Abstracts
BACKGROUND AND OBJECTIVES: For more than 25 years, there has been no discussion in the Brazilian Journal of Anesthesiology about hemophiliac patients' perioperative management. Hemophilia has been described as a disease from the early 19th Century, but still today there are many hemophilia-related breakthroughs. This review aimed at pointing hemophilia patient-related perioperative care, focusing on hemophilia A management and the role of the anesthesiologist as part of the multidisciplinary team. CONTENTS: Hemophilia features are described in terms of clinical and laboratory findings, current pharmacological therapy and intraoperative care of hemophilia patients. CONCLUSIONS: Hemophiliac patients management has improved. As a consequence of this advance, it is important that new knowledge, especially related to replacement therapy, be mastered not only by hematologists but also by the whole clinical-surgical team. A multidisciplinary team of which the anesthesiologist is part has to be involved when hemophilia patients are submitted to surgical procedures. The anesthesiologist should be in charge of adopting most adequate approaches for hemophilia patients, actively participating and communicating with the members of the multidisciplinary team.
ANESTHESIA; ANESTHESIA
JUSTIFICATIVA E OBJETIVOS: Há mais de 25 anos não se discute, na Revista Brasileira de Anestesiologia, de maneira geral, o manuseio do paciente hemofílico durante o peri-operatório. Apesar da hemofilia ter sido definida como doença no início do século XIX, existem, até hoje, muitas descobertas relacionadas a ela. O objetivo dessa revisão é apontar os cuidados relacionados ao paciente hemofílico durante o período peri-operatório, ressaltando o manuseio da hemofilia tipo A e o papel do anestesiologista na equipe multidisciplinar. CONTEÚDO: Estão definidas as características da hemofilia quanto à clínica e aos achados laboratoriais, a terapia farmacológica atual e os cuidados com o manuseio do paciente hemofílico no intra-operatório. CONCLUSÕES: O manuseio do paciente hemofílico foi aprimorado. Como conseqüência desse avanço, percebe-se a importância e a necessidade de que novos conhecimentos, principalmente em relação à terapia de reposição, sejam dominados por hematologistas e por todo o corpo clínico-cirúrgico. Quando pacientes hemofílicos submetem-se a procedimentos cirúrgicos é necessário o envolvimento de uma equipe multidisciplinar da qual o anestesiologista faz parte. A este profissional cabe a responsabilidade de tomar as condutas mais adequadas frente ao paciente hemofílico, participando e comunicando-se ativamente com os membros da equipe multidisciplinar.
ANESTESIA; ANESTESIA
JUSTIFICATIVA Y OBJETIVOS: Hace más de 25 años que en la Revista Brasileña de Anestesiologia, de manera general, no se discute el manoseo del paciente hemofílico durante el peri-operatorio. A pesar de la hemofilia haber sido definida como enfermedad en el inicio del siglo XIX, existen hasta hoy, muchos hallazgos relacionados a ella. El objetivo de esa revisión es apuntar las atenciones relacionadas al paciente hemofílico durante el período peri-operatorio, realzando el manoseo de la hemofilia tipo A y el papel del anestesiologista en el equipo multidisciplinar. CONTENIDO: Están definidas las características de la hemofilia en cuanto a la clínica y a los hallazgos laboratoriales, la terapia farmacológica actual y las atenciones con el manoseo del paciente hemofílico en el intra-operatorio. CONCLUSIONES: El manoseo del paciente hemofílico fue perfeccionado. Como consecuencia de ese avance, se percibe la importancia y la necesidad de que nuevos conocimientos, principalmente con relación a la terapia de reposición, sean dominados por hematologistas y por todo el cuerpo clínico-quirúrgico. Cuando pacientes hemofílicos se someten a procedimientos quirúrgicos, es necesario el envolvimiento de un equipo multidisciplinar de la cual el anestesiologista hace parte. A este profesional cabe la responsabilidad de tomar las conductas más adecuadas frente al paciente hemofílico, participando y comunicándose activamente con los miembros del equipo multidisciplinar.
