Abstract
Electrosurgery is a technology developed over the last few years and has become a very important tool in modern surgery. Most of the equipment is considered safe, although there are risks related to its use. Several lesions may be caused by electrocautery, and burns are the most common and feared. We report two cases of burns related to use of electrocautery and promote a literature review, because knowledge of electrosurgery fundamentals, its correct use, the choice of a safety device, constant monitoring, and immediate investigation before any suspicions surely can improve the operational experience for both surgeon and patient.
KEYWORDS
Complications: burn; Equipment: electrocautery; Surgery: complications
Resumo
A eletrocirurgia é uma tecnologia que se desenvolveu muitos nos últimos anos e se tornou um instrumento de grande importância na cirurgia moderna. A maioria dos equipamentos é considerada segura, embora existam riscos relacionados ao seu uso. Várias lesões podem ser causadas por eletrocautérios, as queimaduras são as mais frequentes e temidas. Relatamos dois casos de queimaduras relacionadas ao uso do bisturi elétrico e promovemos uma revisão de literatura, pois o conhecimento dos fundamentos da eletrocirurgia, seu uso correto, a escolha de um equipamento seguro, o monitoramento constante e a investigação imediata diante de quaisquer suspeitas com certeza podem melhorar a experiência operacional para ambos, cirurgião e paciente.
Palavras-chave
Complicações: queimadura; Equipamento: eletrocautério; Cirurgia: complicações
Introduction
Electricity is a phenomenon that has been used for many years in operating rooms and its current use during surgery is an intrinsic characteristic of modern surgery. Historically, its use in medicine dates back to the 1920s, when Bovie developed an extremely modern instrument for the time, helped to bring it to the forefront of surgical procedures and revolutionized surgery.11 Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Col Surg. 2006;202:520-30.
2 Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63.-33 Wang K, Advincula AV. Current thoughts in electrosurgery. Int J Gynecol Obstet. 2007;97:245-50. In practical terms, electricity can be used in surgery by means of electrosurgery, also called diathermy, or electrocautery. In the latter, the oldest, the electric current is used to heat filament at the cautery tip, returns by the same route, bypasses the patient. The heat is transmitted directly to tissues in order to obtain therapeutic effects.11 Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Col Surg. 2006;202:520-30.
2 Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63.-33 Wang K, Advincula AV. Current thoughts in electrosurgery. Int J Gynecol Obstet. 2007;97:245-50. In electrosurgery, the most widely used method currently, the electrical current is produced by a generator and reaches the patient's body by an active electrode, acts in target tissues, and exits through a neutral electrode. When this electrical current meets the human tissue resistance, it turns into heat and determines the therapeutic effects, known as cutting or coagulation. The active electrode tip does not undergo heating. When the neutral electrode (pad format) is away from the active electrode, there is the monopolar system. When the positive and neutral electrodes are separated by a small distance and limit the flow of electric current, there is the bipolar system.11 Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Col Surg. 2006;202:520-30.
2 Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63.-33 Wang K, Advincula AV. Current thoughts in electrosurgery. Int J Gynecol Obstet. 2007;97:245-50. However, even with long experience in the use of electrosurgery, the risks and complications are still present despite the incorporation of various security measures. There was an increase in the number of injuries and related complications, such as interference with monitoring devices,44 Finlay B, Couchie D, Boyer L. Electrosurgery burns resulting from use of miniature ECG electrodes. Anesthesiology. 1974;47:263-9. pacemakers and other cardiac devices, pulse oximeter probes,55 Bisinotto FMB, Abud TMV, Alves Neto J, et al. Queimadura provocada por bisturi elétrico associado ao oxímetro de pulso. Relato de caso. Rev Bras Anestesiol. 1996;46:133-5. temperature sensors, deep brain stimulation electrodes,66 Roark C, Whicher S, Abosch A. Reversible neurological symptoms caused by diathermy in a patient with deep brain stimulators: case report. Neurosurgery. 2008;62:E256. and, above all, burns. Moreover, other phenomena may be associated, such as stimulation of excitable tissues, leg movement during urological surgery by stimulation of the obturator nerve or direct stimulation of the muscles, causing muscle contractions that can be misinterpreted as inadequate anesthesia, in addition to the potential risk of combustion due to the presence of anesthetic gases.77 Haddad R, Pereira DE, Lima CE, et al. Fogo em via aérea durante traqueostomia eletiva. Pulmão. 2006;15:52-4.,88 Practice advisory for the perioperative management of patients with cardiac implantable electronic devices: pacemakers and implantable cardioverter-defibrillators an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Implantable Electronic Devices. Anesthesiology. 2011;114:247-61. Despite all the advances in electrosurgery, even with its inherent risks, most surgeons and residents have no formal training for its proper use. The aim of this study is to present two cases of burns related to the use of electrosurgery and use them to promote discussion. Noteworthy, these complications are predictable and preventable; nevertheless, they still haunt the operating rooms.
