Abstracts
OBJECTIVE:
to compare the motor coordination, cognitive, and functional development of preterm and term children at the age of 4 years.
METHODS:
this was a cross-sectional study of 124 four-year-old children, distributed in two different groups, according to gestational age and birth weight, paired by gender, age, and socioeconomic level. All children were evaluated by the Movement Assessment Battery for Children - second edition (MABC-2), the Pediatric Evaluation of Disability Inventory (PEDI), and the Columbia Mental Maturity Scale (CMMS).
RESULTS:
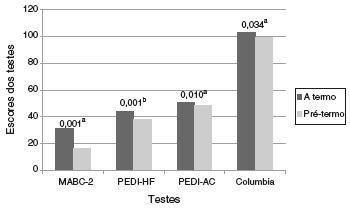
preterm children had worse performance in all tests, and 29.1% of the preterm and 6.5% of term groups had scores on the MABC-2 indicative of motor coordination disorder (p = 0.002). In the CMMS (p = 0.034), the median of the standardized score for the preterm group was 99.0 (± 13.75) and 103.0 (± 12.25) for the term group; on the PEDI, preterm children showed more limited skill repertoire (p = 0.001) and required more assistance from the caregiver (p = 0.010) than term children.
CONCLUSION:
this study reinforced the evidence that preterm children from different socioeconomic backgrounds are more likely to have motor, cognitive, and functional development impairment, detectable before school age, than their term peers.
Prematurity; Child development; Motor coordination; Cognition; Functional performance; Socioeconomic level
OBJETIVO:
comparar o desenvolvimento da coordenação motora, o desenvolvimento cognitivo e o desempenho funcional de crianças nascidas pré-termo e a termo, aos quatro anos de idade.
MÉTODOS:
estudo transversal com 124 crianças de quatro anos de idade, distribuídas em dois grupos distintos, de acordo com a idade gestacional e peso ao nascimento, pareadas com relação ao sexo, idade e nível socioeconômico. Todas as crianças foram avaliadas pelos testes Movement Assessment Battery for Children - Second Edition (MABC-2), Inventário de Avaliação Pediátrica de Incapacidade (PEDI) e Escala de Maturidade Mental Colúmbia (EMMC).
RESULTADOS:
as crianças pré-termo tiveram pior desempenho em todos os testes, sendo que 29,1% das crianças do grupo pré-termo e 6,5% do grupo a termo apresentaram pontuação no MABC-2 indicativa de sinais de transtorno da coordenação motora (p = 0,002). No Columbia (p = 0,034), a mediana do resultado padronizado para o grupo pré-termo foi de 99,0 (±13,75), e do grupo a termo foi 103,0 (±12,25); no PEDI, crianças pré-termo tiveram menor repertório de habilidades (p = 0,001) e necessitaram de maior assistência do cuidador (p = 0,010) do que as crianças a termo.
CONCLUSÃO:
este estudo reforça as evidências de que crianças pré-termo, de diferentes níveis socioeconômicos, são mais propensas a apresentarem alterações no desenvolvimento motor, cognitivo e funcional, detectáveis antes da idade escolar, que seus pares nascidos a termo.
Prematuridade; Desenvolvimento infantil; Coordenacão motora; Cognicão; Desempenho funcional; Nível socioeconômico
Introduction
The increased rates of preterm births in Brazil in recent years11. Silveira MF, Santos IS, Matijasevich A, Malta DC, Duarte EC. Nascidos pré-termo no Brasil entre 1994 e 2005 conforme o Sistema de Informações sobre Nascidos Vivos (SINASC). Cad Saude Publica. 2009;25:1267-75. has made it important to predict the outcome of these children, not only due to the increased mortality risk, but also because gestational age and birth weight are important indicators of biological risk for developmental delay.11. Silveira MF, Santos IS, Matijasevich A, Malta DC, Duarte EC. Nascidos pré-termo no Brasil entre 1994 e 2005 conforme o Sistema de Informações sobre Nascidos Vivos (SINASC). Cad Saude Publica. 2009;25:1267-75. , 22. Vieira ME, Linhares MB. Developmental outcomes and quality of life in children born preterm at preschooland schoolage. J Pediatr (Rio J). 2011;87:281-91. , 33. Goyen TA, Lui K. Developmental coordination disorder in ''apparently normal'' schoolchildren born extremely preterm. Arch Dis Chil. 2009;94:298-302. , 44. Martins IMB, Linhares MB, Martinez FE. Indicadores de desenvolvimento na fase pré-escolar de crianças nascidas pré-termo. Psicol Estud. 