Abstracts
OBJECTIVE: To describe the prevalence and characteristics of epilepsy in patients with cerebral palsy in a tertiary center. METHODS: a total of 100 consecutive patients with cerebral palsy were retrospectively studied. Criteria for inclusion were follow-up period for at least 2 years. Types and incidence of epilepsy were correlated with the different forms of cerebral palsy. Other factors associated with epilepsy such as age of first seizure, neonatal seizures and family history of epilepsy were also analysed. RESULTS: follow-up ranged between 24 and 151 months (mean 57 months). The overall prevalence of epilepsy was 62%. Incidence of epilepsy was predominant in patients with hemiplegic and tetraplegic palsies: 70.6% and 66.1%, respectively. First seizure occurred during the first year of life in 74.2% of patients with epilepsy. Generalized and partial were the predominant types of epilepsy (61.3% and 27.4%, respectively). Thirty-three (53.2%) of 62 patients were seizure free for at least 1 year. Neonatal seizures and family history of epilepsy were associated with a higher incidence of epilepsy. CONCLUSIONS: epilepsy in cerebral palsy can be predicted if seizures occur in the first year of life, in neonatal period and if there is family history of epilepsy.
epilepsy; cerebral palsy; neonatal seizures
OBJETIVO: descrever sobre a prevalência e características da epilepsia em crianças com paralisia cerebral atendidas num serviço terciário. MÉTODO: um total de 100 pacientes com paralisia cerebral foi estudado retrospectivamente, tendo como critérios de inclusão o seguimento regular por pelo menos 2 anos. Os tipos e a incidência de epilepsia foram correlacionados com as diferentes formas de paralisia cerebral. Outros fatores associados com a ocorrência de epilepsia como idade da primeira crise, crises neonatais e história familiar de epilepsia também foram analisados. RESULTADOS: o tempo de seguimento variou de 24 a 151 meses (média 57 meses). A prevalência total de epilepsia foi 62%. Os pacientes com as formas hemiplégicas e tetraplégicas de paralisia cerebral tiveram a maior incidência de epilepsia: 70,6% e 66,1%, respectivamente. A primeira crise ocorreu durante o primeiro ano de vida em 74,2% dos pacientes com epilepsia. As epilepsias do tipo generalizada e parcial foram as predominantes (61,3% e 27,4%, respectivamente). Trinta e três (53,2%) de 62 pacientes permaneciam há pelo menos um ano livres das crises. Crises neonatais e história familiar de epilepsia estiveram associadas com maior incidência de epilepsia. CONCLUSÕES: epilepsia na paralisia cerebral pode ser prevista se ocorrerem crises no primeiro ano de vida e no período neonatal, e se existe história familiar de epilepsia.
epilepsia; paralisia cerebral; crises neonatais
EPILEPSY IN CHILDREN WITH CEREBRAL PALSY
Isac Bruck1 1 Center of Pediatric Neurology (CENEP) Pediatric Department Clinical Hospital, Federal University of Parana (UFPR); Assistant Professor; 2 Medical Resident in Pediatric Neurology; 3 Academic Medicine UFPR. , Sérgio Antônio Antoniuk1 1 Center of Pediatric Neurology (CENEP) Pediatric Department Clinical Hospital, Federal University of Parana (UFPR); Assistant Professor; 2 Medical Resident in Pediatric Neurology; 3 Academic Medicine UFPR. , Adriane Spessatto2 1 Center of Pediatric Neurology (CENEP) Pediatric Department Clinical Hospital, Federal University of Parana (UFPR); Assistant Professor; 2 Medical Resident in Pediatric Neurology; 3 Academic Medicine UFPR. ,Ricardo Schmitt de Bem3 1 Center of Pediatric Neurology (CENEP) Pediatric Department Clinical Hospital, Federal University of Parana (UFPR); Assistant Professor; 2 Medical Resident in Pediatric Neurology; 3 Academic Medicine UFPR. , Romeu Hausberger3 1 Center of Pediatric Neurology (CENEP) Pediatric Department Clinical Hospital, Federal University of Parana (UFPR); Assistant Professor; 2 Medical Resident in Pediatric Neurology; 3 Academic Medicine UFPR. , Carlos Gustavo Pacheco3 1 Center of Pediatric Neurology (CENEP) Pediatric Department Clinical Hospital, Federal University of Parana (UFPR); Assistant Professor; 2 Medical Resident in Pediatric Neurology; 3 Academic Medicine UFPR.
