Abstracts
OBJECTIVE: We compare duplex scan (DS) and magnetic resonance angiography (MRA) with digital angiography (DGA) in respect to accuracy in measuring internal carotid artery (IC) stenosis in symptomatic patients. METHOD: Ten symptomatic patients with IC stenosis greater than 70% previously diagnosed by DS were submitted to another DS and to both MRA and DGA. Both ICs from each patient (total 20 ICs) were evaluated by physicians blinded for the results of other tests. DS and MRA were compared with DGA, using the intraclass correlation coeficient (r) and its 95% confidence interval (95% ci). For each diagnostic test, the study group (20 Ics) was also divided in surgical patients (IC stenosis between 70 and 99%) and non surgical patients, using kappa concordance coeficient (k) to compare the results. RESULTS: Main comparisons are: DS and DGA, r = 0.71 (0.4 - 0.87); MRA and DGA, r = 0.61 (0.25 - 0.82). After division into surgical vs. non-surgical groups, k = 0.857 (p < 0.0001) between DS and DGA; and k = 0.545 (p = 0.003) between MRA and DGA. Most DS and MRA errors occurred in IC sub-occlusions. CONCLUSION: The results suggest that when they are used together, DS and non-contrast MRA may substitute DGA in the evaluation of patients for IC stenosis surgery, except when there is discordance between their results or when the methods show sub-occlusive stenosis.
carotid stenosis; diagnosis; cerebrovascular disease; comparative study
OBJETIVO: Foram comparados duplex scan (DS) e angio-ressonância magnética (AGRM) com angiografia digital (AGD) na avaliação da estenose da artéria carótida interna (CI). MÉTODO: Foram estudados 10 pacientes sintomáticos com estenose da CI superior a 70% em estudos de triagem com DS. Os pacientes foram submetidos a novo DS, AGRM e AGD para estudo de ambas as CIs (total 20 CIs). O DS e a AGRM foram comparados com a AGD utilizando-se o coeficiente de correlação intra-classe (r) e o seu intervalo de confiança a 95% (ic 95%). Para cada método diagnóstico, o grupo de pacientes (considerando as 20 CIs) foi também dicotomizado em casos cirúrgicos (estenose entre 70% e 99%) e não cirúrgicos, utilizando-se o coeficiente kappa de concordância (k). RESULTADOS: Na comparação entre DS e AGD, obteve-se r = 0,71 (0,4 - 0,87). Entre AGRM e AGD, r = 0,61 (0,25 - 0,82). Após a dicotomização da amostra, obteve-se, entre DS e AGD, k = 0,857, p < 0,0001; e entre AGRM e AGD, k = 0,545, p = 0,003. A maioria dos erros de DS e AGRM ocorreu nos casos de suboclusão arterial. CONCLUSÃO: Os resultados sugerem que o DS e a AGRM, usados em conjunto, podem substituir a AGD na indicação da endarterectomia carotídea, exceto quando há discordância entre os dois ou quando algum dos métodos detecta suboclusão arterial.
estenose carotídea; diagnóstico; estudo comparativo; transtornos cérebro-vasculares
INTERNAL CAROTID ARTERY STENOSIS
Comparison of duplex scan and magnetic resonance angiography with digital subtraction angiography
Marco Oliveira Py1 1 Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro, Rio de Janeiro RJ, Brazil: Neurological Service, Department of Internal Medicine; 2 Department of Radiology; 3 IRM ¾ Instituto de Ressonância Magnética; 4 PREVILAB. , Charles André1 1 Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro, Rio de Janeiro RJ, Brazil: Neurological Service, Department of Internal Medicine; 2 Department of Radiology; 3 IRM ¾ Instituto de Ressonância Magnética; 4 PREVILAB. , Feliciano Silva de Azevedo2 1 Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro, Rio de Janeiro RJ, Brazil: Neurological Service, Department of Internal Medicine; 2 Department of Radiology; 3 IRM ¾ Instituto de Ressonância Magnética; 4 PREVILAB. , Romeu Côrtes Domingues3 1 Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro, Rio de Janeiro RJ, Brazil: Neurological Service, Department of Internal Medicine; 2 Department of Radiology; 3 IRM ¾ Instituto de Ressonância Magnética; 4 PREVILAB. , Rodrigo Ferraz Salomão4 1 Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro, Rio de Janeiro RJ, Brazil: Neurological Service, Department of Internal Medicine; 2 Department of Radiology; 3 IRM ¾ Instituto de Ressonância Magnética; 4 PREVILAB.