MISCELLANEOUS
Hemophilia and anesthesia* * Received from CET/SBA do SANE, Porto Alegre, RS
Hemofilia y anestesia
Rafael Py Gonçalves Flores, M.D.I; Airton Bagatini, TSA, M.D.II; Ari Tadeu Lírio dos Santos, TSA, M.D.II; Cláudio Roberto Gomes, TSA, M.D.III; Mário Sérgio Fernandes, M.D.IV; Roger Pelini Molon, M.D.V
IEx-Estagiário do CET/SBA do SANE
IICo-Responsável pelo CET/SBA do SANE
IIIInstrutor do CET/SBA do SANE
IVChefe do Serviço de Hematologia do Hospital São Lucas da PUCRS
VME2 do CET/SBA do SANE
Correspondence Correspondence to Dr. Airton Bagatini Address: Rua Santana, 483/301 ZIP: 90040-373 City: Porto Alegre, Brazil
SUMMARY
BACKGROUND AND OBJECTIVES: For more than 25 years, there has been no discussion in the Brazilian Journal of Anesthesiology about hemophiliac patients' perioperative management. Hemophilia has been described as a disease from the early 19th Century, but still today there are many hemophilia-related breakthroughs. This review aimed at pointing hemophilia patient-related perioperative care, focusing on hemophilia A management and the role of the anesthesiologist as part of the multidisciplinary team.
CONTENTS: Hemophilia features are described in terms of clinical and laboratory findings, current pharmacological therapy and intraoperative care of hemophilia patients.
CONCLUSIONS: Hemophiliac patients management has improved. As a consequence of this advance, it is important that new knowledge, especially related to replacement therapy, be mastered not only by hematologists but also by the whole clinical-surgical team. A multidisciplinary team of which the anesthesiologist is part has to be involved when hemophilia patients are submitted to surgical procedures. The anesthesiologist should be in charge of adopting most adequate approaches for hemophilia patients, actively participating and communicating with the members of the multidisciplinary team.
Key Words: ANESTHESIA, Coexistent diseases: hemophilia
RESUMEN
JUSTIFICATIVA Y OBJETIVOS: Hace más de 25 años que en la Revista Brasileña de Anestesiologia, de manera general, no se discute el manoseo del paciente hemofílico durante el peri-operatorio. A pesar de la hemofilia haber sido definida como enfermedad en el inicio del siglo XIX, existen hasta hoy, muchos hallazgos relacionados a ella. El objetivo de esa revisión es apuntar las atenciones relacionadas al paciente hemofílico durante el período peri-operatorio, realzando el manoseo de la hemofilia tipo A y el papel del anestesiologista en el equipo multidisciplinar.
CONTENIDO: Están definidas las características de la hemofilia en cuanto a la clínica y a los hallazgos laboratoriales, la terapia farmacológica actual y las atenciones con el manoseo del paciente hemofílico en el intra-operatorio.
CONCLUSIONES: El manoseo del paciente hemofílico fue perfeccionado. Como consecuencia de ese avance, se percibe la importancia y la necesidad de que nuevos conocimientos, principalmente con relación a la terapia de reposición, sean dominados por hematologistas y por todo el cuerpo clínico-quirúrgico. Cuando pacientes hemofílicos se someten a procedimientos quirúrgicos, es necesario el envolvimiento de un equipo multidisciplinar de la cual el anestesiologista hace parte. A este profesional cabe la responsabilidad de tomar las conductas más adecuadas frente al paciente hemofílico, participando y comunicándose activamente con los miembros del equipo multidisciplinar.
INTRODUCTION
The State of Rio Grande do Sul has 497 hemophiliac patients (Hemocenter, Porto Alegre; September 2003); these data might be underestimated if we consider the number of non diagnosed patients due to healthcare system deficiencies, because they are asymptomatic or for not having been submitted to surgical procedures. In any way, when this diagnosed population is submitted to surgical procedures, it deserves special care and a multidisciplinary team of health professionals informed about the disease, including qualified hematologist, surgeon and anesthesiologist.
Hemophilia is a hemorrhagic trend almost exclusively affecting males (X-related recessive disease). In 85% of cases it is caused by factor VIII deficiency, being called hemophilia A or classic hemophilia 1-4. In approximately 15% of cases there is factor IX deficiency (hemophilia B). The incidence of hemophilia A is 1 in 5000 or 10000 males and may be classified as mild, moderate or severe.
It is severe if coagulation factor VIII level is below 1%; it is moderate if it is between 1% and 5%; and mild if it is above 5% 1,2,5,6. Normal factor VIII plasma levels vary 0.5 U/mL to 1.5 U/mL and each U/mL corresponds to 100% factor VIII found in 1 mL of plasma. Laboratory diagnosis of hemophilia A is based on prolonged TTPa and factor VIII deficiency, normal factor IX and von Willebrand factor levels. The hemofilic patients may present spontaneous bleedings or trauma-related bleeding. Spontaneous bleeding is more common in severe hemophilia. Joints are in general the most affected, but any other part of the body, including central nervous system (CNS), may be subject to spontaneous hemorrhage 1,7.