Clinical case 1
Newborn, 11 days old, preterm weighing 2 kg, diagnosed with obstructive acute abdomen. Emergency laparotomy was indicated and performed under general anesthesia. The patient was monitored with cardioscope, pulse oximetry, noninvasive blood pressure, and blood gas analysis during the intraoperative period. Monopolar electrosurgery was used with reusable dispersive pad, which was placed in the left plantar region by the surgeon in charge. At the end of surgery, after removing the surgical drapes, a third degree burn was found on the site of the dispersive pad (Fig. 1).
Clinical case 2
Male patient, 30 years old, physical status ASA II due to smoking, reported a prior history of ureterolithiasis. Had undergone implantation of double-J catheter few months before and was scheduled for its withdrawal endoscopically. After standard monitoring, subarachnoid anesthesia was induced by a first year resident, with supervision. T10 sensory level was achieved, and the patient was placed in the lithotomy position. However, due to the long-term catheterization, the catheter withdrawal was not possible as scheduled by the surgical team and there was the need for abdominal approach through suprapubic incision. The patient was then repositioned on the surgical table to a supine position. Monopolar electrosurgery was used, with a disposable dispersive pad placed on the back of the patient. During the intraoperative period, the patient complained of pain in the left side of his back, which was not investigated by the anesthesiology resident. The patient was taken to the post-anesthesia recovery room and was discharged the next day-there were no complaints reported in the hospital records. A month after the incident, he went to the Anesthesiology Clinic for a consultation on further urological procedure and, during the anamnesis, reported the occurrence of burn on his left flank during the procedure previously mentioned. Upon analyzing the injury shape, it was found a similarity with the contact metals of the operating table (Fig. 2). Thus, it was concluded that the burn was caused by direct contact of the patient with the table metallic part. The patient was referred to the plastic surgery department of the institution for clinical management.
Burning in the flank region (left); and surgical table exposing the metal parts coincident with the burning formats (arrows).
Discussion
Although the use of electricity in surgery is highly useful and effective, the risk of complications exists. From the 1970s to the 1990s, the incidence of complications related to electrosurgery remained at about 2-5 per 1000 surgeries, with predominance of electrical burns.11 Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Col Surg. 2006;202:520-30.,99 Demircin S, Aslan F, Karagoz YM, et al. Medicolegal aspects of surgical diathermy burns: a case report and review of the literature. Rom J Leg Med. 2013;21:173-6. These burns are not always detected immediately after surgery, as occurred in Case 2, with a late diagnosis. Jones et al.22 Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63. suggest that one should bear in mind that the depth of thermal energy penetration goes beyond what can be seen with the naked eye. Thus, unrecognized injuries may be seen later, after progression of tissue damage. Furthermore, such injuries may not be recognized as burns, but be misdiagnosed as bedsores, toxic or allergic reactions to aseptic or disinfection solutions. The circumstances in which the general burns occur represent another key factor because many people are involved in the preparation and use of the electrosurgical unit.99 Demircin S, Aslan F, Karagoz YM, et al. Medicolegal aspects of surgical diathermy burns: a case report and review of the literature. Rom J Leg Med. 2013;21:173-6.,1010 Vedovato JW, Pólvora VP, Leonardi DF. Burns as a complication of the use of diatermy. J Burn Care Rehabil. 2004;25:120-3. All this makes the exact incidence of complications related to the use of electrosurgery difficult to be measured. However, this type of injury is still a significant percentage of morbidity associated with surgery. In Closed claims’ American analysis,1111 Metzner J, Posner KL, Lam MS, et al. Closed claims’ analysis. Best Pract & Res Clin Anaesth. 2011;25:263-76. burns in patients from fires in the operating rooms account for about one-fifth of legal cases. In all cases, the electrosurgical unit and supplemental oxygen were used. It is important to understand that such unity is almost always the ignition source for the occurrence of fires; it is one of the three components related to its occurrence, next to oxygen, which acts as combustible, and drapes and/or alcoholic solutions, which function as a fuel. In Case 2, it was not possible to establish whether or not the burn resulted from the excessive amount of antiseptic used in the surgical site or if it was blood, urine, or other liquid solutions used in the procedure that dampened the patient's skin. Considering the lesion feature and similar format to the table metal parts (Fig. 2), it is suspected that there was direct contact of the patient with a metal part of the operating table, which might have caused an alternative exit route for electric current, and thus the heat was concentrated in a small area and caused the burn.
Principles of electrosurgery
A basic knowledge of electricity is required to use electrosurgical technology in operating rooms for patient care.11 Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Col Surg. 2006;202:520-30.