ABSTRACT - OBJECTIVE: We compare duplex scan (DS) and magnetic resonance angiography (MRA) with digital angiography (DGA) in respect to accuracy in measuring internal carotid artery (IC) stenosis in symptomatic patients. METHOD: Ten symptomatic patients with IC stenosis greater than 70% previously diagnosed by DS were submitted to another DS and to both MRA and DGA. Both ICs from each patient (total 20 ICs) were evaluated by physicians blinded for the results of other tests. DS and MRA were compared with DGA, using the intraclass correlation coeficient (r) and its 95% confidence interval (95% ci). For each diagnostic test, the study group (20 Ics) was also divided in surgical patients (IC stenosis between 70 and 99%) and non surgical patients, using kappa concordance coeficient (k) to compare the results. RESULTS: Main comparisons are: DS and DGA, r = 0.71 (0.4 - 0.87); MRA and DGA, r = 0.61 (0.25 - 0.82). After division into surgical vs. non-surgical groups, k = 0.857 (p < 0.0001) between DS and DGA; and k = 0.545 (p = 0.003) between MRA and DGA. Most DS and MRA errors occurred in IC sub-occlusions. CONCLUSION: The results suggest that when they are used together, DS and non-contrast MRA may substitute DGA in the evaluation of patients for IC stenosis surgery, except when there is discordance between their results or when the methods show sub-occlusive stenosis.
KEY WORDS: carotid stenosis, diagnosis, cerebrovascular disease, comparative study.
Estenose da artéria carótida interna extracraniana: comparação de duplex-scan e angio-ressonância com angiografia digital
RESUMO - OBJETIVO: Foram comparados duplex scan (DS) e angio-ressonância magnética (AGRM) com angiografia digital (AGD) na avaliação da estenose da artéria carótida interna (CI). MÉTODO: Foram estudados 10 pacientes sintomáticos com estenose da CI superior a 70% em estudos de triagem com DS. Os pacientes foram submetidos a novo DS, AGRM e AGD para estudo de ambas as CIs (total 20 CIs). O DS e a AGRM foram comparados com a AGD utilizando-se o coeficiente de correlação intra-classe (r) e o seu intervalo de confiança a 95% (ic 95%). Para cada método diagnóstico, o grupo de pacientes (considerando as 20 CIs) foi também dicotomizado em casos cirúrgicos (estenose entre 70% e 99%) e não cirúrgicos, utilizando-se o coeficiente kappa de concordância (k). RESULTADOS: Na comparação entre DS e AGD, obteve-se r = 0,71 (0,4 - 0,87). Entre AGRM e AGD, r = 0,61 (0,25 - 0,82). Após a dicotomização da amostra, obteve-se, entre DS e AGD, k = 0,857, p < 0,0001; e entre AGRM e AGD, k = 0,545, p = 0,003. A maioria dos erros de DS e AGRM ocorreu nos casos de suboclusão arterial. CONCLUSÃO: Os resultados sugerem que o DS e a AGRM, usados em conjunto, podem substituir a AGD na indicação da endarterectomia carotídea, exceto quando há discordância entre os dois ou quando algum dos métodos detecta suboclusão arterial.
PALAVRAS-CHAVE: estenose carotídea, diagnóstico, estudo comparativo, transtornos cérebro-vasculares.
