Abstract
According to the most recent guidelines, the use of intraoperative transesophageal echocardiography in valvular surgeries is well established, as well as its use in the diagnosis, management, and rescue of perioperative complications. The aim of this case report is to illustrate a condition in which its intraoperative use had a positive influence on the outcome.
KEYWORDS
Intraoperative echocardiography; Aortic dissection; Mitral valve replacement
Resumo
O uso da ecocardiografia transesofágica no intraoperatório em cirurgias valvulares é bem estabelecido de acordo com os guidelines mais recentes, assim como o seu uso no diagnóstico, manuseio e resgate de complicações perioperatórias. O objetivo deste relato de caso é ilustrar uma situação em que o seu uso no intraoperatório influenciou de maneira positiva o seu desfecho.
PALAVRAS-CHAVE
Ecocardiografia intraoperatória; Dissecção de aorta; Troca valvar mitral
Background
The use of intraoperative transesophageal echocardiography in valvular surgeries is well established according to the most recent guidelines,11 Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report fromthe American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017;30:303-71. as well as its use in the diagnosis, management, and rescue of perioperative complications.22 Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendation from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26:921-64. The purpose of this case report is to illustrate a condition in which its intraoperative use had a positive influence on the outcome.
Objectives
To describe the role of transesophageal echocardiography in the detection and evaluation of perioperative surgical complications.
Case report
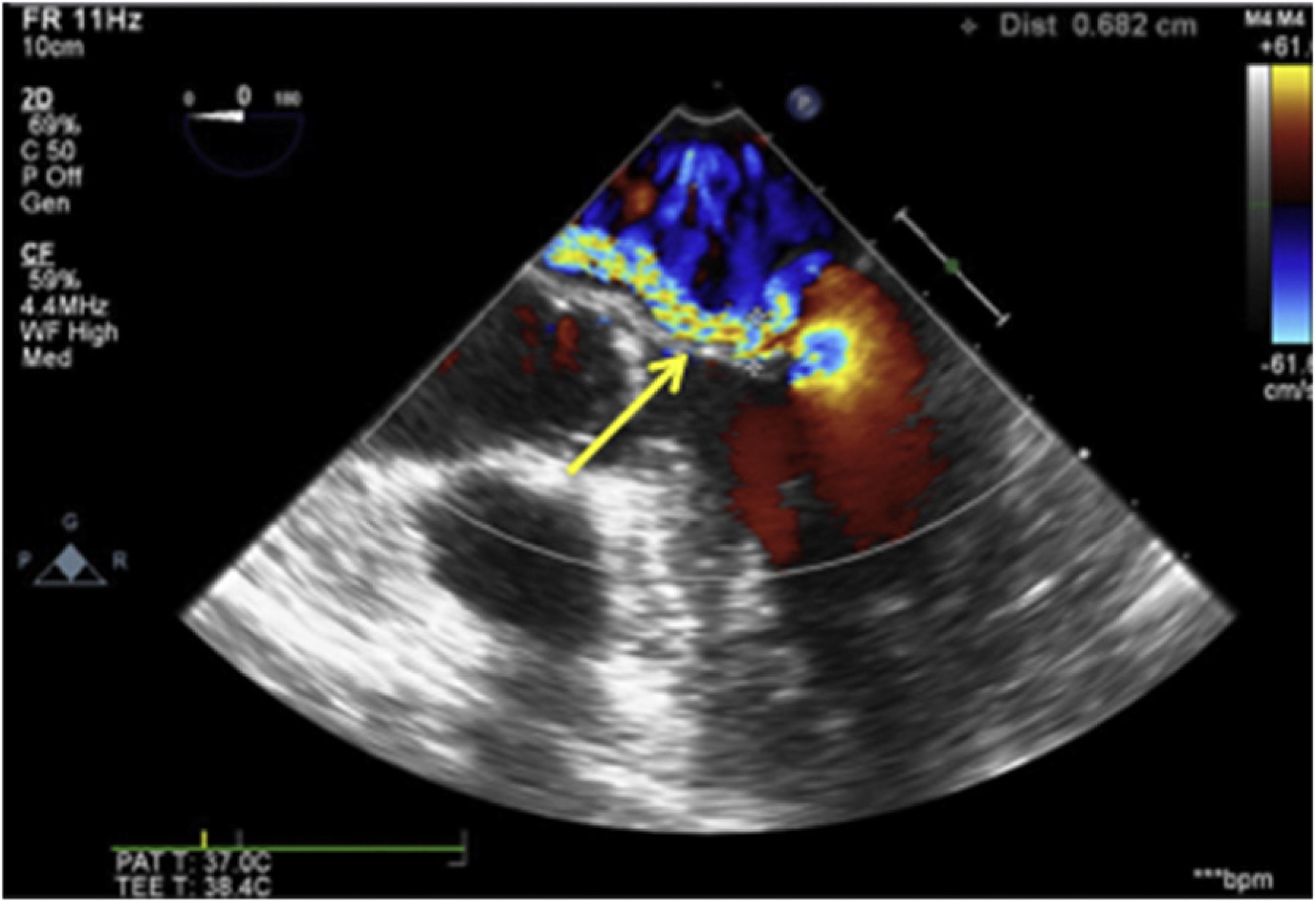
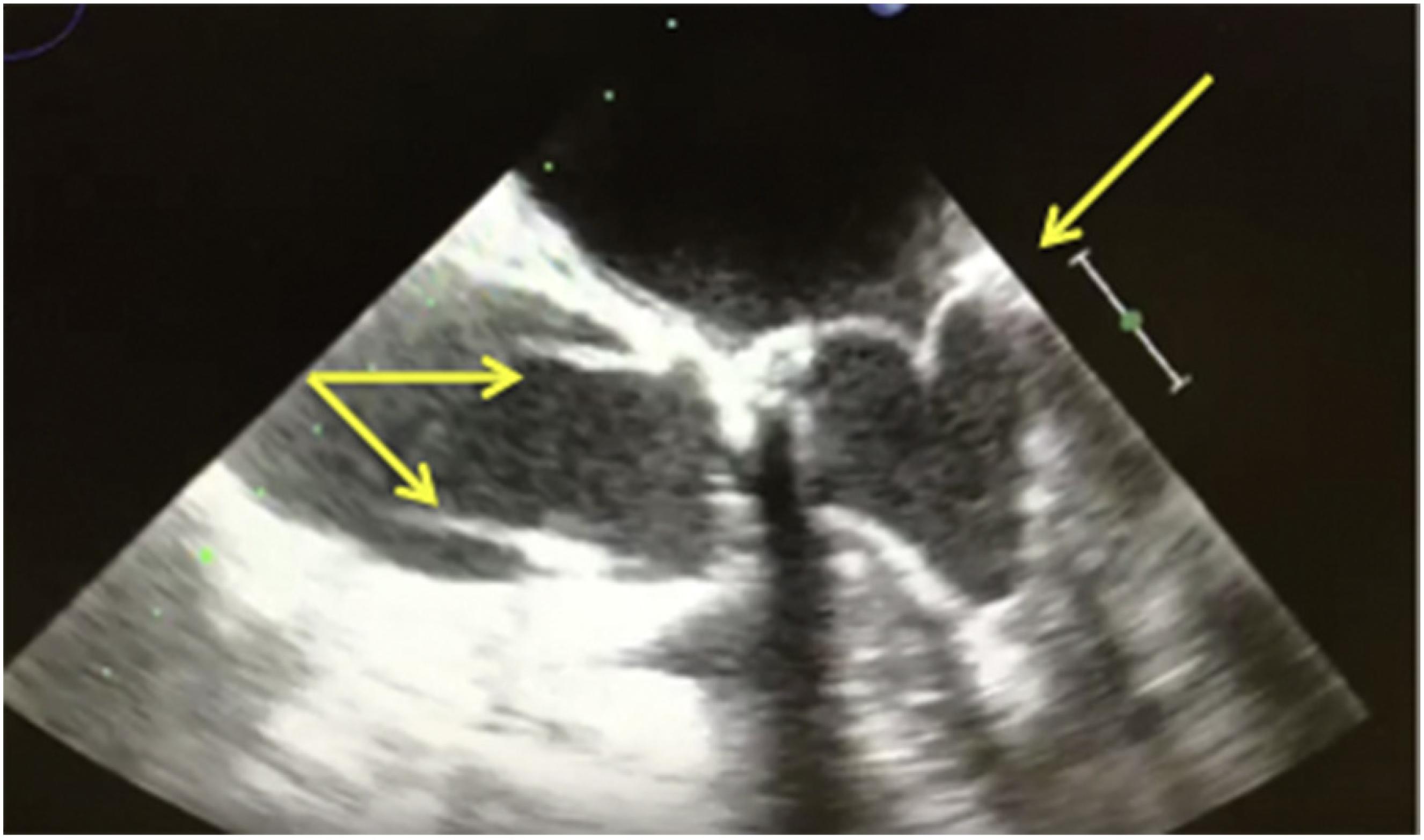
A 73-year-old male patient with severe mitral regurgitation after endocarditis (Figs. 1 and 2) underwent mitral valve replacement with a biological prosthesis implant (Edwards®), number 27, without complications (Fig. 3). Immediately after the extracorporeal circulation (ECC) removal, an image suggestive of dissection flap was seen in the ascending aorta just above the coronary ostia (Figs. 3 and 4) that extended to the aortic arch (Fig. 5). Multiple sections were obtained in order to differentiate the finding from some artifact,33 Pamnani A, Skubas NJ. Imaging artifacts during transesophageal echocardiography. Anesth Analg. 2014;118:516-20. and the diagnosis of ascending aortic dissection (Type A) was confirmed. The patient was then placed on extracorporeal circulation again to correct the injury by means of inserting a Dacron tube. The procedure was completed uneventfully and the patient was transferred in a stable condition to the ICU.
