Abstracts
BACKGROUND AND OBJECTIVES:
A review of all the adjuncts for intravenous regional anaesthesia concluded that there is good evidence to recommend NonSteroidal Anti-Inflammatory agents and pethidine in the dose of 30 mg dose as adjuncts to intravenous regional anaesthesia. But there are no studies to compare pethidine of 30 mg dose to any of the NonSteroidal Anti-Inflammatory agents.
METHODS:
In a prospective, randomized, double blind study, 45 patients were given intravenous regional anaesthesia with either lignocaine alone or lignocaine with pethidine 30 mg or lignocaine with ketprofen 100 mg. Fentanyl was used as rescue analgesic during surgery. For the first 6 h of postoperative period analgesia was provided by fentanyl injection and between 6 and 24 h analgesia was provided by diclofenac tablets. Visual analogue scores for pain and consumption of fentanyl and diclofenac were compared.
RESULTS:
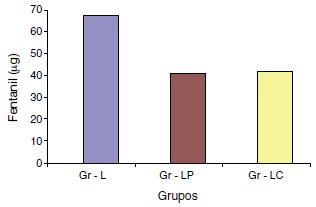
The block was inadequate for one case each in lignocaine group and pethidine group, so general anaesthesia was provided. Time for the first dose of fentanyl required for postoperative analgesia was significantly more in pethidine and ketoprofen groups compared to lignocaine group (156.7 ± 148.8 and 153.0 ± 106.0 vs. 52.1 ± 52.4 min respectively). Total fentanyl consumption in first 6 h of postoperative period was less in pethidine and ketoprofen groups compared to lignocaine group (37.5 ± 29.0 mcg, 38.3 ± 20.8 mcg vs. 64.2 ± 27.2 mcg respectively). Consumption of diclofenac tablets was 2.4 ± 0.7, 2.5 ± 0.5 and 2.0 ± 0.7 in the control, pethidine and ketoprofen group respectively, which was statistically not significant. Side effects were not significantly different between the groups.
CONCLUSION:
Both pethidine and ketoprofen are equally effective in providing postoperative analgesia up to 6 h, without significant difference in the side effects and none of the adjuncts provide significant analgesia after 6 h.
Intravenous regional anaesthesia; Pethidine; Ketoprofen
JUSTIFICATIVA E OBJETIVOS:
uma revisão de todos os adjuvantes para anestesia regional intravenosa concluiu que há boas evidências para recomendar os agentes anti-inflamatórios não esteroides e petidina em dose de 30 mg como adjuvantes para anestesia regional intravenosa. Porém, não há estudos que comparem petidina (30 mg) com quaisquer dos agentes anti-inflamatórios não esteroides.
MÉTODOS:
em um estudo prospectivo, randômico e duplo-cego, 45 pacientes receberam anestesia regional intravenosa com apenas lidocaína ou lidocaína com petidina (30 mg) ou lidocaína com cetoprofeno (100 mg). Fentanil foi usado como analgésico de resgate durante a cirurgia. Durante as seis primeiras horas de pós-operatório, analgesia foi fornecida via injeção de fentanil e, entre seis e 24 horas, analgesia foi fornecida via comprimidos de diclofenaco. Os escores visuais analógicos para dor e do consumo de fentanil e diclofenaco foram comparados.
RESULTADOS:
o bloqueio foi inadequado para um caso tanto do grupo lidocaína quanto do grupo petidina; portanto, anestesia geral foi administrada. O tempo para a primeira dose necessária de fentanil para analgesia pós-operatória foi significativamente maior nos grupos petidina e cetoprofeno em comparação com o grupo lidocaína (156,7 ± 148,8 e 153,0 ± 106,0 vs. 52,1 ± 52,4 minutos, respectivamente). O consumo total de fentanil nas primeiras seis horas de pós-operatório foi menor nos grupos petidina e cetoprofeno em comparação com o grupo lidocaína (37,5 ± 29,0 mcg, 38,3 ± 20,8 mcg vs. 64,2 ± 27,2 mcg, respectivamente). O consumo de comprimidos de diclofenaco foi de 2,4 ± 0,7, 2,5 ± 0,5 e 2,0 ± 0,7 no grupo controle, petidina e cetoprofeno, respectivamente, o que não foi estatisticamente significante. Os efeitos colaterais não foram significativamente diferentes entre os grupos.
