ABSTRACT
Background
Chronic hepatic disease is associated with osteoporosis, osteopenia or osteomalacia. Osteoporosis and fractures due to bone fragility present high prevalences and are more frequent in patients with liver cirrhosis than in the general population. The search for a diagnosis of osteopenia and osteoporosis in this population may allow early intervention and modify unfavorable outcomes.
Objective
To know the prevalence of osteopenia or osteoporosis and of fracture due to bone fragility in individuals with liver cirrhosis, the associated risk factors, and its compromise in their quality of life (QoL).
Methods
Observational, transversal study performed with 71 liver cirrhosis patients of the Hepatology Service of the Hospital de Base do Distrito Federal, Brasília, DF, Brazil, between July 2017 and December 2018. The patients were submitted to bone densitometry (DXA) of the lumbar spine and of the femoral neck, to x-ray of the lumbosacral spine and to the Chronic Liver Disease Questionnaire (CLDQ) for the evaluation of quality of life (QoL). The Fracture Risk Assessment (FRAX) major was calculated for patients >50 years old. The analyses were performed for the evaluation of the risk factors associated with lumbosacral spine fracture.
Results
The majority (62%) of the 71 evaluated patients was diagnosed with osteoporosis or osteopenia on DXA. Of the 44 patients with osteopenia or osteoporosis, 52.3% were female, with a mean age of 62.6±9.51 years old, with the majority (72.7%) being Child A, cirrhotics of alcoholic etiology (36.4%), and with an intermediate QoL according to the CLDQ (3.3). Regarding the patients with lumbosacral spine fracture, the mean age was 61.6±11.1 years old, 60% were female, most of them Child A (66.7%), of alcoholic etiology (46.7%), and with an intermediary QoL according to the CLDQ (3.5). The presence of osteopenia and/or osteoporosis was associated with lumbosacral fracture (P<0.001), without correlation with the other analyzed variables: age, body mass index, gender, presence and absence of ascites, Child-Pugh classification, vitamin D, calcium, and phosphorus serum concentration, cirrhosis etiology and FRAX major.
Conclusion
The prevalence of hepatic osteodystrophy was high, and the occurrence of lumbosacral spine fracture was more associated with osteoporosis and/or osteopenia among the cirrhotic patients studied. The QoL was intermediate and with no differences between cirrhotics with and without fracture.
Keywords:
Osteoporosis; liver cirrhosis; bone fractures; quality of life
RESUMO
Contexto
A doença hepática crônica associa-se com osteoporose, osteopenia ou osteomalácia. A osteoporose e as fraturas por fragilidade óssea têm altas prevalências e são mais frequentes em pacientes com cirrose hepática do que na população geral. A busca por osteopenia e osteoporose nesta população pode permitir a intervenção precoce e modificar os desfechos desfavoráveis.
Objetivo
Conhecer a prevalência de osteopenia ou osteoporose e de fraturas por fragilidade óssea em portadores de cirrose hepática, fatores de risco associados e seu comprometimento na qualidade de vida.
Métodos
Estudo observacional e transversal realizado com 71 pacientes portadores de cirrose hepática do Serviço de Hepatologia do Hospital de Base do Distrito Federal, Brasília, DF, Brasil, no período de julho de 2017 a dezembro de 2018. Os pacientes foram submetidos à densitometria óssea de coluna lombar e colo de fêmur, raio-x de coluna lombo sacra e ao questionário Chronic Liver Disease Questionnaire (CLDQ, na sigla em inglês) para avaliação de qualidade de vida. Foi calculado o escore de Fracture Risk Assessment Tool “FRAX Maior” nos pacientes >50 anos. As análises foram realizadas para a avaliação dos fatores de risco associados à fratura de coluna lombo sacra.
Resultados
Dos 71 pacientes avaliados, a maioria (62%) foi diagnosticada com osteoporose ou osteopenia à densitometria. Dos 44 portadores de osteopenia ou osteoporose, 52,3% eram do sexo feminino, com idade média de 62,6±9,51 anos, sendo a maioria (72,7%) Child A, cirróticos de etiologia alcoólica (36,4%) e com qualidade de vida intermediária ao CLDQ (3,3). Dos pacientes com fratura de coluna lombo sacra, a média de idade foi de 61,6±11,1 anos, 60% eram do sexo feminino, a maioria Child A (66,7%), de etiologia alcoólica (46,7%), e apresentaram qualidade de vida intermediária ao CLDQ (3,5). A presença de osteopenia e/ou osteoporose esteve associada à fratura lombo sacra (P<0,001), sem correlação com as demais variáveis analisadas: idade, índice de massa corporal (IMC), gênero, presença e ausência de ascite, classificação de Child-Pugh, concentrações séricas de vitamina D, cálcio e fósforo, etiologia da cirrose e “FRAX maior”.
Conclusão
A prevalência de osteodistrofia hepática foi elevada, e a ocorrência de fratura de coluna lombo sacra esteve mais associada à osteoporose e/ou osteopenia entre cirróticos estudados. A qualidade de vida se mostrou intermediária e sem diferença entre cirróticos com e sem fratura.
Palavras-chave:
Osteoporose; cirrose hepática; fraturas ósseas; qualidade de vida
INTRODUCTION
The development of liver cirrhosis occurs when the hepatic parenchyma acquires a nodular form as a result of the fibrosis consequent to chronic hepatic damage11. Goral V, Simsek M, Mete N. Hepatic osteodystrophy and liver cirrhosis. World J Gastroenterol. 2010;16:1639-43.. While this occurs, complications secondary to this process also appear, such as bone mineral disease, one of the main complications of chronic hepatic disease22. Leslie WD, Bernstein CN, Leboff MS. AGA technical review on osteoporosis in hepatic disorders. Gastroenterology. 2003;125:941-66.,33. Santos LAA, Romeiro FG. Diagnosis and Management of Cirrhosis-Related Osteoporosis. Biomed Res Int. 2016;2016:1423462. doi: 10.1155/2016/1423462.
https://doi.org/10.1155/2016/1423462...
.