Stroke is a major cause of mortality and disability worldwide. Some authors estimate a prevalence rate of 2.5% and 1.6%, respectively, for men and women, reaching 11.6% and 10.5% for men and women over 85 years-old1. In the USA there are 500,000 new strokes per year, 150,000 deaths and three million survivors with disability2,3. In Brazil, stroke is the third cause of mortality, after cancer and cardiovascular diseases in general4,5.
Extracranial internal carotid artery (IC) stenosis is an important risk factor for cerebrovascular disease6,7. Endarterectomy is an efficient procedure to prevent stroke in patients with severe symptomatic IC stenosis8-12. Digital angiography (DGA) is the standard method to evaluate IC stenosis and to indicate endarterectomy8-10. However, there is a 1 to 4% risk of stroke or death related to this method6,13,14. Also, there is some error related to DGA, as shown when inter-observer concordance is assessed14-16. The present study compares two non-invasive procedures to DGA, attempting to reduce the risks and costs attributed to DGA, as other authors have done before14,16-23.
Magnetic resonance angiography (MRA) can distinguish moving and stationary images, as blood flow inside the vessels. Bi or tri-dimensional images can be obtained and the most frequently used technique is the "time of flight". Paramagnetic contrast may increase the accuracy of the stenosis' measurement13. Some conditions, such as claustrophobia, pacemakers and some kinds of prothesis limit the use of MRA13.
Another diagnostic procedure is duplex scan (DS), which consists in the union of B-mode and Doppler, also using color-Doppler to improve its precision15. B-mode ultrasound allows visualization of a vessel and its wall in grades of gray, while the Doppler effect can be used to obtain information about blood flow velocity24. New technologies, like power-Doppler and "ultrasound contrast" make this exam even more accurate15,25. DS is a safe, non-invasive exam and can be done on bedside, although it is a professional-dependent method13,18.
Some authors compared these three methods to assess the possible indication of IC endarterectomy without DGA, but the methodology is quite variable in different studies. For instance, complications after endarterectomy in patients previously evaluated with MRA and DGA were used as a parameter of efficacy19. Other authors considered the degree of IC stenosis observed during surgery as the gold standard21.
Some studies on this issue divide IC stenosis in categories, from simple dicotomization22 to five categories18. There is also a report distinguishing only occlusion and sub-occlusion16. Continuos numeric variables were also compared14. There is no agreement about the accuracy of non-invasive methods in the various studies. Some showed bad results16,18,20,23, while others obtained good correlation with only limited restrictions, mainly in cases of IC sub-occlusion or when DS and MRA disagree14,17,19,21,22.
Another difference among the various studies is the technology used in each one, that limit further comparison between the results. In the present paper, we intend to achieve regional data about the accuracy of DS and MRA, as compared to DGA.
METHOD
A prospective, longitudinal study with consecutive patients was performed between June 1997 and September 1999. Each diagnostic procedure was independently evaluated by the participating physicians, who were blind to the results of other tests. Ten consecutive patients were selected using the following inclusion criteria: age up to 80 years; history of transient ischemic attack (TIA) or mild stroke ¾ Rankin scale 26 up to grade two ¾ in the IC territory; a DS showing IC stenosis equal or greater than 70% in one or both extracranial ICs; and an informed consent. There were systematic exclusion criteria: kidney, liver or lung failure or cancer leading to an expected patient survival of less than five years; extensive previous stroke; severe diseases that could increase the risk of the endarterectomy; any additional contraindication to surgery or to any tests (e.g. cardiac pacemaker, claustrophobia). Following the ECST criteria10,11, the maximal interval between the neurological event and the performance of the diagnostic tests was six months.
All 10 patients participating in this study were submitted to another DS in a Acuson-Aspen machine, using a 7.5 MHz linear transducer. The same examiner (RFS) performed all the tests, including B-mode ultrasound, spectrum analysis in Doppler and color-Doppler, using a number of published and widely used hemodynamic and anatomic criteria24,27.