CONCLUSÃO:
tanto petidina quanto cetoprofeno são igualmente eficazes para analgesia pós-operatória até seis horas, sem diferença significante nos efeitos colaterais, e nenhum dos adjuvantes proporcionou analgesia significativa após seis horas.
Anestesia regional intravenosa; Petidina; Cetoprofeno
JUSTIFICACIÓN Y OBJETIVOS:
una revisión sobre todos los adyuvantes para la anestesia regional intravenosa concluyó que hay buenas evidencias para recomendar los agentes antiinflamatorios no esteroideos y la petidina en dosis de 30 mg como adyuvantes para la anestesia regional intravenosa. Sin embargo, no hay estudios comparando la petidina (30 mg) con cualesquiera de los agentes antiinflamatorios no-esteroideos.
MÉTODOS:
en un estudio prospectivo, aleatorizado y doble ciego, 45 pacientes recibieron anestesia regional intravenosa con solamente lidocaína o lidocaína con petidina (30 mg) o lidocaína con ketoprofeno (100 mg). El fentanilo fue usado como analgésico de rescate durante la cirugía. Durante las 6 primeras horas del postoperatorio, la analgesia fue suministrada vía inyección de fentanilo y entre 6 y 24 h, la analgesia fue suministrada vía comprimidos de diclofenaco. Se compararon las puntuaciones visuales analógicas para el dolor y el consumo de fentanilo y diclofenaco.
RESULTADOS:
el bloqueo fue inadecuado para un caso tanto del grupo lidocaína como del grupo petidina; por tanto, se administró anestesia general. El tiempo para la primera dosis necesaria de fentanilo para analgesia postoperatoria fue significativamente mayor en los grupos petidina y ketoprofeno en comparación con el grupo lidocaína (156,7 ± 148,8 y 153,0 ± 106,0 vs. 52,1 ± 52,4 min, respectivamente). El consumo total de fentanilo en las primeras 6 h del postoperatorio fue menor en los grupos petidina y ketoprofeno en comparación con el grupo lidocaína (37,5 ± 29,0 mcg; 38,3 ± 20,8 mcg vs. 64,2 ± 27,2 mcg, respectivamente). El consumo de comprimidos de diclofenaco fue de 2,4 ± 0,7; 2,5 ± 0,5; y 2 ± 0,7 en el grupo control, petidina y ketoprofeno, respectivamente, lo que no fue estadísticamente significativo. Los efectos secundarios no fueron significativamente diferentes entre los grupos.
CONCLUSIÓN:
tanto la petidina como el ketoprofeno son igualmente eficaces para la analgesia postoperatoria hasta 6 h, sin diferencia significativa en los efectos secundarios, y ninguno de los adyuvantes proporcionó analgesia significativa después de 6 h.