The term hepatic osteodystrophy, which is controversial in the literature, but is still cited in recent publications, is used to define the bone disease associated with chronic hepatic disease, and includes osteoporosis, osteopenia and, more rarely, osteomalacia44. Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-8.
5. Danford CJ, Trivedi HD, Papamichael K, Tapper EB, Bonder A. Osteoporosis in primary biliary cholangitis. World J Gastroenterol . 2018;24:3513-20.-66. Pares A, Guanabens N. Primary biliary cholangitis and bone disease. Best Pr Res Clin Gastroenterol. 2018;35:63-70.. Bone disease occurs when there is an imbalance in bone remodeling, followed by the reduction in osteogenesis and higher bone resorption77. Guarino M, Loperto I, Camera S, Cossiga V, Di Somma C, Colao A, et al. Osteoporosis across chronic liver disease. Osteoporos Int. 2016;27:196777.,88. Chen CC, Wang SS, Jeng FS, Lee SD. Metabolic bone disease of liver cirrhosis: is it parallel to the clinical severity of cirrhosis? J Gastroenterol Hepatol. 1996;11:417-21.. Therefore, in advanced cases, the bone mass will reduce, and the risk of fracture will increase99. Bonkovsky HL, Hawkins M, Steinberg K, Hersh T, Galambos JT, Henderson JM, et al. Prevalence and prediction of osteopenia in chronic liver disease. Hepatology. 1990;12:273-80..
Osteoporosis and fractures due to bone fragility are more frequent in patients with liver cirrhosis than in the general population1010. Liang J, Meng WD, Yang JM, Li SL, Zhong MN, Hou XX, et al. The association between liver cirrhosis and fracture risk: A systematic review and meta-analysis. Clin Endocrinol. 2018;89:408-13., even in the absence of risk factors such as cholestasis or alcohol abuse1111. Giouleme OI, Vyzantiadis TA, Nikolaidis NL, Vasiliadis TG, Papageorgiou AA, Eugenidis NP, et al. Pathogenesis of osteoporosis in liver cirrhosis. Hepatogastroenterology. 2006;53:938-43.. The prevalence of osteoporosis among patients with chronic hepatic disease is reported to be between 12 and 55%44. Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-8.,1212. Matloff DS, Kaplan MM, Neer RM, Goldberg MJ, Bitman W, Wolfe HJ. Osteoporosis in primary biliary cirrhosis: effects of 25-hydroxyvitamin D3 treatment. Gastroenterology. 1982;83:97-102., depending on the criteria used for the diagnosis, as well as on the etiology, nutritional status, age group, and degree of hepatic disease22. Leslie WD, Bernstein CN, Leboff MS. AGA technical review on osteoporosis in hepatic disorders. Gastroenterology. 2003;125:941-66.,44. Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-8..
As such, a better approach is mandatory to evaluate the prevalence of osteopenia or osteoporosis and of fractures due to bone fragility in individuals with liver cirrhosis, the associated risk factors, as well as to evaluate the interference in the quality of life (QoL) of these individuals.
METHODS
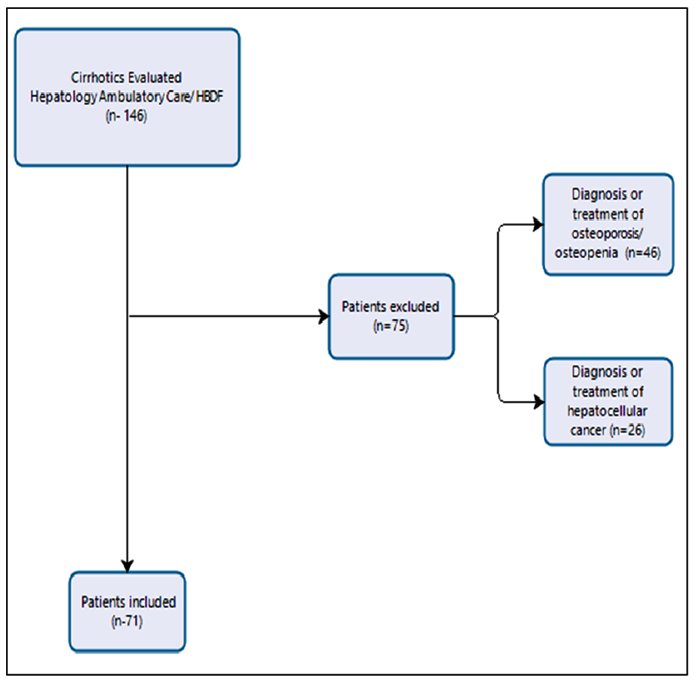
Initially, a total of 146 cirrhotics was included in the present observational, transversal study performed in the hepatology ambulatory care facility of the Hospital de Base do Distrito Federal (HBDF, in the Portuguese acronym), Brasília, DF, Brazil, in the period between July 2017 and December 2018, established for data collection. Out of this total, 46 patients were excluded because they had a previous diagnosis of osteopenia and/or osteoporosis and were already being treated for this condition. These patients were excluded because they were already in treatment (either with or without medication) for osseous alterations and, therefore, were under a lower risk of fracture, and because this was a confounding factor in the prevalence of osseous fracture in the studied sample. Besides, this could also generate a bias in the QoL questionnaire.
The sample consisted of 71 patients with liver cirrhosis of the hepatology service of the HBDF, selected during routine ambulatorial consultations. All patients had liver cirrhosis from any etiology, were >18 years old, had not presented hospital internment in the previous 30 days, and signed the free and informed consent form. All subjects were informed of the objectives of the present research.
The research project was approved by the Ethics and Research Committee of the Fundação de Ensino e Pesquisa em Ciências da Saúde (FEPECS, in the Portuguese acronym). The patients were ensured of the anonymity and confidentiality concerning the provided information. The present research was approved under CAAE opinion number 78583417.2.0000.5553.
The exclusion criteria were pregnancy, patients with neoplasia in any site and bone metastasis, use of medication that interfere in bone metabolism, and previous osteoporosis or osteopenia under treatment.