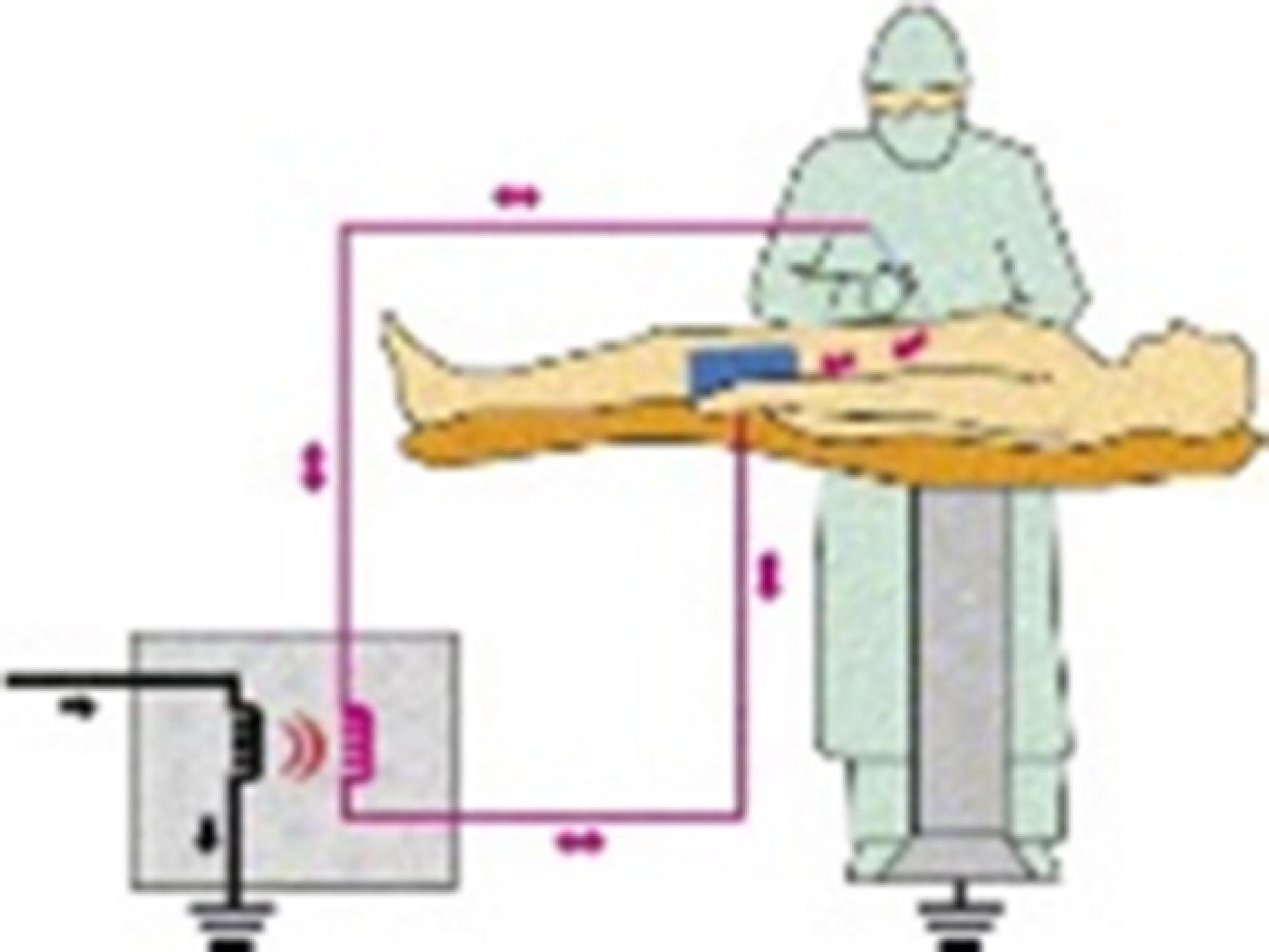
2 Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63.-33 Wang K, Advincula AV. Current thoughts in electrosurgery. Int J Gynecol Obstet. 2007;97:245-50.,1212 Hay DJ. Electrosurgery. Surgery. 2007;26:66-9. Atoms are composed of protons, neutrons, and electrons. Electric current flows as electrons move from one atom to another through an adjacent circuit. Voltage is the force that drives the movement of electrons; it is the current driving force against the circuit resistance. When electrons encounter this resistance, there is heat. And for current to flow, a continuous circuit is needed. Electricity has three basic principles22 Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63.: (1) It always follows the path of least resistance; (2) it always tries to return to a reservoir of electrons, such as ground; and (3) there should always be a complete circuit. Much of the understanding of how electrosurgery works, as well as the complications related, is based on these principles.33 Wang K, Advincula AV. Current thoughts in electrosurgery. Int J Gynecol Obstet. 2007;97:245-50. In the operating room, the circuit is composed of the electrosurgical unit and the patient and the active and return electrodes. The principle of electrosurgery is based on the passage of high frequency electrical current through target tissues to achieve a desired clinical effect. Voltage is supplied by the generator, which from the common alternating current of low frequency (60 Hz) generates electric currents of very high frequencies (0.4-3 MHz) and high voltage (400-500 V). The current released through an active electrode goes through the patient's body, whose tissues determine the resistance (impedance) to the current flow. At the end of the circuit, the current flows out of a neutral electrode, which is the dispersing pad or neutral electrode, and returns to the electrosurgical unit,22 Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63.,1313 Van Way CW, Hinrichs CS. Technology focus: electrosurgery 201: basic electrical principles. Curr Surg. 2000;57:261-4. forms a single circuit, without need for grounding (Fig. 3).
