GUIDELINES
Guidelines for acute ischemic stroke treatment - part I
Diretrizes para tratamento do acidente vascular isquêmico - parte I
Jamary Oliveira-Filho; Sheila Cristina Ouriques Martins; Octávio Marques Pontes-Neto; Alexandre Longo; Eli Faria Evaristo; João José Freitas de Carvalho; Jefferson Gomes Fernandes; Viviane Flumignan Zétola; Rubens José Gagliardi; Leonardo Vedolin; Gabriel Rodríguez de Freitas
Executive Committee from Brazilian Stroke Society and the Scientific Department in Cerebrovascular Diseases of the Brazilian Academy of Neurology
Correspondence Correspondence: Jamary Oliveira-Filho Instituto de Ciências da Saúde Rua Reitor Miguel Calmon s/n sala 455 40110-100 Salvador BA - Brasil E-mail: jamaryof@ufba.br
These guidelines are a result of several meetings from the Brazilian Stroke Society (Sociedade Brasileira de Doenças Cerebrovasculares - SBDCV, website www.sbdcv.org.br), which represents the Scientific Department in cerebrovascular diseases of the Brazilian Academy of Neurology, responsible for technical opinions and educational projects related to cerebrovascular diseases. Members from SBDCV participated in web-based discussion forum with pre-defined themes, followed by a formal onsite meeting in which controversies and final position statements were discussed. Finally, a writing group was created to revise and translate the final document, which was approved by all members of the SBDCV. The final text aims to guide specialists and non-specialists in stroke care in managing patients with acute ischemic stroke. The hemorrhagic stroke guideline has been previously published by the same group1. In the final recommendations, Oxford classification for evidence level and recommendation grade was used:
EVIDENCE LEVELS
1. Randomized controlled clinical trial (RCT) or systematic review (SR) of RCT with clinical endpoints.
2. RCT or SR of lower quality: with substitute, validated endpoints; with subgroup analysis or with a posteriori hypotheses; with clinical endpoints, but with methodological flaws.
3. RCT with substitute, non-validated endpoints case-control studies.
4. Study with clinical endpoint, but with a higher potential bias (as in experiment without comparison group and other observational studies).
5. Representative forum or expert opinion without above-mentioned evidence.
RECOMMENDATION GRADES
A Systematic review (homogeneous) of RCT; or single RCT with narrow confidence interval; or therapeutic results of "all or nothing" type.
B Systematic review (homogeneous) of cohort studies; or cohort study and RCT of lower quality; or outcomes research or ecological study; or systematic review (homogeneous) of case-control studies; or case-control study.
C Case reports (including cohort or case-control study of lower quality).
D Expert opinion without critical evaluation, based on physiological or animal studies.
In this first part of the guidelines, specific topics included were: epidemiology, stroke as a medical emergency, education, pre-hospital management, emergency management, neuroimaging and laboratory evaluation. A translated version of these guidelines in Portuguese is available in the Society's webpage (www.sbdcv.org.br).
EPIDEMIOLOGICAL ASPECTS
Among the 58 million deaths per year worldwide, 5.7 million were caused by stroke. Therefore, stroke was the second most common cause of death, responsible for 10% of all deaths in world2. However, the global distribution is heterogeneous, as 85% of deaths occurred among developing countries and one-third affected economically active individuals2,3. This impact is expected to increase in the next decades, as projected by a 300% increase in the elderly population of developing countries in the next 30 years, specially in Latin America and Asia4.
In Brazil, stroke was responsible, in 2005, for 10% of all deaths (90,006 deaths) and for 10% of all public hospital admissions4,5. In that year, Brazil spent 2,7 billion dollars in health care on cardiac diseases, stroke and diabetes mellitus4,5.
In Latin America, stroke incidence rates adjusted for age vary between 35 and 183 per 100,0006, and, in Brazil, vary between 137 and 168 per 100,000 inhabitants7-9. In two recent studies of stroke-related mortality, a steady drop in mortality rates were observed in the last two decades10,11. Although the reasons for this drop are unknown, classically mortality rates are directly related to changes in incidence or lethality rates11. Incidence rates are influenced by socio-economical conditions and quality of primary prevention, while lethality is dependent on disease severity of the sample and quality of hospital care11. Any combination of these factors may have improved in Brazil during this time period.
STROKE: A MEDICAL EMERGENCY
The concept of stroke as a medical emergency is still not well established in Brazil. In a recent study performed in four Brazilian cities, with 814 individuals, 28 different names were given for stroke12. Only 35% knew that "192" was the appropriate emergency number in Brazil, 22% did not recognize any stroke warning sign, and only 51% would call for emergency rescue if a family member had symptoms of stroke.
Studies on recognition and activation of emergency services performed in developed countries have systematically concluded that interventions are necessary to increase the number of patients eligible for acute stroke treatment, such as educational campaigns targeting the immediate recognition of warning signs, triggering a proactive attitude towards rescuing the stroke victim.
Thus, the delay in reaching acute stroke care can be identified as one among many different factors that influence lethality. Other factors include: early identification of warning signs by the population, recall and correct use of the national emergency number "192", emergency rescue triage and priorization in transportation, hospital diagnosis, communication between health professionals and early access to neuroimaging.
The causes of delay in pre-hospital care include the lack of knowledge of stroke warning signs, denial of disease state and the hope of spontaneous resolution of symptoms. Educational initiatives should target patients at risk, as well as their family members. Considering that approximately 45-48% of patients are referred by a general clinician, educational campaigns should also be directed towards the medical community, emphasizing the importance of emergency treatment13.
Eight non-randomized studies evaluated the impact of educational measures on health care of the stroke victim; they demonstrated that thrombolysis rate increased after the educational campaign, but only during six months. This shows that an educational intervention requires periodic recycling in order to maintain a positive result14-21.
Recommendations
Periodical educational programs to increase stroke awareness in the general population are recommended (level of evidence: 1, recommendation grade: B).
Periodical educational programs to increase stroke awareness among medical professionals, other health professionals and emergency services are recommended (level of evidence: 1, recommendation grade: B).