During childhood, bleeding may manifest as macules or hematoma, but as the child grows intra-articular hemorrhage or hemarthrosis may be more frequent. Family attitude of protecting these children may promote severe psychological disorders in some individuals.
Treatment of hemophilia is complex because the deficiency of a coagulation protein affects several body systems and is reflected in the ability to psycho-social adaptation 1,8
IMPORTANT ASPECTS OF PERIOPERATIVE MANAGEMENT OF HEMOPHILIC PATIENTS DURING ELECTIVE SURGERIES
Hemophiliac patients may be admitted for several surgical procedures, from vascular access procedures to major orthopedic surgeries 9,10.
Hemophiliac patients procedures need a multidisciplinary approach involving medical, lab and physical therapy skills 1,11.
The aim therapy objective is to adequately correct factor deficiency before, during and after surgery, for a period enough to allow wound healing 12.
Preoperative Period
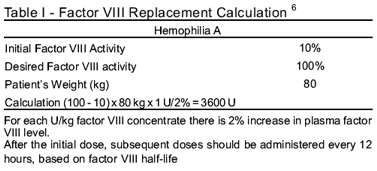
The goal in this stage is to correct factor VIII deficiency before the procedure, which is hematologists responsibility. It must be known that patients need 100% correction of their factor VIII before any surgical procedure, and this must be confirmed before surgery 5,12,13. For every Ul/kg of infused factor VIII concentrate, there is 2% increase in its respective plasma level 5,6.
During this stage, the hematologist should also rule out the presence of factor VIII inhibiting antibodies, orient about the non-use of anti-platelet drugs one week prior to surgery and assure the presence of adequate amounts of factor VIII concentrate available in the perioperative period.
During preanesthetic evaluation, the anesthesiologist should evaluate the status of joints, look for spontaneous hematomas, check tracheal intubation conditions and the presence of oral injuries (especially endo and periodontal injuries, which are very common) 2. The anesthesiologists should also be aware of the procedures scheduled by the hematologist, discuss possible intraoperative approaches and be vigilant for adequate hemostatic monitoring of such patients before surgery.
Patients should receive concentrate before minor invasive procedures, such as lumbar puncture, arterial blood gases collection or bronchoscopy with lavage material and biopsy.
Last but not least, it is specifically to the surgeon to schedule the surgical procedure in the beginning of the week and as early as possible during the day to help access to laboratories and specialists, in addition to scheduling minor procedures close to major procedures to prevent a new replacement stage, thus avoiding more costs and risks 6.
Intraoperative Period
The coagulation consumption factors is highly increased during surgery. The anesthesiologist must take some minor care to prevent the anesthetic technique of contributing to the possibility of hemorrhages or hematomas distant from the surgical site. Even being unlikely, if the patient is adequately treated in terms or factor VIII replacement, it is important to stress some anesthetic management steps:
a) Positioning: monitoring patients' position on the operating table observing their articular limitations;
b) Induction: allowing for a relaxed induction, in a timing necessary for drugs action and effect. Avoiding superficial anesthesia or drugs such as succinylcholine to prevent muscle shakes which may worsen muscle and joints hemorrhagic state;
c) Intubation and airway handling: this should be extremely careful, tubes should be previously greased with vaseline to decrease attrition with the mucosa and nasotracheal intubation should be avoided. Care is also needed with the insertion of probes and thermometers, preventing trauma injuries by manipulation because tongue and airway muscles bleeding may rapidly lead to airway obstruction 6;
d) Maintenance of anesthesia: hypertension and tachycardia are undesirable because they lead to increased surgical field bleeding; controlled hypotension techniques are not recommended because the will prevent the surgeon to hemostasis small vessels, which are major postoperative bleeding sources 2. It is necessary to maintain hemodynamic conditions as close as possible to normal;
e) Recovery: it is desirable that extubation is performed in anesthetic depth without cough reflex. Pharyngeal aspiration should be extremely careful and delicate. Anesthetic blocks are counterindicated as well as muscular injections 2,6. There are however reports of successful anesthetic blocks (axillary, epidural and spinal) in hemophilic patients, provided factor VIII levels were maintained above 30% throughout the perioperative period 14.