Isolated circuit: the power released through the active electrode travels through the patient's body, exits through the neutral electrode, and returns to the electrosurgical unit.
Heat generation is described by Joule's Law, which is expressed by the equation:
Q = I2 × t × R
in which the heat produced (Q) increases proportionally with the square of the current intensity (I), with the duration of exposure to the current (t) and tissue resistance (R).
Thus, by the exposed formula, the effects determined by the electrosurgical unit, as well as the causes of complications related to its use, are understood. Heat promotes coagulation, cutting or fulguration depends on the current intensity (I), exposed surface, tissue resistance (conductivity), and exposure time.1414 Waldron RP, Copeland GP, Murphy AF. Surgical diathermy: a potential hazard. Br J Clin Pract. 1984;38:283.,1515 Afonso CT, Silva AL, Fabrini DS, et al. Risco do uso de eletrocautério em pacientes portadores de adornos metálicos. ABCD Arq Bras Cir Dig. 2010;28:183-6. On the side of the electrode (cautery tip), the rate at which tissues are heated plays a crucial role in determining the clinical effect. When an oscillating current is applied to the tissue, the rapid movement of electrons through cell cytoplasm increases intracellular temperature. The amount of released thermal energy and the time fraction in which this occurs will determine the effects on tissues. Thus, cell damage is reversible when temperatures are lower than 45 °C, but when temperatures reach over 45 °C, cell proteins start to denature and there is loss of cell integrity. Tissue fluid evaporates and dries at temperatures above 90 °C and other tissue solid components are reduced to carbon when the tissue temperature reaches 200 °C. Temperature can increase markedly, exceeding 1000 °C. Besides the heating effect, living tissues are affected in other ways, particularly the depolarization of cells from cell membrane due to disruption of cellular function. This can lead to neuromuscular stimulation, abnormal conduction, myocardial fibrillation, and death.1212 Hay DJ. Electrosurgery. Surgery. 2007;26:66-9. Current intensity (I)-defined as the amount of electricity flowing through a tissue area-is the most important concept to understand electrosurgery, as the tissue exposed to the highest intensity undergoes greater thermal effects. The dispersion plate placement site is directly related to the current intensity. For example, if the plate is placed near the surgical site, less energy is lost in the circuit and thus lower current densities are necessary to achieve the desired tissue effects. On the other hand, if the plate is placed further away from the surgical site, a greater amount of energy is lost due to the body's resistance, which requires higher density, and there is the possibility of exposing the patient to increased risk of injury.1414 Waldron RP, Copeland GP, Murphy AF. Surgical diathermy: a potential hazard. Br J Clin Pract. 1984;38:283.
15 Afonso CT, Silva AL, Fabrini DS, et al. Risco do uso de eletrocautério em pacientes portadores de adornos metálicos. ABCD Arq Bras Cir Dig. 2010;28:183-6.-1616 Gomide LC, Santos CERG, Pereira CJ, et al. Queimadura de terceiro grau no local da placa eletrocirúrgica durante artroscopia de ombro: relato de caso. Rev Bras Ortop. 2011;46:91-3. The time of exposure (t) to the electric current plays an obvious role in the extension of the effects of its passage through the human body. The duration of exposure to current is directly related to the heat produced in the tissue. The longer the exposure time, the greater the effect and the risk of injury due to the greater potential for heat propagation to adjacent tissues. A prolonged activation will produce broader and deeper tissue damage. Other relevant factor is the target tissue resistance (R), as the greater the resistance to the electric current, the greater the amount of heat produced. The higher this inherent resistance, then higher will be the voltage required for the current passage. Also, the more superficial tissues are cauterized, the less they become electrically conductive, which increases its strength and requires a greater amount of voltage for current to penetrate into deeper tissue layers. Conductive materials, such as metal, soil, ionic solutions, and the human body are those that offer least resistance. The tissue specific resistance depends on the type of tissue concerned, humidity and thickness of the skin, presence of bony protuberances, and vascularization. Various tissue types have different electrical resistances that affect the rate of heat. The resistance of fat and bone tissue is greater than the skin, muscle tissue, and well vascularized areas. This is important in selecting a location to place the dispersive plate; areas with more vascularized tissues and muscles should be preferred, avoid fat regions, bony prominences, and thick skin such as the plantar region. In Case I, besides the plate inadequacy, it was placed in a region with great resistance that allows the passage of electrical current, as the plantar area, which in addition to having a thicker skin it may facilitate contact with bony prominences. Resistance is also important to understand Case 2. The conductive materials (low resistance), such as the surgical table metal part, in addition to patient's metallic ornaments, can offer an optional route for the electrical current to exit from the patient's body. In Case 2, the patient's body came in contact with the operating table metal part (Fig. 2), which has become an optional rout to the electric current exit, resulting in great heat and burning. This same mechanism explains the burning cases of patients with metal ornaments, with ECG and EEG electrodes, and other internal monitoring devices using needles. Understanding it is also important to explain to the patient the mandatory removal of all conductive (low resistance) materials, such as jewellery, ear rings, piercings, clasps, buttons, and other metal adornments.1515 Afonso CT, Silva AL, Fabrini DS, et al. Risco do uso de eletrocautério em pacientes portadores de adornos metálicos. ABCD Arq Bras Cir Dig. 2010;28:183-6. The effect of electrosurgery also depends on the type of electrode. Smaller electrodes promote a higher current intensity and concentrate the heat effect on the contact site. For example, a needle tip electrode provides a greater heat effect compared to a ball tip electrode. This same concept applies to the return electrode.11 Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Col Surg. 2006;202:520-30.