Anestesia regional intravenosa; Petidina; Ketoprofeno
Introduction
Intravenous regional anaesthesia (IVRA) is safe and effective way to provide anaesthesia for the forearm and hand surgeries lasting up to 90 min. Main limitations to its use are significant tourniquet pain during surgery and lack of postoperative analgesia. To overcome these problems many of adjuncts drugs have been used along with local anaesthetic agents in IVRA. A systemic review of all the adjuncts used in IVRA, by Choyce and Peng11. Choyce A, Peng P. A systemic review of adjuncts for intravenous regional anaesthesia for surgical procedures. Can J Anaesth. 2002;49:32-45. concluded that there is good evidence to use NonSteroidal Anti-Inflammatory agents (NSAIDs), particularly ketorolac. Among the opioids, the review suggested that only the pethidine in a dose of 30 mg has substantial postoperative benefit, but at the expense of post deflation side effects. Ketoprofen is an NSAID available in intravenous formulation, which has a proven efficacy in providing postoperative analgesia in surgeries such as tonsillectomy, thyroid and nasal surgeries.22. Basto ER, Waintrop C, Mourey FD, Landru JP, Eurin BJ, Jacob LP. Intravenous ketoprofen in thyroid and parathyroid surgery. Anesth Analg. 2001;92:1052-7. , 33. Tuomilehto H, Kokki H, Tuovinen K. Comparison of intravenous and oral ketoprofen for post operative pain after adenoidec- tomy in children. Br J Anaesth. 2000;85:224-7. , 44. Elhakim M. Comparison of intravenous ketoprofen with pethi- dine for postoperative pain relief following nasal surgery. Acta Anaesthesiol Scand. 1991;35:279-82. , 55. Subramaniam R, Ghai B, Khetarpal M, Subramanyam MS. A comparison of intravenous ketoprofen versus pethidine on peri-operative analgesia and post-operative nausea and vomiting in paediatric vitreoretinal surgery. J Postgrad Med. 2003;49:123-6. and 66. Priya V, Divatia JV, Sareen R, Upadhye S. Efficacy of intra- venous ketoprofen for pre-emptive analgesia. J Postgrad Med. 2002;48:109-12. Dexketoprofen has been shown to provide postoperative analgesia when given in IVRA, compared to giving it intravenously.77. Yurtlu S, Hanci V, Kargi E, Erdogan G, Kosal BG, Gul S, et al. The analgesic effect of dexketoprofen when added to lig- nocaine for intravenous regional anaesthesia: a prospective, randomized placebo controlled study. J Int Med Res. 2011;39:1923-31. Aim of this study is to compare ketoprofen with pethidine 30 mg as adjunct to lignocaine in IVRA.
Methods
After taking approval from the ethics committee of the institute and informed consent, 45 ASA grade I and II patients posted for elective forearm and hand surgeries were selected for a prospective, randomized, double blind study. All the patients were preoperatively evaluated and visual analogue score for pain was explained to them. The patients were premeditated with intravenous midazolam 1 mg, 10 min before the procedure. Routine monitoring included ECG, NIBP, and SpO2. A 20 G cannula was inserted and secured in a distal vein of the arm to be operated, over the dorsum of the hand. A double-cuffed tourniquet was applied over the arm. The arm was exsanguinated by elevation and application of Esmarch bandage. The proximal cuff of the tourniquet was inflated to the pressure of 300 mm Hg. Isolation of the limb from systemic circulation was confirmed by observing the arm for the absence of distended veins and confirming absence of radial pulse. The Esmarch bandage was removed and 40 mL of IVRA solution was injected through the venous cannula slowly over a period of 90 s.
The patients were randomly divided into three groups of 15 each, by closed envelope technique. They received either 40 mL of 0.5% lignocaine (Gr-L) or 40 mL of 0.5% lignocaine along with pethidine 30 mg (Gr-LP) or 40 mL of 0.5% lignocaine along with ketoprofen 100 mg (Gr-LK).
Pulse rate, blood pressure, and SpO2 were recorded every 5 min. Intra operative tourniquet pain was assessed every 15 min using visual analogue scale of 0-10. During intra operative period, for tourniquet pain (VAS > 3) 25 mcg of fentanyl was given intravenously. After deflation of cuff, pain was assessed using VAS scale at 0, 15, 30, 60, 120, 180, 240 and 360 min. For early postoperative pain up to 6 h, for VAS > 3, bolus dose of fentanyl 25 mcg was given intravenously. Time for first analgesic consumption and total number of fentanyl boluses consumed were noted.