ABSTRACT - Objective: To describe the prevalence and characteristics of epilepsy in patients with cerebral palsy in a tertiary center. Methods: a total of 100 consecutive patients with cerebral palsy were retrospectively studied. Criteria for inclusion were follow-up period for at least 2 years. Types and incidence of epilepsy were correlated with the different forms of cerebral palsy. Other factors associated with epilepsy such as age of first seizure, neonatal seizures and family history of epilepsy were also analysed. Results: follow-up ranged between 24 and 151 months (mean 57 months). The overall prevalence of epilepsy was 62%. Incidence of epilepsy was predominant in patients with hemiplegic and tetraplegic palsies: 70.6% and 66.1%, respectively. First seizure occurred during the first year of life in 74.2% of patients with epilepsy. Generalized and partial were the predominant types of epilepsy (61.3% and 27.4%, respectively). Thirty-three (53.2%) of 62 patients were seizure free for at least 1 year. Neonatal seizures and family history of epilepsy were associated with a higher incidence of epilepsy. Conclusions: epilepsy in cerebral palsy can be predicted if seizures occur in the first year of life, in neonatal period and if there is family history of epilepsy.
KEY WORDS: epilepsy, cerebral palsy, neonatal seizures.
Epilepsia em crianças com paralisia cerebral
RESUMO - Objetivo: descrever sobre a prevalência e características da epilepsia em crianças com paralisia cerebral atendidas num serviço terciário. Método: um total de 100 pacientes com paralisia cerebral foi estudado retrospectivamente, tendo como critérios de inclusão o seguimento regular por pelo menos 2 anos. Os tipos e a incidência de epilepsia foram correlacionados com as diferentes formas de paralisia cerebral. Outros fatores associados com a ocorrência de epilepsia como idade da primeira crise, crises neonatais e história familiar de epilepsia também foram analisados. Resultados: o tempo de seguimento variou de 24 a 151 meses (média 57 meses). A prevalência total de epilepsia foi 62%. Os pacientes com as formas hemiplégicas e tetraplégicas de paralisia cerebral tiveram a maior incidência de epilepsia: 70,6% e 66,1%, respectivamente. A primeira crise ocorreu durante o primeiro ano de vida em 74,2% dos pacientes com epilepsia. As epilepsias do tipo generalizada e parcial foram as predominantes (61,3% e 27,4%, respectivamente). Trinta e três (53,2%) de 62 pacientes permaneciam há pelo menos um ano livres das crises. Crises neonatais e história familiar de epilepsia estiveram associadas com maior incidência de epilepsia. Conclusões: epilepsia na paralisia cerebral pode ser prevista se ocorrerem crises no primeiro ano de vida e no período neonatal, e se existe história familiar de epilepsia.
PALAVRAS-CHAVE: epilepsia, paralisia cerebral, crises neonatais.
Cerebral palsy (CP) is a chronic disorder of movement and posture. It is the result of a non-progressive damage of the immature nervous system caused by several factors1 that have occurred in prenatal, perinatal or postnatal periods2-5. It can manifest itself in several ways, mainly as spastic, athetoid and ataxic palsies; moreover, it is one of the most common causes of motor disability in children and frequently is associated with other problems, such as mental retardation, sensory defects and epilepsy6.