PRE-HOSPITAL CARE AND TRANSPORTATION
Stroke is a medical and eventually surgical emergency. After time-dependent therapies have demonstrated to be successful; acute stroke management is tightly linked to this concept of emergency care. However, only a minority of patients arrive at emergency rooms on time to benefit from reperfusion therapies for the region affected by ischemia or for control of intracerebral hemorrhage22-23. This delay is due to a series of factors, including lack of knowledge of stroke warning signs to underutilization of specialized rescue services, as the Serviço de Atendimento Móvel de Urgência - SAMU (Mobile Emergency Service) in Brazil12,20,24-26. Many studies have demonstrated that utilization of private vehicles or previous contact with a primary care physician increase the time between stroke onset and hospital admission, often delaying or contraindicating reperfusion therapy27-31. However, SAMU does not exist in all Brazilian cities and in many ones it suffers from lack of equipments, human resources, educational training programs, besides the lack of a structured protocol for stroke management. Many cities also lack reference hospitals for acute stroke treatment. A multidisciplinary approach, using written protocols associated with health professional training and recycling, involving every link in a chain of pre-hospital care, is an important differential in acute stroke treatment32-35.
Aiming for a rapid sequence of recognition, emergency service activation and stroke victim rescue, transportation and treatment to become standard of care in Brazil, we recommend:
1. To initiate educational campaigns targeted toward the population, aiming at recognition of stroke warning signs and immediate activation of emergency medical services (level of evidence: 1, recommendation grade: B)12,20,24-26,32,36.
2. To encourage the immediate use of SAMU (telephone number 192) or other pre-hospital emergency services in case of an acute stroke identification. These possibilities of access should be highly publicized and known by the general population. Due to eventual communication difficulties by the patient, in cases of telephone contact, the central station should have telephone-localization capabilities (level of evidence: 1, recommendation grade: B)12,27,28,30,32.
3. The SAMU and other pre-hospital mobile systems should give maximum priority to acute stroke victims, and their professionals should be prepared to recognize, perform a basic differential diagnosis and initiate management of acute stroke using specific scales and protocols. Once stabilized, transportation should be priorized to a hospital with the best relationship between distance/technical quality, notifying the hospital previously by radio or telephone (level of evidence: 1, recommendation grade: B)32,35,37,38.
4. To perform training and continuous education for SAMU and other pre-hospital mobile system professionals (telephone service professional, MD, ambulance professionals), so that they may quickly recognize and trigger decisions on initial treatment, transportation and final destination when a stroke victim is identified (level of evidence: 1, recommendation grade: B)20,32,33.
5. To adopt, in all pre-hospital transportation: monitorization of oxygen saturation, and in all who have saturation below 95% to apply oxygen supplementation; clinical evaluation of hydration and, in case of dehydration, to apply intravenous hydration with 0.9% normal saline; finger stick testing for blood glucose, and to dispense glucose-containing fluids only in case of detected hypoglycemia (level of evidence: 1, recommendation grade: B)39-42; and not to treat systemic hypertension routinely (level of evidence: 1, recommendation grade: C)32.
6. To adopt, in all pre-hospital transportation, the systematic use of evaluation and pre-hospital triage scales, such as the Cincinnati and Los Angeles scales, to identify stroke patients, specially those who are candidates for reperfusion therapy (level of evidence: 1, recommendation grade: C)34,35.
STROKE IN THE EMERGENCY DEPARTMENT
The treatment of stroke patients in the emergency must begin with the evaluation of vital functions (ABC) and the establishment of basic support, as it is not possible to safely proceed in any diagnostic or therapeutic decision without them.
Stroke is the main differential diagnosis in patients with neurological deficits of sudden onset. In such cases, a written and multi-professional protocol allows fast diagnostic and therapeutic settling. Clinical and neurological evaluation scales assist in the standardization of the monitoring process and prognostic estimate of the cases. The treatment of stroke patients accompanied by a neurologist seems to improve the diagnostic and prognostic accuracy for these patients43-53.
It is fundamental to consider the possibility of differential diagnoses. In most cases, this is possible with information of the patient's clinical history, supported by complementary exams (neuroimaging and laboratory tests)54,55.
Stroke patients may present, as a cause or consequence, multiple organ dysfunctions, which justifies carrying out further tests. Some changes of cardiac function, particularly arrhythmias and acute myocardial infarction, are common after a stroke56-62.
There is no evidence in favor of oxygen supplementation for all patients in the acute phase of stroke. It is assumed, however, that maintaining a good oxygenation is important, especially in the penumbra region, the main therapeutic target in ischemic stroke at this stage. Altered consciousness, seizure, aspiration pneumonia, heart failure and pulmonary thromboembolism are possible complications that require special ventilatory care, although the necessity of orotracheal intubation determines, frequently, a poor prognosis39,63,64.
Dehydration in stroke patients is usually associated with a worse prognosis. Although there is no evidence of the intravenous fluid supply impact during the acute phase of stroke, it is accepted that the maintenance of adequate hydration favors homeostasis. It is observed that specialized services for the treatment of stroke (stroke units) make use of a more aggressive intravenous hydration. Hypotonic fluids, however, can bring harm, as they elevate the risk of cerebral edema and intracranial hypertension, especially in extensive infarcts65,66.
Hyperglycemia occurs in more than half of the patients in the acute phase of stroke, even the ones with no history of diabetes mellitus, and it is associated with increased morbidity and mortality, regardless of age, the mechanism of ischemic stroke or the extent of the ischemic injury. Glucose levels above 140 mg/dL are associated with worse outcomes in thrombolytic treatment and worse functional prognosis in 90 days. However, it is not clear whether normalizing glucose levels have a positive impact on prognosis, as well as the best way to correct hyperglycemia, which remains controversial. On the other hand, hypoglycemia can cause neurological dysfunction or tissue damage, representing a differential diagnosis of stroke40,67-75.
Hypertension is commonly observed in acute ischemic stroke. Reasons for this phenomenon include physiological compensation due to brain ischemia and reactive increase in mean arterial pressure secondary to progressive elevation of intracranial pressure. Some studies demonstrate neurological worsening associated with reduced blood pressure, especially on the first day. However, the recent CHHIPS study did not demonstrate neurological worsening in the actively treated group (after a 72-hour evolution), but the group with antihypertensive treatment started immediately presented lower mortality at three months. Other issues include the possibility of different effects of blood pressure reduction on the ischemic brain tissue in normotensive and hypertensive individuals, and the influence on intracranial pressure, determined by antihypertensive drugs, such as sodium nitroprusside and hydralazine, which present an intracranial vasodilator property. The answers to what would be the optimal values of blood pressure and what would be the indications and best forms of control during this period remain controversial. The tendency is to avoid aggressive interventions in acute stroke76-80.
