ABSTRACT
Objective:
to explain the approaches and discussions about the Advance Healthcare Directives spread among health professionals, lawyers and society.
Method:
bibliographic search in the databases SciELO, LILACS, BDENF, in Portuguese, carried out from December 2017 to January 2018.
Results:
22 articles were considered for analysis with interviews and testimonies of physicians, intensivists and geriatricians, nurses, technicians and Nursing auxiliaries, Medical students, lawyers and Law students.
Conclusion:
there is a small number of papers on the Advance Healthcare Directives in Brazil, and a wide range of approaches that have not yet been clarified. The theme is not widely spread and little clarified in its essence.
Descriptors:
Living Will; Early Directives; Bioethics, Personal Autonomy, Right to Die
RESUMEN
Objetivo:
explicitar los enfoques y discusiones sobre las Directivas Anticipadas difundidas entre los profesionales de la salud, los abogados y la sociedad.
Método:
investigación bibliográfica realizada en las bases de datos SciELO, LILACS, BDENF, en portugués, del diciembre 2017 hasta enero 2018.
Resultados:
se consideraron 22 artículos para el análisis con entrevistas y testimonios médicos, intensivistas y geriatras, enfermeros, técnicos y auxiliares de Enfermería, estudiantes de Medicina, de Derecho y abogados.
Conclusión:
hay un pequeño número de trabajos sobre las Directivas Anticipadas en Brasil, y una amplia gama de enfoques poco elucidados. El tema sigue siendo poco difundido y poco esclarecido en su esencia.
Descriptores:
Testamentos sobre la Vida; Directivas Anticipadas; Bioética, Autonomía Personal, Derecho a Morir
RESUMO
Objetivo:
explicitar as abordagens e discussões sobre as Diretivas Antecipadas da Vontade difundidas entre os profissionais de saúde, advogados e a sociedade.
Método:
pesquisa bibliográfica nas bases de dados SciELO, LILACS, BDENF, em Língua Portuguesa, realizada no período de dezembro de 2017 a janeiro de 2018.
Resultados:
foram considerados 22 artigos para análise com entrevistas e depoimentos de médicos, intensivistas e geriatras, enfermeiros, técnicos e auxiliares de Enfermagem, estudantes de Medicina, de Direito e advogados.
Conclusão:
há um pequeno número de trabalhos sobre as Diretivas Antecipadas da Vontade no Brasil, e uma ampla gama de abordagens ainda pouco elucidadas. O tema ainda é pouco difundido e pouco esclarecido em sua essência.
Descritores:
Testamentos quanto à Vida; Diretivas Antecipadas; Bioética, Autonomia Pessoal, Direito a Morrer
INTRODUCTION
Individual and social values have changed throughout times and situations, and thus have also changed moral standards. What was considered absurd came to be normality. This happened with the death of the human body, which went from something untouchable to simple material to be used for the survival of another(11 Pessini L. [At the origins of bioethics: Potter's bioethical creed to Fritz Jahr's imperative bioethical]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 13];21(1):9-19. Available from: http://dx.doi.org/10.1590/S1983-80422013000100002 Portuguese.
http://dx.doi.org/10.1590/S1983-80422013...
).
With the evolution of civilized society there was a judicialization of death. What was characterized by any individual in society as the cessation of life, came to have eminently scientific and legal connotations; and tests or procedures were necessary for the characterization of death. Today, with cutting-edge technology and the specialization of Medical Science, dying has become slow and often painful(22 Pinto LF, Baia AF. A representação da morte: desde o medo dos povos primitivos ateus a negação na atualidade. Rev Humanae [Internet]. 2013 [cited 2017 Oct 13];7(1). Available from: http://humanae.esuda.com.br/index.php/humanae/article/view/74/66
http://humanae.esuda.com.br/index.php/hu...
).
Then some new concepts arise during the disease process. The patient who is beyond therapeutic possibility and yet has his/her body invaded will be the victim of dysthanasia, that is, the methods used cause suffering without any further clinical improvement. Orthotanasia refers to the acts and procedures used in terminal patients so that death occurs with the maximum possible comfort(33 Martin LM. Eutanásia e distanásia. In: Costa SI, Oselka G, Garrafa V (coords.). Iniciação à Bioética [Internet]. Brasília: Conselho Federal de Medicina 1998 [cited 2017 Oct 14]. p. 171-92.. Available from: https://portal.cfm.org.br/images/stories/biblioteca/iniciao%20%20biotica.pdf
https://portal.cfm.org.br/images/stories...
).
With the emergence of Bioethics, a science that has emerged to unite the advances of biotechnology with the study of ethics and its implications, the act of dying takes on another dimension. Man begins to have control over life and, consequently, death: a hopeful power, but extremely dangerous(11 Pessini L. [At the origins of bioethics: Potter's bioethical creed to Fritz Jahr's imperative bioethical]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 13];21(1):9-19. Available from: http://dx.doi.org/10.1590/S1983-80422013000100002 Portuguese.
http://dx.doi.org/10.1590/S1983-80422013...
).
In the São Paulo State there is a law that deals with the rights of terminal patients of the health system, allowing them to refuse medical treatment. Law 10.245/1999 states that it is the patient's right to refuse painful or extraordinary treatments to try to prolong life(44 Assembléia Legislativa do Estado de São Paulo. Lei 10.241, 17 de março de 1999. Os direitos dos usuários dos serviços e das ações de saúde no Estado e dá outras providencias. Governo do Estado de São Paulo [Internet]. São Paulo: Secretaria da Assembléia Legislativa do Estado de São Paulo; 2001 [cited 2017 Oct 14]. [about 2 screens]. Available from: https://www.al.sp.gov.br/repositorio/legislacao/lei/1999/lei-10241-17.03.1999.html
https://www.al.sp.gov.br/repositorio/leg...
).
Resolution No. 41/1.995 of the National Council for the Rights of the Child and Adolescent (CONANDA), legally bound to the Ministry of Justice, in a text prepared by the Brazilian Society of Pediatrics, ensures the young or infant patient the right to a dignified death together to their families, when all therapeutic resources available have been depleted(55 Conselho Nacional dos Direitos da Criança e do Adolescente (CONANDA). Resolução No 41 de 17 de outubro de 1995. Os direitos da criança e do adolescente hospitalizada [Internet]. Diário Oficial da União: República Federativa do Brasil; 1995 [cited 2018 Nov 3]. Oct 17, Seção 1: [about 1 screen]. Available from http://www.mpdft.mp.br/portal/pdf/unidades/promotorias/pdij/Legislacao%20e%20Jurisprudencia/Res_41_95_Conanda.pdf
http://www.mpdft.mp.br/portal/pdf/unidad...