2005;10:235-43. and 55. Aylward GP. Cognitive and neuropsychological outcomes: more than IQ scores. Ment Retard Dev Disabil. 2002;8:234-40. Longitudinal studies have demonstrated that approximately 15% of preterm infants with very low birth weight are at risk for severe neurodevelopmental dysfunctions55. Aylward GP. Cognitive and neuropsychological outcomes: more than IQ scores. Ment Retard Dev Disabil. 2002;8:234-40. , 66. Cooke RW. Perinatal and postnatal factors in very preterm infants and subsequent cognitive and motor abilities. Arch Dis Child Fetal Neonatal. 2005;90:F60-3. , 77. Roberts G, Anderson PJ, Davis N, Luca C, Cheong J, Doyle LW, The Victorian Infant Collaborative Study Group. Developmental coordination disorder in geographic cohorts of 8-year-old children born extremely preterm or extremely low birthweight in the 1990s. Dev Med Child Neurol. 2011;53:55-60. , 88. Davis NM, Ford GW, Anderson PJ, Doyle LW. Developmental coordination disorder at 8 years of age in a regional cohort of extremely-low-birth weight or very preterm infants. Dev Med Child Neurol. 2007;49:325-30. and 99. Foulder-Hughes LA, Cooke RW. Motor, cognitive, and behavioural disorders in children born very preterm. Dev Med Child Neurol. 2003;45:97-103. and, in the absence of major disorders, 30% to 50% of them have subtle motor, cognitive, and behavioral difficulties,55. Aylward GP. Cognitive and neuropsychological outcomes: more than IQ scores. Ment Retard Dev Disabil. 2002;8:234-40. , 66. Cooke RW. Perinatal and postnatal factors in very preterm infants and subsequent cognitive and motor abilities. Arch Dis Child Fetal Neonatal. 2005;90:F60-3. , 77. Roberts G, Anderson PJ, Davis N, Luca C, Cheong J, Doyle LW, The Victorian Infant Collaborative Study Group. Developmental coordination disorder in geographic cohorts of 8-year-old children born extremely preterm or extremely low birthweight in the 1990s. Dev Med Child Neurol. 2011;53:55-60. , 1010. Wocadlo C, Rieger I. Motor impairment and low achievement in very preterm children at eight years of age. Early Hum Dev. 2008;84:769-76. and 1111. Goyen TA, Lui K, Hummell J. Sensorimotor skills associated with motor dysfunction in children born extremely preterm. Early Hum Dev. 2011;87:489-93. which can be detected in preschoolers.66. Cooke RW. Perinatal and postnatal factors in very preterm infants and subsequent cognitive and motor abilities. Arch Dis Child Fetal Neonatal. 2005;90:F60-3. , 1212. Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80. , 1313. Kessel-Feddema B, Kleine M, Verhaak C. Concordance between school outcomes and developmental follow-up results of very preterm and/or low birth weight children at the age of 5 years. Eur J Pediatr. 2007;166:693-9. , 1414. Claas MJ, Vries LS, Bruinse HW, Haastert IC, Uniken Venema MM, Peelen LM, et al. Neurodevelopmental outcome over time of preterm born children < 750 g at birth. Early Hum Dev. 2011;87:183-91. and 1515. Rodrigues MC, Mello RR, Silva KS, Carvalho ML. Desenvolvimento cognitivo de prematuros à idade escolar: proposta de modelo hierarquizado para investigaçao dos fatores de risco. Cad Saude Publica. 2011;27:1154-64. Many of these children attend regular schools, but experience difficulties in learning and performing activities of daily living, and show poor academic performance.33. Goyen TA, Lui K. Developmental coordination disorder in ''apparently normal'' schoolchildren born extremely preterm. Arch Dis Chil. 2009;94:298-302. , 66. Cooke RW. Perinatal and postnatal factors in very preterm infants and subsequent cognitive and motor abilities. Arch Dis Child Fetal Neonatal. 2005;90:F60-3. , 88. Davis NM, Ford GW, Anderson PJ, Doyle LW. Developmental coordination disorder at 8 years of age in a regional cohort of extremely-low-birth weight or very preterm infants. Dev Med Child Neurol. 2007;49:325-30. , 1010. Wocadlo C, Rieger I. Motor impairment and low achievement in very preterm children at eight years of age. Early Hum Dev. 2008;84:769-76. , 1212. Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80. and 1313. Kessel-Feddema B, Kleine M, Verhaak C. Concordance between school outcomes and developmental follow-up results of very preterm and/or low birth weight children at the age of 5 years. Eur J Pediatr. 2007;166:693-9.