Hypotension is rare in acute stroke patients and is usually associated with acute myocardial infarction, congestive heart failure, hypovolemia and sepsis. In a further analysis from the International Stroke Trial (IST), levels of systolic blood pressure <140 mmHg were associated with worse prognosis, which was proportionally greater for every 10 mmHg decrease in systolic blood pressure81.
Clinical and experimental observational studies show the association between hyperthermia and a worse stroke prognosis. Possible reasons for this include increased metabolic demand in a context of brain ischemia, excitotoxicity and increased local inflammatory response82-85.
Recommendations
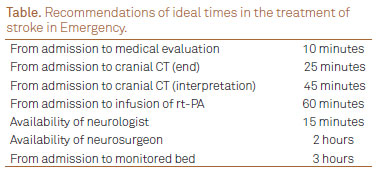
1. The treatment directed towards the type of stroke diagnosed (ischemic stroke, intraparenchymal hemorrhage or subarachnoid hemorrhage) must be initiated within 60 minutes of admission to the hospital service, ideally observing the times in
. (level of evidence: 5; recommendation grade: D)
2. Development and application of multi-professional, integrated written protocols, for the treatment of any suspected stroke cases. (level of evidence: 3B; recommendation grade: B)
3. The treatment of a stroke patient should be guided by a neurologist. (level of evidence: 2B, recommendation grade: B)
4. Perform laboratory tests for exclusion of differential diagnoses and therapeutic decision aid. (level of evidence: 5, recommendation grade: D)
5. Perform neuroimaging tests to guide therapy in acute phase of stroke. (CT - level of evidence: 1, recommendation grade: A; or MRI - level of evidence: 2B, recommendation grade: B)
6. Non-invasive cardiovascular monitoring (level of evidence: 5, recommendation grade: D)
7. Blood oxygen saturation must be evaluated in patients with acute stroke, if possible, with pulse oximetry. (level of evidence: 5, recommendation grade: D)
8. Oxygen supplementation should only be performed, if necessary, to maintain oxygen saturation at levels equal to or above 95% (level of evidence: 2B, recommendation grade: B)
9. The indication for ventilatory support and airway protection should be carefully evaluated, especially in patients with lowered level of consciousness and neurological symptoms suggestive of brainstem ischemic stroke. (level of evidence 5, recommendation grade: D)
10. The patient with acute stroke should be adequately hydrated with isotonic saline solution (e.g. 0.9% saline). The volume administered intravenously (around 100 mL/hour) should be considered individually, based on the baseline hydration and possible comorbidities that limit water supply. (level of evidence: 4, recommendation grade: C)
11. Evaluate the possible diagnosis of diabetes mellitus in patients with hyperglycemia in acute stroke, even if previously healthy, through examination of glycosylated hemoglobin. (level of evidence: 4, recommendation grade: C)
12. Prevent and treat additional causes of hyperglycemia (e.g. corticosteroids and infection). (level of evidence: 5; recommendation grade: D)
13. Use insulin to correct hyperglycemia, aiming to keep blood glucose between 80 and 140 mg/dL. (level of evidence: 5; recommendation grade: D)
14. Promptly correct hypoglycemia (blood glucose below 70 mg/dL). (level of evidence: 5; recommendation grade: D)
15. Do not reduce blood pressure in acute ischemic stroke, except when levels are extremely high (SBP>220 mmHg or DBP>120 mmHg). In these cases, reduction must not exceed 15% of the initial blood pressure values in the first 24 hours. (level of evidence: 5, recommendation grade: D)
16. Use antihypertensive medication in patients with indication for thrombolytic treatment, but with blood pressure >185 x 110 mmHg before the start of the treatment. (level of evidence 1; recommendation grade: A)
17. Utilize antihypertensive medication in acute stroke patients which, even with moderate elevations of blood pressure, present other medical indications for urgent treatment (hypertensive emergencies), such as heart failure, aortic dissection, acute myocardial infarct and acute renal failure. (level of evidence: 5; recommendation grade: D)
18. Do not abruptly reduce blood pressure in acute stroke. For this reason, the use of nifedipine is contraindicated. (level of evidence: 4; recommendation grade: C)
19. Blood pressure must be kept above a mean arterial pressure of 90 mmHg. This must be done through the administration of isotonic fluids, as saline solution, and, when necessary, volume expanders and vasoactive drugs. Some drugs are used for this purpose, such as norepinephrine, dopamine and phenilephrine. Due to the absence of inotropic and chronotropic effect (β-adrenergic action), thereby reducing the risk of heart complications, phenilephrine may be a preferable option in patients with prior heart disease. (level of evidence: 5; recommendation grade: D)
20. Keep axillary temperature below 37.5ºC. If necessary, antipyretic medications should be used, as acetaminophen and dipyrone. (level of evidence 5, recommendation grade: D)
21. In cases of hyperthermia, investigate infectious causes. Fever of central origin should always be an exclusion diagnosis. (level of evidence 5; recommendation grade: D)
IMAGING IN ACUTE STROKE
Head CT without contrast is essential in the emergency assessment of patients with acute ischemic stroke. It identifies 90-95% of subarachnoid hemorrhages and almost 100% of intraparenchymal hemorrhages, and helps to rule out non-vascular causes of neurological symptoms86,87.
In patients with involvement of the middle cerebral artery (MCA), early signs of ischemia are present in approximately 60% of the cases with only two hours from symptom onset88, and in 82% of the cases within six hours89, and are associated with worse prognosis90. The presence of these signs affecting a large area of brain tissue is also associated with greater risk of hemorrhagic transformation after the use of thrombolytic medication, especially when the territory is larger than one-third of the MCA90. Specific training is needed to recognize these signs and define the true extent of the affected area in the CT91-94. The use of ASPECT score for the evaluation of early ischemic alterations objectively quantifies the affected territory, can improve detection of the affected area and provide information about prognosis, but is not validated to include or exclude patients from thrombolysis32,95. The only early sign used as an exclusion criterion for the treatment is hypodensity in more than one-third of MCA territory.
