One. 2017;12:e0184737. doi: 10.1371/journal.pone.0184737.
» https://doi.org/10.1371/journal.pone.0184737 -
15Amorim CA, De Souza LP, Moreira JP, Luiz RR, Carneiro AJV, De Souza HSP. Geographic distribution and time trends of esophageal cancer in Brazil from 2005 to 2015. Mol Clin Oncol. 2019;10:631-8. doi: 10.3892/mco.2019.1842.
» https://doi.org/10.3892/mco.2019.1842 -
16World Health Organization. International statistical classification of diseases and related health problems, 10th rev. [Internet]. [Accessed 2020 June 16]. World Health Organization. 1994. Available from: Available from: https://apps.who.int/iris/handle/10665/38450
» https://apps.who.int/iris/handle/10665/38450 -
17GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736-88. doi: 10.1016/S0140-6736(18)32203-7.
» https://doi.org/10.1016/S0140-6736(18)32203-7 -
18National Cancer Institute. Joinpoint Regression Program - Surveillance Research Program. Joinpoint Trend Analysis Software. Statistical methodology and applications branch, Surveillance Research Program. 2019. [Internet]. [Accessed in 2020 June 16]. Available from: Available from: https://surveillance.cancer.gov/joinpoint/
» https://surveillance.cancer.gov/joinpoint/ -
19Gao X, Wang Z, Kong C, Yang F, Wang Y, Tan X. Trends of Esophageal Cancer Mortality in Rural China from 1989 to 2013: An Age-Period-Cohort Analysis. Int J Environ Res Public Health. 2017;14:218. doi: 10.3390/ijerph14030218.
» https://doi.org/10.3390/ijerph14030218 -
20Gupta B, Kumar N. Worldwide incidence, mortality and time trends for cancer of the oesophagus. Eur J Cancer Prev. 2017;26:107-18. doi: 10.1097/CEJ.0000000000000249.
» https://doi.org/10.1097/CEJ.0000000000000249 -
21Wong MCS, Hamilton W, Whiteman DC, Jiang JY, Qiao Y, Fung FDH, et al. Global Incidence and mortality of oesophageal cancer and their correlation with socioeconomic indicators temporal patterns and trends in 41 countries. Sci Rep. 2018;8:4522. doi: 10.1038/s41598-018-19819-8.
» https://doi.org/10.1038/s41598-018-19819-8 -
22Queiroga RC, Pernambuco AP. [Esophageal Cancer: Epidemiology, Diagnosis, and Treatment]. [Internet]. [Accessed in 2020 June 16]. [Article in Portuguese]. Revista Brasileira de Cancerologia. 2006;52:173-8. Available from: https://rbc.inca.gov.br/site/arquivos/n_52/v02/pdf/revisao3.pdf
» https://rbc.inca.gov.br/site/arquivos/n_52/v02/pdf/revisao3.pdf -
23West R. Tobacco smoking: Health impact, prevalence, correlates and interventions. Psychol Health. 2017;32:1018-36. doi: 10.1080/08870446.2017.1325890.
» https://doi.org/10.1080/08870446.2017.1325890 -
24Abnet CC, Arnold M, Wei WQ. Epidemiology of Esophageal Squamous Cell Carcinoma. Gastroenterology. 2018;154:360-73. doi: 10.1053/j.gastro.2017.08.023.
» https://doi.org/10.1053/j.gastro.2017.08.023 -
25Sukocheva OA, Li B, Due SL, Hussey DJ, Watson DI. Androgens and esophageal cancer: What do we know?. World J Gastroenterol . 2015;21:6146-56. doi: 10.3748/wjg.v21.i20.6146.
» https://doi.org/10.3748/wjg.v21.i20.6146 -
26Malta DC, Bernal RTI, Lima MG, Araújo SSC, Silva MMA, Freitas MIF, et al. [Noncommunicable diseases and the use of health services: analysis of the National Health Survey in Brazil]. [Article in En, Portuguese]. Rev Saude Publica. 2017;51(Suppl 1):4s. doi: 10.1590/s1518-8787.2017051000090.
» https://doi.org/10.1590/s1518-8787.2017051000090 -
27Nunes BP, Flores TR, Garcia LP, Chiavegatto Filho ADP, Thumé E, Facchini LA. [Time trend of lack of access to health services in Brazil, 1998-2013]. [Article in En, Portuguese]. Epidemiol Serv Saude. 2016;25:777-87. doi: 10.5123/S1679-49742016000400011.
» https://doi.org/10.5123/S1679-49742016000400011 -
28Noone AM, Cronin KA, Altekruse SF, Howlader N, Lewis DR, Petkov VI, Penberthy L. Cancer incidence and survival trends by subtype using data from the Surveillance Epidemiology and End Results Program, 1992-2013. Cancer Epidemiol Biomarkers Prev. 2017;26:632-41. doi: 10.1158/1055-9965.EPI-16-0520.
» https://doi.org/10.1158/1055-9965.EPI-16-0520 -
29Miranda GMD, Mendes ACG, Silva ALA da. O envelhecimento populacional brasileiro: desafios e consequências sociais atuais e futuras [Population aging in Brazil: current and future social challenges and consequences]. Rev Bras Geriatr Gerontol. 2016;19:507-19. doi: 10.1590/1809-98232016019.150140.