Electrosurgical units
Currently, electrocautery, thermocautery, diathermy, electric and electronic scalpels are terms used interchangeably in reference to electrosurgery. Most authors agree that the generic term electrosurgical unit is the most appropriate regarding the current generator used for electrosurgery.11 Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Col Surg. 2006;202:520-30.,22 Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63. There are two types of electrosurgical units: generators called "ground referenced", which were used until 1970, and the latest, which are isolated. In the first type, the electrical current goes through the patient and then earth ground completes the circuit through a dispersive plate attached to the patient. In the absence of a complete circuit, the current will seek the earth (grounding). In this situation, any contact of the patient with a possible grounding, the current will choose the path of least resistance, may pass through the operating table, ECG electrodes or metal of a venous catheter in contact with the patient. If the current intensity is high enough at the contact point, there is the possibility of burning. This potential danger has been eliminated with the introduction of generators isolated from ground, in which the current passes through the patient and returns to the generator through the dispersive plate. The optional paths are avoided because there is no connection of the return electrode with the ground. The current flow is limited between the patient's active electrode and return electrode, which provides a low resistance path for the current coming from patient to return to the generator (Fig. 3).11 Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Col Surg. 2006;202:520-30.,33 Wang K, Advincula AV. Current thoughts in electrosurgery. Int J Gynecol Obstet. 2007;97:245-50.,1717 Odell RG. Electrosurgery: principles and safety issues. Clin Obstet Gynecol. 1995;38:610-21. The electrosurgical unit activation is mediated by the hands or feet. This isolated generator system has reduced significantly the cases of burns, but did not eliminate entirely the possibility of this complication.22 Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63.
Electrosurgical modalities
Generators can apply monopolar or bipolar energy. In monopolar mode, the current released passes from the generator to the active electrode, in which its effect is produced, passes through the patient and exits through the dispersive electrode (or neutral plate), returns to the generator and forms a complete circuit. Because the neutral electrode surface is much larger than that of the active electrode (on which the cutting, coagulation or ablation takes place), the current is spread over a large area, which minimizes the heating of tissue in contact with the dispersive plate. It is most often used due to its greater versatility. However, it offers more risk because larger amounts of tissue are exposed to electricity. In the bipolar mode, the instruments resemble surgical tweezers and there is no need for a dispersive return electrode, as both the active and return electrodes are integrated in order to release energy and promote its return. The energy does not travel through the patient because it is confined to the tissue between the forceps. Because of this configuration, the bipolar mode offers little chance of an unintended dispersal of current. The power generated by bipolar scalpel is smaller compared to the monopolar. It is indicated for delicate surgeries such as neurosurgery.