Although head CT has relatively low sensitivity in detecting small acute infarcts, especially in the posterior fossa, it is still the first-line test in most centers using thrombolytic treatment. Head CT for acute phase evaluation is sufficient, fast, available in most emergencies and may exclude the possibility of intracranial hemorrhage, possibly providing prognostic information (early signs)55,86. Since time is crucial, patients with acute stroke should be given priority over other patients for brain imaging. A CT scan performed immediately is the most cost-effective strategy for the imaging evaluation in patients with acute stroke96. In patients with indication for thrombolytic therapy, CT should be performed within 25 minutes after patient admission, and interpretation must be obtained in the next 20 minutes96.
Some centers prefer using cranial MRI, with diffusion-weighted imaging (DWI) technique, in the routine investigation of acute stroke. It has greater sensitivity to identify the ischemic region (as early as 35 minutes of symptom onset), and image acquisition takes only a few seconds97. However, not all MRI systems are capable of performing DWI. MRI is particularly useful in posterior circulation strokes, lacunar infarctions, small cortical infarcts and, above all, in unusual images when there are doubts as to the diagnosis of stroke. Gradient echo-sequences allow exclusion of hemorrhage with sensitivity and specificity of 100%98. Thrombolytic initiation must not be delayed to carry out MRI99,100.
The difference between the volume of DWI signal change (corresponds, in most cases, to the core of brain tissue already infarcted)101 and the perfusion image (brain tissue with critical hypoperfusion) is called mismatch (corresponds to the penumbra, volume of ischemic potentially reversible brain tissue)102. This feature may be used in thrombolysis decisions based on the persistency of ischemic penumbra in individuals beyond the approved therapeutic window103 or in cases of uncertain time of symptom onset, despite no evidence of a major response to thrombolysis up to nine hours104. Recently, dynamic perfusion imaging in CT has been used as an alternative to this method105,106.
Performing emergency angiography or magnetic resonance angiography of intra and extracranial vessels to detect occlusions or stenosis of large vessels in the acute phase of stroke may be used in centers that provide structure for intra-arterial recanalization treatment107,108.
Transcranial doppler (TCD) is useful for the diagnosis of occlusions of major brain arteries and may be used to monitor the effects of thrombolytic therapy in the acute phase, besides aiding in prognosis determination109-111. However, between 7 and 20% of patients with acute stroke do not have an adequate acoustic window112,113.
Recommendations
1. For patients with acute stroke, an urgent nonconstrast head CT is recommended (level of evidence: 1A, recommendation grade: A) or, alternatively, cranial MRI with the inclusion of diffusion and gradient echo sequences. (level of evidence: 1B, recommendation grade: A)
2. Brain imaging must be interpreted by a physician with cranial CT or MRI evaluation training. (level of evidence: 5, recommendation grade: D)
3. The use of multimodal neuroimaging can be useful for patient selection for thrombolytic therapy in patients with onset of symptoms with an indefinite duration or beyond 4 hours and 30 minutes. (level of evidence: 3, recommendation grade: C).
LABORATORIAL INVESTIGATION
Inflammation markers in stroke
All phases of atherothrombosis are characterized by a vascular inflammatory process. However, there are no specific studies proving the validity of these markers in acute stroke. The predictive value of complications (progression of thrombosis, new arterio-arterial emboli) or of indication of any intervention in the acute phase based in biomarkers is still not well-established114. While systematic reviews of the role of blood biomarkers in the diagnosis of ischemic stroke show that we still cannot recommend these tests in clinical practice, it is highly desirable that new studies be performed so that a faster diagnosis of ischemic stroke may be possible, even before reaching the hospital, through biological markers of cerebral ischemia or inflammation115.
Chest x-ray
Performed routinely even without evidence of cardiac or pulmonary disease, chest x-rays have been subject of various studies, showing that it may change management in 3.8% of the cases. Although it is a small percentage, it is not negligible116.
Glucose
In relation to glucose levels, importance resides in defining if the clinical situation is a stroke or hypoglycemia, which can mimic it. Hyperglycemic values are also important, as they can indicate unfavorable prognosis.
Exams in the subacute phase to define etiology and act upon risk factors
Stroke patients are at increased risk of recurrence, and our action is needed to reduce this risk with secondary prevention measures. With this objective, we must recognize individual risk factors. In relation to the lipid profile, it is necessary to mention studies from Amarenco, which showed reduction of stroke risk, resulting from a 50% or more decrease of LDL-C levels. In this context, there was a 31% reduction in stroke risk, 33% reduction of ischemic stroke, with no statistically significant increase in hemorrhage stroke incidence, as well as 37% decrease in major coronary events117.
Laboratory exams in emergency must be quickly available and cannot be the reason to delay the use of thrombolitics (expert consensus).
Thus, it is well established the requirement, on admission, of exams, such as complete blood count, blood glucose and glycozilated hemoglobin (in cases of hyperglycemia), creatinine, urea, electrolytes, arterial blood gas analysis and coagulation, as well as electrocardiogram and cardiac enzymes, due to the common comorbidity of acute myocardial infarction. (level of evidence: 5; recommendation grade: D)
Exams to be requested in the sub-acute phase: lipid profile, serology for Chagas' disease and syphilis, and, in young patients, in addition to the ones already mentioned, evaluation of autoimmune diseases, arteritis, homocysteine levels, AVM research, coagulopathy and genetic profile for thrombophylia. (level of evidence: 5, recommendation grade: D)
Examination of CSF is only recommended when there is strong evidence of subarachnoid hemorrhage with no blood evident on CT or when clinical investigation suggests infection as the cause of the deficit.
EEG is indicated when seizure is the possible cause for the deficit or when it is a complication of the stroke. It may be a differential diagnosis of stroke and may change treatment indication118.
There is indication of ECG, transthoracic echocardiography, Holter monitoring and cardiac enzymes for cases of cardiac arrhythmias with suspected embolic stroke, either by atrial fibrillation, acute myocardial infarction with ventricular dysfunction, valvular failure or in dilated heart disease, such as in Chagas' disease119.
In young patients, the execution of transesophageal echocardiography is preferable due to the incidence of patent foramen ovale. Other exams will be performed as diagnostic hypotheses are raised and according to the necessity to evaluate treatment, as toxicologic exams, pregnancy tests and HIV serology.
In summary, laboratory exams will be divided in two phases of activity:
In the emergency, for the diagnosis of stroke, for diagnosis of stroke type and for decision to apply treatment.