After 6 h if the patient had pain, patient was asked to take oral tablet of diclofenac 50 mg. The patient was asked to take tablet of diclofenac 50 mg every 8th hour, if pain persisted. Total numbers of tablets taken in 24 h were noted by telephonic interview. Postoperative nausea and vomiting, pruritis, tinnitus and dizziness and respiratory depression (respiratory rate <10/min or SpO2 < 90%) were noted. Sedation was noted at 0, 30, 60 min after the deflation of tourniquet using a numerical scale (1 = completely awake, 2 = awake but drowsy, 3 = asleep but responsive to verbal commands, 4 = asleep but responsive to tactile stimulus, 5 = asleep and not responsive to any stimulus).
Data were analyzed using SPSS 11.0 statistical analysis software. Ordinal data such as demographic data, tourniquet time, surgical duration, haemodynamic parameters and number of diclofenac tablets consumed were compared using one-way ANOVA. If the difference was statistically significant, Schiff's post hoc analysis was performed. Number of patients needing fentanyl during intraoperative period and in the first 6 h of postoperative period and the side effects were compared using Chi-square test. Continuous data like intraoperative and postoperative pain scores and sedation scores within the groups were compared with Friedman rank test. The pain scores and sedation scores between the groups were compared using Kruskal-Wallis test. p value of <0.05 was considered statistically significant.
Results
One patient in the control group (Gr-L) and one in the pethidine group (Gr-LP) had patchy block and were given general anaesthesia. There were no differences among the groups in demographic variable, tourniquet time and surgical duration (Table 1). There was no difference between groups for haemodynamics parameters (heart rate, systolic and diastolic blood pressure).
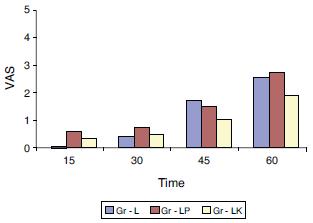
Within each group VAS scores increased progressively from 15 to 90 min (Fig. 1). In order to find out, when the tourniquet pain became significant, Friedman test (rank test) was ( Table 2) within each of these groups. Tourniquet pain increased significantly between 30 and 45 min in all the groups. The VAS scores were comparable between the groups during surgery. Fentanyl requirement for treatment of intra operative tourniquet pain was not significant between the groups.
Postoperative VAS scores were comparable between the groups. Time for the first dose of fentanyl consumption was significantly delayed in groups LP and LK compared to group L (156.7 ± 148.8 and 153.0 ± 106.0 vs. 52.1 ± 52.4 min respectively) (Fig. 2). Total fentanyl consumption in first 6 h of postoperative period (Fig. 3) was lesser in Gr-LP and Gr-LK compared to Gr L (37.5 ± 29.0 mcg, 38.3 ± 20.8 mcg vs. 64.2 ± 27.2 mcg respectively) (Table 3).
Number of diclofenac tablets consumed between 6 and 24 h was not significantly different between the groups (2.4 ± 0.7, 2.5 ± 0.5, 2.0 ± 0.7 in Gr-L, Gr-LP, Gr-LK respectively).
One patient in the control group, four patients in pethidine group and two patients in ketoprofen had tinnitus and dizziness. Only one patient in pethidine had postoperative nausea and vomiting and none of patients in control or ketoprofen had PONV. Two patients in ketoprofen group, but none in pethidine or control group had pruritus. None of these side effects were statistically significant between the groups. None of the patients in any group had significant respiratory depression. Sedation scores were not significantly different between the groups (mean scores of 1.2 ± 0.1, 1.1 ± 0.1, 1.4 ± 0.1 for groups L, LP and LK respectively) (Table 4).
Discussion
We found that the addition of pethidine or ketoprofen as adjuncts in IVRA provides significantly better postoperative analgesia in the first 6 h. However their efficacy postoperative analgesia is limited beyond 6 h. Addition of either of the adjuncts does not increase the tourniquet tolerance when compared to the control group.