Hemodynamic criteria included peak systolic velocity (PSV) in the narrower point of the IC stenosis, to determine the degree of stenosis: stenosis up to 40%, if PSV less than 125 cm/sec; stenosis between 41% and 69%, if PSV between 125 and 229 cm/sec; and stenosis equal or greater than 70%, if PSV greater than 229 cm/sec.
When PSV was greater than 229 cm/sec, other variables were used: end diastolic velocity (EDV), measured in the narrower point of the stenosis; peak systolic velocity ratio (PSVr), which is the relation between PSV in the stenotic zone and PSV in normal common carotid artery; and end diastolic velocity ratio (EDVr), which is the relation between EDV in the stenotic zone and EDV in the common carotid artery. These variables agree with PSV for stenosis equal or greater than 70%, when they are greater than: 40 cm/sec; 1.8; and 2.6, respectively. In total occlusion, all values are equal to zero. Anatomic criteria for determination of the degree of stenosis were based on the measurement of the stenotic area in a transverse slice of carotid bulb in the narrower zone, using B-mode and color-Doppler. They show a precise measurement of the stenosis but are valid only when in agreement with hemodynamic criteria.
DGA was made in a Stenoscop (General Electric) machine, using Seldinger method following femoral artery catheterization, always by the same examiner (FSA). All four cervical arteries and the intracranial vessels were studied. The NASCET method9 was used to measure IC stenosis: artery diameter in the stenotic zone divided by the IC diameter distal to the stenosis, in an area free of angles.
MRA was made in a Vectra (General Electric) 0.5 Tesla machine, always by the same examiner (RCD). The technique was the bi-dimensional time of flight, with images from cervical and intracranial vessels in axial plan and multiplanar reconstruction by the maximum intensity projection (MIP) method, without paramagnetic contrast. The NASCET method9 was used to measure IC stenosis, except when there was a signal gap, indicating severe stenosis that makes it impossible to directly measure the artery diameter. In these cases, as described previously14, a 90% stenosis was diagnosed, except when reduced flow distal to stenosis was found, in which case a value of 99% stenosis was attributed. Intracranial arteries were assessed by MRA and DGA, because severe stenosis in these vessels may contraindicate endarterectomy9-12,28.
We constructed graphics comparing DS vs DGA and MRA vs DGA, as suggested by Bland and Altman29. These graphics measure the dispersion of the values over a given line, comparing the obtained values in each diagnostic test. If there is a perfect correlation between comparing variables, all values will be on the given line; the more distant from the line, the more discordant are the values.
Intraclass correlation coefficient (r) was also applied to the numeric results, measuring the correlation between each tested method and the gold standard29. The 95% confidence interval (95% ci) was calculated, determining limits of correlation with a 5% error. Sample size and variability of results were taken into account in 95% ci calculation. We also divided the study group in surgical patients ¾ IC stenosis from 70% to 99% ¾ and non-surgical patients ¾ ICs exibiting less than 70% stenosis or total occlusion. Kappa concordance coefficient (k) and its p value are given to these groups, comparing DS vs DGA and MRA vs DGA. Kappa coefficient measures observed concordance, excluding concordance by chance30,31. Sensitivity, specificity, positive predictive value and negative predictive value were also calculated for DS and MRA, with their respective 95% ci. Values of "r" and "k" were classified as bad (less than 0.4), good (0.4 to 0.75) or excellent (greater than 0.75), following Landis and Koch's criteria32.
Besides global comparison of the results, an individual analysis and comparison of each diagnostic procedure was performed: differences greater than 10% between the results were considered to indicate discordance, and differences less than 10% as indicating concordance. This level of difference was chosen because it is outside the range of measurement error33 and because meaningful increments in stroke risk occur between decile levels34.