Although long-term developmental changes in preterm children are well described in the literature, the emergence of these difficulties at preschool age is less well documented. It is important to investigate the development at preschool age, considering that an assessment focused on motor coordination, cognitive development, and functional performance at early ages could identify preterm infants at risk for developmental disorders, enabling early intervention and allowing parents to be alerted regarding the potential difficulties their children might experience, prior to the start of elementary school.
The aim of this study was to compare the development of motor coordination, cognitive development, and functional performance in preterm and full-term children at 4 years of age. The hypothesis investigated was that at this age, considering the same social level, children born preterm who are apparently normal have significantly lower motor, cognitive, and functional performance than their full-term peers.
Methods
This cross-sectional, observational study was conducted from June of 2010 to August of 2011, with a convenience sample recruited from patients of the Follow up Clinic for Children at Risk Children (Ambulatório de Acompanhamento a Criança de Risco - ACRIAR), from two private practices as well as from four public and five private schools in Belo Horizonte, state of Minas Gerais.
The study included children aged from 4 years to 4 years and 11 months, divided into two distinct groups according to gestational age and birth weight, matched for gender, age, and socioeconomic status. For sample size calculation, analysis of variance (ANOVA) for two groups was used, assuming the same number of observations per group. For a significance level of 5% and 80% power, a minimum of 45 children per group was estimated, with a total of 90 children. The preterm group (PT) included 62 children with gestational age < 34 weeks and birth weight < 1,500 g, and the full-term group (FT) group included 62 children with gestational age > 37 weeks and birth weight > 2,500g. Each group had an equal number (31) of males and females. The PT group was recruited in the follow-up clinic, schools, and private practices, and the FT group was recruited from public and private schools.
Both groups consisted of apparently normal children with no evidence of diagnoses such as cerebral palsy, intellectual disability, genetic disorders, and malformations. In the PT group, three had grade III peri-intraventricular hemorrhage (PIVH), with no motor sequelae. Children in the FT group had no history of neonatal complications. Data related to the children's birth and neonatal complications were obtained from the discharge summary and the Child Health Handbook. Other information, such as education and profession of the parents, were provided by parents. Only children whose parents signed the informed consent authorizing their participation in the study were evaluated.
Data were collected to be representative of children of low socioeconomic level,
selected from the follow up clinic and public schools, and children of high
socioeconomic level, recruited from private practices and private schools. The economic
classification was estimated using the Economic Classification Criteria (ECC) proposed
by the Brazilian Association of Businesses and Research.1616. Associaçao Brasileira de Empresas de, Pesquisa, Adoçao do CCEB.
Critério de Classificaçao Econômica Brasil. 2010 [cited 10 Feb 2010]. Available from:
http://www.abep.org/novo/Content.aspx?SectionID=84.
http://www.abep.org/novo/Content.aspx?Se...
All children who participated in this study were evaluated through the Movement Assessment Battery for Children - second edition (MABC-2), the Pediatric Evaluation of Disability Inventory (PEDI), and the Columbia Mental Maturity Scale (CMMS) by the first author, who was previously trained in the application of each test. Since MABC-2 is a test of performance, inter-rater reliability was verified before data collection through the scoring of ten children evaluated jointly and scored independently, with the specific purpose of checking reliability, obtaining an index of 0.82 (intraclass correlation) for the total percentile of motor classification.
MABC-21717. Henderson SE, Sugden DA, Barmett AL. Movement assessment battery for children2 second edition (Movement ABC-2). London. UK: The Psychological Corporation. 2007. is a screening test used to identify motor impairment in children aged three to 16 years and 11 months, divided by age range; only the first age band, for children ages 3 years to 6 years and 11 months, was used this study. The test consists of eight tasks that assess manual dexterity, static and dynamic balance, and ball skills. According to this test's criteria, this study considered that children with scores < fifth percentile had motor coordination problems or atypical performance; scores from the sixth to the 15th percentile indicated suspected cases; and children with scores above the 16th percentile were considered as having normal motor performance. The MABC-2 does not have normative data for Brazilian children, but it has been used in research, including in the area of prematurity.1818. Oliveira GE, Magalhaes LC, Salmela LF. Relaçao entre muito baixo peso ao nascimento, fatores ambientais e o desenvolvimento motor e cognitivo de crianças aos 5 e 6 anos. Revs Bras Fisioter. 2011;15:138-45. and 1919. Souza C, Ferreira L, Catuzzo MT, Corrêa UC. O teste ABC do Movimento em crianças de ambientes diferentes. Rev Port Cien Desp. 2007;7:36-47. There is evidence of the validity of the MABC-2 in different countries,2020. Smits-Engelsman BCM, Henderson SE, Michels CGS. The assessment of children with developmental coordination disorders in the Netherlands: the relationship between the Movement Assessment Battery for Children and the Korperkoordinations Test für Kinder. Hum Mov Sci. 1998;17:699-709. and 2121. Ellinoudis T, Evaggelinou C, Kourtessis T, Konstantinidou Z, Venetsanou F, Kambas A. Reliability and validity of age band 1 of the Movement Assessment Battery for Children - Second Edition. Dev Disabilities. 2011;32:1046-51. and the present study compared data from two Brazilian samples.