The following clinical data were collected: etiology of liver cirrhosis, gender, and age; and the Child-Turcotte-Pugh score1313. Sanhueza E, Contreras J, Zapata R, Sanhueza M, Elgueta F, Lopez C, et al. [Comparative evaluation of survival prognosis using MELD or Child-Pugh scores in patients with liver cirrhosis in Chile]. Rev Med Chil. 2017;145:17-24. and body mass index (BMI) were calculated. From blood retrieved from the antecubital vein, after night fasting of 8 hours, the following markers were measured: calcium (o-cresolphthalein complexone [oCPC] method) corrected by serum albumin, with normal values between 8.5 and 10.2 mg/dL, and phosphorus (phosphorus phosphomolybdate method), with normal values between 2.5 and 4.5 mg/dL, and 1.25-dihydroxycholecalciferol vitamin (quimioluminescence method; normal values between 30 and 60 ng/mL). Serum concentrations of 25-hydroxyvitamin D (vitamin D) <30 ng/mL1414. Maeda SS, Borba VZC, Camargo MBR, Silva DMW, Borges JLC, Bandeira F, et al. Recomendações da Sociedade Brasileira de Endocrinologia e Metabologia (SBEM) para o diagnóstico e tratamento da hipovitaminose D. Arq Bras Endocrinol Metabol [Internet]. 2014;58:411- 33. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302014000500411&nrm=iso
http://www.scielo.br/scielo.php?script=s...
were considered hypovitaminosis D for higher-risk patients, such as patients with chronic hepatic disease.
For the evaluation of bone mineral density (BMD), bone densitometry (DXA) of the lumbar spine and of the femoral neck was performed with an explorer QDR bone densitometer (Hologic, Inc., Marlborough, MA, USA). The diagnostic parameters used in standard deviation (SD) were in accordance with the 2008 guidelines of the Sociedade Brasileira de Densitometria Clínica1515. Brandão CMA, Camargos BM, Zerbini CA, Plapler PG, Mendonça LM de C, Albergaria B-H, et al. Posições oficiais 2008 da Sociedade Brasileira de Densitometria Clínica (SBDens). Arq Bras Endocrinol Metabol [Internet]. 2009;53:107-12. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302009000100016&nrm=iso
http://www.scielo.br/scielo.php?script=s...
. Premenopausal women and males <50 years old who presented a Z-score ≤2.00 were defined as having a BMD below the estimated value for this age group. Those with a Z-score >2.00 were considered as having a BMD within the estimated value for this age group. Postmenopausal women and males >50 years old with a T-score ≤ -1 were classified as having a normal BMD, those with a T-score between -1 and -2.5 were considered as having osteopenia, and those with a T-score ≤2.5 were considered as having densitometric osteoporosis.
The diagnosis of fracture due to bone fragility was made by radiography of the lumbosacral spine, in anteroposterior and profile incidences, which was performed in all patients, both symptomatic and asymptomatic. Fracture due to bone fragility was defined as a vertebral body fracture due to minimal trauma, such as fall from one’s own height or even without identification of the trauma.
The FRAX-Brazil score of patients >50 years old was calculated. The probability of fracture within 10 years was calculated from data such as age, gender, BMI, and risk factors such as a history of fractures due to bone fragility, family history of fracture of the femur, smoking, prolonged use of corticosteroids, rheumatoid arthritis, other causes of secondary osteoporosis and high alcohol intake1616. Centre for Metabolic Bone Diseases U of S. FRAX Tool. Instrumento de avaliação do risco de fratura. 2008.[Internet]. Available from https://www.sheffield.ac.uk/FRAX/tool.aspx?lang=pr
https://www.sheffield.ac.uk/FRAX/tool.as...
17. Bastos-Silva Y, Aguiar LB, Pinto-Neto AM, Baccaro LF, Costa-Paiva L. Correlation between osteoporotic fracture risk in Brazilian postmenopausal women calculated using the FRAX with and without the inclusion of bone densitometry data. Arch Osteoporos. 2016;11:16.-1818. Felisberto MM, Costi MES, Heluany CCV. Relação entre resultados da FRAX-Brasil e de densitometrias ósseas TT - Relationship between the results of FRAX-Brazil and bone densitometries. Rev Soc Bras Clín Méd [Internet]. 2018;16:7-12. Available from: http://docs.bvsalud.org/biblioref/2018/06/884976/161.pdf
http://docs.bvsalud.org/biblioref/2018/0...
. The DXA was also used for the calculation of the FRAX. In the present study, we calculated the FRAX major of the patients during the consultation, without knowing which patients had fractures, with the aim of correlating higher FRAX scores for major fracture in the patients subsequently diagnosed with fracture of the lumbosacral spine. For the calculation of the FRAX, we only included patients >50 years old or postmenopausal women, because for its calculation, only the T-score of the femoral neck is used, and not the Z-score1919. Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N, et al. Interpretation and use of FRAX in clinical practice. Osteoporos Int . 2011;22:2395-411..
The Chronic Liver Disease Questionnaire (CLDQ) was applied by a single examiner and it was translated into Portuguese considering the cultural adaptation of this instrument for its use in Brazil. The authors translated it from English into Portuguese, and its equivalence was evaluated by a bilingual translator. The patients responded to the 29 questions distributed into six domains, and each question had seven levels of answers: from one (all the time) to seven (never). The six domains evaluated were abdominal symptoms, fatigue, systemic symptoms, activity, emotional function and worrying2020. Younossi ZM, Guyatt G, Kiwi M, Boparai N, King D. Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut. 1999;45:295-300.. It was considered that the closer the score is to seven, the higher the QoL of the patient, and the closer the score is to one, the worse the QoL of the patient, and intermediate values correspond to an intermediate QoL. The correlation between the presence or absence of bone fracture and QoL was studied. The authors have opted for the use of the CLDQ because it is validated for patients with liver disease.
The diagnosis of liver cirrhosis was defined by biopsy or by the combination of clinical, radiological, laboratory and/or endoscopic findings compatible with liver insufficiency and portal hypertension.
The Child-Turcotte-Pugh score was used for the evaluation of the severity of the disease, according to the following scores: Child-Pugh A (5 and 6 points); Child-Pugh B (7-9 points); and Child-Pugh C (10-15 points)1313. Sanhueza E, Contreras J, Zapata R, Sanhueza M, Elgueta F, Lopez C, et al. [Comparative evaluation of survival prognosis using MELD or Child-Pugh scores in patients with liver cirrhosis in Chile]. Rev Med Chil. 2017;145:17-24..