RESULTS
Ten patients ¾ five men ¾ were included in the study, with a mean age 63.8 years (ranging from 40 to 80 years). The most common associated disease was systemic arterial hypertension (nine patients); followed by diabetes mellitus, high cholesterol levels, and cardiovascular disease (six patients each); peripheral arterial disease (three patients); and heart failure (two patients). Two patients were smokers and one ¾ a 40 year-old woman without hypertension - suffered from the anti-cardiolipin antibody syndrome.
Two patients died during the study. One from refractory cardiogenic shock after coronary bypass surgery; the other suffered sudden death. Three patients underwent endarterectomy and one presented transient complications ¾ left hemiparesis that remitted after 48 hours. One patient suffered a stroke during DGA, with partial recovery.
Six patients had TIAs and four a mild stroke as the event that brought them to study. The time since the cerebrovascular event and the first diagnostic test ranged from four days to six months (median 2.5 months). The interval between the three procedures was 9 to 104 days (median 23.5 days).
Table 1 shows the main values obtained. Figures 1 and 2 show graphics with plotted values, respectively from comparison between DS vs DGA and MRA vs DGA.
Table 2 shows the results of r, k, sensitivity, specificity, positive and negative predictive values for DS and MRA, compared with DGA. Correlation was good for both comparisons; and concordance was considered excellent for DS and good for MRA.
DISCUSSION
The results showed good correlation for both DS and MRA, compared to DGA. DS was associated with better results, as previously described14,18,22. The most important task of the diagnostic tests evaluated here is to determine which should be referred to endarterectomy. Therefore, we divided the group of patients in surgical ¾ 70% to 99% stenosis - and non-surgical ¾ less than 70% or total occlusion - IC. The 70% cut-point followed the NASCET results9, although the final results of that study12,28 have also shown benefit of endarterectomy in selected patients with 50 to 69% IC stenosis. Concordance with DGA was excellent for DS and good for MRA after such division. Sensitivity, specificity, positive and negative predictive values were also high, especially for DS.
Table 3 shows a direct comparison of the stenosis degree found in the three diagnostic methods, considering differences greater than 10%. DS displayed a tendency to overestimate the degree of IC stenosis (in nine arteries). Only in one case there was underestimation. In three cases DS observed mild stenosis, while DGA showed a normal IC. DS results alone would induce one error in indicating endarterectomy, as it identified IC sub-occlusion in a patient with total occlusion.
MRA also overestimated IC stenosis in seven arteries; and underestimated the degree of stenosis in three (always considering differences greater than 10%). Nevertheless, the most important error attributed to MRA was the misdiagnosis of sub-occlusion, in three cases, with DGA-proved total occlusion. In another IC, MRA attributed a severe degree of IC stenosis (70%), whereas DGA showed only a 50% stenosis. Thus, four patients would be incorrectly referred to endarterectomy by MRA results alone. In all cases, the time interval between diagnostic tests were less than 21 days and no new symptom appeared, reasonably excluding the possibility of a IC occlusion between the exams.
The tendency to overestimate the degree of IC stenosis, by either DS and MRA as compared to DGA, has been previously detected13,18. Other authors have also found it difficult to differentiate sub-occlusion and total occlusion of the extracranial IC, mainly with MRA, but also with DS13,14,16,18. The most common error occured when MRA and/or DS find a total occlusion but actually there was some patency of the vessel, as measured by DGA13,14,16,18. Nevertheless, the opposite error is also well documented, both for DS14,24 and MRA14,16,18. In studies evaluating inter-observer concordance, it was shown that even DGA may misdiagnose IC occlusion, possibly related to vasospasm from contrast injection or to retrograde flow through the occluded artery14,16. In a meta-analysis on the usefulness of DS and MRA in the evaluation of IC stenosis35, sensitivity in cases with total IC occlusion ranged from 0.82 to 0.86 and specificity was 0.98 for the two methods. In stenosis equal or greater than 70%, sensitivity ranged from 0.83 to 0.86 and specificity from 0.89 to 0.94.