).
More recently, in 2012, the Federal Council of Medicine (CFM), through CFM Resolution 1.995/1.995, legitimizes the medical position on patients' advance directives. In addition to its timeliness and innovation in the face of new technical and scientific challenges, it guarantees, with regard to decisions on care and treatment, the consideration of the prior will and expressly declared by the patient, provided that in accordance with the precepts determined by the Code of Medical Ethics; this will must prevail over any other non-medical opinion, including the will of family members(66 Conselho Federal de Medicina (CFM). Resolução n. 1995, 9 de agosto de 2012. Dispõe sobre as diretivas antecipadas de vontade dos pacientes [Internet]. Diário Oficial da União: República Federativa do Brasil; 2012 [cited 2018 Nov 3]. Aug 31Seção 1: [about 5 screens]. Available from: http://www.portalmedico.org.br/resolucoes/cfm/2012/1995_2012.pdf
http://www.portalmedico.org.br/resolucoe...
).
The Advance Healthcare Directives (AHD) are understood as the set of will previously expressed by the patient about care and treatment that he or she will to receive when unable to freely and autonomously express his/her will. AHD recognize the patient's right to refuse futile medical care, also known as extraordinary treatment, that is, treatments that aim only to prolong their biological life without guaranteeing their quality(77 Dadalto L, Tupinambás U, Greco DB. [Advanced directive: a brasilian model]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 20];21(3):463-76. Available from: http://dx.doi.org/10.1590/S1983-80422013000300011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422013...
).
In Brazil, there is still no specific legislation for AHD, and since CFM Resolution 1.995/2012, discussions have taken place informally and discreetly among groups of professionals. Scientific studies bring up this discussion, which for many there remains some confusion.
The present study questions whether there is an expressive approach to the Advance Healthcare Directives in the literature.
OBJECTIVE
To know the diverse lines of approaches and reflections on the Advance Healthcare Directives contained in articles published in Brazil.
METHOD
Type of study
An integrative review of the literature was conducted, making it possible to collect, analyze, synthesize and present the approach of multiple studies published on the subject in a systematic and orderly manner, contributing to the knowledge of its current approaches.
Methodological procedures
The subject, and the inclusion and exclusion criteria were defined; the articles were selected; the interpretation of results and presentation of the review were carried out(88 Mendes KDS, Silveira RCCP, Galvao CM. [Integrative literature review: a research method to incorporate evidence in health care and nursing]. Rev Text Contexto Enferm [Internet]. 2008 [cited 2017 Oct 23];17:758-64. Available from: http://dx.doi.org/10.1590/S0104-07072008000400018 Portuguese.
http://dx.doi.org/10.1590/S0104-07072008...
). The formulation of the problem included the following guiding question: approaches and reflections on AHD contained in articles published in Brazil.
Data sources
research was carried out in the world wide web, in the Virtual Health Library (VHL) databases: Scientific Electronic Library Online (SciELO), Latin American and Caribbean Literature in Health Sciences (LILACS) and Nursing Database (BDENF).
Data collection occurred from October 2017 to January 2018. The descriptors "medical directives" (MD), "advance directives" (AD) and "living will" (LW), referred to in the Descriptors in Health Sciences (DeCS) were used to select articles produced in Brazil and their different approaches, in addition to the association of key words. After the search for scientific productions, an analysis of the articles was carried out to verify their approximation with the proposed objective.
Sample; inclusion and exclusion criteria
For refinement, the following inclusion criteria were defined: scientific articles that explained the methodological procedures adopted, written in Portuguese, without restriction regarding the year of publication and related to the descriptors.
They were then subjected to careful reading of the title and abstract, verifying their suitability to the theme.
Data analysis
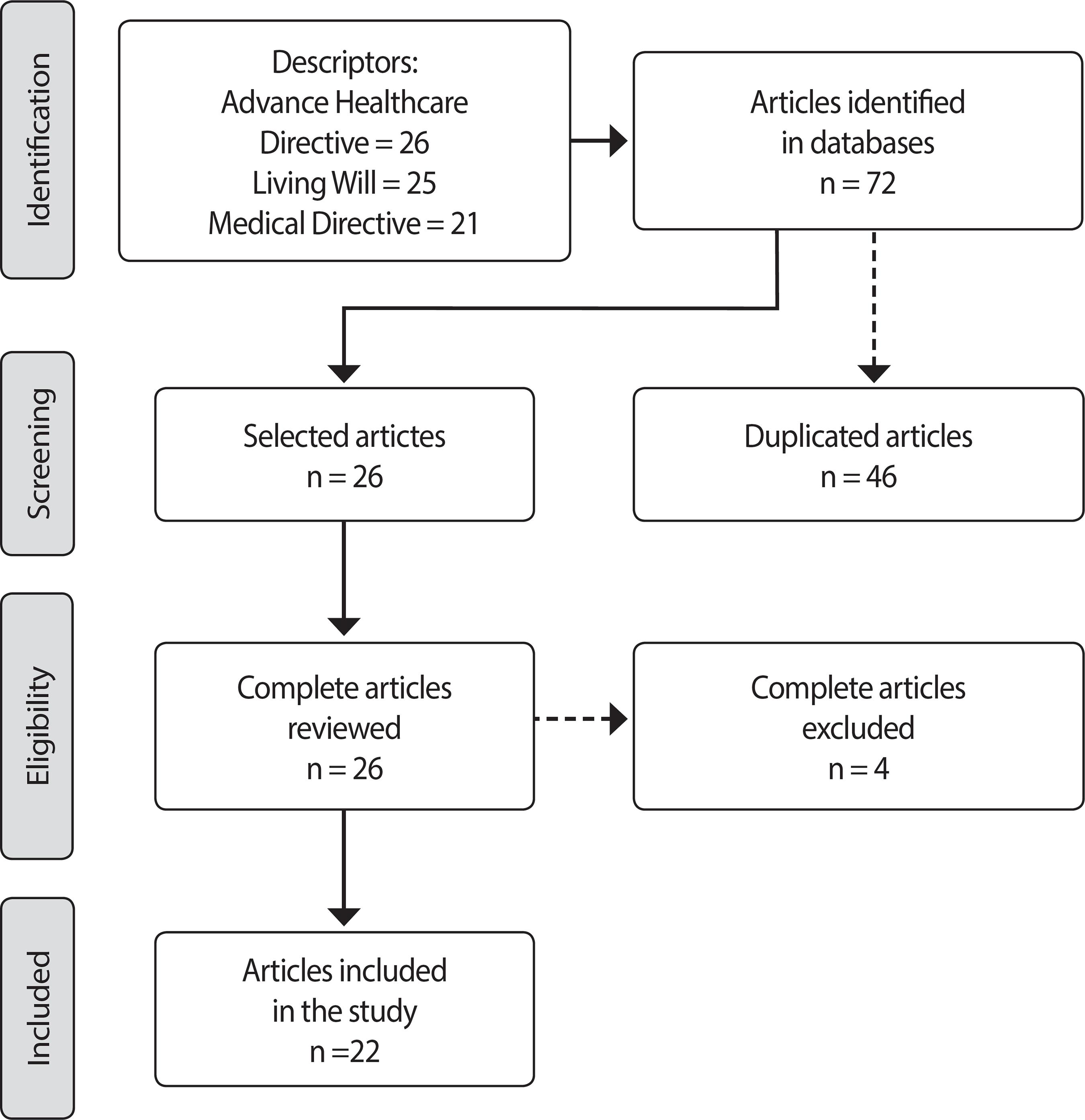
In the search for the national articles in the databases described, considering the mentioned descriptors, 72 articles were found. With the descriptor Advance Healthcare Directive 26 articles were found in the VHL, in the databases SciELO, LILACS,BDENF, in Portuguese, from 2011 to 2017.