The PEDI2222. Mancini MC. Inventário de Avaliaçao Pediátrica de Incapacidade (PEDI) - manual da versao brasileira adaptada. Belo Horizonte: Editora UFMG. 2005. is a questionnaire administered as a structured interview with parents or one of the child's caregivers, which reports on the functional profile of children between 6 months and 7 years and 6 months, in three levels of function: self-care, mobility, and social function. The functional profile documented by PEDI describes both the skills available in the child's repertoire to perform activities and tasks of daily living (Part 1), as well as the level of independence or the amount of help provided by the caregiver (Part 2), and the environmental modifications that are necessary for functional performance (Part 3). The self-care subscale of part 1 (functional skills [FS]) and part 2 (caregiver assistance [CA]) were used in this study. In Part 1, each item is evaluated as a score of 1 (if the child is able to perform the activity of daily living) or a score of 0 (if the child is not able to perform it).
The scores given to items are summed, resulting in a total gross score. In part 2, the amount of caregiver assistance is measured on an ordinal scale ranging from 0 (indicating need for total assistance) to 5 (the child is independent in the performance), with intermediate graduations. The score given for the tasks are added, resulting in a raw score of independence, which is converted into a standardized score, adjusted for the child's age. The PEDI has been translated and culturally adapted to Brazilian children.2222. Mancini MC. Inventário de Avaliaçao Pediátrica de Incapacidade (PEDI) - manual da versao brasileira adaptada. Belo Horizonte: Editora UFMG. 2005.
The CMMS2323. Alves ICB, Duarte JLM. Escala de Maturidade Mental Columbia - padronizaçao brasileira - manual para aplicaçao e interpretaçao. Casa do Psicólogo. 2001. test is applied individually, with a mean duration of 15 to 20 minutes, and provides an estimate of general reasoning capacity of children aged 3 years and 6 months to 9 years and 11 months. The 92 items are organized in a series of eight scales, and the children performs the segment corresponding to the most appropriate level for their chronological age. The raw score is obtained by the number of items correctly answered by the child, which can be converted into derived scores.
The Age Standardized Result (ASR) is a numeric index that indicate the children's status when their general reasoning capacity is compared to that of other children of the same age from the normative sample. The ASR can be converted to percentile, which is one of the most popular ways to interpret performance on standardized tests. A standardized version for Brazilian children was used in the present study.
Before each child's evaluation, parents were contacted by telephone or by letter sent by the school to inform them about the research, clarify the study objectives, and request their cooperation. The letter included a short questionnaire about their child's birth and place for signature, authorizing the child's participation in the study. This study was approved by the Research Ethics Committee of the Universidade Federal de Minas Gerais (UFMG).
The descriptive results were obtained through absolute and relative frequencies for categorical variables, whereas measures of central tendency and dispersion were used for quantitative variables. Quantitative variables were assessed for normal distribution using the Shapiro-Wilk's test. Student's t-test was used for variables that had normal distribution, while the nonparametric Mann-Whitney test was used for those that did not, when comparing the groups.
Exact and asymptotic chi-squared tests were used to assess the association between groups and categorical variables. The Kruskal-Wallis test was used to verify the association between level of motor performance and results in cognitive and functional tests. Regression analysis was used to investigate the impact of gestational age and birth weight on test scores. The significance level was set at 0.05 for all analyses.
Results
A total of 124 children, divided into two distinct groups, were evaluated. The sociodemographic and perinatal morbidity data are shown in Table 1. The quantitative variables that showed significant differences in the comparisons between groups were gestational age and birth weight.
Fig. 1 presents the results of motor, functional, and cognitive performance for the PT and T groups. Significant differences between groups were observed in all tests, with better performance for the children in the T group.
Performance at the MABC-2, PEDI and Columbia tests for the full-term and preterm groups.(a) Test Mann Whitney.(b) t-test.