Continuous variables with normal and nonnormal distribution were presented in mean (standard deviation [SD]) and median (interquartile range [IQ]), and categorical variables were presented in percentage. Categorical variables were compared using the chi-squared test, and continuous variables were compared using the t-test or the Mann-Whitney test, according to their distribution. A P-value <0.05 was considered statistically significant. Thus, the analysis of the bivariate models were performed. Those who presented an altered DXA (presence of osteopenia or osteoporosis) were categorized in a single variable, called altered femoral and lumbosacral spine DXA, and its distribution was assessed in relation to the following variables: age, gender, BMI, Child-Pugh, etiology of cirrhosis, ascites, CLDQ, and serum concentrations of vitamin D, calcium, and phosphorus. The individuals were categorized as with presence or absence of bone fractures (BFs) in the x-ray of the lumbosacral spine. The FRAX major was compared with the presence or absence of fractures in order to try to establish a correlation by the Student t-test.
RESULTS
A total of 29 patients diagnosed with and under treatment for hepatocellular carcinoma was also excluded, since these patients could present with secondary osseous compromise or be using medication that interfere with bone metabolism and, therefore, could also be a confounding factor in the prevalence of hepatic osteodystrophy and spontaneous bone fracture. Besides, the presence of a neoplasm and the possibility of the use of sorafenib may cause asthenia and interfere in the result of the CLDQ. The final sample consisted of 71 patients who fulfilled the inclusion criteria of the present study (Figure 1).
The epidemiological, clinical, and laboratory characteristics of the 71 patients are presented in Table 1. It is observed that the patients were adults and that there was a discrete predominance of males. Most participants were classified as Child-Pugh A and did not present ascites. The mean BMI was 25.9 kg/m2. The mean serum concentrations of vitamin D, ionized calcium, and phosphorus were within the parameters of normality. The average CLDQ score was 3.9, characterizing an intermediate QoL in the total sample.
The basal characteristics of the 27 (38%) patients without hepatic osteodystrophy (osteopenia/osteoporosis) and of the 44 (62%) patients with hepatic osteodystrophy are shown in Table 2.
In the normal DXA group, the patients were adults, with a predominance of males, and the main etiology of hepatic disease was cirrhosis of viral etiology. Most of the patients were Child A and did not present with ascites. The mean BMI and the mean serum concentration of phosphorus, calcium, and vitamin D were within the parameters of normality. The average CLDQ score was 3.4, characterizing an intermediary QoL in these patients.
In the altered DXA group, the patients were adults, with a discrete predominance of females. The main etiology of hepatic disease in these patients was cirrhosis of alcoholic etiology, and the minority by nonalcoholic steatohepatitis (NASH). Most of the patients were Child A and did not present with ascites. The mean BMI and the mean serum concentrations of phosphorus, calcium and vitamin D were within the parameters of normality. The average CLDQ score was 3.3, characterizing an intermediate QoL in this sample.
Comparing both groups, we observed that the age was significantly higher in the altered DXA group compared with the normal DXA group. The other parameters examined were not significantly different between both groups.
We present and compare the clinical and laboratory characteristics between the group of patients who had fractures and those who did not have fractures in Table 3. It is observed that there was no significant difference between both groups in any of the examined characteristics, except for the presence of osteopenia and/or osteoporosis on DXA as an associated factor to lumbosacral fracture (P<0.001).
The FRAX major of all patients >50 years old was calculated. Of the 15 fractured patients, two patients <50 years old were excluded. In the FRAX major and lumbosacral spine fracture association (Student t-test), we found a P-value of 0.051, and a confidence interval (CI) of 0.0005-2.094.
DISCUSSION
In the present study, we have shown that individuals with liver cirrhosis present a high incidence of osteoporosis and osteopenia, as well as of BFs in the lumbar spine. Most of the patients were classified as Child A, did not present with ascites, and their serum concentrations of vitamin D, calcium, and phosphorus were within the normality parameters. The QoL of the patients was intermediate. The only significant difference in the evaluation of the patients with and without fractures was a normal DXA in those who did not have fractures.
In the last decades, with the advancement in the management of the complications of cirrhosis and the offer of liver transplantation, it became possible to have higher survival and QoL rates in cirrhotic patients. Currently, a compensated cirrhotic reaches an average survival rate of 12 years after the diagnosis of liver cirrhosis2121. D’Amico G, Morabito A, Pagliaro L, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31:468-75.. However, the higher survival rate of these patients increased the risk of extrahepatic complications, such as osteoporosis2222. Luxon BA. Bone disorders in chronic liver diseases. Curr Gastroenterol Rep. 2011;13:40-8.,2323. Shiomi S. [Secondary osteoporosis. Bone disease in liver cirrhosis]. Clin Calcium . 2018;28:1659-64..
In the present study, we have shown that liver cirrhosis patients of various etiologies, but mainly of viral or alcoholic etiologies, present a high rate of osteoporosis or osteopenia (62%).
Regardless of the etiology of chronic hepatic disease, the presence of cirrhosis implies in a twofold higher risk of BF in relation to the noncirrhotic population44. Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-8., and the etiology of these disorders is complex and multifactorial22. Leslie WD, Bernstein CN, Leboff MS. AGA technical review on osteoporosis in hepatic disorders. Gastroenterology. 2003;125:941-66.. In a study2424. Hajiabbasi A, Shafaghi A, Fayazi HS, Shenavar Masooleh I, Hedayati Emami MH, Ghavidel Parsa P, et al. The factors affecting bone density in cirrhosis. Hepat Mon. 2015;15:e26871. that followed 97 liver cirrhosis patients of several etiologies, the prevalence of hepatic osteodystrophy was of 78.4%, corroborating the hypothesis, like the present study, that liver cirrhosis patients may have a higher chance of presenting altered DXA, regardless of the etiology of the hepatic disease.