With the descriptor "MD" 25 articles were found; with "LW", 21 articles in the databases SciELO, LILACS and BDENF, from 2011 to 2015. A total of 46 articles was excluded by repetition. In addition to these, a thesis, a monograph and a letter to the editor. Regarding the association of keywords, five articles were found. They were then subjected to careful reading of the title and abstract, verifying their suitability to the theme (Figure 1).
Data organization
For the demonstration of the approaches to the topic, a data collection instrument was created (Chart 1), containing: year of publication, title of article, main referenced approaches, results and conclusions. Finally, the articles were analyzed in full, and the results were produced in a descriptive way.
RESULTS
At the end, 22 papers were considered for analysis. Studies with interviews and testimonies of physicians, intensivists and geriatricians, nurses, Nursing technicians and assistants, Medical students, lawyers and Law students were conducted, as well as integrative and literature reviews. They are presented in Chart 1.
DISCUSSION
Death can be seen through different prisms since ancient times. Dying close to the family, encouraging the continuity of will and sharing goods were valued in the Middle Ages(1616 Kovács MJ. [Towards death with dignity in the XXI Century]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(1):94-104. Available from: http://dx.doi.org/10.1590/S1983-80422014000100011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422014...
). In this way, unexpected and solitary deaths were not the predominant desire. The view of death presented a different view than that of contemporary times.
Nowadays, prolonging and isolating the lives of many patients leads to the growing desire for a quick and painless death, with relatives present, dying with dignity and preserving patients' beliefs and values(3030 Menezes RA. Em busca da boa morte: antropologia dos cuidados paliativos. Rio de Janeiro: Garamond; 2004. 228 p.).
When the subject "dying with dignity" is approached, there is intense discussion. Palliative care programs focus on death with dignity, facilitating the patient's autonomy in decisions that involve prolonging life. Thus, good death, painless, respecting the will of patients, establishes a new topic of communication between family members and health professionals(1616 Kovács MJ. [Towards death with dignity in the XXI Century]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(1):94-104. Available from: http://dx.doi.org/10.1590/S1983-80422014000100011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422014...
).
Bioethics seeks to show a new direction to the impasse between religiosity and AHD, emphasizing autonomy, beneficence and otherness. When technology and death are confronted, there are relevant and complex ethical dilemmas. Many questions arise, leading people to reflect and question their human values. The complexity increases when the spiritual element is added to these reflections, effervescing ethical and existential questions about the interventions of the health professional. In this sense, when it comes to AHD, it is necessary to establish exact criteria for good clinical practice, because when the principle of alterity is approached health professionals can have their perception modified when putting them in the patient's shoes(3131 Asai A FS, Lo B. Attitude of Japanese and Japanese-American physicians towards life sustaining treatment. Lancet [Internet]. 1995 [cited 2018 Jan 21];346(8971):356-9. Available from: doi:https://doi.org/10.5555/uri:pii:S014067369592230X
https://doi.org/10.5555/uri:pii:S0140673...
).
The option of persisting in the treatment of terminally ill patients, instead of opening dialogue about possibilities of end-of-life procedures, may lead to difficulties and changes in the comfort zone of health professionals. It is not possible to deny the limitations on the implementation of AHD, either by the feeling of impotence or by the therapeutic obstinacy of professionals(2323 Cogo SB, Lunardi VL, Quintana AM, et al. Challenges to implementation of advance directives of will in hospital practice. Rev Bras Enferm [Internet]. 2016 [cited 2017 Oct 30];69(6):969-76. Available from: http://www.scielo.br/pdf/reben/v69n6/0034-7167-reben-69-06-1031.pdf
http://www.scielo.br/pdf/reben/v69n6/003...
). On the other hand, for family caregivers, hiding the diagnosis from the terminal patient impairs adherence to the practice of AHD.
An alternative is the approach of terms called Advanced Care Planning, which expresses the preference or refusal of the patient to certain interventions, such as mechanical ventilation, parenteral nutrition and hemodialysis as care goals(3232 Stone J. Advance directives, autonomy and unintended death. Rev Bioethics [Internet]. 1994 [cited 2018 Jan 23];8(3):223-46. Available from: https://doi.org/10.1111/j.1467-8519.1994.tb00256.x
https://doi.org/10.1111/j.1467-8519.1994...
).
Since AHD are an instrument of patients and involve decisions of the medical professionals and the proxy, it is fundamental that the difference between the model of pure autonomy and the substitute judgment be clarified. Whereas the former applies exclusively to patients who were already autonomous and expressed an autonomous or preferably relevant decision, the latter seeks to unveil what the patient's will would be if he/she could express his/her will, a situation in which the proxies act as if they were the patient. Given these definitions, the AHD containing patient guidelines and the appointment of a proxy include both models(3333 Beauchamp TL. Princípios de ética biomédica. 3 ed. Rio de Janeiro: Loyola. 2002. 576 p.).
There are three clinical states in which decision-making on the end-of-life are cited in AHD interviews: terminal illness, persistent vegetative state, and advanced dementias. However, there is still a conflict between cultural and individual values and technical criteria. On the other hand, the medical professional fears fulfilling the patient's desire and suffering the consequences of judicialization of Medicine. It is justified that both the CFM and the Legislative Branch should be directed and defined to provide legal support for health professionals to reformulate their concepts regarding AHD, since the refusal of patients to be hydrated and fed by probes becomes invalid if the professionals do not respect their desire(77 Dadalto L, Tupinambás U, Greco DB. [Advanced directive: a brasilian model]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 20];21(3):463-76. Available from: http://dx.doi.org/10.1590/S1983-80422013000300011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422013...