The significance of epilepsy in patients with CP is discussed controversially in the literature. There are studies showing that epilepsy varies from 12 to ninety percent in children with CP7-11. Some authors argue that in certain types of CP occur higher rate of epilepsy6 and has been seen that about one third of the patients with CP exhibit seizures and this figure is proportional to the degree of motor and cognitive disabilities12,13.
The present study aimed to describe the prevalence and characteristics of epilepsy in a population of patients with cerebral palsy.
METHOD
In a retrospective study were reviewed the charts of 100 consecutive patients with cerebral palsy evaluated between 1996 and 1998 in the Pediatric Neurology Unit at Clinical Hospital of Federal University of Parana (HC-UFPR), for at least 2 years. The following data were obtained: gender, gestational age (prematures, matures, or postmatures newborns), follow-up period in the service, age at manifestation of CP, types of CP, its etiology (prenatal, perinatal, postnatal or unknown)14, its degree of severity (very severe: when patients do not have any postural control; severe: can walk with maximum support or, in hemiplegic patients it does not have voluntary manual grasp; moderate: can walk with some support or when the patient globally used the paretic hand without possibility of individual movements of the fingers and; mild: can walk independently15. Mental subnormality (that was evaluate through the level of speech: aphasia, monosyllable, disyllable, sentences; and school performance: do not attend, special school, special classroom in regular school, normal classroom in regular school16,17 and; age at manifestation of epilepsy, types of epilepsy, use of antiepileptic drugs, neonatal seizures, family history of seizures and findings from electroencephalogram (EEG) and computed tomography (CT) scan of the brain.
Patients were included into CP types based upon the classification proposed by Nelson et al.18: spastic tetraplegia (spasticity of all four limbs with involvement of the arms more marked than or equal to that of the legs), spastic diplegia (spasticity of the lower extremities with a variable but a lesser degree of involvement of the upper limbs), spastic hemiplegia (spasticity of the arm and leg on one side), hypotonic and mixed forms (the last one encopass a combination of previous types, as well as athetoid, ataxic and dystonic, due to reduce number of cases).
Epilepsy was defined as the occurrence of at least two unprovoked epileptic seizures that were not diagnosed as neonatal or as febrile seizures19. The diagnosis was based on history, clinical description and EEG's findings. Epilepsies were classified in accordance with the International Classification of Epilepsies and Seizure Disorders (ILAE - 1989)20, in which are defined four main categories: partial (including simple, complex and secondary generalized), generalized (including absences, tonic, clonic, tonic-clonics and myoclonics), infantile spasms and undeterminate (when it does not fit in any of the previous category). Seizure outcome was defined as good when the patients were seizure free during the last year while using drugs and when they did not have any relapse of seizures two years after withdrawal of antiepileptic drugs (AED).
Results were evaluated by means of a descriptive method guided by the Statistic Laboratory of the Federal University of Parana, Brazil. Differences among groups were assessed by non-parametric tests: Fisher's Exact Test or chi-square test when appropriate and using the EPI-INFO - Version 6.0 epidemiological package21.
RESULTS
A total of 100 patients with the diagnosis of CP were included in this study (49 girls and 51 boys). Ages ranged from 24 to 209 months (mean age 88,4 months) and the diagnosis of CP from 1 to 96 months (mean age 8,2 months). Followed up period ranged from 24 to 151 months (means 57 months). From them, 19 were prematures, 79 matures and only 2 postmatures.
As far as etiology of CP, 41 were prenatal, 37 perinatal and 10 postnatal. In 12 it could not be determined (Table 1). Fifty six were tetraplegic and most of them with very severe and severe disabilities, 17 hemiplegic, 10 hypotonic, 10 mixed and 7 diplegic (Table 2).
Sixty nine patients had seizures, and 62 (89.9%) of them developed epilepsy. The average age of the onset of epilepsy was 12.59 months, with the first seizure occurring during the first year of live in 74.2% of the patients.