At the site of surgical trauma there will be release of inflammatory mediators such as histamine, serotonin, bradykinins and metabolites of cycloxygenase and lipooxigenase pathways.88. Woolf CJ. Recent advances in pathophysiology of acute pain. Br J Anaesth. 1989;63:139-46. NSAIDs inhibit the production of prostaglandins from arachidonic acid in the phospholipid membrane.99. Foedt Weser J. Nonsteroidal anti-inflammatory drugs. New Eng J Med. 1980;302:1179-85. Pretreatment of the extremity with NSAIDs might be expected to interfere with the initiation of pain. By preventing the synthesis of mediators prior to surgical trauma, NSAIDs might minimize the activation of or sensitization of peripheral nociceptors. Although the concept of pre-emptive analgesia is controversial, evidence from the animal studies supports the theory that breaking the link between surgical trauma and primary or secondary hyperalgesia reduce both early and late postoperative pain.1010. Woolf CJ, Chang MS. Preemptive analgesia - treating post- operative pain by preventing the establishment of central sensitization. Anesth Analg. 1993;77:362-79. Ketoprofen is a NSAID agent available in intravenous preparation. It has proven efficacy in providing postoperative analgesia in tonsillectomy, thyroid and nasal surgeries.22. Basto ER, Waintrop C, Mourey FD, Landru JP, Eurin BJ, Jacob LP. Intravenous ketoprofen in thyroid and parathyroid surgery. Anesth Analg. 2001;92:1052-7. , 33. Tuomilehto H, Kokki H, Tuovinen K. Comparison of intravenous and oral ketoprofen for post operative pain after adenoidec- tomy in children. Br J Anaesth. 2000;85:224-7. , 44. Elhakim M. Comparison of intravenous ketoprofen with pethi- dine for postoperative pain relief following nasal surgery. Acta Anaesthesiol Scand. 1991;35:279-82. , 55. Subramaniam R, Ghai B, Khetarpal M, Subramanyam MS. A comparison of intravenous ketoprofen versus pethidine on peri-operative analgesia and post-operative nausea and vomiting in paediatric vitreoretinal surgery. J Postgrad Med. 2003;49:123-6. and 66. Priya V, Divatia JV, Sareen R, Upadhye S. Efficacy of intra- venous ketoprofen for pre-emptive analgesia. J Postgrad Med. 2002;48:109-12. The NSAIDs have already been shown to be of definitive advantage when used as adjuncts in IVRA. NSAIDs used in previous studies are ketorolac and tenoxicam.1111. Steinberg RB, Reuben SS, Gardener G. The dose-response relationship of ketorolac as a component of intravenous regional anesthesia with lignocaine. Anesth Analg. 1998;86:791-3. Lornaxicam when used as adjunct to lignocaine provided better analgesia compared to the control.1212. Sen1 S, Ugur B, Aydın ON, Ogurlu M, Gezer E, Savk O. The analgesic effect of lornoxicam when added to lido- caine for intravenous regional anaesthesia. Br J Anaesth. 2006;97:408-13. Similarly dexketoprofen as additive to lignocaine has been shown to provide good postoperative analgesia compared to giving the same drug intravenously or when compared to the placebo.77. Yurtlu S, Hanci V, Kargi E, Erdogan G, Kosal BG, Gul S, et al. The analgesic effect of dexketoprofen when added to lig- nocaine for intravenous regional anaesthesia: a prospective, randomized placebo controlled study. J Int Med Res. 2011;39:1923-31.
Peripheral action of opioids could be mediated by either peripheral opioid receptors or by local anaesthetic action of their own.1313. Stein C, Yassouridis A. Peripheral morphine analgesia. Pain. 1997;71:119-21 [editorial]. Many opioids (morphine, pethidine, fentanyl, tramadol, sufentanil and alfentanil) have been used as adjuncts in IVRA previously. Among these opioids, only pethidine in the dose above 30 mg has substantial postoperative benefits but at the expense of post deflation side effects.11. Choyce A, Peng P. A systemic review of adjuncts for intravenous regional anaesthesia for surgical procedures. Can J Anaesth. 2002;49:32-45.