).
As can be seen, in the midst of conflicts and discussions already mentioned, the patient's AHD are located, an instrument written in advance to be applied at the end of the author's life, a moment that generates so many ethical, legal and religious controversies.
The LW is helpful here, and can be understood as the act of caring for the patient, allowing him or her to join or dispense with treatments and/or procedures at the end of life, and ensuring control in decisions about his/her health. The Living Will appeared in the United States in the late 1960s as a written statement refusing perceived treatments, such as therapeutic obstinacy, which should be given to doctors, family members, and legal representatives(77 Dadalto L, Tupinambás U, Greco DB. [Advanced directive: a brasilian model]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 20];21(3):463-76. Available from: http://dx.doi.org/10.1590/S1983-80422013000300011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422013...
). In this context, therapeutic obstinacy is also discussed as well as palliative care observed in complex cases that new technologies and scientific knowledge offer(3434 Nebot C, Ortega B, Mira J, et al. Dying with dignity. A study of living wills. Gac Sanit. 2010;24(6):437-45. doi:10.1016/j.gaceta.2010.09.006
https://doi.org/10.1016/j.gaceta.2010.09...
). During these discussions, terminal patients and the goal of alleviating and reducing suffering must not be forgotten. The LW humanizes care and reduces suffering.
A recent study conducted in Rio Grande do Sul State shows that the nursing team has little knowledge about AHD. It is a recent and important topic and should be addressed and discussed both in the academy and in professional practice. Thus, the extensive discussion on the topic will lead to the valorization of the patient's guidelines and will, and legal aspects in Brazil(2020 Cassol PB, Quintana AM, Velho MTAC. [Anticipated policy will: perception of nursing staff of blood-oncology]. Rev J Nurs Health [Internet]. 2015 [cited 2017 Oct 24];5(1):04-13. Available from: doi: http://dx.doi.org/10.15210/jonah.v5i1.5497 Portuguese.
http://dx.doi.org/10.15210/jonah.v5i1.54...
).
AHD are recent themes in the patient care scenario, which aim to attend to and respect the autonomy of patients or their family members. However, they also produce discussions and conflicts among health professionals because they modify the routines used in patient care(2020 Cassol PB, Quintana AM, Velho MTAC. [Anticipated policy will: perception of nursing staff of blood-oncology]. Rev J Nurs Health [Internet]. 2015 [cited 2017 Oct 24];5(1):04-13. Available from: doi: http://dx.doi.org/10.15210/jonah.v5i1.5497 Portuguese.
http://dx.doi.org/10.15210/jonah.v5i1.54...
).
The Federal Constitution of 1988 guarantees rights to citizens, and among them is the principle of human dignity, which can be understood as a subjective and personal satisfaction. Thus, granting the death-conscious request to a terminal patient would not be contrary to Article 5 of the Federal Constitution. Nevertheless, some authors do not understand it in this way, since men take all the risks and suffer all the consequences of living with a dynamic society and becoming increasingly freer from prejudice(1616 Kovács MJ. [Towards death with dignity in the XXI Century]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(1):94-104. Available from: http://dx.doi.org/10.1590/S1983-80422014000100011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422014...
).
Avoiding death is related to new medical technologies, which fascinates people and health professionals. Death has been replaced from houses to hospitals. Currently, death in an unexpected and violent manner has increased, and occurs, to a large extent, without protection or care. Under a different perspective, with the approach of death, terminal patients and their families can have access to humanized death, accepting suffering, focusing attention on the patient, returning to the natural process of dying, with respect, humility, without banishment or banalization(1616 Kovács MJ. [Towards death with dignity in the XXI Century]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(1):94-104. Available from: http://dx.doi.org/10.1590/S1983-80422014000100011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422014...
).
Terminal patients are stigmatized and labeled, and there is an expectation of pain, suffering, and isolation at death. In addition, the patient experiences a feeling of powerlessness, distancing from the family, work, causing loss of autonomy and health(1616 Kovács MJ. [Towards death with dignity in the XXI Century]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(1):94-104. Available from: http://dx.doi.org/10.1590/S1983-80422014000100011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422014...
).
Medical technology is present in diagnostics and treatments, allowing significant progress in curing diseases and extending life. However, it is necessary to consider possible damage of prolonging the life of sick people. What is behind this discussion is the need to put people at the center of the process, favoring dignity and autonomy of their choices, the sense of belonging – provisions that become even more urgent when it comes to vulnerable people. Humanization involves solidarity, compassion, rapprochement and respect(1616 Kovács MJ. [Towards death with dignity in the XXI Century]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(1):94-104. Available from: http://dx.doi.org/10.1590/S1983-80422014000100011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422014...
).
At first, technology assists in improving methods to ensure longer life for a terminally ill patient, since some methods are not enough to achieve cure and sometimes only prolong the patient's suffering(11 Pessini L. [At the origins of bioethics: Potter's bioethical creed to Fritz Jahr's imperative bioethical]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 13];21(1):9-19. Available from: http://dx.doi.org/10.1590/S1983-80422013000100002 Portuguese.
http://dx.doi.org/10.1590/S1983-80422013...
).
With the advancement of medical technology, the prolongation of life and the conflicts generated about the theme, the change in the connotation of euthanasia is questioned. Despite legal support, religious, scientific, and ethical issues continue in conflict with patients, family members, representatives, and health professionals. The main purpose of euthanasia is leading to death to abbreviate pain; that of dysthanasia is preventing death at any cost. Orthotanasia seeks death with dignity at the right moment, controling pain and physical and psychic symptoms, as well as issues related to social and spiritual dimensions(1616 Kovács MJ. [Towards death with dignity in the XXI Century]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(1):94-104. Available from: http://dx.doi.org/10.1590/S1983-80422014000100011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422014...
).
Euthanasia means the medical procedures aimed at shortening patient's life, such as the application of a lethal medication or the withdrawal of a fundamental device for the patient, e.g., artificial ventilation. On the other hand, dysthanasia is considered the reverse procedure of euthanasia, in which the doctor uses extreme means, such as devices and innovations in the area, to maximize the patient's life(3535 Pithan LH. A dignidade humana como fundamento jurídico das "ordens de não-ressuscitação". 1 ed. Porto Alegre: EDIPUCRS. 2004. 137 p.).