Severe IC stenosis ¾ generally greater than 90% - leads to a phenomenon known as a signal void in MRA, which may misdiagnose total occlusion in a patent vessel13,14,16,18. On the other hand, in occluded arteries, a distal branch of external carotid artery may be misidentified as a branch of the IC14.
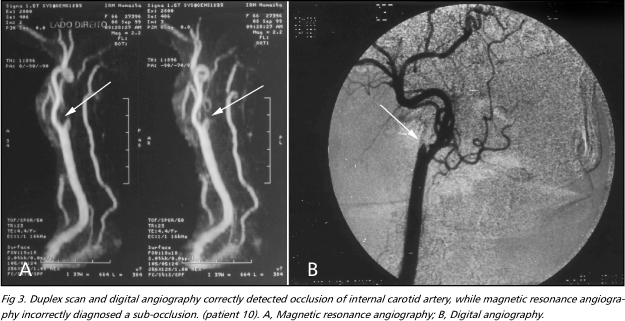
Figure 3 shows an example of misidentification of sub-occlusion by MRA. Probably a branch of the external carotid artery was thought to be the distal IC. Similarly, the most common error of DS is the misdiagnosis of occlusion in a patent artery, because of the difficulty to assess a severely reduced blood flow13,14,16,18,24. Color-Doppler, ultrasound contrast and power Doppler may minimize this possibility15,24. On the other hand, the misidentification of another artery, thought to be a branch of the IC, may misdiagnose sub-occlusion in an occluded vessel24.
Some authors suggest that when there is concordance between DS and MRA, DGA would not be necessary14,17,21. In the present study, one patient would have been incorrectly referred to surgery using these criteria. In this case ¾ in which there was a severe ipsilateral stenosis of the external carotid artery - both DS and MRA misdiagnosed IC sub-occlusion and DGA correctly showed its occlusion. Some authors indicate endarterectomy only with DS, as this procedure shows a better correlation with DGA than MRA14,18,22. Nevertheless, MRA shows anatomic information that can be helpful to the surgeon and is not available in DS studies. Also, it shows the intracranial vessels13,14,18. On the other hand, DS can determine the characteristics of the atherosclerotic plaque better than MRA or DGA15,24 and transcranial Doppler may add in evaluating the intracranial circulation36,37. Both DS and MRA are best seen as complementary techniques13,14.
New techniques may improve the accuracy of DS and MRA. For example, tri-dimensional MRA and the injection of paramagnetic contrast improve sensitivity, specificity and even the differentiation between occlusion and sub-occlusion13,17. In our study, only bi-dimensional MRA without contrast in a low-field (0.5 T) equipment was made. Also, new DS technologies not used in our study, such as power Doppler and the use of ultrasound contrast, are now available15,25. These new techniques may improve the results and should be tested in other studies, but even without them, we demonstrated a good correlation and concordance between non-invasive procedures and DGA.
We must recognize that the results presented here have large confidence intervals, reflecting the small sample size. Also, the chosen selection criteria (first DS with stenosis equal or greater than 70% in at least one extracranial IC) may have contributed to overestimate the usefulness of DS. Thus, the present study should be continued to include a greater number of patients and reduce the chance of error. Despite these limitations, we concludethat extracranial IC endarterectomy may usually be indicated following the careful analysis of the noninvasive exams - DS and MRA. The main exceptions occur when there is discordance between DS and MRA; when it is not possible to study the patient with either DS or MRA; and in cases with apparent sub-occlusion. In these cases, DGA seems imperative.
Acknowledgements ¾ We are in debt with Professor Ronir Raggio Luiz for planning the statistical analysis of this study.
Received 31 January 2001, received in final form 4 May 2001. Accepted 14 May 2001.