There are no studies to compare pethidine of 30 mg dose to any of NSAIDs. So the aim of our study was to compare pethidine in a dose of 30 mg with a NSAID, ketoprofen with respect to efficacy and side effects.
Previous studies have suggested 30 mg as the optimal dose of pethidine as an adjuncts in IVRA.1414. Reuben S, Steinberg RB, Lurie SD, Gibson CS. A dose-response study of intravenous regional anesthesia with pethidine. Anesth Analg. 1999;88:831-5. Optimum dose of ketorolac for use as adjuncts in IVRA was determined as twenty milligrams.1111. Steinberg RB, Reuben SS, Gardener G. The dose-response relationship of ketorolac as a component of intravenous regional anesthesia with lignocaine. Anesth Analg. 1998;86:791-3. Since twenty milligrams of ketorolac is equipotent to 100 mg of ketoprofen, we used 100 mg of ketoprofen in our study.
In our study there was no significant difference in the intraoperative fentanyl consumption and intraoperative VAS scores for the tourniquet pain between the groups. In all the three groups the tourniquet pain increased significantly between 30 and 45 min period. This is in correlation with the other studies that suggest under regional anaesthesia tourniquet pain usually appears about 45 min after inflation and becomes more intense with time.1515. Terse T, Horlocker Wedel DJ. Anaesthesia for orthopaedic surgery. In: Barash PG, Cullen BF, Stoelting RK, editors. Clini- cal anaesthesia. Philadelphia: Lippincott Williams and Wilkins; 2001. p. 1114. Thus both of the adjuncts used in this present study do not delay or reduce the severity of intraoperative tourniquet pain compared to the control.
The analgesic consumption for treatment of early postoperative pain was significantly less in pethidine and ketoprofen group compared to control. The time for first analgesic requirement was also delayed when pethidine and ketoprofen were used as adjuncts when compared to the control. This signifies that pethidine and ketoprofen provide significantly better postoperative analgesia in the first 6 h. Both pethidine and ketoprofen are equally efficacious in providing postoperative analgesia, when used as adjuncts to lignocaine in IVRA.
Analgesic consumption was not significantly different between 6 and 24 h period after the surgery. Therefore addition of pethidine or ketoprofen is unlikely to provide significant analgesia beyond 6 h.
In our study there was no significant difference in the incidence of side effects between the three groups. The results are in contrast to high incidence of side effects in pethidine group in Scott Reuben's study.1414. Reuben S, Steinberg RB, Lurie SD, Gibson CS. A dose-response study of intravenous regional anesthesia with pethidine. Anesth Analg. 1999;88:831-5. Two of the forty-five patients had successful block in our study. Thus the success rate was 95.56%. This is close to 96-100% success rate described by other studies.1616. Brill S, Middleton W, Brill G, Fisher A. Bier's block; 100 years old and still going strong!. Acta Anaesthesiol Scand. 2004;48:117-22. , 1717. Brown EM, McGriff JT, Malinowski RW. Intravenous regional anaesthesia (Bier's block): review of 20 years experience. Can J Anaesth. 1989;36:307-10. and 1818. Hollingworth A, Wallace WA, Dabir R. Comparison of bupiva- caine and prilocaine used in Bier's block: a double blind trial. Injury. 1982;13:331.
Thus we conclude that addition of pethidine or ketoprofen as adjuncts in IVRA provides significantly better postoperative analgesia in the first 6 h. However their efficacy postoperative analgesia is limited beyond 6 h. Addition of either of the adjuncts does not increase the tourniquet tolerance when compared to the control group. Neither of these adjuncts increases the incidence of side effects compared to the control group.
We recommend the use of pethidine 30 mg or ketoprofen 100 mg as safe and effective adjuncts in IVRA.