Euthanasia can be classified in an active and passive way, so that passive euthanasia is more commonly accepted, since it aims to end the patient's suffering and pain; however, it is not characterized as a medical action, but as a suspension of a medical therapy applied to the terminal patient. Therefore, the health professional stops practicing an action or a procedure that could prolong life, usually by interrupting the treatment(3636 Bento LA. Bioética: Desafios éticos no debate contemporâneo. 1 ed. São Paulo: Paulinas, 2008. 462 p.). Dysthanasia means etymologically the "exaggerated prolongation of the agony, suffering and death of a patient", that is, it is the medical procedure that follows the opposite direction of euthanasia, since it aims to prolong the patient's life until the last moment. Orthotanasia is a way of guaranteeing the dignity of the patient, without disrespecting his/her will, and it has a conformity between his/her will and the fundamental principle, guaranteed constitutionally. In the etymological sense, some authors observe the antagonism of euthanasia and dysthanasia, but refer to a similarity with morality and ethics in its application(3636 Bento LA. Bioética: Desafios éticos no debate contemporâneo. 1 ed. São Paulo: Paulinas, 2008. 462 p.).
To carry out the Living Will, it suffices to have civil capacity and registration, and it will be valid until its revocation or the death of the author. The public deed, or proxy, does not express the real will, because the disease process does not exist; under this process, the will may be contrary to that previously expressed in the will written.
The proxy will be able to assist the medical staff when the family is against the will written and to decide when the LW is omitted, since the doctor feels it is difficult to respect the AHD when the family is contrary to this will(77 Dadalto L, Tupinambás U, Greco DB. [Advanced directive: a brasilian model]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 20];21(3):463-76. Available from: http://dx.doi.org/10.1590/S1983-80422013000300011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422013...
).
Legally, the doctor is not bound to Resolution CFM 1.995/2012, in an ethical manner related to the LW, not being obliged to abide by them, because there is freedom guaranteed by the Federal Constitution, which in its article 5, paragraph II, reports that nobody will be obliged to do or not to do anything, except if provided in law. There is no legal prohibition, and the doctor can, legally, not abide by the patient's AHD(1313 Bussinguer ECA, Barcellos IA. [The right to live one's own death and its constitutionality]. Rev Ciênc Saúde Colet [Internet]. 2013 [cited 2017 Oct 24];18(9):2691-8. Available from: http://dx.doi.org/10.1590/S1413-81232013000900024 Portuguese
http://dx.doi.org/10.1590/S1413-81232013...
).
The patient's and the health professional's insecurity to use and accept AHD faces the fear of violating ethical and legal norms of Resolution 1.995/2012, which has no force of law. The absence of legal force makes an important instrument for interpreting and directing legal hermeneutics possible, and the fact that AHD are not prescribed by law does not immediately exclude their inclusion in the legal system of the country(1515 Pattela LHD, Alves RGO, Loch JA. [Advanced directives by the patient: a brief introduction to the theme]. Rev AMRIGS [Internet]. 2014 [cited 2017 Oct 24];58(2):162-5. Available from: http://www.amrigs.org.br/revista/58-02/014.pdf Portuguese
http://www.amrigs.org.br/revista/58-02/0...
).
The future applicability of Resolution 1.995/2012 involves important elements such as bioethical and legal aspects, language and the end of life. However, the Brazilian context does not have any law that makes it possible to legislate on the elaboration of a document that expresses the patient's will.
The discussion about the so-called orthotanasia is on the agenda in Bill No. 6.715 of 2009, of the Federal Senate, which foresees to amend the Penal Code (CP) to exclude from unlawfulness orthotanasia, that is, the "discontinuation of disproportionate and extraordinary therapeutic measures for the artificial maintenance of patients' lives in imminent and inevitable death attested by two doctors"(88 Mendes KDS, Silveira RCCP, Galvao CM. [Integrative literature review: a research method to incorporate evidence in health care and nursing]. Rev Text Contexto Enferm [Internet]. 2008 [cited 2017 Oct 23];17:758-64. Available from: http://dx.doi.org/10.1590/S0104-07072008000400018 Portuguese.
http://dx.doi.org/10.1590/S0104-07072008...
).
The civil responsibility of doctors is very much related to the role that these professionals have been developing, i.e., the responsibility to save lives using several means of treatment. What are the limits to take responsibility for the failure of treatment or for errors and what are the limits that can follow; and to what extent will he be held liable for non-compliance(1212 Crippa A, Buonicore GP, Feijó AGS. [Advance directives of will and the civil responsibility of the Physician]. Rev AMRIGS [Internet]. 2013 [cited 2017 Oct 24];57(4):344-8. Available from: http://www.amrigs.org.br/revista/57-04/0000222859-15_1288_Revista%20AMRIGS.pdf Portuguese
http://www.amrigs.org.br/revista/57-04/0...
)?
The great question of AHD regards what kind of civil liability will be applied: the objective, which is independent of guilt and which configures damage and the causal link of guilt; or subjective, which is related to guilt in which the causative agent will be held liable if he/she has acted guiltily or wilfully. As noted, there is still no jurisprudence and doctrines on the subject, since they are relatively recent directives(1212 Crippa A, Buonicore GP, Feijó AGS. [Advance directives of will and the civil responsibility of the Physician]. Rev AMRIGS [Internet]. 2013 [cited 2017 Oct 24];57(4):344-8. Available from: http://www.amrigs.org.br/revista/57-04/0000222859-15_1288_Revista%20AMRIGS.pdf Portuguese
http://www.amrigs.org.br/revista/57-04/0...
).
The civil liability of doctors is, as a rule, subjective and can be held liable if they do not respect these AHD and, consequently, do not respect patients' autonomy. It should be noted that, although there is no specific law regarding the Advance Healthcare Directives, the Code of Medical Ethics and Resolution CFM 1.995/2012, which deal with the issue, are broad rules to be followed and respected(1212 Crippa A, Buonicore GP, Feijó AGS. [Advance directives of will and the civil responsibility of the Physician]. Rev AMRIGS [Internet]. 2013 [cited 2017 Oct 24];57(4):344-8. Available from: http://www.amrigs.org.br/revista/57-04/0000222859-15_1288_Revista%20AMRIGS.pdf Portuguese
http://www.amrigs.org.br/revista/57-04/0...
).