Table 2 presents the motor performance classification according to the MABC-2 for the two groups; a higher frequency of motor coordination signs and problems was observed in the PT group. Preterm children with atypical motor performance (MABC-2 < 5%) had a worse outcome in the CMMS test (p = 0.003), but there was no significant difference regarding functional performance (PEDI-FS: p = 0.897; and PEDI-CA: p = 0.697). At the regression analysis, no significant association was found between gestational age or weight and scores in the motor, cognitive, and functional tests. Although some preterm children had PIVH, the Mann-Whitney test indicated a significant difference between children with and without hemorrhage only in the CMMS test (p = 0.021). No significant difference was observed in the performance on any of the tests between children with and without bronchopulmonary dysplasia.
Discussion
The results of the present study demonstrated that a significant proportion of apparently normal preterm children had worse motor, cognitive, and functional performance at preschool age than their peers born at full-term.
In the motor area, children from the PT group obtained significantly lower scores on the MABC-2 test. These results are consistent with national and international studies showing that preterm and very-low birth weight children aged 4 to 6 years had significantly greater motor impairment than children born full-term.1212. Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80. , 1313. Kessel-Feddema B, Kleine M, Verhaak C. Concordance between school outcomes and developmental follow-up results of very preterm and/or low birth weight children at the age of 5 years. Eur J Pediatr. 2007;166:693-9. , 1818. Oliveira GE, Magalhaes LC, Salmela LF. Relaçao entre muito baixo peso ao nascimento, fatores ambientais e o desenvolvimento motor e cognitivo de crianças aos 5 e 6 anos. Revs Bras Fisioter. 2011;15:138-45. , 2424. Goyen T, Lui K. Longitudinal motor development of ''apparently normal'' high-risk infants at 18 months, 3 and 5 years. Early Hum Dev. 2002;70:103-15. and 2525. Goyen TA, Lui K, Woods R. Visual-motor, visual-perceptual, and fine motor outcomes in very-low-birthweight children at 5 years. Dev Med Child Neurol. 1998;40:76-81.
In a study by Oliveira et al.1818. Oliveira GE, Magalhaes LC, Salmela LF. Relaçao entre muito baixo peso ao nascimento, fatores ambientais e o desenvolvimento motor e cognitivo de crianças aos 5 e 6 anos. Revs Bras Fisioter. 2011;15:138-45. to assess the association between low birth weight, prematurity, environmental factors, and cognitive and motor development of children aged 5 and 6 years old, it was observed that preterm children had significantly lower scores on the MABC-2 test, whose motor performance was below that expected for age. In addition to the difference between the groups, the results of our study showed that preterm children with poorer motor performance had worse outcome in the CMMS, which is also consistent with the literature.99. Foulder-Hughes LA, Cooke RW. Motor, cognitive, and behavioural disorders in children born very preterm. Dev Med Child Neurol. 2003;45:97-103. , 1212. Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80. and 2626. Marlow N, Hennessy EM, Bracewell MA, Wolke D. Motor and executive function at 6 years of age after extremely preterm birth. Pediatr. 2007;120:793-804. For instance, Howe et al.,1212. Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80. comparing the performance of preterm and full-term children at 5 years of age, found a higher rate of cognitive, visual-motor, and adaptive behavior problems in preterm children with motor difficulties.
Contrary to the evidence, no association was observed between birth weight and gestational age and motor, cognitive, and functional development in the preterm group. One possible explanation for this result is the influence of socioeconomic factors. Considering that the sample included different socioeconomic levels, it was observed that preterm children with lower gestational age were those of higher socioeconomic status, which have access to better-quality neonatal care. These children's development also occur in more stimulating environments, which may have influenced test performance.
In the MABC-2 classification (Table 2), the prevalence of signs of coordination disorders was 29.1% among children in the PT group, and was significantly higher than the 6.5% in the FT group, using the fifth-percentile cutoff. The present results are in agreement with values found in the literature, which reports rates of motor impairment ranging from 5% to 6% in the term and from 30% to 50% in the preterm populations.33. Goyen TA, Lui K. Developmental coordination disorder in ''apparently normal'' schoolchildren born extremely preterm. Arch Dis Chil. 2009;94:298-302. , 99. Foulder-Hughes LA, Cooke RW. Motor, cognitive, and behavioural disorders in children born very preterm. Dev Med Child Neurol. 2003;45:97-103. , 1010. Wocadlo C, Rieger I. Motor impairment and low achievement in very preterm children at eight years of age. Early Hum Dev. 2008;84:769-76. and 1212. Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80. The studies by Foulder-Hughes and Cooke99. Foulder-Hughes LA, Cooke RW. Motor, cognitive, and behavioural disorders in children born very preterm. Dev Med Child Neurol. 2003;45:97-103. and by Howe et al.1212. Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80. reported rates of 30.7% and 35.5%, respectively, below the fifth percentile among preterm children.