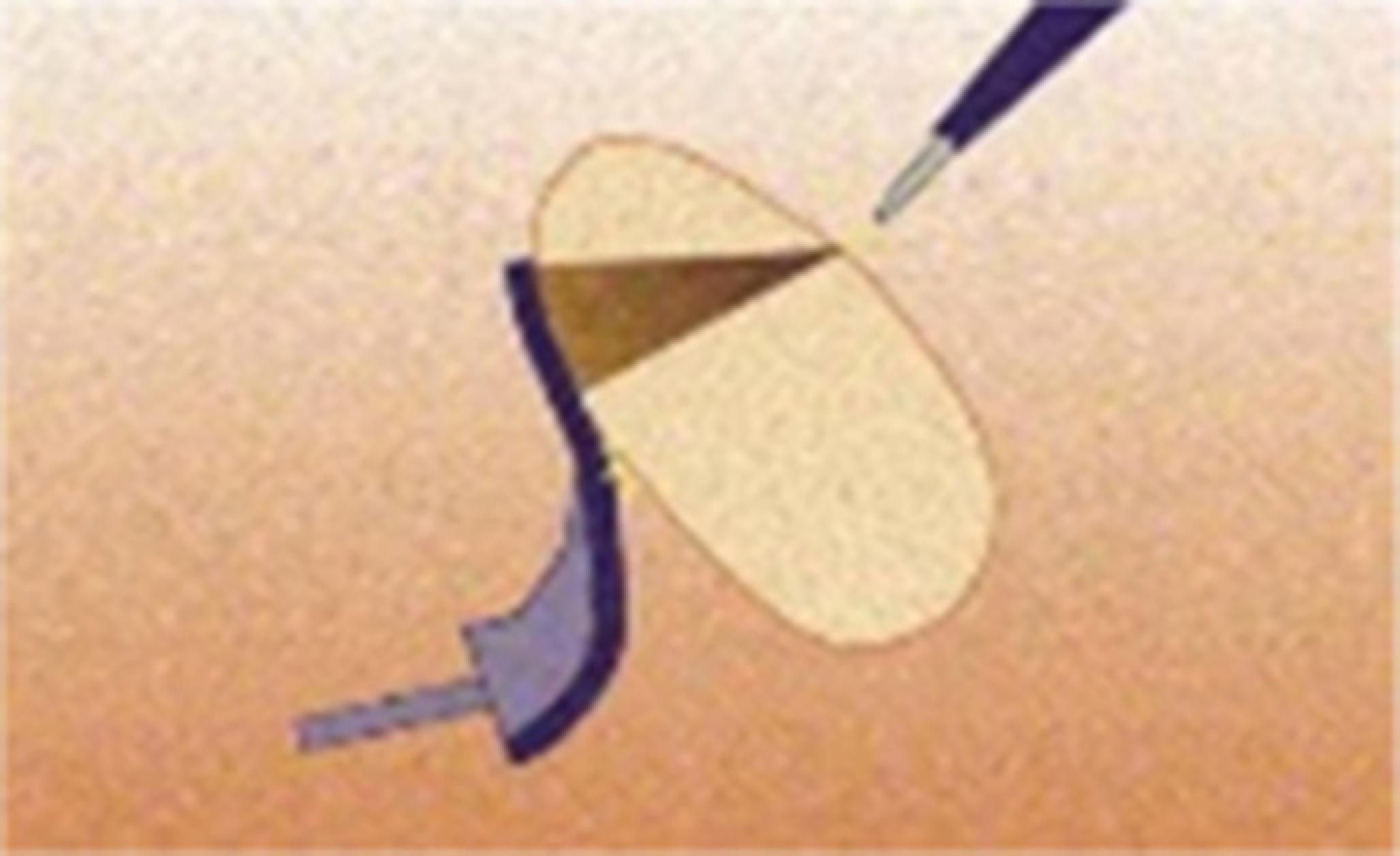
Dispersive plate or neutral electrode
Various types of dispersive plate or neutral electrode are available, such as the single-use disposable and reusable adhesives. Such plates should be of sufficient size to maintain a wide area of electricity dispersion, in order not to cause tissue damage. The surface varies from 60 cm2 for children to 170-180 cm2 for adults, depending upon the supplier. The output power is limited to 150 and 400 W for children and adults, respectively. Moreover, gels or pastes should be used to increase contact between plate and skin and reduce its resistance. If the plate is not completely attached (Fig. 4), or any kind of fluid is accumulate between the plate and the skin, the total area of dispersion becomes smaller, providing more risks. It is also necessary to select the location, as well as the plate correct placement. It should not be placed in scar tissue, bony prominences, metal implants, and fat regions of the body.1010 Vedovato JW, Pólvora VP, Leonardi DF. Burns as a complication of the use of diatermy. J Burn Care Rehabil. 2004;25:120-3. Skin preparation for dispersive plate placement includes a gentle cleaning of the area to remove any trace of fat (without using alcohol, as this may cause increased skin resistance) and hair removal. It is necessary to wait until any combustible cleaning agent used evaporates. When an adhesive grounding plate is fully adhered to the patient's skin, there is adequate area sufficient for current intensity dispersal, which subsequently returns to the generator.