The subject is quite controversial and is still being discussed in several countries, so that in some countries there are already resolutions or even laws that allow the LW. In Italy and Portugal there is no express regulation that it, nor even the appointment of a proxy(3737 Kfouri Neto MI. Testamento Vital. Rev Judic Paraná [Internet]. 2006 [cited 2018 Jan 18];1:201-16. Available from: http://www.revistajudiciaria.com.br/portfolio-posts/revista-judiciaria-do-parana-edicao-02-2/
http://www.revistajudiciaria.com.br/port...
).
The right to life also refers to the moment of death. The Federal Constitution in its Article 5 caput determines the inviolability of the right to life as an unwaivable right(3838 Parizotto T. Polêmica: Eutanásia à luz do Direito. Rev Jornal da UEM [Internet]. J Univ Est Maringá [Internet]. 2011 [cited 2018 Jan 28];101:[about 2 screens]. Available from: http://www.jornal.uem.br/2011/index.php/edicoes-2011/87-jornal-101-setembro-2011/759-eutanasia-a-luz-do-direito
http://www.jornal.uem.br/2011/index.php/...
), that is, something you cannot decide, make it what you want, refers to its own right to use.
At the moment life ends, the principle of the dignity of a person appears, which means that every person has the right to a dignified death. As expected, the draft of the new Penal Code typifies active Euthanasia with imprisonment. Passive euthanasia is characterized by an omission or the expression of the will of both the family and the patient in not being subjected to life by artificial means(3939 Carvalho GM. Aspectos Jurídicos-penais da Eutanásia. São Paulo: IBCCRIM; 2001. 206 p.).
Fears related to legal implications appear as a determining and limiting factor in the application of AHD by nurses, doctors and family caregivers in the hospital context. CFM Resolution 1.995/12 still raises questions as to its applicability(2323 Cogo SB, Lunardi VL, Quintana AM, et al. Challenges to implementation of advance directives of will in hospital practice. Rev Bras Enferm [Internet]. 2016 [cited 2017 Oct 30];69(6):969-76. Available from: http://www.scielo.br/pdf/reben/v69n6/0034-7167-reben-69-06-1031.pdf
http://www.scielo.br/pdf/reben/v69n6/003...
). Moreover, an uncertainty of the patient's diagnosis added to the ignorance of his/her illness and prognosis are points that translate into fears of professionals and family members(2424 Cogo SB, Lunardi VL, Quintana AM, et al. Advance directives: wills of health professional and Family caregivers. Rev Baiana Enferm [Internet]. 2017 [cited 2017 Oct 30];31(1):e16932. Available from: doi 10.18471/rbe.v31i1.16932
https://doi.org/10.18471/rbe.v31i1.16932...
). The multiprofessional team recognizes patients' autonomy rights at the terminal stage. However, when it is necessary to dialogue with relatives so that they can express themselves on the patient's will, there is no security to attend to the exposed will, due to the understanding that relatives are in a moment of suffering.
Resolution CFM 1.995/12 states that it is up to doctors to record AHD in the medical record when they are communicated directly by the patient. The patient's expression of will interferes greatly with medical conduct and, in most cases, the licensed authority is technically vulnerable to do so(77 Dadalto L, Tupinambás U, Greco DB. [Advanced directive: a brasilian model]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 20];21(3):463-76. Available from: http://dx.doi.org/10.1590/S1983-80422013000300011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422013...
).
A legal responsible for making decisions when the patient is terminally ill is a way of maintaining and accepting the patient's will. However, relatives prefer that decisions be coordinated between the medical staff and the patient(1010 Campos MO, Bonamigo EL, Steffani JA, et al. [Living wills: perception of oncology patients and accompanying family members]. Rev Bioethikos [Internet]. 2012 [cited 2017 Oct 24];6(3):253-9. Available from: https://saocamilo-sp.br/assets/artigo/bioethikos/96/1.pdf Portuguese.
https://saocamilo-sp.br/assets/artigo/bi...
). With AHD, patients expose and discuss with their medical staff their will about which treatments they prefer to perform if they are terminally ill(4040 Holland S. Bioética enfoque filosófico. São Paulo: Loyola. 2008. 304 p.).
In Brazil, the level of knowledge among health professionals and students, regarding AHD, is a subject that is not well discussed in classes, since there are few studies on the subject. Despite this, the participants were prone to the acceptance of AHD(77 Dadalto L, Tupinambás U, Greco DB. [Advanced directive: a brasilian model]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 20];21(3):463-76. Available from: http://dx.doi.org/10.1590/S1983-80422013000300011 Portuguese.
http://dx.doi.org/10.1590/S1983-80422013...
,99 Piccini CF, Steffani JA, Bonamigo EL, et al. [Living will in the perspective of doctors, lawyers and students]. Rev Bioethikos [Internet]. 2011 [cited 2017 Oct 24];5(4):384-91. Available from: https://saocamilo-sp.br/assets/artigo/bioethikos/89/A4.pdf Portuguese.
https://saocamilo-sp.br/assets/artigo/bi...
,4141 Stolz C, Gehlen G, Bonamigo EL, et al. Manifestation of patient's anticipated will as dysthanasia inhibiting factor. Rev Bioét [Internet]. 2014 [cited 2018 Jan 28];19(3):833-45. Available from: http://revistabioetica.cfm.org.br/index.php/revista_bioetica/article/view/679
http://revistabioetica.cfm.org.br/index....
).
Surveys carried out in Spain and Australia found that more than 50% of lawyers, doctors and students were aware of the Living Will and declared themselves in favor of its implementation, provided that it is regulated, since the patient's will are to be respected.
A study found that the professionals interviewed still have difficulty dealing with this issue and that they would feel more capable of fulfilling the desire expressed by the terminal patient if the law to support clinical practice was established(1313 Bussinguer ECA, Barcellos IA. [The right to live one's own death and its constitutionality]. Rev Ciênc Saúde Colet [Internet]. 2013 [cited 2017 Oct 24];18(9):2691-8. Available from: http://dx.doi.org/10.1590/S1413-81232013000900024 Portuguese
http://dx.doi.org/10.1590/S1413-81232013...
). Other studies have found that students of Medicine have little knowledge about AHD. It was verified that the subject is discussed superficially in the discipline of Medical Ethics and, in view of this result, there is a need to insert the subject in discussions and clarifications of the theme throughout medical training(4343 Gusmão A. [Living will]. Arq CRMPR [Internet]. 2013 [cited 2018 Jan 20];30(118):1-2. Available from: http://crmpr.org.br/publicacoes/cientificas/index.php/arquivos/article/view/437
http://crmpr.org.br/publicacoes/cientifi...