In the cognitive test, children from the PT group had worse performance than the FT group. These results corroborate the findings of other authors who have demonstrated that preterm infants have cognitive development within the normal range; however, when compared with their peers born full-term, they demonstrate significantly poorer performance on cognitive and neuropsychological tests.55. Aylward GP. Cognitive and neuropsychological outcomes: more than IQ scores. Ment Retard Dev Disabil. 2002;8:234-40. , 1212. Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80. , 1414. Claas MJ, Vries LS, Bruinse HW, Haastert IC, Uniken Venema MM, Peelen LM, et al. Neurodevelopmental outcome over time of preterm born children < 750 g at birth. Early Hum Dev. 2011;87:183-91. , 2727. Espirito Santo JL, Portuguez MW, Nunes ML. Cognitive and behavioral status of low birth weight preterm children raised in a developing country at preschool age. J Pediatr. 2009;85:35-40. and 2828. Méio MD, Lopes CS, Morsch DS, Monteiro AP, Rocha SB, Borges RA, et al. Desenvolvimento cognitivo de crianças prematuras de muito baixo peso na idade pré-escolar. J Pediatr (Rio J). 2004;80:95-502. Espírito Santo et al.,2727. Espirito Santo JL, Portuguez MW, Nunes ML. Cognitive and behavioral status of low birth weight preterm children raised in a developing country at preschool age. J Pediatr. 2009;85:35-40. in a study aiming to assess cognitive and behavioral development of 80 preterm infants with low birth weight, aged 4 to 5 years, observed a higher incidence of cognitive dysfunction and behavioral disorders in preterm infants, whose intellectual level was rated as predominantly medium or medium-low.
Conversely, Méio et al.,2828. Méio MD, Lopes CS, Morsch DS, Monteiro AP, Rocha SB, Borges RA, et al. Desenvolvimento cognitivo de crianças prematuras de muito baixo peso na idade pré-escolar. J Pediatr (Rio J). 2004;80:95-502. assessing the cognitive development at preschool age of very-low birth weight preterm infants, observed that the mean intelligence quotient, using the WPPSI-R, was below the normal range, close to borderline functional deficit at the evaluation. However, their sample included children with neurological impairment, behavioral disturbance, and visual function impairment, which could have influenced their results.
Consistent with the literature, the presence of atypical motor performance and history of PIVH contribute to increase the difference in cognitive performance between the PT and T groups.
Regarding the PEDI, the present results demonstrated that, regardless of the level of motor performance, children in the PT group had lower functional skill repertoire and required greater caregiver assistance than children in the FT group.
Other studies have also shown that preterm children have worse performance in activities of daily living when compared to full-term peers.1212. Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80. and 2929. Sullivan MC, Msall ME. Functional performance of preterm children at age 4. J Pediatr Nurs August. 2007;22: 297-309. At 4 years old, many self-care tasks are expected to be carried out with minimal caregiver assistance.2929. Sullivan MC, Msall ME. Functional performance of preterm children at age 4. J Pediatr Nurs August. 2007;22: 297-309. However, in preterm children, functional performance represents the junction of their capacities and limitations, and it may be affected by motor delay and health status. Thus, a child who is clumsy or has gross and/or fine motor coordination problems may not be able to button or zip up clothes, and/or use the toilet independently.2929. Sullivan MC, Msall ME. Functional performance of preterm children at age 4. J Pediatr Nurs August. 2007;22: 297-309.
Additionally, the literature also indicates that, in the relationship between preterm children and their caregivers, the latter tend to exert a more dominant role in the interaction and for a longer period of time, when compared to caregivers of children born full-term.2929. Sullivan MC, Msall ME. Functional performance of preterm children at age 4. J Pediatr Nurs August. 2007;22: 297-309. and 3030. Mancini MC, Megale L, Brandao MB, Melo APP, Sampaio RF. Efeito moderador do risco social na relaçao entre risco biológico e desempenho funcional infantil. Rev Bras Saúde Matern Infant. 2004;4:25-34. This behavior can be attributed, as reported by some mothers, to the tendency to distraction and difficulty completing the requested tasks, i.e., the greater participation of parents or caregivers in functional activities derives from the lower participation of the children.