Surgeon should give special attention to small vessels hemostasis which would otherwise have been left for hemostatic physiological mechanisms 2.
Postoperative Period
Hemophiliac patients need special postoperative hemostatic therapy. So far, there are no precise values determined for the level of factor VIII activity and for the period of time they should be postoperatively maintained. It is recommended that factor VIII should be continuous to maintain its postoperative levels in approximately 50% 5,9,12,13.
These levels should be maintained for up to 6 weeks after orthopedic procedures and 1 to 2 weeks for other procedures 6. Monitoring should be achieved by dosing factor VIII levels once or twice a day. Although not ideal, it is also possible to monitoring with serial TTPa measurement if serial factor VIII measurement is not available. Patients' coagulation will be considered acceptable when the ratio between patients' TTPa and normal TTPa is equal to or below 1.2 2.
It is important for the medical team to keep in touch with patients after hospital discharge, even in the absence of bleeding; and the institution shall have factor VIII reserves in case of perioperative hemorrhagic emergency.
PHARMACOLOGICAL THERAPY
1) Fresh frozen plasma: used since the 50s to treat hemophilia5. It contains 175 to 250 mL of volume per bag with 70 to 90 U/dL factor VIII, factor IX, von Willebrand factor and other coagulating factors. It is able to replace 15% to 20% factor VIII with a volume of 800 to 1000 mL 2. It may be used to treat known coagulation factor deficiencies in cases when the specific concentrate is not available 15.
2) Cryoprecipitate: it has been a major advance in factor VIII replacement therapy during the 60s. It is extracted from fresh frozen plasma bags after slow thawing and centrifugation of the cryoprecipitate part, rich in factor VIII and fibrinogen. In normal preparations, they are not submitted to viral attenuation and contain 60 to 100 factor VIII units and 200 to 300 mg fibrinogen in a volume of 20 to 30 mL. Currently they are not recommended, but may be used in cases when factor VIII concentrate is not available 15.
3) Factor VIII concentrate: purified factor VIII concentrate (dry frozen) is the product of choice for replacement therapy 1,5,6,12. It is preferred because it is stable, easy to handle and store, and contains standardized amounts of coagulating factor, with lower probability of transmitting viral diseases as compared to cryoprecipitate or plasma 12. Concentrates are prepared as from a plasma pool of a large number of donors or, as it is done more recently, through the use of recombinant DNA technology, and may be classified according to their degree of purity. For example: intermediate-high purity concentrate or ultrapure products obtained through techniques using chromatography by immunoaffinity with monoclonal antibodies and recombinant DNA techniques. Factor VIII concentrate is commercially available since the 70s, and since 1985 it is submitted to viral attenuation procedures, which significantly decrease the risk for HIV and hepatitis transmission, as compared to older products.
Approximately 20% to 33% of moderate and severe hemophilia A patients develop factor VIII inhibiting antibodies. The development of such inhibitors complicates the management of hemophilia patients because it makes them refractory to factor VIII therapy. These patients may be divided in low and high response groups, as for the production of inhibitors. Therapeutic options for those patients include replacement with porcine factor VIII (Table I), prothrombin complex concentrate, therapy with activated factor VII and even plamapheresis as a palliative measure in emergency situations 5,9.
4) Desmopressin: it is a synthetic vasopressin analog, useful for patients with mild hemophilia who have obtained good response after a previous test with the drug. Desmopressin stimulates endogenous factor VIII release by endothelial cells to the systemic circulation and may increase 2 to 3-fold the levels of factor VIII, being an alternative for less severe hemorrhages in mild hemophilia patients. Administration may be intravenous, subcutaneous or nasal (specific spray for hemophilics). Intravenous dose is 0.3 µg.kg-1 diluted in 30 to 50 mL saline, infused in 15 to 20 minutes. Nasal dose is 150 µg.kg-1 for individuals weighing less than 50 kg and 300 µg.kg-1 for individuals with more than 50 kg 5,12,16.
5) Antifibrinolytics: these are important adjuvant agents for hemorrhage prevention and treatment during oral and dental surgeries because they act by inhibiting the fibrinolytic action of salivary enzymes. Epsilon aminocaproic acid may be orally or intravenously administered in the doses of 200 mg.kg-1, followed by 100 mg.kg-1 every 6 hours (maximum 5 g/dose). Tranexamic acid may be administered in the oral dose of 25 mg.kg-1 (maximum 1.5 g) or in the intravenous dose of 10 mg.kg-1 (maximum 1 g) every 8 hours. Both drugs are counterindicated in the presence of hematuria and in patients with factor VIII inhibitors being treated with prothrombin complex concentrate, due to the risk for thromboembolism 5,12,16.