Dr. Marco Oliveira Py ¾ Rua Gal. Ribeiro da Costa 38/401 - 22010-050 Rio de Janeiro RJ ¾ Brasil. E-mail: marcopy@uninet.com.br
- 1. Bots ML, Looman SJ, Koudstaal PJ, Hofman A, Hoes AW, Grobbee DE. Prevalence of stroke in the general population. The Rotterdam study. Stroke 1996;27:1499-1501.
- 2. Adams HP Jr, Brott TG, Crowell RM, et al. Guidelines for the management of patients with acute ischemic stroke: a statement for healthcare professionals from a special writing group of the stroke council, American Heart Association. Stroke 1994;25:1901-1914.
- 3. Marshall RS, Mohr JP. Current management of ischemic stroke. J Neurol Neurosurg Psichiatry 1993;56:6-16.
- 4. Fernandes JG. Modificaçăo de fatores de risco para as doenças cerebrovasculares isquęmicas. In Gagliardi RJ (ed). Doenças cerebrovasculares: condutas. Săo Paulo: Geo-Gráfica e Editora 1996:39-50.
- 5. Gomes MM, Becker RA. Diferenças demográficas na incidęncia das doenças cerebrovasculares no Brasil. Rev Bras Neurol 1990;26:10-14.
- 6. Feinberg WM, Albers GW, Barnett HJM et al. Guidelines for the management of transient ischemic attacks. Stroke 1994;25:1320-1335.
- 7. Albers GW, Hart RG, Lutsep HL, Newell DW, Sacco RL. Supplement to the guidelines for the management of transient ischemic attacks: a statement from the ad hoc committee on guidelines for the management of transient ischemic attacks, stroke council, American Heart Association. Stroke 1999;30:2502-2511.
- 8. Biller J, Feinberg WM, Castaldo JE, et al. Guidelines for carotid endarterectomy: a statement for healthcare professionals from a special writing group of the stroke council, American Heart Association. Circulation 1998;97:501-509.
- 9. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 1991;325:445-453.
-
10European Carotid Surgery Trialists' Collaborative Group. MRC European carotid surgery trial: interim results for symptomatic patients with severe (70-99%) or mild (0-29%) carotid stenosis. Lancet 1991;337:1235-1243.
-
11European Carotid Surgery Trialists' Collaborative Group. Randomized trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European carotid surgery trial (ECST). Lancet 1998;351:1379-1387.
- 12. Barnett HJM, Taylor DW, Eliasziw M, et al, for the North American Symptomatic Carotid Endarterectomy Trial Collaborators. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. N Engl J Med 1998;339:1415-1425.
- 13. Culebras A, Kase CS, Masdeu JC et al. Practice guidelines for the use of imaging in transient ischemic attacks and acute stroke. Stroke 1997;28:1480-1497.
- 14. Young GR, Humphrey PRD, Shaw MDM, Nixon TE, Smith ETS. Comparison of magnetic resonance angiography, duplex ultrasound, and digital subtraction angiography in assessment of extracranial internal carotid artery stenosis. J Neurol Neurosurg Psychiatry 1994;57:1466-1478.
- 15. Ringelstein EB. Sketicism toward carotid ultrasonography: a virtue, an atitude, or fanaticism? Stroke 1995;26:1743-1746.
- 16. Fürst G, Saleh A, Wenserski F et al. Reliability and validity of noninvasive imaging of internal carotid artery pseudo-occlusion. Stroke 1999;30:1444-1449.
- 17. Patel MR, Kuntz KM, Klufas RA et al. Preoperative assessment of the carotid bifurcation: can magnetic resonance angiography and duplex ultrasonography replace contrast arteriography? Stroke 1995;26:1753-1758.
- 18. Riles TS, Eidelman EM, Litt AW, Pinto RS, Oldford F, Schwartzenberg GWST. Comparison of magnetic resonance angiography, conventional angiography, and duplex scanning. Stroke 1992;23:341-346.