Another factor that can justify the extra help from parents of preterm children in self-care activities may be related to the tendency to overprotect these children, who are more vulnerable from birth; this tendency may manifest as an underestimation of these children's capacities.2929. Sullivan MC, Msall ME. Functional performance of preterm children at age 4. J Pediatr Nurs August. 2007;22: 297-309. and 3030. Mancini MC, Megale L, Brandao MB, Melo APP, Sampaio RF. Efeito moderador do risco social na relaçao entre risco biológico e desempenho funcional infantil. Rev Bras Saúde Matern Infant. 2004;4:25-34. Thus, the functional performance at 4 years of age can be influenced both by prematurity and the environmental context of the child.
This study has some limitations, since due to the lack of standardized tools to assess the development of motor coordination in Brazilian children, the use of imported tests was necessary; however, comparisons were made only with the control group, tested under the same conditions as the study group.
Another limitation was the fact that the researcher had prior knowledge of which group each child belonged to; however, training was undertaken and the inter-examiner reliability was verified to ensure examiner's impartiality. This study was cross-sectional and had a convenience sample; although prospective studies are more adequate to evaluate the development of premature infants, these are difficult to perform in Brazil. Moreover, as this study aimed to assess a specific time in preschool, the cross-sectional design was chosen.
This study augments the evidence that preterm infants are more likely to have worse motor, cognitive, and functional performance than their peers born full-term, emphasizing the importance of early assessment, as these changes are already detectable at preschool age. Differentiating it from other Brazilian studies on the subject is the fact that its sample included children from different socioeconomic levels.
Considering the high rates of survival for preterm infants with low birth weight, even in developing countries, the results of this study may help in the planning of educational needs for this at-risk population.
It has been confirmed that children born prematurely constitute an at-risk group, and may benefit from effective educational or therapeutic intervention programs. It is noteworthy that there is better knowledge about the evolution of preterm newborns who have evident neurological signs and receive early diagnosis; however, children with mild sequelae, which will manifest later, are not yet provided proper attention, especially in the public healthcare system. Objective data documenting functional sequelae in these children may encourage the development of preventive programs for developmental stimulation, which are still scarce in Brazil.
References
-
1Silveira MF, Santos IS, Matijasevich A, Malta DC, Duarte EC. Nascidos pré-termo no Brasil entre 1994 e 2005 conforme o Sistema de Informações sobre Nascidos Vivos (SINASC). Cad Saude Publica. 2009;25:1267-75.
-
2Vieira ME, Linhares MB. Developmental outcomes and quality of life in children born preterm at preschooland schoolage. J Pediatr (Rio J). 2011;87:281-91.
-
3Goyen TA, Lui K. Developmental coordination disorder in ''apparently normal'' schoolchildren born extremely preterm. Arch Dis Chil. 2009;94:298-302.
-
4Martins IMB, Linhares MB, Martinez FE. Indicadores de desenvolvimento na fase pré-escolar de crianças nascidas pré-termo. Psicol Estud. 2005;10:235-43.
-
5Aylward GP. Cognitive and neuropsychological outcomes: more than IQ scores. Ment Retard Dev Disabil. 2002;8:234-40.
-
6Cooke RW. Perinatal and postnatal factors in very preterm infants and subsequent cognitive and motor abilities. Arch Dis Child Fetal Neonatal. 2005;90:F60-3.
-
7Roberts G, Anderson PJ, Davis N, Luca C, Cheong J, Doyle LW, The Victorian Infant Collaborative Study Group. Developmental coordination disorder in geographic cohorts of 8-year-old children born extremely preterm or extremely low birthweight in the 1990s. Dev Med Child Neurol. 2011;53:55-60.
-
8Davis NM, Ford GW, Anderson PJ, Doyle LW. Developmental coordination disorder at 8 years of age in a regional cohort of extremely-low-birth weight or very preterm infants. Dev Med Child Neurol. 2007;49:325-30.
-
9Foulder-Hughes LA, Cooke RW. Motor, cognitive, and behavioural disorders in children born very preterm. Dev Med Child Neurol. 2003;45:97-103.
-
10Wocadlo C, Rieger I. Motor impairment and low achievement in very preterm children at eight years of age. Early Hum Dev. 2008;84:769-76.
-
11Goyen TA, Lui K, Hummell J. Sensorimotor skills associated with motor dysfunction in children born extremely preterm. Early Hum Dev. 2011;87:489-93.
-
12Howe TH, Sheu CF, Wang TN, Hsu YW, Wang LW. Neuromotor outcomes in children with very low birth weight at 5 years of age. Am J Phys Med Rehabil. 2011;90:667-80.