The incidence and the types of epilepsy in 100 patients with cerebral palsy is shown in Figure 1.
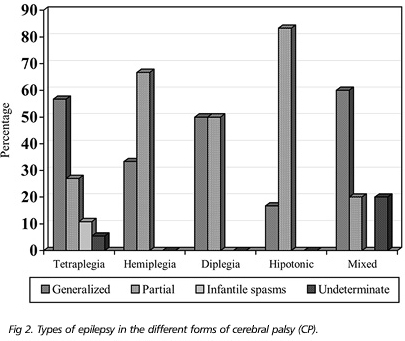
The only significant difference of incidence of epilepsy in the different types of CP was in spastic hemiplegia when comparing with spastic diplegia since epilepsy occurred in twelve patients (70.6%) with spastic hemiplegia and in only two patients with spastic diplegia (p<0.03). The distribution of types of epilepsy in the different forms of CP is shown in Figure 2. History of neonatal seizures and family history of epilepsy were correlated with a higher prevalence of epilepsy (p<0.004 and p<0.02 respectively) (Table 3).
There was not apparently any relationship between epilepsy and cognitive level; however, 38 of 46 children with both epilepsy and age above 59 months were unable to speak and 42 of them were placed in special schools or did not attend any type of school (Table 4). Twenty two (78.6%) of 28 children with aphasia and 15 (75%) of 20 patients who were not attending any type of school carried the diagnosis of CP tetraplegic.
Regarding response to anticonvulsant therapy, control of seizures was achieved in 33 cases (53.2%) and 8 of them are without any antiepileptic drug (n=29) (Table 5).
DISCUSSION
Epilepsy is one of the most prevalent neuroimpairment in childhood and is present in 4.0 - 8.8 per 1000 in population-based studies22. When other neuroimpairments (i.e., mental retardation and cerebral palsy) are present, the proportion of epilepsy in these children is strikingly higher23. Although seizures can be controlled by pharmacotherapy, epilepsy remains a major cause of anxiety for the family who had children with CP.
The patients in this sample are not necessarily representative of the population of children and adolescents with CP since the HC-UFPR is a tertiary institution and for this reason a great number of patients coming to the clinic are the most severely affected.
The literature mentioned that there is a straight relationship between epilepsy and degree of motor impairment, as well as their association with mental retardation13,24-26. In our study this is also true, since the majority of tetraplegic patients presented epilepsy and intellectual impairment .
Approximately 74% of the children with CP had their first seizure under 12 months, which is in accordance with Zafeiriou et al.27, while is in contrast with other studies in which the incidence is only 10%28.
The incidence of epilepsy in our sample was greater when comparing with the literature29,30, perhaps related to the higher degree of motor and mental disabilities of the patients studied in these population7,28.
The predominant form of epilepsy was generalized, what is in accordance with some studies accomplished in children with or without CP12,25,31. Niedemayer32 justified this finding saying that the generalized epileptiform activity can be attributed either to a genetic predisposition, or to a quick secondary bilateral synchronization, such as the one induced sometimes by a frontal focus. On rare occasions, deep subcortical cerebral lesion can also generate this kind of epileptiform activity.
The presence of neonatal seizures has been a useful marker for subsequent epilepsy in CP28. History of neonatal seizures were found in 30 (48.4%) patients from our population studied.
Normal CT findings were recorded in only 9 from 57 patients with CP and epilepsy, but this group showed a high degree of motor impairment (2 with very severe, 3 with severe and 4 with moderate motor disability) and when mental subnormality was evaluated all the patients were incapable to articulate words and do not attend any type of school and when so did it in especial schools. The generalized epilepsy was the predominant form in these patients and only 2 were seizure free, one on and the other without AED.