Causes of burns
Especially for monopolar mode, there are four basic causes of burns. The first refers to burn on surgical site itself as a result of inadvertent activation or inappropriate use. Exposure to electric current for long periods without interruption has direct association with the intensity of its effects and risk of injury. The second relates to the heating of solutions that results in thermal injury. Such injuries can be attributed to heated solutions by both the active and neutral electrodes. The third relates to thermal trauma in the dispersive plate region, also called return tissue damage. It happens when there is inappropriate contact between the plate and the skin of the patient (Fig. 4), or when the plate size and positioning site are inadequate, scatter energy in a smaller area, increasing the heat at the points of contact with the plate and causes burn (injury mechanism of the first reported case). A condition often relegated to the background is tissue hypoperfusion. Typically, there is no injury at the dispersive plate site because the contact area is large and skin blood circulation dissipates the heat generated at the site. However, in situations where tissue perfusion at the plaque site becomes inadequate (shock, hypotension, hypothermia, tissue compression at the plate area), the lack of adequate heat dissipation can cause injury. In an effort to reduce burns, since 1981 the devices have a safety system to ensure that the generator operates only if the dispersion plate is attached. Finally, the fourth cause relates to burns that can also occur when the current takes a path through the patient's body other than the dispersive electrode. The partial or total interruption of the dispersive plate contact with the electrosurgical unit allows the flow of electric current through optional routes, including all the contact points of the patient's body to the ground potential. Among the most common optional routes, there are:
-
Body surface in direct contact with the grounded operating table;
-
Electrodes attached to the patient which enable contact with the ground potential (i.e., monitoring electrodes);
-
Patient contact with conductive materials, plastic or rubber (tubes or mattresses), for static dissipation.
If the contact surface at these sites is small (high electrical resistance), there will be a large concentration of current, increased temperature, and tissue damage, often severe. In Case 2, the table metal parts in contact with the patient's skin worked as optional routes for the passage of electric current. Noteworthy in this case is the underestimation of the patient's complaint, who was able to refer pain in the area of the burn that was not included in the level obtained by anesthesia, but his complaint was dismissed by the team that probably related the patient's reaction to the effect of sedatives. Monitoring electrodes may cause injury even with the proper functioning of the neutral plate. When the dispersive plate is positioned at a point too distant from the active electrode action site, the electric current from it can be divided into two parts. One returns to the dispersive plate and the other returns through the monitoring electrode. Due to the reduced area of this electrode, burns occur in the skin of the patient. Several studies in the literature report the occurrence of burns related to ECG, EEG, rectal temperature probes or skin electrodes and internal monitoring devices using needles. The electric current circulation through optional routes other than the diathermy circuit may also involve:
-
Electrocution (electric shock): passage of electrical current through the body. Its consequences include shock-like sensation, burn, nerve injury, asphyxia (paralysis of respiratory muscles and respiratory centers), and others. Low frequency currents (60 Hz) can cause serious problems in excitable tissues, such as contraction of large muscle groups, which can be misinterpreted as intraoperative awakening of the patient and serious cardiac arrhythmias;
-
Electromagnetic interferences: the alternating electrical current, particularly of high frequency, generates a magnetic field that can produce interference in the functioning of other equipment (artifacts or noise in the pulse oximeter and cardioscope, for example). The best way to prevent this event is the use of proper grounding and electromagnetic isolation devices;
-
Fires and explosions: the production of an electric spark in a rich environment of flammable gases and vapors can produce catastrophic accidents. Flammable materials (gauze or dry swabs, alcohol solutions for antisepsis, PVC endotracheal tube), in the presence of rich atmospheres with combustible gases, such as oxygen, may enter into rapid combustion with a single electric spark.
Burn injury related to capacitance and magnetic induction phenomena are rare events. Both the first and the second are able to induce currents in conductive means (monitor cables connected to a patient, which function as "antennas") and may occur during use of an electrosurgical unit, which generates an extremely high-frequency alternating current, thus representing a further risk to a patient integrity. To avoid this type of accident, the unit should be placed as far as possible from monitors and wiring must be positioned perpendicular to each other.
Guidelines for the use of electrosurgical unit
Some recommendations regarding the use of electrosurgery are established to reduce the risks related to this technology application, serving as preventive measures to be taken by all professionals working in the operating room:
-
The key point in preventing accidents with the use of electrosurgery is the correct positioning of the patient on the operating table. The contact with metal parts of the patient or the table and monitoring electrodes can concentrate the electric current or cause its leakage and result in injury. Insulating devices in the table and in the arm/leg rests must be used to prevent current leakage through the metal areas, in addition to dry swabs placed between the arms, torso or legs to avoid current concentration in areas with fluid accumulation.
-
Removal of metallic ornaments is mandatory, and electrodes should be placed as far as possible from the surgical site.
-
When using the monopolar scalpel in patients with prosthetic conductive joints, every effort to place the prosthesis out of the direct path of the circuit should be made. If the patient has a right hip prosthesis, for example, the return plate should be placed on the left side of the patient.
-
The warning systems should always be working. The device sound indicator volume should be kept in audible level to signal immediately when the electrosurgical unit is inadvertently activated or when it is not working properly.
-
One should also avoid placing the dispersive electrode on tattoos, many of which contain metallic dyes. The active electrode should be placed away from the site when not in use; it avoids unintended activation and injuries.