In the present study, we observed that more advanced age was more associated with altered DXA. The pathogenesis of the bone disorders in cirrhotic patients remains not completely elucidated1111. Giouleme OI, Vyzantiadis TA, Nikolaidis NL, Vasiliadis TG, Papageorgiou AA, Eugenidis NP, et al. Pathogenesis of osteoporosis in liver cirrhosis. Hepatogastroenterology. 2006;53:938-43., but already established that risk factors for osteoporosis, such as advanced age, alcohol abuse, smoking, previous fractures, denutrition, and loss of muscular mass, are frequent in patients with liver cirrhosis2525. Guichelaar MM, Kendall R, Malinchoc M, Hay JE. Bone mineral density before and after OLT: long-term follow-up and predictive factors. Liver Transpl. 2006;12:1390-402..
It was also possible to observe the diagnosis of lumbosacral spine fracture on x-ray in 21% of these cirrhotic patients. In a literature review, the prevalence of fractures in patients with chronic hepatic disease varied between 7 and 35%2626. Guanabens N, Pares A. Liver and bone. Arch Biochem Biophys. 2010;503:84-94.. Many of the differences in frequency found between what we have observed and what has been observed in other studies are related to the selection of patients. In the analysis of risk factors, no significant difference was found between patients with and without fracture in relation to age, gender, BMI, presence of ascites, Child-Pugh classification, serum concentrations of vitamin D, calcium, and phosphorus, etiology of the cirrhosis, and FRAX major. However, the presence of osteopenia or osteoporosis on DXA was significantly correlated with lumbosacral fracture (P<0.001).
The detection of osteoporosis requires a high level of clinical suspicion for its diagnosis, since around one-third of vertebral spine fractures are asymptomatic and will only be detected radiologically44. Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-8.. Both conditions, osteoporosis and BF, have a significant impact on these patients, for they cause fractures that may result in chronic pain, prolonged immobility, deformities, and may affect the QoL and even the survival rate22. Leslie WD, Bernstein CN, Leboff MS. AGA technical review on osteoporosis in hepatic disorders. Gastroenterology. 2003;125:941-66.,44. Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-8.,2727. Loria I, Albanese C, Giusto M, Galtieri PA, Giannelli V, Lucidi C, et al. Bone disorders in patients with chronic liver disease awaiting liver transplantation. Transpl Proc. 2010;42:1191-3.. Bone fracture implies in a higher risk of refracture2828. Hsiao PC, Chen TJ, Li CY, Chu CM, Su TP, Wang SH, et al. Risk factors and incidence of repeat osteoporotic fractures among the elderly in Taiwan: a population-based cohort study. Med. 2015;94:e532., which may impact even more the morbidity and the worsening of the QoL of the patient with liver cirrhosis44. Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-8.,2929. Danford CJ, Trivedi HD, Bonder A. Bone Health in Patients With Liver Diseases. J Clin Densitom. 2020;23:212-22..
With the development of DXA, it has become possible to measure the BMD and, thus, to evaluate which patients would be under a higher risk of BF. Conventional diagnostical radiographies also are an important component in the evaluation of osteoporosis, since they are useful in the detection of fractures due to fragility, such as fractures due to vertebral compression, regardless of the DXA44. Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-8..
According to the 2014 Clinical Protocol and Therapeutic Guidelines for Osteoporosis (PCDT, in the Portuguese acronym) of the Brazilian Ministry of Health, the tracing of osteoporosis in women ≥65 years old and in men >70 years old is indicated, regardless of the presence of risk factors3030. Brasil. Ministério da Saúde. Portaria no 224, de 26 de março de 2014. Aprova o Protocolo Clínico e Diretrizes Terapêuticas da Osteoporose. Saúde S de A à, editor. Diário Oficial da União no 109 de 10 de junho de 2014, seção 1, página 48; 2014.. In this manual, liver cirrhosis is not included as a risk factor for osteoporosis, only primary biliary cholangitis (PBC), not contemplating other individuals with chronic hepatic disease, as has been commented in previous studies3131. Mendes LSC, Neves BC, de Menezes ALS, Carneiro MV, Trevizoli JE, Lobão PN, et al. Low bone mineral density manifests in cirrhotic patients 15 to 20 years before the usual screening age. Acta Gastroenterol Latinoam. 2020;50:264-70..
According to the data presented in the present study, we have observed an average age of 61.6±11 years old among osteoporosis or osteopenia patients with lumbosacral fracture, which could have been avoided if this tracing had been established earlier. Besides, fractures in liver cirrhosis patients who presented only with osteopenia were found. In 13.3% of the sample of fractured patients, lumbosacral spine fracture occurred in osteopenia patients.
A study evidenced a prevalence of 27% of fractures in liver cirrhosis patients of various etiologies, being higher in the osteoporosis group than in the group without this ailment (P<0.001)3232. Monegal A, Navasa M, Guanabens N, Peris P, Pons F, Martinez de Osaba MJ, et al. Osteoporosis and bone mineral metabolism disorders in cirrhotic patients referred for orthotopic liver transplantation. Calcif Tissue Int. 1997;60:148-54.. It is interesting that any type of previous fracture was considered, which may have overestimated this result, but it had a slightly higher result than what we have observed evaluating only fractures due to bone fragility.
Clinical tools may also be useful in the assessment of the risk of fracture due to bone fragility, such as the FRAX algorithm. This score was developed by the World Health Organization (WHO) with the aim of evaluating the probability of bone fracture in the next 10 years (the probability of hip fracture and of major fracture is expressed in percentage) and of evaluating the decision regarding the initiation of medical treatment for osteoporosis3333. Pinheiro M de M, Camargos BM, Borba VZC, Lazaretti-Castro M. FRAXTM: construindo uma ideia para o Brasil. Arq Bras Endocrinol Metabol . [Internet]. 2009;53:783-90. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302009000600015&nrm=iso
http://www.scielo.br/scielo.php?script=s...
,3434. Ayres LRO, Clarke S, Digby-Bell J, Dhanda AD, Dharmasiri S, Caddick K, et al. Fragility fracture risk in cirrhosis: a comparison of the fracture risk assessment tool, British Society of Gastroenterology and National Institute for Health and Clinical Excellence guidelines. Front Gastroenterol. 2012;3:220-7..