-
13Kessel-Feddema B, Kleine M, Verhaak C. Concordance between school outcomes and developmental follow-up results of very preterm and/or low birth weight children at the age of 5 years. Eur J Pediatr. 2007;166:693-9.
-
14Claas MJ, Vries LS, Bruinse HW, Haastert IC, Uniken Venema MM, Peelen LM, et al. Neurodevelopmental outcome over time of preterm born children < 750 g at birth. Early Hum Dev. 2011;87:183-91.
-
15Rodrigues MC, Mello RR, Silva KS, Carvalho ML. Desenvolvimento cognitivo de prematuros à idade escolar: proposta de modelo hierarquizado para investigaçao dos fatores de risco. Cad Saude Publica. 2011;27:1154-64.
-
16Associaçao Brasileira de Empresas de, Pesquisa, Adoçao do CCEB. Critério de Classificaçao Econômica Brasil. 2010 [cited 10 Feb 2010]. Available from: http://www.abep.org/novo/Content.aspx?SectionID=84.
» http://www.abep.org/novo/Content.aspx?SectionID=84 -
17Henderson SE, Sugden DA, Barmett AL. Movement assessment battery for children2 second edition (Movement ABC-2). London. UK: The Psychological Corporation. 2007.
-
18Oliveira GE, Magalhaes LC, Salmela LF. Relaçao entre muito baixo peso ao nascimento, fatores ambientais e o desenvolvimento motor e cognitivo de crianças aos 5 e 6 anos. Revs Bras Fisioter. 2011;15:138-45.
-
19Souza C, Ferreira L, Catuzzo MT, Corrêa UC. O teste ABC do Movimento em crianças de ambientes diferentes. Rev Port Cien Desp. 2007;7:36-47.
-
20Smits-Engelsman BCM, Henderson SE, Michels CGS. The assessment of children with developmental coordination disorders in the Netherlands: the relationship between the Movement Assessment Battery for Children and the Korperkoordinations Test für Kinder. Hum Mov Sci. 1998;17:699-709.
-
21Ellinoudis T, Evaggelinou C, Kourtessis T, Konstantinidou Z, Venetsanou F, Kambas A. Reliability and validity of age band 1 of the Movement Assessment Battery for Children - Second Edition. Dev Disabilities. 2011;32:1046-51.
-
22Mancini MC. Inventário de Avaliaçao Pediátrica de Incapacidade (PEDI) - manual da versao brasileira adaptada. Belo Horizonte: Editora UFMG. 2005.
-
23Alves ICB, Duarte JLM. Escala de Maturidade Mental Columbia - padronizaçao brasileira - manual para aplicaçao e interpretaçao. Casa do Psicólogo. 2001.
-
24Goyen T, Lui K. Longitudinal motor development of ''apparently normal'' high-risk infants at 18 months, 3 and 5 years. Early Hum Dev. 2002;70:103-15.
-
25Goyen TA, Lui K, Woods R. Visual-motor, visual-perceptual, and fine motor outcomes in very-low-birthweight children at 5 years. Dev Med Child Neurol. 1998;40:76-81.
-
26Marlow N, Hennessy EM, Bracewell MA, Wolke D. Motor and executive function at 6 years of age after extremely preterm birth. Pediatr. 2007;120:793-804.
-
27Espirito Santo JL, Portuguez MW, Nunes ML. Cognitive and behavioral status of low birth weight preterm children raised in a developing country at preschool age. J Pediatr. 2009;85:35-40.
-
28Méio MD, Lopes CS, Morsch DS, Monteiro AP, Rocha SB, Borges RA, et al. Desenvolvimento cognitivo de crianças prematuras de muito baixo peso na idade pré-escolar. J Pediatr (Rio J). 2004;80:95-502.
-
29Sullivan MC, Msall ME. Functional performance of preterm children at age 4. J Pediatr Nurs August. 2007;22: 297-309.
-
30Mancini MC, Megale L, Brandao MB, Melo APP, Sampaio RF. Efeito moderador do risco social na relaçao entre risco biológico e desempenho funcional infantil. Rev Bras Saúde Matern Infant. 2004;4:25-34.
-
☆
Please cite this article as: Maggi EF, Magalhães LC, Campos AF, Bouzada MC. Preterm children have unfavorable motor, cognitive, and functional performance when compared to term children of preschool age. J Pediatr (Rio J). 2014;90:377-83.
-
☆☆
Study conducted in Faculdade de Medicina, Universidade Federal de Minas Gerais.
Publication Dates
-
Publication in this collection
Jul-Aug 2014
History
-
Received
02 Aug 2013 -
Accepted
16 Oct 2013