-4444 Bomtempo TV. A ortotanásia e o direito de morrer com dignidade: uma análise constitucional. Rev Int Direito Cid [Internet]. 2011 [cited 2018 Jan 22];(9):169-182. Available from: http://www.ipebj.com.br/docdown/_7ce.pdf
http://www.ipebj.com.br/docdown/_7ce.pdf...
). On the other hand, terminal cancer patients, after orientations, prefer to edit their own LW, and the companions agree with this point of view(2020 Cassol PB, Quintana AM, Velho MTAC. [Anticipated policy will: perception of nursing staff of blood-oncology]. Rev J Nurs Health [Internet]. 2015 [cited 2017 Oct 24];5(1):04-13. Available from: doi: http://dx.doi.org/10.15210/jonah.v5i1.5497 Portuguese.
http://dx.doi.org/10.15210/jonah.v5i1.54...
).
Deciding about what to do or not to the terminally ill patient is always an ethical dilemma for doctors(4545 Schiff R SP, Snook J, Rajkumar C, Bulpitt CJ. Living wills and the mental capacity act: a postal questionnaire survey of UK geriatricians. Age Ageing [Internet]. 2006 [cited 2018 Jan 11];35(2):116-21. Available from: https://doi.org/10.1093/ageing/afj035
https://doi.org/10.1093/ageing/afj035...
). AHD allow doctors and their health care team to respect the patient's autonomy and fulfill their will in the face of numerous palliative treatment options. However, asking the patient or his/her representative to decide what kind of treatment should be done or not is a broad ethical dilemma(4646 Martínez K. The living will. An Sis Sanit Navarra [Internet]. 2007 [cited 2018 Jan 26];30(Suppl 3):87-102. Available from: http://scielo.isciii.es/pdf/asisna/v30s3/original6.pdf
http://scielo.isciii.es/pdf/asisna/v30s3...
).
The doctor-patient relationship based on respect and ethics is fundamental for the family to consider accepting the will expressed by the patient or designated by his/her legal representative when there is no more possibility for cure, thus respecting patients' autonomy(1515 Pattela LHD, Alves RGO, Loch JA. [Advanced directives by the patient: a brief introduction to the theme]. Rev AMRIGS [Internet]. 2014 [cited 2017 Oct 24];58(2):162-5. Available from: http://www.amrigs.org.br/revista/58-02/014.pdf Portuguese
http://www.amrigs.org.br/revista/58-02/0...
).
Study limitations
As a limitation, the small number of studies found in the literature is pointed out; for future investigations it is recommended to expand the databases.
Contributions to the Nursing, Health or Public Policy fields
The present study synthesized the main results regarding AHD, generating a broad vision and providing knowledge and visualization of the most varied lines of debates, encouraging new studies to be conducted on ethical, technical and managerial impacts in the clinical practice of Nursing. As member of the multiprofessional team, Nursing based on care, regardless of expectation of healing, feels the impact of the challenge of being before someone who has already decided not to be kept alive. The care plan is being transformed as it reorients the care route once linked to comfort, enhancing existing skills such as better patient care.
FINAL CONSIDERATIONS
With the present study, it is concluded that the number of papers on Advance Healthcare Directives in Brazil is still not expressive. The AHD present themselves as a concept that is still not widely spread and is not very clear, in its essence, in the studies found. The studies present several approaches: the position and performance of the health professional, health technologies, the family and their legal representatives, the patient, the social, cultural and religious contexts, the forms of communication and their ambiguities, legislation and resolutions. Notwithstanding, it all appears in a fragmented way. Through this, this study summarized the approaches and the focus of each debate, thus generating a broad vision about Advance Healthcare Directives and enabling its application in an adequate, coherent and global way with the patient.
REFERENCES
-
1Pessini L. [At the origins of bioethics: Potter's bioethical creed to Fritz Jahr's imperative bioethical]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 13];21(1):9-19. Available from: http://dx.doi.org/10.1590/S1983-80422013000100002 Portuguese.
» http://dx.doi.org/10.1590/S1983-80422013000100002 -
2Pinto LF, Baia AF. A representação da morte: desde o medo dos povos primitivos ateus a negação na atualidade. Rev Humanae [Internet]. 2013 [cited 2017 Oct 13];7(1). Available from: http://humanae.esuda.com.br/index.php/humanae/article/view/74/66
» http://humanae.esuda.com.br/index.php/humanae/article/view/74/66 -
3Martin LM. Eutanásia e distanásia. In: Costa SI, Oselka G, Garrafa V (coords.). Iniciação à Bioética [Internet]. Brasília: Conselho Federal de Medicina 1998 [cited 2017 Oct 14]. p. 171-92.. Available from: https://portal.cfm.org.br/images/stories/biblioteca/iniciao%20%20biotica.pdf
» https://portal.cfm.org.br/images/stories/biblioteca/iniciao%20%20biotica.pdf -
4Assembléia Legislativa do Estado de São Paulo. Lei 10.241, 17 de março de 1999. Os direitos dos usuários dos serviços e das ações de saúde no Estado e dá outras providencias. Governo do Estado de São Paulo [Internet]. São Paulo: Secretaria da Assembléia Legislativa do Estado de São Paulo; 2001 [cited 2017 Oct 14]. [about 2 screens]. Available from: https://www.al.sp.gov.br/repositorio/legislacao/lei/1999/lei-10241-17.03.1999.html
» https://www.al.sp.gov.br/repositorio/legislacao/lei/1999/lei-10241-17.03.1999.html -
5Conselho Nacional dos Direitos da Criança e do Adolescente (CONANDA). Resolução No 41 de 17 de outubro de 1995. Os direitos da criança e do adolescente hospitalizada [Internet]. Diário Oficial da União: República Federativa do Brasil; 1995 [cited 2018 Nov 3]. Oct 17, Seção 1: [about 1 screen]. Available from http://www.mpdft.mp.br/portal/pdf/unidades/promotorias/pdij/Legislacao%20e%20Jurisprudencia/Res_41_95_Conanda.pdf
» http://www.mpdft.mp.br/portal/pdf/unidades/promotorias/pdij/Legislacao%20e%20Jurisprudencia/Res_41_95_Conanda.pdf -
6Conselho Federal de Medicina (CFM). Resolução n. 1995, 9 de agosto de 2012. Dispõe sobre as diretivas antecipadas de vontade dos pacientes [Internet]. Diário Oficial da União: República Federativa do Brasil; 2012 [cited 2018 Nov 3]. Aug 31Seção 1: [about 5 screens]. Available from: http://www.portalmedico.org.br/resolucoes/cfm/2012/1995_2012.pdf
» http://www.portalmedico.org.br/resolucoes/cfm/2012/1995_2012.pdf -
7Dadalto L, Tupinambás U, Greco DB. [Advanced directive: a brasilian model]. Rev Bioét [Internet]. 2013 [cited 2017 Oct 20];21(3):463-76. Available from: http://dx.doi.org/10.1590/S1983-80422013000300011 Portuguese.