In the present work, the FRAX major of the patients >50 years old was calculated in the first consultation, without knowledge of the results of the lumbosacral spine x-ray, as an attempt to avoid observation bias. Afterwards, no correlation was found between higher FRAX major scores in patients with lumbosacral spine fracture on x-ray (P=0.051). However, the long CI (0.005-2.094) suggests that this correlation may be possible with a larger sample of patients. A limitation of this tool is that in order to calculate the FRAX, the femoral T-score is used, being possible to include only men >50 years old and/or menopausal women. In the present study, the calculations of the FRAX of 2 of the 15 fractured patients were excluded because they were <40 years old.
According to the data described here, age, gender, presence of ascites, Child score, serum concentrations of vitamin D, calcium, and phosphorus, and the etiology of liver cirrhosis were not predictors of the development of BF diagnosed with lumbosacral spine x-ray. Only the DXA of the lumbar spine and/or of the femoral neck evidencing osteopenia or osteoporosis was a common characteristic in all fractured patients.
A meta-analysis of prospective studies showed that the risk of fracture increases progressively with BMD reduction3535. Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. Bmj. 1996;312:1254-9.. The DXA has high specificity for fracture, but low sensibility3636. Collier JD, Ninkovic M, Compston JE. Guidelines on the management of osteoporosis associated with chronic liver disease. Gut. 2002;50(Suppl 1):1-9.. Therefore, associating lumbosacral spine x-ray with DXA, as we have done in the present work, may be a strategy to increase the diagnostic sensibility of fracture due to bone fragility, which is often asymptomatic3737. Lopes JB, Fung LK, Cha CC, Gabriel GM, Takayama L, Figueiredo CP, et al. The impact of asymptomatic vertebral fractures on quality of life in older community-dwelling women: the Sao Paulo Ageing & Health Study. Clin (Sao Paulo). 2012;67:1401-6..
Regarding the QoL related to BF, it is known that vertebral fractures are often asymptomatic or lightly symptomatic, but that, in the long term, they may affect substantially the QoL of the patients3737. Lopes JB, Fung LK, Cha CC, Gabriel GM, Takayama L, Figueiredo CP, et al. The impact of asymptomatic vertebral fractures on quality of life in older community-dwelling women: the Sao Paulo Ageing & Health Study. Clin (Sao Paulo). 2012;67:1401-6.. Osteoporosis increases the risk of fractures and compromises the QoL of the patients due to pain and deformities3838. Guanabens N, Pares A. Management of osteoporosis in liver disease. Clin Res Hepatol Gastroenterol. 2011;35:438-45.
39. Lems WF, Raterman HG. Critical issues and current challenges in osteoporosis and fracture prevention. An overview of unmet needs. Ther Adv Musculoskelet Dis. 2017;9:299-316.-4040. Muhsen IN, AlFreihi O, Abaalkhail F, AlKhenizan A, Khan M, Eldali A, et al. Bone mineral density loss in patients with cirrhosis. Saudi J Gastroenterol. 2018;24:342-7..
In the present study, an inferior QoL was not observed in fractured patients. The QoL analysis was performed with the CLDQ, an approved questionnaire for the use in liver cirrhosis patients, which allows the evaluation of six domains related to the life of the patient4141. Raszeja-Wyszomirska J, Kucharski R, Zygmunt M, Safranow K, Miazgowski T. The impact of fragility fractures on health-related quality of life in patients with primary sclerosing cholangitis. Hepat Mon. 2015;15:e25539..
However, this questionnaire, in our critical evaluation, has important limitations, being very subjective, with answers that may be very similar to one another, but with different scores that may alter the final result of the questionnaire. Besides, only the previous 2 weeks of the lives of the patients are evaluated, which may difficult the global evaluation of their QoL. Perhaps, with the use of other questionnaires that may be more objective and that evaluate a longer period of the life of the patient, we may find data that better evaluate the QoL of these patients. This is because it has been shown that the QoL of fractured patients, which was evaluated by three different questionnaires, was compromised4141. Raszeja-Wyszomirska J, Kucharski R, Zygmunt M, Safranow K, Miazgowski T. The impact of fragility fractures on health-related quality of life in patients with primary sclerosing cholangitis. Hepat Mon. 2015;15:e25539..
Regarding vitamin D serum concentrations, it is known that vitamin D deficiency is widely diagnosed in patients with chronic hepatic disease4242. Arteh J, Narra S, Nair S. Prevalence of vitamin D deficiency in chronic liver disease. Dig Dis Sci . 2010;55:2624-8.,4343. Fisher L, Fisher A. Vitamin D and parathyroid hormone in outpatients with noncholestatic chronic liver disease. Clin Gastroenterol Hepatol. 2007;5:513-20.. Its origin is multifactorial and is correlated with the severity of hepatic disease2424. Hajiabbasi A, Shafaghi A, Fayazi HS, Shenavar Masooleh I, Hedayati Emami MH, Ghavidel Parsa P, et al. The factors affecting bone density in cirrhosis. Hepat Mon. 2015;15:e26871.,4242. Arteh J, Narra S, Nair S. Prevalence of vitamin D deficiency in chronic liver disease. Dig Dis Sci . 2010;55:2624-8.,4444. Karoli Y, Karoli R, Fatima J, Manhar M. Study of Hepatic Osteodystrophy in Patients with Chronic Liver Disease. J Clin Diagn Res. 2016;10:31-4.. Low serum concentration of vitamin D is associated with osteoporosis and with a high risk of BF, especially in elderly patients4545. Rouillard S, Lane NE. Hepatic osteodystrophy. Hepatology. 2001;33:301-7.,4646. Wariaghli G, Allali F, El Maghraoui A, Hajjaj-Hassouni N. Osteoporosis in patients with primary biliary cirrhosis . Eur J Gastroenterol Hepatol . 2010;22:1397-401.. However, in our sample, it was not possible to correlate low vitamin D serum concentration with fractures. Perhaps, this may be explained by the small sample size or by the fact that the patients live in a region where solar exposure is much higher than that of the locations of other studies.