At the hospital, to establish nosological diagnosis and apply secondary prevention measures.
Received 18 February 2012
Received in final form 22 February 2012
Accepted 29 February 2012
Conflict of interest: There is no conflict of interest to declare.
Executive Committee: Charles André, Aroldo Luiz Bacellar, Daniel da Cruz Bezerra, Roberto Campos, João José Freitas de Carvalho, Gabriel Rodrigues de Freitas, Roberto de Magalhães Carneiro de Oliveira, Sebastião Eurico Melo de Souza, Soraia Ramos Cabette Fábio, Eli Faria Evaristo, Jefferson Gomes Fernandes, Maurício Friedrich, Marcia Maiumi Fukujima, Rubens José Gagliardi, Sérgio Roberto Haussen, Maria Clinete Sampaio Lacativa, Bernardo Liberato, Alexandre L. Longo, Sheila Cristina Ouriques Martins, Ayrton Roberto Massaro, Cesar Minelli, Carla Heloísa Cabral Moro, Jorge El-Kadum Noujaim, Edison Matos Nóvak, Jamary Oliveira-Filho, Octávio Marques Pontes-Neto, César Noronha Raffin, Bruno Castelo Branco Rodrigues, José Ibiapina Siqueira-Neto, Elza Dias Tosta, Raul Valiente, Leonardo Vedolim, Marcelo Gabriel Veja, Leonardo Vedolin, Fábio Iuji Yamamoto, Viviane Flumignan Zétola.
- 1. Pontes-Neto OM, Oliveira-Filho J, Valiente R, et al. [Brazilian guidelines for the manegement of intracerebral hemorrhage]. Arq Neuropsiquiatr 2009;67:940-950.
-
2The WHO stepwise approach to stroke surveillance. Overview and Manual (version2.0). Noncommunicable Diseases and Mental Health. World Health Organization. [Internet] [accessed 2005 Nov 01]. Available from: www.who.int/entity/ncd_surveillance/steps/en
- 3. Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA 2004;291:2616-2622.
- 4. Organização Pan Americana da Saúde. Rede interagencial de informações para a Saúde. [Internet] [accessed 2007]. Available from: http://www.opas.org.br/ripsa/produto_final_det.cfm?id=9
- 5. Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol 2007;6:182-187.
- 6. Saposnik G, Del Brutto OH. Stroke in South America: a systematic review of incidence, prevalence, and stroke subtypes. Stroke 2003;34:2103-2107.
- 7. Lessa I, Bastos CA. Epidemiology of cerebrovascular accidents in the city of Salvador, Bahia, Brazil. Bull Pan Am Health Organ 1983;17:292-303.
- 8. Cabral NL, Longo AL, Moro CH, Amaral CH, Kiss HC. [Epidemiology of cerebrovascular disease in Joinville, Brazil. An institutional study]. Arq Neuropsiquiatr 1997;55:357-363.
- 9. Minelli C, Fen LF, Minelli DP. Stroke incidence, prognosis, 30-day, and 1-year case fatality rates in Matao, Brazil: a population-based prospective study. Stroke 2007;38:2906-2911.
- 10. Andre C, Curioni CC, Braga da Cunha C, Veras R. Progressive decline in stroke mortality in Brazil from 1980 to 1982, 1990 to 1992, and 2000 to 2002. Stroke 2006;37:2784-2789.
- 11. Souza MFM, Alencar AP, Malta DC, Moura L, Mansur AP. Análise de séries temporais da mortalidade por doenças isquêmicas do coração e cerebrovasculares, nas cinco regiões do Brasil, no período de 1981 a 2001. Arq Bras Cardiol 2006;87:735-740.
- 12. Pontes-Neto OM, Silva GS, Feitosa MR, et al. Stroke awareness in Brazil: alarming results in a community-based study. Stroke 2008;39:292-296.
- 13. Wein TH, Staub L, Felberg R, et al. Activation of emergency medical services for acute stroke in a nonurban population: the T.L.L. Temple Foundation Stroke Project. Stroke 2000;31:1925-1928.
- 14. Luiz T, Moosmann A, Koch C, Behrens S, Daffertshofer M, Ellinger K. [Optimized logistics in the prehospital management of acute stroke]. Anasthesiol Intensivmed Notfallmed Schmerzther 2001;36:735-741.
- 15. Schmidt NK, Huwel J, Weisner B. [Causes of a prolonged prehospital phase in patients admitted to a stroke unit. Can it be influenced by campaigns to educate the public?]. Nervenarzt 2005;76:181-185.
- 16. Alberts MJ, Perry A, Dawson DV, Bertels C. Effects of public and professional education on reducing the delay in presentation and referral of stroke patients. Stroke 1992;23:352-356.
- 17. Barsan WG, Brott TG, Broderick JP, Haley EC Jr., Levy DE, Marler JR. Urgent therapy for acute stroke. Effects of a stroke trial on untreated patients. Stroke 1994;25:2132-2137.
- 18. Hodgson C, Lindsay P, Rubini F. Can mass media influence emergency department visits for stroke? Stroke 2007;38:2115-2122.
- 19. Morgenstern LB, Staub L, Chan W, et al. Improving delivery of acute stroke therapy: The TLL Temple Foundation Stroke Project. Stroke 2002;33:160-166.
- 20. Morgenstern LB, Bartholomew LK, Grotta JC, Staub L, King M, Chan W. Sustained benefit of a community and professional intervention to increase acute stroke therapy. Arch Intern Med 2003;163:2198-2202.
- 21. Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, Persse D, Grotta JC. Houston paramedic and emergency stroke treatment and outcomes study (HoPSTO). Stroke 2005;36:1512-1518.
- 22. Barsan WG, Brott TG, Broderick JP, Haley EC, Levy DE, Marler JR. Time of hospital presentation in patients with acute stroke. Arch Intern Med 1993;153:2558-2561.
- 23. Mosley I, Nicol M, Donnan G, Patrick I, Dewey H. Stroke symptoms and the decision to call for an ambulance. Stroke 2007;38:361-363.
- 24. Chiti A, Fanucchi S, Sonnoli C, Barni S, Orlandi G. Stroke symptoms and the decision to call for an ambulance: turn on people's minds! Stroke 2007;38:58-59.
- 25. Rosamond WD, Evenson KR, Schroeder EB, Morris DL, Johnson AM, Brice JH. Calling emergency medical services for acute stroke: a study of 9-1-1 tapes. Prehosp Emerg Care 2005;9:19-23.