From the patients with CP and epilepsy treated with antiepileptic drugs, 33 (53.2%) were free of seizures, the majority of them on monotherapy. Similar results were obtained in other studies12,30,33. Skatvedt34 found a remission of epilepsy in 43.5% of 46 children with cerebral palsy after 1 year of follow-up. From the 8 patients without use of antiepileptic drugs that are more than 2 years under seizures control, 6 had the generalized form of epilepsy and 5 of them had mild degree of motor impairment. From 29 patients with epilepsy could not achieved a good control, 18 (62.1%) were on polytherapy.
In this study the majority of patients had a severe form of CP and as was mentioned before, there is straight relationship between degree of severity and occurrence of epilepsy. Neonatal seizures and positive family history were a common finding associated with epilepsy, and it is difficult to have seizure control in these patients.
Although none of the patients of this study was submitted to surgery intervention, the new antiepileptic drugs and advances on surgery intervention are promising in improving the care of epileptic children with mental retardation and cerebral palsy, offering a better quality of life and allowing the integration of these patients and their families in the society.
Received 20 July 2000, received in final form 16 October 2000. Accepted 20 October 2000.
Dr. Isak Bruck - CENEP - Rua Floriano Essenfelder 81 - 80060-270 Curitiba PR - Brasil. Fax: (41) 264 9101 / 362 9380
- 1. Curatolo P, Arpino C, Stazi MA, Medda E. Risk factors for the co-occurrence of partial epilepsy, cerebral palsy and mental retardation. Dev Med Child Neurol 1995;37:776-782.
- 2. Ellenberg JH, Nelson KB. Early recognition of infants at high risk for cerebral palsy: examination at age four months. Dev Med Child Neurol 1981; 23:705-716.
- 3. Brett EM. Cerebral palsy, perinatal injury to the spinal cord and brachial plexus birth injury. In Brett EM (ed.) Paediatric neurology. Edinburgh: Churchill Livingstone, 1983.
- 4. Hanefeld F. Infantile Zerebralparesen. In Hopf HC, Poeck K, Schliack H (eds) Neurologie in Praxis und Klinic. Stuttgart: Thieme, 1983.
- 5. Ingram T. Paediatric aspects of cerebral palsy. Edinburgh: Churchill Livingstone, 1964.
- 6. Arts WFH, Visser LH, Loonen MCB, Tjiam AT, Stroink H, Stuurmanm PM. Follow-up of 146 children with epilepsy after withdrawal of antiepileptic therapy. Epilepsia 1988; 29:244-250.
- 7. Aicardi J. Epilepsy in brain-injured children. Dev Med Child Neurol 1990;32:191-202.
- 8. Aicardi J, Bax M. Cerebral palsy. In Aicardi J (ed.) Diseases of the nervous system in childhood. Clinics in Developmental Medicine No. 115/118. London: Mac Keith Press 1992:330-374.
- 9. Rossiter EJR, Hallowes R, Pearson RD. Developmental assessment of children who had one or more convulsive episodes. Austr Paediatr J 1977;13:182-186.
- 10. Edebol-Tysk K. Preliminary results of studies on tetraplegic cerebral palsy. (Abstr) Spastics Society International Symposium, Cambridge 1984.
- 11. Aksu E. Nature and prognosis of seizures in patients with cerebral palsy. Dev Med Child Neurol 1990;32: 661-668.
- 12. Suma P, Sánches López A, Pedrola GD, Ponces VJ, Boira CM. Consideraciones acerca de la parálisis cerebral infantil y su relación com alteraciones electroencefalográficas y epilepsia. An Esp Pediatr 1988;28:197-200.
- 13. Benassi G, Guarino M, Cammarata S, et al. An epidemiological study on severe mental retardation among school children in Bologna, Italy. Dev Med Child Neurol 1990; 32: 895-901.
- 14. Diament A. Encefalopatias crônicas na infância (Paralisia Cerebral). In Diament A, Cypel S (eds) Neurologia infantil. 3.Ed. Săo Paulo: Atheneu. 1996:791-797.