» https://doi.org/10.1590/1809-98232016019.150140 -
30Instituto Brasileiro de Geografia e Estatísticas − IBGE. Pesquisa Nacional por Amostra de Domicílios Contínua − PNAD Contínua. Características gerais dos domicílios e dos moradores. 2018. Available from: https://www.ibge.gov.br/estatisticas/sociais/trabalho/17270-pnad-continua.html?edicao=24437&t=resultados Accessed in 2020 (Jun 16).
» https://www.ibge.gov.br/estatisticas/sociais/trabalho/17270-pnad-continua.html?edicao=24437&t=resultados -
31Soares EO, Mattos IE, Monteiro GTR. Tendência da mortalidade por câncer de esôfago em capitais brasileiras, 1980-2002. Escola Nacional de Saúde Pública Sérgio Arouca (ENSP). 2008. Available from: Available from: http://www6.ensp.fiocruz.br/repositorio/resource/363454 Accessed in 2020 (Jun 16).
» http://www6.ensp.fiocruz.br/repositorio/resource/363454 -
32Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise em Saúde e Vigilância de Doenças não Transmissíveis. Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico, Vigitel 2018. Brasília: Ministério da Saúde; 2019. [Accessed 2020 June 16]. Available from: Available from: http://bvsms.saude.gov.br/bvs/publicacoes/vigitel_brasil_2018_vigilancia_fatores_risco.pdf
» http://bvsms.saude.gov.br/bvs/publicacoes/vigitel_brasil_2018_vigilancia_fatores_risco.pdf -
33Instituto Nacional do Câncer. Dados e números da prevalência do tabagismo. INCA − Instituto Nacional de Câncer. Observatório da Política Nacional de Controle do Tabaco. 2018. [Accessed 2020 June 16]. Available from: https://www.inca.gov.br/observatorio-da-politica-nacional-de-controle-do-tabaco/dados-e-numeros-prevalencia-tabagismo
» https://www.inca.gov.br/observatorio-da-politica-nacional-de-controle-do-tabaco/dados-e-numeros-prevalencia-tabagismo -
34Brasil. Presidência da República. Casa Civil. Decreto no 5.658, de 2 de janeiro de 2006. [Accessed 2020 June 16]. Available from: http://www.planalto.gov.br/ccivil_03/_Ato2004-2006/2006/Decreto/D5658.htm
» http://www.planalto.gov.br/ccivil_03/_Ato2004-2006/2006/Decreto/D5658.htm -
35Brasil. Presidência da República. Casa Civil. Subchefia para Assuntos Jurídicos. Lei nº 12.546, de 14 de dezembro de 2011. [Accessed 2020 June 16]. Available from: http://www.planalto.gov.br/CCIVIL_03/_Ato2011-2014/2011/Lei/L12546.htm
» http://www.planalto.gov.br/CCIVIL_03/_Ato2011-2014/2011/Lei/L12546.htm -
36Brasil. Presidência da República. Casa Civil. Decreto no 8.262, de 31 de maio de 2014. Altera o Decreto no 2.018, de 1o de outubro de 1996, que regulamenta a Lei no 9.294, de 15 de julho de 1996. [Accessed 2020 June 16]. Available from: http://presrepublica.jusbrasil.com.br/legislacao/121697845/decreto-8262-14
» http://presrepublica.jusbrasil.com.br/legislacao/121697845/decreto-8262-14 -
37Malta DC, Silva AG, Machado ÍE, De Sá ACMGN, Dos Santos FM, Prates EJS, Cristo EB. Trends in smoking prevalence in all Brazilian capitals between 2006 and 2017. J Bras Pneumol. 2019;45. doi: 10.1590/1806-3713/e20180384.
» https://doi.org/10.1590/1806-3713/e20180384 -
38Parakh S, Gan HK, Parslow AC, Burvenich IJG, Burgess AW, Scott AM. Evolution of anti-HER2 therapies for cancer treatment. Cancer Treat Rev. 2017;59:1-21. PMID: 28715775; doi: 10.1016/j.ctrv.2017.06.005.
» https://doi.org/10.1016/j.ctrv.2017.06.005 -
39Arantes V, Forero Piñeros EA, Yoshimura K, Toyonaga T. [Advances in the management of early esophageal carcinoma]. Rev Col Bras Cir. 2012;39:534-43. doi: 10.1590/S0100-69912012000600015.
» https://doi.org/10.1590/S0100-69912012000600015
-
Disclosure of funding: Productivity Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) to the author DCM. The GBD Brazil network has a support from Brazilian Ministry of Health (MS FNS - TED 125- 2017).
-
Research performed at: Universidade do Sul de Santa Catarina, Programa de Pós-Graduação em Ciências da Saúde. Tubarão, SC, Brasil.
Publication Dates
-
Publication in this collection
23 Apr 2021 -
Date of issue
Jan-Mar 2021
History
-
Received
17 Sept 2020 -
Accepted
06 Oct 2020