- 26. Novak EM, Zetola Vde H, Muzzio JA, Puppi M, Carraro Junior H, Werneck LC. [Lay knowledge about stroke]. Arq Neuropsiquiatr 2003;61:772-776.
- 27. Schroeder EB, Rosamond WD, Morris DL, Evenson KR, Hinn AR. Determinants of use of emergency medical services in a population with stroke symptoms: the Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke 2000;31:2591-2596.
- 28. Morris DL, Rosamond WD, Hinn AR, Gorton RA. Time delays in accessing stroke care in the emergency department. Acad Emerg Med 1999;6:218-223.
- 29. Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and emergency department delays after acute stroke: the Genentech Stroke Presentation Survey. Stroke 2000;31:2585-2590.
- 30. Lacy CR, Suh DC, Bueno M, Kostis JB. Delay in presentation and evaluation for acute stroke: Stroke Time Registry for Outcomes Knowledge and Epidemiology (S.T.R.O.K.E.). Stroke 2001;32:63-69
- 31. Rossnagel K, Jungehülsing GJ, Nolte CH, et al. Out-of-hospital delays in patients with acute stroke. Ann Emerg Med 2004;44:476-483.
- 32. Adams HP Jr, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke 2007;38:1655-1711.
- 33. Kothari R, Barsan W, Brott T, Broderick J, Ashbrock S. Frequency and accuracy of prehospital diagnosis of acute stroke. Stroke 1995;26:937-941.
- 34. Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati Prehospital Stroke Scale: reproducibility and validity. Ann Emerg Med 1999;33:373-378.
- 35. Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke 2000;31:71-76.
- 36. Silver FL, Rubini F, Black D, Hodgson CS. Advertising strategies to increase public knowledge of the warning signs of stroke. Stroke 2003;34:1965-1968.
- 37. Handschu R, Poppe R, Rauss J, Neundorfer B, Erbguth F. Emergency calls in acute stroke. Stroke 2003;34:1005-1009.
- 38. Suyama J, Crocco T. Prehospital care of the stroke patient. Emerg Med Clin North Am 2002;20:537-552.
- 39. Ronning OM, Guldvog B. Should stroke victims routinely receive supplemental oxygen? A quasi-randomized controlled trial. Stroke 1999;30:2033-2037.
- 40. Bruno A, Biller J, Adams HP Jr, et al. Acute blood glucose level and outcome from ischemic stroke. Trial of ORG 10172 in Acute Stroke Treatment (TOAST) Investigators. Neurology 1999;52:280-284.
- 41. Farrokhnia N, Björk E, Lindbäck J, Terent A. Blood glucose in acute stroke, different therapeutic targets for diabetic and non-diabetic patients? Acta Neurol Scand 2005;112:81-87.
- 42. Godoy DA, Pinero GR, Svampa S, Papa F, Di Napoli M. Hyperglycemia and short-term outcome in patients with spontaneous intracerebral hemorrhage. Neurocrit Care 2008;9:217-229.
- 43. Bethesda. National Institute of Neurological Disorders and Stroke. Rapid identification and treatment of acute stroke. Proceedings of a national symposium. National Institutes of Health Monograph 1997.
- 44. Douglas VC, Tong DC, Gillum LA, et al. Do the Brain attack coalition's criteria for stroke centers improve care for ischemic stroke? Neurology 2005;64:422-427.
- 45. Tilley BC, Lyden PD, Brott TG, Lu M, Levine SR, Welch KM. Total quality improvement method for reduction of delays between emergency department admission and treatment of acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Arch Neurol 1997;54:1466-1474.
- 46. LaBresh KA, Reeves MJ, Frankel MR, Albright D, Schwamm LH. Hospital treatment of patients with ischemic stroke or transient ischemic attack using the "Get With The Guidelines" program. Arch Intern Med 2008;168:411-417.
- 47. Newell SD Jr, Englert J, Box-Taylor A, Davis KM, Koch KE. Clinical efficiency tools improve stroke management in a rural southern health system. Stroke 1998;29:1092-1098.
- 48. Wentworth DA, Atkinson RP. Implementation of an acute stroke program decreases hospitalization costs and length of stay. Stroke 1996;27:1040-1043.
- 49. Bowen J, Yaste C. Effect of a stroke protocol on hospital costs of stroke patients. Neurology 1994;44:1961-1964.
- 50. Jorgensen HS, Nakayama H, Raaschou HO, Larsen K, Hubbe P, Olsen TS. The effect of a stroke unit: reductions in mortality, discharge rate to nursing home, length of hospital stay, and cost. A community-based study. Stroke 1995;26:1178-1182.
- 51. Mitchell JB, Ballard DJ, Whisnant JP, Ammering CJ, Samsa GP, Matchar DB. What role do neurologists play in determining the costs and outcomes of stroke patients? Stroke 1996;27:1937-1943.
- 52. Goldstein LB, Matchar DB, Hoff-Lindquist J, Samsa GP, Horner RD. VA Stroke Study: neurologist care is associated with increased testing but improved outcomes. Neurology 2003;61:792-796.
- 53. Hand PJ, Kwan J, Lindley RI, Dennis MS, Wardlaw JM. Distinguishing between stroke and mimic at the bedside: the brain attack study. Stroke 2006;37:769-775.
- 54. Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581-1587.
- 55. Kidwell CS, Chalela JA, Saver JL, et al. Comparison of MRI and CT for detection of acute intracerebral hemorrhage. JAMA 2004;292:1823-1830.
- 56. Bamford J, Dennis M, Sandercock P, Burn J, Warlow C. The frequency, causes and timing of death within 30 days of a first stroke: the Oxfordshire Community Stroke Project. J Neurol Neurosurg Psychiatry 1990;53:824-829.
- 57. Broderick JP, Phillips SJ, O'Fallon WM, Frye RL, Whisnant JP. Relationship of cardiac disease to stroke occurrence, recurrence, and mortality. Stroke 1992;23:1250-1256.
- 58. Korpelainen JT, Sotaniemi KA, Huikuri HV, Myllya VV. Abnormal heart rate variability as a manifestation of autonomic dysfunction in hemispheric brain infarction. Stroke 1996;27:2059-2063.