- 15. Arguelles PP, Lima JM, Vilaplana FS. Epilepsia en nińos com parálisis cerebral. Acta Pediatr Esp 1995;53:304-308.
- 16. Hecaen H. Language representation and brain. In Beremberg SR. Fetal and infant development. Hage: Martineis Nijhoff Medical Division, 1977:112.
- 17. Krashen S. Lateralization language learning and critical period: some new evidences. Langu Learn 1973;23:63-67.
- 18. Nelson KB, Swaiman KF, Russman BS. Cerebral palsy. In Swaiman KF (ed.) Pediatric neurology: principles and practice. St Louis: Mosby, 1994.
- 19. Commission on Epidemiology and Prognosis of the International League Against Epilepsy. Guidelines for epidemiologic studies on epilepsy. Epilepsia 1993;34:592-596.
- 20. Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia 1989;30:389-399.
- 21. Dean AG, Dean JA, Coulombier D, et al. Epi-info. Version 6: a word processing data base and statistics program for epidemiology on microcomputers. Atlanta, Georgia, USA: Centres for Disease Control and Prevention, 1994.
- 22. Steffenburg U, Hagberg G, Kyllerman M. Characteristics of seizures in a population-based series of mentally retarded children with active epilepsy. Epilepsia 1996;37: 850-856.
- 23. Steffenburg U, Hagberg B, Olow I. The changing panorama of cerebral palsy in Sweden: VI. Prevalence and origin during the birth year period 1983-1986. Acta Paediatr 1993;82:387-393.
- 24. Goulden KJ, Shinnar S, Koller H, Katz M, Richardson SA. Epilepsy in children with mental retardation: a cohort study. Epilepsia 1991;32:690-697.
- 25. Lagergren J. Children with motor handicaps: epidemiological, medical and socio-paediatric aspects of motor handicapped children in a Swedish county. Acta Paediatr Scand 1981;Suppl 289:1-71.
- 26. Viggedal G, Steffenburg U, Hagberg G, Kyllerman M. Active epilepsy in mentally retarded children. I. Prevalence and additional neuroimpairments. Acta Paediatr 1995;84:1147-1152.
- 27. Zafeiriou D, Kontopoulos E, Tsikoulas I. Characteristics and prognosis of epilepsy in children with cerebral palsy. J Child Neurol 1999;14:289-294.
- 28. Kwong KL, Wong SN, So KT. Epilepsy in children with cerebral palsy. Pediatr Neurol 1998;19:31-36.
- 29. Sussová J, Seidl Z, Faber J. Hemiparetic forms of cerebral palsy in relation to epilepsy and mental retardation. Dev Med Child Neurol 1990;32:792-795.
- 30. Hadjipanayis A, Hadjichristodoulou C, Yoroukos S. Epilepsy in patients with cerebral palsy. Dev Med Child Neurol 1997;39:659-663.
- 31. Gibbs FA, Gibbs EL, Meyer A, Perstein MA, Rich CL. Electroencephalographic and clinical aspects of cerebral palsy. Pediatrics 1963;32:73-84.
- 32. Niedermayer E. Abnormal EEG patterns (epileptic and paroxysmal). In Niedermayer E, DaSilva FL (eds): Electroencephalography: basic principles, clinical applications and related fields. Baltimore: Urban & Schwarzemberg ,1987:405-510.
- 33. Trevathan E, Yeargin-Allsopp M, Murphy CC, Ding G. Epilepsy among children with mental retardation. Ann Neurol 1988;24:321.
- 34. Skatvedt M. Cerebral palsy: a clinical study of 370 cases. Acta Paediatr 1958;46(Suppl 111):72-83.
Publication Dates
-
Publication in this collection
06 Apr 2001 -
Date of issue
Mar 2001
History
-
Reviewed
16 Oct 2000 -
Received
20 July 2000 -
Accepted
20 Oct 2000