Five-chamber view with color showing severe mitral regurgitation with anteriorly directed regurgitation jet.
Three-dimensional atrial view showing posterior leaflet prolapse associated with damaged chordae.
Five-chamber view shows dissection flaps just above the coronary ostia (arrows). Biological prosthesis in mitral position is also seen.
Long-axis view of aortic valve with color showing dissection flap and swirling flow just above coronary ostia (arrow).
Short-axis view of aortic arch. Note the larger diameter of false lumen (arrow) compared to true lumen.
Discussion
Type A aortic dissection (involving the ascending aorta) is a surgical emergency; it is caused by a single or multiple lesions in the intima aortic layer, which under blood pressure are dissected from the middle layer and give rise to the false lumen.44 Sheikh AS, Ali K, Mazhar S. Acute aortic syndrome. Circulation. 2013;128:1122-7. The most common complications related to dissection include rupture of the false lumen (pericardium, pleural space, or abdominal cavity), acute aortic insufficiency, and coronary occlusion (caused by the dissection flap). Transesophageal echocardiography is an excellent tool to differentiate between true and false lumen (the false lumen usually has a larger diameter and expands in diastole) as well as to diagnose the other complications mentioned above.55 Katz ES, Tunick PA, Colvin SB, et al. Aortic dissection complicating cardiac surgery: diagnosis by intraoperative biplane transesophageal echocardiography. J Am Soc Echocardiogr. 1993;6:217-22. However, it is important to emphasize that because some artifacts (e.g., reverberation) resemble a dissection flap, which makes diagnosis difficult, a complete examination of the ascending aorta in different planes and incidences is necessary.33 Pamnani A, Skubas NJ. Imaging artifacts during transesophageal echocardiography. Anesth Analg. 2014;118:516-20. An artifact will hardly be found in orthogonal planes or have the same density and texture as true structures (Table 1).
In this case, the dissection flap location just above the origin of the coronary arteries suggests that the puncture site of the cardioplegia catheter was the triggering factor of the event, a fact proven intraoperatively after the opening of the ascending aorta.
Conclusion
Transesophageal echocardiography is an important tool in the diagnosis of aortic dissection, especially during the intraoperative period in which other diagnostic modalities are not available.66 Goldstein SA, Evangelista A, Abbara S, et al. Multimodality imaging of diseases of the thoracic aorta in adults: from the American Society of Echocardiography and the European Association of Cardiovascular Imaging Endorsed by the Society of Cardiovascular Computed Tomography and Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2015;28:119-82. Upon suspicion of dissection, a complete aortic echocardiographic examination should be performed in order to identify the site of dissection, its extent and possible associated complications (tamponade, coronary occlusion, aortic insufficiency), as all of them have an impact on the surgical management of such complication.
References
-
1Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report fromthe American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017;30:303-71.
-
2Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendation from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26:921-64.
-
3Pamnani A, Skubas NJ. Imaging artifacts during transesophageal echocardiography. Anesth Analg. 2014;118:516-20.
-
4Sheikh AS, Ali K, Mazhar S. Acute aortic syndrome. Circulation. 2013;128:1122-7.
-
5Katz ES, Tunick PA, Colvin SB, et al. Aortic dissection complicating cardiac surgery: diagnosis by intraoperative biplane transesophageal echocardiography. J Am Soc Echocardiogr. 1993;6:217-22.
-
6Goldstein SA, Evangelista A, Abbara S, et al. Multimodality imaging of diseases of the thoracic aorta in adults: from the American Society of Echocardiography and the European Association of Cardiovascular Imaging Endorsed by the Society of Cardiovascular Computed Tomography and Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2015;28:119-82.
Publication Dates
-
Publication in this collection
25 Apr 2019 -
Date of issue
Mar-Apr 2019
History
-
Received
18 Feb 2018 -
Accepted
7 May 2018