Regardless of the Child-Pugh score, of the etiology of chronic liver disease and of vitamin D serum concentration, we should consider the risk of already fractured patients presenting with a new fracture. This has been reported by a study2828. Hsiao PC, Chen TJ, Li CY, Chu CM, Su TP, Wang SH, et al. Risk factors and incidence of repeat osteoporotic fractures among the elderly in Taiwan: a population-based cohort study. Med. 2015;94:e532. that evidenced that the risk of refracture is 1.73 times higher in patients with previous vertebral fracture. It may be possible that this risk is even higher in liver cirrhosis patients; however, to our knowledge, this data is not available in the literature. If the fractured is not detected and approached early, in the future the fracture may evolve to refracture and impact significantly the QoL of these patients.
Even though the sample was small, this present study draws attention to the hypothesis that the high prevalence of hepatic osteodystrophy in liver cirrhosis patients and the higher risk of BFs secondary to low BMD raises questions about considering tracing these patients at a lower age than that of the general population. This way, we will be able to identify and to intervene in the risk factors associated with bone disease and to institute an early therapeutic program. Therefore, we will be able to avoid negative outcomes that compromise the QoL and the life expectancy of this population.
CONCLUSION
The rate of lumbosacral spine fracture was high in our casuistry, and it is correlated with the presence of osteoporosis and/or osteopenia. This suggests that liver cirrhosis patients should undergo DXA and lumbosacral spine x-ray for early diagnosis and treatment. The QoL of patients with hepatic osteodystrophy is intermediate and there is no difference between patients with and without fracture, but this may reflect the limitations of the CLDQ, which was used in the present research.
ACKNOWLEDGMENTS
The authors would like to thank the Gastroenterology Service of the Hospital de Base do Distrito Federal for having made possible and enabled the conduction of the present study.
REFERENCES
-
1Goral V, Simsek M, Mete N. Hepatic osteodystrophy and liver cirrhosis. World J Gastroenterol. 2010;16:1639-43.
-
2Leslie WD, Bernstein CN, Leboff MS. AGA technical review on osteoporosis in hepatic disorders. Gastroenterology. 2003;125:941-66.
-
3Santos LAA, Romeiro FG. Diagnosis and Management of Cirrhosis-Related Osteoporosis. Biomed Res Int. 2016;2016:1423462. doi: 10.1155/2016/1423462.
» https://doi.org/10.1155/2016/1423462 -
4Collier J. Bone disorders in chronic liver disease. Hepatology. 2007;46:1271-8.
-
5Danford CJ, Trivedi HD, Papamichael K, Tapper EB, Bonder A. Osteoporosis in primary biliary cholangitis. World J Gastroenterol . 2018;24:3513-20.
-
6Pares A, Guanabens N. Primary biliary cholangitis and bone disease. Best Pr Res Clin Gastroenterol. 2018;35:63-70.
-
7Guarino M, Loperto I, Camera S, Cossiga V, Di Somma C, Colao A, et al. Osteoporosis across chronic liver disease. Osteoporos Int. 2016;27:196777.
-
8Chen CC, Wang SS, Jeng FS, Lee SD. Metabolic bone disease of liver cirrhosis: is it parallel to the clinical severity of cirrhosis? J Gastroenterol Hepatol. 1996;11:417-21.
-
9Bonkovsky HL, Hawkins M, Steinberg K, Hersh T, Galambos JT, Henderson JM, et al. Prevalence and prediction of osteopenia in chronic liver disease. Hepatology. 1990;12:273-80.
-
10Liang J, Meng WD, Yang JM, Li SL, Zhong MN, Hou XX, et al. The association between liver cirrhosis and fracture risk: A systematic review and meta-analysis. Clin Endocrinol. 2018;89:408-13.
-
11Giouleme OI, Vyzantiadis TA, Nikolaidis NL, Vasiliadis TG, Papageorgiou AA, Eugenidis NP, et al. Pathogenesis of osteoporosis in liver cirrhosis. Hepatogastroenterology. 2006;53:938-43.
-
12Matloff DS, Kaplan MM, Neer RM, Goldberg MJ, Bitman W, Wolfe HJ. Osteoporosis in primary biliary cirrhosis: effects of 25-hydroxyvitamin D3 treatment. Gastroenterology. 1982;83:97-102.
-
13Sanhueza E, Contreras J, Zapata R, Sanhueza M, Elgueta F, Lopez C, et al. [Comparative evaluation of survival prognosis using MELD or Child-Pugh scores in patients with liver cirrhosis in Chile]. Rev Med Chil. 2017;145:17-24.
-
14Maeda SS, Borba VZC, Camargo MBR, Silva DMW, Borges JLC, Bandeira F, et al. Recomendações da Sociedade Brasileira de Endocrinologia e Metabologia (SBEM) para o diagnóstico e tratamento da hipovitaminose D. Arq Bras Endocrinol Metabol [Internet]. 2014;58:411- 33. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302014000500411&nrm=iso
» http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302014000500411&nrm=iso -
15Brandão CMA, Camargos BM, Zerbini CA, Plapler PG, Mendonça LM de C, Albergaria B-H, et al. Posições oficiais 2008 da Sociedade Brasileira de Densitometria Clínica (SBDens). Arq Bras Endocrinol Metabol [Internet]. 2009;53:107-12. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302009000100016&nrm=iso
» http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302009000100016&nrm=iso -
16Centre for Metabolic Bone Diseases U of S. FRAX Tool. Instrumento de avaliação do risco de fratura. 2008.[Internet]. Available from https://www.sheffield.ac.uk/FRAX/tool.aspx?lang=pr
» https://www.sheffield.ac.uk/FRAX/tool.aspx?lang=pr -
17Bastos-Silva Y, Aguiar LB, Pinto-Neto AM, Baccaro LF, Costa-Paiva L. Correlation between osteoporotic fracture risk in Brazilian postmenopausal women calculated using the FRAX with and without the inclusion of bone densitometry data. Arch Osteoporos. 2016;11:16.