- 19. Dandapani BK, Grove MK. Preoperative diagnostic imaging of carotid stenosis [abstract]. Stroke 2000;31:330.
- 20. Goldstein LB. Carotid endarterectomy decision-making: noninvasive testing vs. Angiography [abstract]. Stroke 2000;31:327.
- 21. Polak JF, Kalina P, Donaldson MC, O'Leary DH, Whittemore AD, Mannick JA. Carotid endarterectomy: preoperative evaluation of candidates with combined Doppler sonography and MR angiography. Radiology 1993;186:333-338.
- 22. Polak JF, Bajakian RL, O'Leary DH, Anderson MR, Donaldson MC, Jolesz FA. Detection of internal carotid artery stenosis: comparison of MR angiography, color Doppler sonography, and arteriography. Radiology 1992;182:35-40.
- 23. Bowler JV, Chan RTK, Eliasziw M, et al. Imaging carotid stenosis: a correlative study of conventional angiography, magnetic resonance angiography and duplex Doppler [abstract]. Stroke 1999;30:237.
- 24. Reutern GM, Büdingen HJ. Ultrasound diagnosis of cerebrovascular disease: Doppler sonography of the extra and intracranial arteries, duplex scanning. Trad. Telger TC. New York: Thieme Medical Publ 1993.
- 25. Droste DW, Jürgens R, Nabavi DG, Schuierer G, Weber S, Ringelstein EB. Echocontrast-enhanced ultrasound of extracranial internal carotid artery high-grade stenosis and occlusion. Stroke 1999;30:2302-2306.
- 26. Rankin J. Cerebral vascular accidents in patients over the age of 60. Scott Med J 1957;2:200-215.
- 27. AbuRahma AF, Robinson PA, Strickler DL, Alberts S, Young L. Proposed new duplex classification for threshold stenoses used in various symptomatic and asymptomatic carotid endarterectomy trials. Ann Vasc Surg 1998;12:349-358.
- 28. Ferguson GG, Eliasziw M, Barr HWK et al, for the North American Symptomatic Carotid Endarterectomy Trial (NASCET) Collaborators. The North American Symptomatic Carotid Endarterectomy Trial. Surgical results in 1415 patients. Stroke 1999;30:1751-1758.
- 29. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307-310.
- 30. Koran LM. The reliability of clinical methods, data and judgments (first of two parts). N Engl J Med 1975;293:642-646.
- 31. Koran LM. The reliability of clinical methods, data and judgments (second of two parts). N Engl J Med 1975;293:695-701.
- 32. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-174.
- 33. Eliasziw M, Fox AJ, Sharpe BL, Barnett HJ. Carotid artery stenosis: external validity of the North American Symptomatic Carotid Endarterectomy Trial measurement method. Radiology 1997;204:229-233.
- 34. Morgenstern LB, Fox AJ, Sharpe BL, Eliasziw M, Barnett HJ, Grotta JC. The risks and benefits of carotid endarterectomy in patients with near occlusion of the carotid artery. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. Neurology 1997;48:911-915.
- 35. Blakeley DD, Oddone EZ, Hasselblad V, Simel DL, Matchar DB. Noninvasive carotid artery testing. A meta-analytic review. Ann Intern Med 1995;122:360-367.
- 36. Anzola GP, Gasparotti R, Magoni M, Prandini F. Transcranial doppler sonography and magnetic resonance angiography in the assessment of collateral hemisferic flow in patients with carotid artery disease. Stroke 1995;26:214-217.
- 37. Singh R, El-Saden S, Cohen SN et al. Intracranial vascular assessment in patients with cerebrovascular disease: can non-invasive methods replace conventional angiography?[abstract]. Stroke 1998;29:284.
Publication Dates
-
Publication in this collection
05 Oct 2001 -
Date of issue
Sept 2001
History
-
Accepted
14 May 2001 -
Received
31 Jan 2001