Abstracts
Background and objectives:
Walker-Warburg Syndrome is a rare, autosomal recessive congenital muscular dystrophy manifested by central nervous system, eye malformations and possible multisystem involvement. The diagnosis is established by the presence of four criteria: congenital muscular dystrophy, type II lissencephaly, cerebellar malformation, and retinal malformation. Most of the syndromic children die in the first three years of life because of respiratory failure, pneumonia, seizures, hyperthermia and ventricular fibrillation.
Case report:
The anesthetic management of a two-months-old male child listed for elective ventriculo-peritoneal shunt operation was discussed.
Conclusions:
A careful anesthetic management is necessary due to the multisystem involvement. We reported anesthetic management of a two-months-old male child with Walker -Warburg Syndrome who was listed for elective ventriculo-peritoneal shunt operation.
Walker-Warburg Syndrome; Congenital muscular dystrophy; General anesthesia
Justificativa e objetivos:
A síndrome de Walker-Warburg é uma distrofia muscular autossômica recessiva congênita rara, manifestada pelo sistema nervoso central com malformações oculares e possível envolvimento de vários sistemas. O diagnóstico é estabelecido pela presença de quatro critérios: distrofia muscular congênita, lisencefalia tipo II, malformação cerebelar e malformação da retina. A maioria das crianças com a síndrome morre nos primeiros três anos de vida por causa de insuficiência respiratória, pneumonia, convulsões, hipertermia e fibrilação ventricular.
Relato de caso:
É discutida a conduta anestésica em uma criança do sexo masculino, de dois meses, programada para cirurgia eletiva de derivação ventrículo-peritoneal.
Conclusões:
Uma abordagem anestésica cuidadosa é necessária por causa do envolvimento de vários sistemas. Relatamos a conduta anestésica em uma criança do sexo masculino de dois meses com síndrome de Walker-Warburg, que foi programada para cirurgia eletiva de derivação ventrículo-peritoneal.
Síndrome de Walker-Warburg; Distrofia muscular congênita; Anestesia geral
Justificativa y objetivos:
el síndrome de Walker-Warburg es una distrofia muscular autosómica recesiva congénita rara, manifestada por el sistema nervioso central con malformaciones oculares y la posible participación de varios sistemas. El diagnóstico se establece por la presencia de 4 criterios: distrofia muscular congénita, lisencefalia tipo II, malformación cerebelar y malformación de la retina. La mayoría de los niños con el síndrome se muere a los primeros 3 años de vida debido a la insuficiencia respiratoria, neumonía, convulsiones, hipertermia y fibrilación ventricular.
Relato de caso:
se discute aquí la conducta anestésica en un niño del sexo masculino, de 2 meses de edad, programado para la cirugía electiva de derivación ventrículo-peritoneal.
Conclusiones:
un cuidadoso abordaje anestésico se hace necesario debido a la involucración de varios sistemas. Relatamos la conducta anestésica en un niño del sexo masculino de 2 meses de edad, con el síndrome de Walker-Warburg, que fue programado para la cirugía electiva de derivación ventrículo-peritoneal
Síndrome de Walker-Warburg; Distrofia muscular congénita; Anestesia general
Introduction
Walker-Warburg Syndrome (WWS) is a rare, autosomal recessive congenital muscular dystrophy (CMD).11. Walker AE. Lissencephaly. Arch Neurol Psychiatry. 1942;48:13-29. The diagnosis is generally depends on clinical manifestations, genetic diagnosis has been made by DNA analysis only in 10-20% of the cases. The diagnosis is established by the presence of four criteria: CMD, type II lissencephaly, cerebellar malformation, and retinal malformation.22. Dobyns WB, Pagon RA, Armstrong D, et al. Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet. 1989;32:195-210. The other frequently observed abnormalities are ventricular dilatation with or without hydrocephalus, anterior chamber malformation of eye, congenital macrocephaly, Dandy-Walker malformation. Congenital microcephaly, microphthalmia, ocular coloboma, congenital cataract, urogenital anomalies, cleft lip and cleft palate are the less frequently observed abnormalities. Differential diagnosis with Fukuyama CMD, muscle-eye-brain disease, cerebro-ocular-cerebral syndrome is depend on the severity of the clinical manifestations and radiological findings.22. Dobyns WB, Pagon RA, Armstrong D, et al. Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet. 1989;32:195-210.,33. Sahajanda H, Meneges J. Anaesthesia for a child with Walker-Warburg syndrome. Pediatr Anesth. 2003;13:624-8. Clinical manifestation are present at birth or or appears after in a short period. Most of the syndromic children dies in the first three years of life because of respiratory failure, pneumonia, seizures, hyperthermia and ventricular fibrillation. Prenatal diagnosis is possible and the risk of having another child with this syndrome is 25% in the families with one affected child.44. Crowe C, Jassani M, Dickerman L. The perinatal diagnosis of the Walker-Warburg syndrome. Diagnosis. 1986;6:177-85.