- 59. Lane RD, Wallace JD, Petrosky PP, Schwartz GE, Gradman AH. Supraventricular tachycardia in patients with right hemisphere strokes. Stroke 1992;23:362-366.
- 60. Christensen H, Fogh Christensen A, Boysen G. Abnormalities on ECG and telemetry predict stroke outcome at 3 months. J Neurol Sci 2005;234:99-103.
- 61. Fure B, Bruun Wyller T, Thommessen B. Electrocardiographic and troponin T changes in acute ischaemic stroke. J Intern Med 2006;259:592-597.
- 62. Tatschl C, Stöllberger C, Matz K, et al. Insular involvement is associated with QT prolongation: ECG abnormalities in patients with acute stroke. Cerebrovasc Dis 2006;21:47-53.
- 63. Grotta J, Pasteur W, Khwaja G, Hamel T, Fisher M, Ramirez A. Elective intubation for neurologic deterioration after stroke. Neurology 1995;45:640-4.
- 64. Bushnell CD, Phillips-Bute BG, Laskowitz DT, Lynch JR, Chilukuri V, Borel CO. Survival and outcome after endotracheal intubation for acute stroke. Neurology 1999;52:1374-1381.
- 65. Ronning OM, Guldvog B. Stroke unit versus general medical wards, II: neurological deficits and activities of daily living: a quasi-randomized controlled trial. Stroke 1998;29:586-590.
- 66. Bhalla A, Sankaralingam S, Dundas R, Swaminathan R, Wolfe CD, Rudd AG. Influence of raised plasma osmolality on clinical outcome after acute stroke. Stroke 2000;31:2043-2048.
- 67. Bhalla A, Sankaralingam S, Tilling K, Swaminathan R, Wolfe C, Rudd A. Effect of acute glycaemic index on clinical outcome after acute stroke. Cerebrovasc Dis 2002;13:95-101.
- 68. Baird TA, Parsons MW, Phanh T, et al. Persistent poststroke hyperglycemia is independently associated with infarct expansion and worse clinical outcome. Stroke 2003;34:2208-2214.
- 69. Van den Berghe G, Schoonheydt K, Becx P, Bruyninckx F, Wouters PJ. Insulin therapy protects the central and peripheral nervous system of intensive care patients. Neurology 2005;64:1348-1353.
- 70. Gray CS, Hildreth AJ, Sandercock PA, et al. Glucose-potassium-insulin infusions in the management of post-stroke hyperglycaemia: the UK Glucose Insulin in Stroke Trial (GIST-UK). Lancet Neurol 2007;6:397-406.
- 71. Bruno A, Kent TA, Coull BM, et al. Treatment of hyperglycemia in ischemic stroke (THIS): a randomized pilot trial. Stroke 2008;39:384-389.
- 72. Fuentes B, Diez-Tejedor E. General care in stroke: relevance of glycemia and blood pressure levels. Cerebrovasc Dis 2007;24:S134-S142.
- 73. Alvarez-Sabin J, Molina CA, Montaner J, et al. Effects of admission hyperglycemia on stroke outcome in reperfused tissue plasminogen activator--treated patients. Stroke 2003;34:1235-1241.
- 74. Parsons MW, Barber PA, Desmond PM, et al. Acute hyperglycemia adversely affects stroke outcome: a magnetic resonance imaging and spectroscopy study. Ann Neurol 2002;52:20-28.
- 75. Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein HC. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke 2001;32:2426-2432.
- 76. Sprigg N, Gray LJ, Bath PM, et al. Relationship between outcome and baseline blood pressure and other haemodynamic measures in acute ischaemic stroke: data from the TAIST trial. J Hypertens 2006;24:1413-1417.
- 77. Oliveira-Filho J, Silva SC, Trabuco CC, Pedreira BB, Sousa EU, Bacellar A. Detrimental effect of blood pressure reduction in the first 24 hours of acute stroke onset. Neurology 2003;61:1047-1051.
- 78. Castillo J, Leira R, Garcia MM, Serena J, Blanco M, Davalos A. Blood pressure decrease during the acute phase of ischemic stroke is associated with brain injury and poor stroke outcome. Stroke 2004;35:520-526.
- 79. Aslanyan S, Fazekas F, Weir CJ, Horner S, Lees KR. Effect of blood pressure during the acute period of ischemic stroke on stroke outcome: a tertiary analysis of the GAIN International Trial. Stroke 2003;34:2420-2425.
- 80. Potter JF RT, Ford GA, Mistri A, et al. Controlling hypertension and hypotension immediately post-stroke (CHHIPS): a randomised, placebo-controlled, double-blind pilot trial. Lancet Neurol 2009;8:48-56.
- 81. Leonardi-Bee J, Bath PM, Phillips SJ, Sandercock PA. Blood pressure and clinical outcomes in the International Stroke Trial. Stroke 2002;33:1315-1320.
- 82. Hajat C, Hajat S, Sharma P. Effects of poststroke pyrexia on stroke outcome: a meta-analysis of studies in patients. Stroke 2000;31:410-414.
- 83. Azzimondi G, Bassein L, Nonino F, et al. Fever in acute stroke worsens prognosis. A prospective study. Stroke 1995;26:2040-2043.
- 84. Reith J, Jorgensen HS, Pedersen PM, et al. Body temperature in acute stroke: relation to stroke severity, infarct size, mortality, and outcome. Lancet 1996;347:422-425.
- 85. Boysen G, Christensen H. Stroke severity determines body temperature in acute stroke. Stroke 2001;32:413-417.
- 86. Jacobs L, Kinkel WR, Heffner RR Jr. Autopsy correlations of computerized tomography: experience with 6,000 CT scans. Neurology 1976;26:1111-1118.
- 87. Wardlaw JM, Keir SL, Dennis MS. The impact of delays in computed tomography of the brain on the accuracy of diagnosis and subsequent management in patients with minor stroke. J Neurol Neurosurg Psychiatry 2003;74:77-81.
- 88. Saur D, Kucinski T, Grzyska U, et al. Sensitivity and interrater agreement of CT and diffusion-weighted MR imaging in hyperacute stroke. AJNR Am J Neuroradiol 2003;24:878-885.
- 89. von Kummer R, Nolte PN, Schnittger H, Thron A, Ringelstein EB. Detectability of cerebral hemisphere ischaemic infarcts by CT within 6 h of stroke. Neuroradiology 1996;38:31-33.