References
-
1Choyce A, Peng P. A systemic review of adjuncts for intravenous regional anaesthesia for surgical procedures. Can J Anaesth. 2002;49:32-45.
-
2Basto ER, Waintrop C, Mourey FD, Landru JP, Eurin BJ, Jacob LP. Intravenous ketoprofen in thyroid and parathyroid surgery. Anesth Analg. 2001;92:1052-7.
-
3Tuomilehto H, Kokki H, Tuovinen K. Comparison of intravenous and oral ketoprofen for post operative pain after adenoidec- tomy in children. Br J Anaesth. 2000;85:224-7.
-
4Elhakim M. Comparison of intravenous ketoprofen with pethi- dine for postoperative pain relief following nasal surgery. Acta Anaesthesiol Scand. 1991;35:279-82.
-
5Subramaniam R, Ghai B, Khetarpal M, Subramanyam MS. A comparison of intravenous ketoprofen versus pethidine on peri-operative analgesia and post-operative nausea and vomiting in paediatric vitreoretinal surgery. J Postgrad Med. 2003;49:123-6.
-
6Priya V, Divatia JV, Sareen R, Upadhye S. Efficacy of intra- venous ketoprofen for pre-emptive analgesia. J Postgrad Med. 2002;48:109-12.
-
7Yurtlu S, Hanci V, Kargi E, Erdogan G, Kosal BG, Gul S, et al. The analgesic effect of dexketoprofen when added to lig- nocaine for intravenous regional anaesthesia: a prospective, randomized placebo controlled study. J Int Med Res. 2011;39:1923-31.
-
8Woolf CJ. Recent advances in pathophysiology of acute pain. Br J Anaesth. 1989;63:139-46.
-
9Foedt Weser J. Nonsteroidal anti-inflammatory drugs. New Eng J Med. 1980;302:1179-85.
-
10Woolf CJ, Chang MS. Preemptive analgesia - treating post- operative pain by preventing the establishment of central sensitization. Anesth Analg. 1993;77:362-79.
-
11Steinberg RB, Reuben SS, Gardener G. The dose-response relationship of ketorolac as a component of intravenous regional anesthesia with lignocaine. Anesth Analg. 1998;86:791-3.
-
12Sen1 S, Ugur B, Aydın ON, Ogurlu M, Gezer E, Savk O. The analgesic effect of lornoxicam when added to lido- caine for intravenous regional anaesthesia. Br J Anaesth. 2006;97:408-13.
-
13Stein C, Yassouridis A. Peripheral morphine analgesia. Pain. 1997;71:119-21 [editorial].
-
14Reuben S, Steinberg RB, Lurie SD, Gibson CS. A dose-response study of intravenous regional anesthesia with pethidine. Anesth Analg. 1999;88:831-5.
-
15Terse T, Horlocker Wedel DJ. Anaesthesia for orthopaedic surgery. In: Barash PG, Cullen BF, Stoelting RK, editors. Clini- cal anaesthesia. Philadelphia: Lippincott Williams and Wilkins; 2001. p. 1114.
-
16Brill S, Middleton W, Brill G, Fisher A. Bier's block; 100 years old and still going strong!. Acta Anaesthesiol Scand. 2004;48:117-22.
-
17Brown EM, McGriff JT, Malinowski RW. Intravenous regional anaesthesia (Bier's block): review of 20 years experience. Can J Anaesth. 1989;36:307-10.
-
18Hollingworth A, Wallace WA, Dabir R. Comparison of bupiva- caine and prilocaine used in Bier's block: a double blind trial. Injury. 1982;13:331.
-
☆
This work was conducted in the Department of Anesthesiology and Critical Care, All India Institute of Medical Sciences, New Delhi, India.
-
☆☆
This article was presented as poster in International Congress on Regional Anaesthesia and Pain Medicine, New Delhi, February 20-22, 2004.
Publication Dates
-
Publication in this collection
Jul-Aug 2014
History
-
Received
15 May 2012 -
Accepted
20 Mar 2013