-
Active electrodes should not be used in the presence of anesthetic gases and flammable agents, such as antiseptics for skin antisepsis. This is particularly important in ENT and head and neck surgeries, due to proximity to anesthetic gases.
-
The electrosurgical unit power should be confirmed prior to activation, which should be the lower and most effective possible, in order to achieve the desired effect for cutting or coagulation. If the surgeon requests continuous increase of power, or if there is unusual response from the patient, or if there is interference with the monitoring signal during its use, it is necessary to investigate the entire circuit for failures.
-
The dispersive plate location is generally dictated by the surgical site, it should be positioned as close as possible to the operative field, preferably in a clean, dry skin, placed in a well vascularized area and with greater muscle mass.
-
Patients with pacemaker should be continuously monitored because, although modern devices are designed to be protected from the current flow, they are still subject to interference and may be damaged beyond repair or have its function altered. Additional precautions should be taken to minimize accidents, such as checking the pacemaker proper function with the cardiologist during the use of electrosurgery, having a pacemaker programming unit available to set it in asynchronous mode, having a defibrillator on hand to immediate use in case of emergencies, keeping all the electrosurgical unit cables and wires away from the pacemaker and its connections and the generator power setting as low as possible. It is also recommended that bipolar electrosurgery should be used whenever possible, but, if necessary, the use of monopolar electrosurgery must ensure that the distance between the active and dispersive electrodes is as short as possible.
Conclusion
The entire perioperative period present risks to the patient, from the moment he enters the operating theatre to his return to the unit of origin, and electrosurgery is one of those risks. Knowledge of scientific and physical principles of electrosurgical units should be aimed at all those involved in the surgical setting, not only to increase efficiency and allow the use of all useful features of the devices, but also to prevent its misuse and damage to patients.
References
-
1Massarweh NN, Cosgriff N, Slakey DP. Electrosurgery: history, principles, and current and future uses. J Am Col Surg. 2006;202:520-30.
-
2Jones CM, Pierre KB, Nicoud IB, et al. Electrosurgery. Curr Surg. 2006;63:458-63.
-
3Wang K, Advincula AV. Current thoughts in electrosurgery. Int J Gynecol Obstet. 2007;97:245-50.
-
4Finlay B, Couchie D, Boyer L. Electrosurgery burns resulting from use of miniature ECG electrodes. Anesthesiology. 1974;47:263-9.
-
5Bisinotto FMB, Abud TMV, Alves Neto J, et al. Queimadura provocada por bisturi elétrico associado ao oxímetro de pulso. Relato de caso. Rev Bras Anestesiol. 1996;46:133-5.
-
6Roark C, Whicher S, Abosch A. Reversible neurological symptoms caused by diathermy in a patient with deep brain stimulators: case report. Neurosurgery. 2008;62:E256.
-
7Haddad R, Pereira DE, Lima CE, et al. Fogo em via aérea durante traqueostomia eletiva. Pulmão. 2006;15:52-4.
-
8Practice advisory for the perioperative management of patients with cardiac implantable electronic devices: pacemakers and implantable cardioverter-defibrillators an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Implantable Electronic Devices. Anesthesiology. 2011;114:247-61.
-
9Demircin S, Aslan F, Karagoz YM, et al. Medicolegal aspects of surgical diathermy burns: a case report and review of the literature. Rom J Leg Med. 2013;21:173-6.
-
10Vedovato JW, Pólvora VP, Leonardi DF. Burns as a complication of the use of diatermy. J Burn Care Rehabil. 2004;25:120-3.
-
11Metzner J, Posner KL, Lam MS, et al. Closed claims’ analysis. Best Pract & Res Clin Anaesth. 2011;25:263-76.
-
12Hay DJ. Electrosurgery. Surgery. 2007;26:66-9.
-
13Van Way CW, Hinrichs CS. Technology focus: electrosurgery 201: basic electrical principles. Curr Surg. 2000;57:261-4.
-
14Waldron RP, Copeland GP, Murphy AF. Surgical diathermy: a potential hazard. Br J Clin Pract. 1984;38:283.
-
15Afonso CT, Silva AL, Fabrini DS, et al. Risco do uso de eletrocautério em pacientes portadores de adornos metálicos. ABCD Arq Bras Cir Dig. 2010;28:183-6.
-
16Gomide LC, Santos CERG, Pereira CJ, et al. Queimadura de terceiro grau no local da placa eletrocirúrgica durante artroscopia de ombro: relato de caso. Rev Bras Ortop. 2011;46:91-3.
-
17Odell RG. Electrosurgery: principles and safety issues. Clin Obstet Gynecol. 1995;38:610-21.
Publication Dates
-
Publication in this collection
Sep-Oct 2017
History
-
Received
7 Aug 2015 -
Accepted
31 Aug 2015