- 90. Hacke W, Kaste M, Fieschi C, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA 1995;274:1017-1025.
- 91. Wardlaw JM, Dorman PJ, Lewis SC, Sandercock PA. Can stroke physicians and neuroradiologists identify signs of early cerebral infarction on CT? J Neurol Neurosurg Psychiatry 1999;67:651-653.
- 92. Schriger DL, Kalafut M, Starkman S, Krueger M, Saver JL. Cranial computed tomography interpretation in acute stroke: physician accuracy in determining eligibility for thrombolytic therapy. JAMA 1998;279:1293-1297.
- 93. Grotta JC, Chiu D, Lu M, et al. Agreement and variability in the interpretation of early CT changes in stroke patients qualifying for intravenous rtPA therapy. Stroke 1999;30:1528-1533.
- 94. Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet 2000;355:1670-1674.
- 95. Demchuk AM, Hill MD, Barber PA, Silver B, Patel SC, Levine SR. Importance of early ischemic computed tomography changes using ASPECTS in NINDS rtPA Stroke Study. Stroke 2005;36:2110-2115.
- 96. Wardlaw JM, Keir SL, Seymour J, et al. What is the best imaging strategy for acute stroke? Health Technol Assess 2004;8:1-180.
- 97. Chalela JA, Kidwell CS, Nentwich LM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet 2007;369:293-298.
- 98. Fiebach JB, Schellinger PD, Gass A, et al. Stroke magnetic resonance imaging is accurate in hyperacute intracerebral hemorrhage: a multicenter study on the validity of stroke imaging. Stroke 2004;35:502-506.
- 99. Kang DW, Chalela JA, Dunn W, Warach S. MRI screening before standard tissue plasminogen activator therapy is feasible and safe. Stroke 2005;36:1939-1943.
- 100. Zivin JA. Perfusion-weighted imaging/diffusion-weighted imaging mismatch on MRI can now be used to select patients for recombinant tissue plasminogen activator beyond 3 hours: con. Stroke 2005;36:1105-1106.
- 101. Albers GW. Diffusion-weighted MRI for evaluation of acute stroke. Neurology 1998;51:S47-S49.
- 102. Coutts SB, Simon JE, Tomanek AI, et al. Reliability of assessing percentage of diffusion-perfusion mismatch. Stroke 2003;34:1681-1683.
- 103. Albers GW, Thijs VN, Wechsler L, et al. Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann Neurol 2006;60:508-517.
- 104. Hacke W, Albers G, Al-Rawi Y, et al. The Desmoteplase in Acute Ischemic Stroke Trial (DIAS): a phase II MRI-based 9-hour window acute stroke thrombolysis trial with intravenous desmoteplase. Stroke 2005;36:66-73.
- 105. Schramm P, Schellinger PD, Klotz E, et al. Comparison of perfusion computed tomography and computed tomography angiography source images with perfusion-weighted imaging and diffusion-weighted imaging in patients with acute stroke of less than 6 hours' duration. Stroke 2004;35:1652-1658.
- 106. Mayer TE, Hamann GF, Baranczyk J, et al. Dynamic CT perfusion imaging of acute stroke. AJNR Am J Neuroradiol 2000;21:14411-1449.
- 107. Lev MH, Farkas J, Rodriguez VR, et al. CT angiography in the rapid triage of patients with hyperacute stroke to intraarterial thrombolysis: accuracy in the detection of large vessel thrombus. J Comput Assist Tomogr 2001;25:520-528.
- 108. Qureshi AI, Isa A, Cinnamon J, et al. Magnetic resonance angiography in patients with brain infarction. J Neuroimaging 1998;8:65-70.
- 109. Christou I, Alexandrov AV, Burgin WS, et al. Timing of recanalization after tissue plasminogen activator therapy determined by transcranial doppler correlates with clinical recovery from ischemic stroke. Stroke 2000;31:1812-1816.
- 110. Demchuk AM, Burgin WS, Christou I, et al. Thrombolysis in brain ischemia (TIBI) transcranial Doppler flow grades predict clinical severity, early recovery, and mortality in patients treated with intravenous tissue plasminogen activator. Stroke 2001;32:89-93.
- 111. Alexandrov AV, Wojner AW, Grotta JC. CLOTBUST: design of a randomized trial of ultrasound-enhanced thrombolysis for acute ischemic stroke. J Neuroimaging 2004;14:108-112.
- 112. Postert T, Federlein J, Przuntek H, Buttner T. Insufficient and absent acoustic temporal bone window: potential and limitations of transcranial contrast-enhanced color-coded sonography and contrast-enhanced power-based sonography. Ultrasound Med Biol 1997;23:857-862.
- 113. Alexandrov AV, Burgin WS, Demchuk AM, El-Mitwalli A, Grotta JC. Speed of intracranial clot lysis with intravenous tissue plasminogen activator therapy: sonographic classification and short-term improvement. Circulation 2001;103:2897-2902.
- 114. Muir KW, Tyrrell P, Sattar N, Warburton E. Inflammation and ischaemic stroke. Curr Opin Neurol 2007;20:334-342.
- 115. Rubens José Gagliardi CA, Marcia Maiumi Fukujima, Sebastião Eurico Melo-Souza VFZ. Abordagem da doença carotídea na fase aguda do Acidente Vascular Cerebral - Opinião Nacional. Arq Neuropsiquiatr 2005;63:709-712.
- 116. Sagar G, Riley P, Vohrah A. Is admission chest radiography of any clinical value in acute stroke patients? Clin Radiol 1996;51:499-502.
- 117. Amarenco P, Goldstein LB, Szarek M, et al. Effects of intense low-density lipoprotein cholesterol reduction in patients with stroke or transient ischemic attack: the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial. Stroke 2007;38:3198-3204.
- 118. Bladin CF, Alexandrov AV, Bellavance A, et al. Seizures after stroke: a prospective multicenter study. Arch Neurol 2000;57:1617-1622.
- 119. Liao J, Khalid Z, Scallan C, Morillo C, O'Donnell M. Noninvasive cardiac monitoring for detecting paroxysmal atrial fibrillation or flutter after acute ischemic stroke: a systematic review. Stroke 2007;38:2935-2940.
Correspondence:
Publication Dates
-
Publication in this collection
14 Aug 2012 -
Date of issue
Aug 2012