-
18Felisberto MM, Costi MES, Heluany CCV. Relação entre resultados da FRAX-Brasil e de densitometrias ósseas TT - Relationship between the results of FRAX-Brazil and bone densitometries. Rev Soc Bras Clín Méd [Internet]. 2018;16:7-12. Available from: http://docs.bvsalud.org/biblioref/2018/06/884976/161.pdf
» http://docs.bvsalud.org/biblioref/2018/06/884976/161.pdf -
19Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N, et al. Interpretation and use of FRAX in clinical practice. Osteoporos Int . 2011;22:2395-411.
-
20Younossi ZM, Guyatt G, Kiwi M, Boparai N, King D. Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut. 1999;45:295-300.
-
21D’Amico G, Morabito A, Pagliaro L, Marubini E. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig Dis Sci. 1986;31:468-75.
-
22Luxon BA. Bone disorders in chronic liver diseases. Curr Gastroenterol Rep. 2011;13:40-8.
-
23Shiomi S. [Secondary osteoporosis. Bone disease in liver cirrhosis]. Clin Calcium . 2018;28:1659-64.
-
24Hajiabbasi A, Shafaghi A, Fayazi HS, Shenavar Masooleh I, Hedayati Emami MH, Ghavidel Parsa P, et al. The factors affecting bone density in cirrhosis. Hepat Mon. 2015;15:e26871.
-
25Guichelaar MM, Kendall R, Malinchoc M, Hay JE. Bone mineral density before and after OLT: long-term follow-up and predictive factors. Liver Transpl. 2006;12:1390-402.
-
26Guanabens N, Pares A. Liver and bone. Arch Biochem Biophys. 2010;503:84-94.
-
27Loria I, Albanese C, Giusto M, Galtieri PA, Giannelli V, Lucidi C, et al. Bone disorders in patients with chronic liver disease awaiting liver transplantation. Transpl Proc. 2010;42:1191-3.
-
28Hsiao PC, Chen TJ, Li CY, Chu CM, Su TP, Wang SH, et al. Risk factors and incidence of repeat osteoporotic fractures among the elderly in Taiwan: a population-based cohort study. Med. 2015;94:e532.
-
29Danford CJ, Trivedi HD, Bonder A. Bone Health in Patients With Liver Diseases. J Clin Densitom. 2020;23:212-22.
-
30Brasil. Ministério da Saúde. Portaria no 224, de 26 de março de 2014. Aprova o Protocolo Clínico e Diretrizes Terapêuticas da Osteoporose. Saúde S de A à, editor. Diário Oficial da União no 109 de 10 de junho de 2014, seção 1, página 48; 2014.
-
31Mendes LSC, Neves BC, de Menezes ALS, Carneiro MV, Trevizoli JE, Lobão PN, et al. Low bone mineral density manifests in cirrhotic patients 15 to 20 years before the usual screening age. Acta Gastroenterol Latinoam. 2020;50:264-70.
-
32Monegal A, Navasa M, Guanabens N, Peris P, Pons F, Martinez de Osaba MJ, et al. Osteoporosis and bone mineral metabolism disorders in cirrhotic patients referred for orthotopic liver transplantation. Calcif Tissue Int. 1997;60:148-54.
-
33Pinheiro M de M, Camargos BM, Borba VZC, Lazaretti-Castro M. FRAXTM: construindo uma ideia para o Brasil. Arq Bras Endocrinol Metabol . [Internet]. 2009;53:783-90. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302009000600015&nrm=iso
» http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302009000600015&nrm=iso -
34Ayres LRO, Clarke S, Digby-Bell J, Dhanda AD, Dharmasiri S, Caddick K, et al. Fragility fracture risk in cirrhosis: a comparison of the fracture risk assessment tool, British Society of Gastroenterology and National Institute for Health and Clinical Excellence guidelines. Front Gastroenterol. 2012;3:220-7.
-
35Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. Bmj. 1996;312:1254-9.
-
36Collier JD, Ninkovic M, Compston JE. Guidelines on the management of osteoporosis associated with chronic liver disease. Gut. 2002;50(Suppl 1):1-9.
-
37Lopes JB, Fung LK, Cha CC, Gabriel GM, Takayama L, Figueiredo CP, et al. The impact of asymptomatic vertebral fractures on quality of life in older community-dwelling women: the Sao Paulo Ageing & Health Study. Clin (Sao Paulo). 2012;67:1401-6.
-
38Guanabens N, Pares A. Management of osteoporosis in liver disease. Clin Res Hepatol Gastroenterol. 2011;35:438-45.
-
39Lems WF, Raterman HG. Critical issues and current challenges in osteoporosis and fracture prevention. An overview of unmet needs. Ther Adv Musculoskelet Dis. 2017;9:299-316.
-
40Muhsen IN, AlFreihi O, Abaalkhail F, AlKhenizan A, Khan M, Eldali A, et al. Bone mineral density loss in patients with cirrhosis. Saudi J Gastroenterol. 2018;24:342-7.
-
41Raszeja-Wyszomirska J, Kucharski R, Zygmunt M, Safranow K, Miazgowski T. The impact of fragility fractures on health-related quality of life in patients with primary sclerosing cholangitis. Hepat Mon. 2015;15:e25539.
-
42Arteh J, Narra S, Nair S. Prevalence of vitamin D deficiency in chronic liver disease. Dig Dis Sci . 2010;55:2624-8.
-
43Fisher L, Fisher A. Vitamin D and parathyroid hormone in outpatients with noncholestatic chronic liver disease. Clin Gastroenterol Hepatol. 2007;5:513-20.
-
44Karoli Y, Karoli R, Fatima J, Manhar M. Study of Hepatic Osteodystrophy in Patients with Chronic Liver Disease. J Clin Diagn Res. 2016;10:31-4.
-
45Rouillard S, Lane NE. Hepatic osteodystrophy. Hepatology. 2001;33:301-7.
-
46Wariaghli G, Allali F, El Maghraoui A, Hajjaj-Hassouni N. Osteoporosis in patients with primary biliary cirrhosis . Eur J Gastroenterol Hepatol . 2010;22:1397-401.
-
Disclosure of funding: no funding received
Publication Dates
-
Publication in this collection
15 Apr 2022 -
Date of issue
Jan-Mar 2022
History
-
Received
07 Mar 2021 -
Accepted
23 Aug 2021