6) Porcine factor VIII concentrate: used in patients with human factor VIII inhibitors. After treatment some patients may develop porcine factor VIII inhibitors.
7) Prothrombin concentrate complex: made up of prothrombin concentrate, factors IX and X and variable factor VIII amounts. Used in hemophilia A in patients with factor VIII inhibitors, in the doses of 75 to 100 U/kg. It is associated to thromboembolic problems 5.
Brazilian Journal of Anesthesiology, 2004; 54: 6: 865-871
Hemophilia and anesthesia
Rafael Py Gonçalves Flores; Airton Bagatini; Ari Tadeu Lírio dos Santos;
Cláudio Roberto Gomes; Mário Sérgio Fernandes; Roger Pelini Molon
CONCLUSION
Hemophiliac patients' management has improved along the years. As a consequence of this advance, it is important that new knowledge, especially related to replacement therapy, be mastered not only by hematologists but also by the whole clinical-surgical team. According to what has been described, a multidisciplinary team, of which the anesthesiologist is part, has to be involved when hemophilia patients are submitted to surgical procedures. The anesthesiologist should be in charge of adopting most adequate approaches for hemophiliac patients, actively participating in the medical team, maintaining the necessary communication with clinician, surgeon and hematologist.
REFERENCES
Submitted for publication February 4, 2004
Accepted for publication May 17, 2004
- 01. Boayue KB, Bell BA - Characteristics and management of bleeding in hemophilia and von Willebrand disease, Int J Pediat Hem Onc, 1994;1:449-461.
- 02. Ferreira AA, Cangiani LM, Vanetti LFA - Anestesia e o paciente hemofílico. Rev Bras Anestesiol, 1977;27:467-474.
- 03. Lusher JM, Warrier I - Hemophilia A. Hematol Oncol Clin North Am, 1992;6:1021-1033.
- 04. Hedner U, Glazer S - Management off hemophilia patients with inhibitors. Hematol Oncol Clin North Am. 1992;6:1035-1046.
- 05. DiMichele D, Neufeld EJ - Hemophilia. A new approach to an old disease. Hematol Oncol Clin North Am, 1998;12:1315-1344.
- 06. Parmet JL, Horrow JC - Hematological Diseases, em: Benumof JI - Anesthesia and Uncommon Diseases. Philadelphia W B Saunders, 1998;299-301.
- 07. Guyton AC, Hall JE - Tratado de Fisiologia Médica, 9Ş Ed, Editora Guanabara Koogan, Rio de Janeiro, 1997;421-430.
- 08. Roizen MF- Anesthesia Implications of Concurrent Diseases, em Miller RD - Anesthesia. 5th Ed, Philadelphia, Churchill Livingstone, 2000;903-1015.
- 09. Chaney JD, Nielsen VG - Considerations for the hemophiliac patient with inhibitors to factor VIII. Anesth Analg, 2001;92: 785-786.
- 10. Martlew VJ - Perioperative management of patients with coagulation disorders. Br J Anaesth, 2000;85:446-455.
- 11. Hoyer LW - Hemophilia A. N Engl J Med, 1994;330:38-47.
- 12. The United States Pharmacopoeia Convention, Inc - Hemophilia Management, em Transfusion Medicine Reviews, 1998;12:2: 128-140.
- 13. Hemophilia of Georgia, Inc - Protocols for the Treatment of Hemophilia and von Willebrand Disease, em Monograph Series nş 14, 1998.
- 14. Kang SB, Rumball KM, Ettinger RS - Continuous axillary brachial plexus analgesia in patient with severe hemophilia. J Clin Anesth, 2003;15:38-40.
- 15. Practice guidelines for blood component therapy: a report by the American Society of Anesthesiologists Task Force on blood component therapy. Anesthesiology 1996;84:732-747.
- 16. Lethagen S - Desmopressin - a haemostatic drug: state-of-the-art review. Eur J Anaesthesiol, 1997;14:1-9.
Publication Dates
-
Publication in this collection
26 Jan 2005 -
Date of issue
Dec 2004
History
-
Received
04 Feb 2004 -
Accepted
17 May 2004