Case report
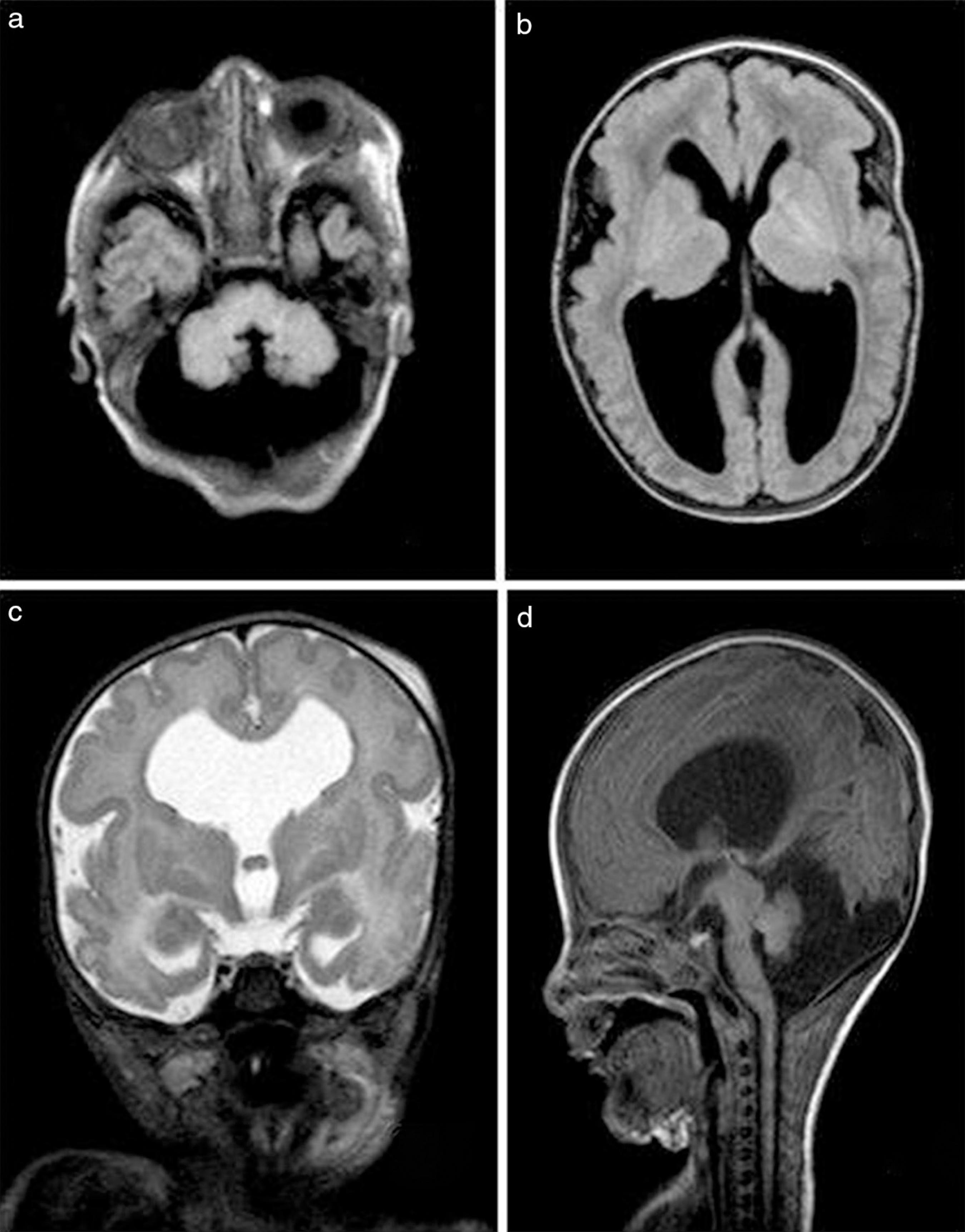
A two-months-old male child weighing 3.3 kg was listed for elective ventriculo-peritoneal shunt operation. Delivery had been by cesarean section at the 38th weeks of gestation. The mother's previous gestation had been ended by medical abortus due to determined hydrocephalus by ultrasonographic evaluations and the parents were relative. The patient was admitted to intensive care unit of newborn because of hydrocephalus and respiratory distress. Macrocephalia, low nasal bridge, frontal bulging of the forehead, micrognathia, receding mandible, moderate hypotonia, and bilateral retinal detachment were determined by physical examination. Creatine phosphokinase (CPK) levels were measured as 4226 u L−1 (normal 24-195 u L−1). Magnetic resonance imaging (MRI) was revealed type II lissencephaly, hypomyelination of white matter, dilated ventricles, bilateral cerebellar hypoplasia, agesis of septum pellucidum, Dandy-Walker malformation, bilateral hyperplasia of vitreus and buphthalmus (Fig. 1).
FLAIR MR scan images demonstrating Dandy-Walker abnormality (A and D); and lissencephaly with hydrocephalus (B).T2 WI MR scan image demonstrating septum pellucidum dysgenesis (C).
After obtaining written informed parental consent, the patient was fasted for 3 h. The probability of difficult entubation was thought and equipment was prepared. Following the monitorization of pulse oxymetry, noninvasive blood pressure, electrocardiography, body temperature, anesthesia induction was made with sevoflurane and nitrous oxide in oxygen. An intravenous cannula was inserted and laryngoscopy was performed during spontaneous ventilation. The intubation attempts performed using traditional midline approach with anterior cervical pressure and increased extension of head were failed, view was evaluated as grade 4. Therefore, the patient's head was slightly turned to left and Miller size zero straight blade was introduced extreme right side of the mouth. The tip of the epiglottis visualized by the aid of the external manipulation of the larynx and blind intubation was performed by using a 3.5 mm uncuffed endotracheal tube. The endotracheal tube placement was confirmed with capnography and auscultation of lungs. The endotracheal tube was fixed and an oropharyngeal throat pack was inserted. Anesthesia was maintained with sevoflurane 2% with oxygen and nitrous oxide mixture in the ratio of 50:50. Neither neuromuscular blocker agents nor opioids were used during the surgery. Fluid management was made intravenous administration of balanced electrolyte solution regarding the calculation of the perioperative fluid deficits and basal requirement of the child. At the end of the surgery, the throat pack was removed, and the trachea was extubated when the patient was full-awake. Postoperative analgesia was provided with paracetamol 25 mg kg-1. After a uneventful recovery period, the patient was taken into the intensive care unit.
Discussion
A careful anesthetic management is necessary due to the multisystem involvement. Difficult airway should always keep in mind because of short neck, micrognathia, receding mandible and sometimes accompanied cleft lip and/or cleft palate. After the difficult intubation preparation, we preferred inhalation induction with sevorane without suppression of spontan ventilation. Due to the intrusion possibility of a curved blade into the view line, Miller size zero straight blade was used but visualization of larynx could not be provided by the traditional midline approach. Therefore, paraglossal straight blade laryngoscopy described in difficult tracheal intubation was used and blind intubation was performed after visualization of the tip of the epiglottis.55. Henderson J. The use of paraglossal straight blade laryngoscopy in difficult tracheal intubation. Anaesthesia. 1997;52:522-6. Lateral approach was provided to bypass the tongue and maxillary structures and improved view of the glottis. In case of unsuccessful intubation, our back-up plan was to perform fiber-optic laryngoscopy. The use of laryngeal mask airway was discussed but was not preferred because to provide a safe airway could be impossible due to the movements of head during the operation and the probability of the aspiration of the oropharyngeal secretions. To use the succinylcholine was avoided because it can cause exaggerated potassium release, fatal cardiac dysrhytmias and malign hyperthermia. Because of the increased hyperthermia risk in WWS, body temperature was monitored during the surgery and postoperative period.22. Dobyns WB, Pagon RA, Armstrong D, et al. Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet. 1989;32:195-210.,33. Sahajanda H, Meneges J. Anaesthesia for a child with Walker-Warburg syndrome. Pediatr Anesth. 2003;13:624-8. Nondepolarizing muscle relaxants and opioids were not used due to the possibility of delayed recovery and postoperative respiratory depression resulting from the chronic weakness of respiratory muscles.22. Dobyns WB, Pagon RA, Armstrong D, et al. Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet. 1989;32:195-210.,33. Sahajanda H, Meneges J. Anaesthesia for a child with Walker-Warburg syndrome. Pediatr Anesth. 2003;13:624-8. Postoperative analgesia was provided with paracetamol, heavy sedation was avoided. Postoperative pulmonary dysfunction and consequent aspiration pneumonia was kept in the mind and oropharyngeal secretions were suctioned regularly.
Although, our patient had not any cardiac or genitourinary abnormality, renal dysfunction and involvement of cardiac muscles can observe in WWS and it is important to recognize the increased perioperative cardiac and renal failure risk.22. Dobyns WB, Pagon RA, Armstrong D, et al. Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet. 1989;32:195-210. Maintenance of adequate fluid management should be provide to avoid the renal dysfunction and cardiovascular depression.
Children with WWS may have increased intracranial pressure (ICP), so anesthetic management should include the precautions to provide adequate cerebral circulation such as to avoid the excessive decrease or increase in mean arterial pressure.33. Sahajanda H, Meneges J. Anaesthesia for a child with Walker-Warburg syndrome. Pediatr Anesth. 2003;13:624-8. It is also important to recognize that the patients with WWS are prone to develop seizures, episodes of central and obstructive apnea, difficulty in swallowing and consequent cardiorespiratory failure, aspiration pneumonia and sepsis.22. Dobyns WB, Pagon RA, Armstrong D, et al. Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet. 1989;32:195-210.,33. Sahajanda H, Meneges J. Anaesthesia for a child with Walker-Warburg syndrome. Pediatr Anesth. 2003;13:624-8. It should be avoid the use of the epileptogenic drugs and hypoxic episodes which can lead to seizures.
In summary, for an unevenful anesthetic management and postoperative care it should be keep in mind that WWS is a severe CMD with multisystemic involvement.
Referências
-
1Walker AE. Lissencephaly. Arch Neurol Psychiatry. 1942;48:13-29.
-
2Dobyns WB, Pagon RA, Armstrong D, et al. Diagnostic criteria for Walker-Warburg syndrome. Am J Med Genet. 1989;32:195-210.
-
3Sahajanda H, Meneges J. Anaesthesia for a child with Walker-Warburg syndrome. Pediatr Anesth. 2003;13:624-8.
-
4Crowe C, Jassani M, Dickerman L. The perinatal diagnosis of the Walker-Warburg syndrome. Diagnosis. 1986;6:177-85.
-
5Henderson J. The use of paraglossal straight blade laryngoscopy in difficult tracheal intubation. Anaesthesia. 1997;52:522-6.
Publication Dates
-
Publication in this collection
Mar-Apr 2014
History
-
Received
30 Oct 2012 -
Accepted
19 Dec 2012