» http://dx.doi.org/10.1590/S1983-80422013000300011 -
8Mendes KDS, Silveira RCCP, Galvao CM. [Integrative literature review: a research method to incorporate evidence in health care and nursing]. Rev Text Contexto Enferm [Internet]. 2008 [cited 2017 Oct 23];17:758-64. Available from: http://dx.doi.org/10.1590/S0104-07072008000400018 Portuguese.
» http://dx.doi.org/10.1590/S0104-07072008000400018 -
9Piccini CF, Steffani JA, Bonamigo EL, et al. [Living will in the perspective of doctors, lawyers and students]. Rev Bioethikos [Internet]. 2011 [cited 2017 Oct 24];5(4):384-91. Available from: https://saocamilo-sp.br/assets/artigo/bioethikos/89/A4.pdf Portuguese.
» https://saocamilo-sp.br/assets/artigo/bioethikos/89/A4.pdf -
10Campos MO, Bonamigo EL, Steffani JA, et al. [Living wills: perception of oncology patients and accompanying family members]. Rev Bioethikos [Internet]. 2012 [cited 2017 Oct 24];6(3):253-9. Available from: https://saocamilo-sp.br/assets/artigo/bioethikos/96/1.pdf Portuguese.
» https://saocamilo-sp.br/assets/artigo/bioethikos/96/1.pdf -
11Alves CA. [Language, Advance Directives and Living Will: a national and international interface]. Rev Bioethikos [Internet]. 2013 [cited 2017 Oct 24];7(3):259-70. Available from: https://saocamilo-sp.br/assets/artigo/bioethikos/105/1810.pdf Portuguese
» https://saocamilo-sp.br/assets/artigo/bioethikos/105/1810.pdf -
12Crippa A, Buonicore GP, Feijó AGS. [Advance directives of will and the civil responsibility of the Physician]. Rev AMRIGS [Internet]. 2013 [cited 2017 Oct 24];57(4):344-8. Available from: http://www.amrigs.org.br/revista/57-04/0000222859-15_1288_Revista%20AMRIGS.pdf Portuguese
» http://www.amrigs.org.br/revista/57-04/0000222859-15_1288_Revista%20AMRIGS.pdf -
13Bussinguer ECA, Barcellos IA. [The right to live one's own death and its constitutionality]. Rev Ciênc Saúde Colet [Internet]. 2013 [cited 2017 Oct 24];18(9):2691-8. Available from: http://dx.doi.org/10.1590/S1413-81232013000900024 Portuguese
» http://dx.doi.org/10.1590/S1413-81232013000900024 -
14Nunes MI, Anjos MF. [The advance directive: benefits, obstacles and limits]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(2):241-51. Available from: http://dx.doi.org/10.1590/1983-80422014222005 Portuguese.
» http://dx.doi.org/10.1590/1983-80422014222005 -
15Pattela LHD, Alves RGO, Loch JA. [Advanced directives by the patient: a brief introduction to the theme]. Rev AMRIGS [Internet]. 2014 [cited 2017 Oct 24];58(2):162-5. Available from: http://www.amrigs.org.br/revista/58-02/014.pdf Portuguese
» http://www.amrigs.org.br/revista/58-02/014.pdf -
16Kovács MJ. [Towards death with dignity in the XXI Century]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(1):94-104. Available from: http://dx.doi.org/10.1590/S1983-80422014000100011 Portuguese.
» http://dx.doi.org/10.1590/S1983-80422014000100011 -
17Saldanha RR. [The possible failures of the vital will in the brazilian right in front of the constitutional guarantee of the worthy death]. Rev Bioet Latino Am [Internet]. 2014 [cited 2017 Oct 24];14(1):143-68. Available from: http://www.saber.ula.ve/handle/123456789/39041 Portuguese.
» http://www.saber.ula.ve/handle/123456789/39041 -
18Salles AA. [Bioethics and religious processes among terminally ill patients in Brazil]. Rev Bioét [Internet]. 2014 [cited 2017 Oct 24];22(3):397-406. Available from: http://dx.doi.org/10.1590/1983-80422014223021 Portuguese.
» http://dx.doi.org/10.1590/1983-80422014223021 -
19Cogo SB, Lunardi VL. [Anticipated directives will to the terminal patients: integrative review]. Rev Bras Enferm [Internet]. 2015 [cited 2017 Oct 24];68(3):524-34. Available from: http://dx.doi.org/10.1590/0034-7167.2015680321i Portuguese.
» http://dx.doi.org/10.1590/0034-7167.2015680321i -
20Cassol PB, Quintana AM, Velho MTAC. [Anticipated policy will: perception of nursing staff of blood-oncology]. Rev J Nurs Health [Internet]. 2015 [cited 2017 Oct 24];5(1):04-13. Available from: doi: http://dx.doi.org/10.15210/jonah.v5i1.5497 Portuguese.
» http://dx.doi.org/10.15210/jonah.v5i1.5497 -
21Silva JAC, Souza LEA, Costa JLF, et al. Knowledge of medical students regarding living wills. Rev Bioét [Internet]. 2015 [cited 2017 Oct 24];23(3):563-71. Available from: http://dx.doi.org/10.1590/1983-80422015233093
» http://dx.doi.org/10.1590/1983-80422015233093 -
22Chehuen Neto JA, Ferreira RE, Silva NCS, et al. Living will: What do healthcare professionals think about it?. Rev Bioét [Internet]. 2015 [cited 2017 Oct 24];23(3):572-82. Available from: http://dx.doi.org/10.1590/1983-80422015233094
» http://dx.doi.org/10.1590/1983-80422015233094 -
23Cogo SB, Lunardi VL, Quintana AM, et al. Challenges to implementation of advance directives of will in hospital practice. Rev Bras Enferm [Internet]. 2016 [cited 2017 Oct 30];69(6):969-76. Available from: http://www.scielo.br/pdf/reben/v69n6/0034-7167-reben-69-06-1031.pdf
» http://www.scielo.br/pdf/reben/v69n6/0034-7167-reben-69-06-1031.pdf -
24Cogo SB, Lunardi VL, Quintana AM, et al. Advance directives: wills of health professional and Family caregivers. Rev Baiana Enferm [Internet]. 2017 [cited 2017 Oct 30];31(1):e16932. Available from: doi 10.18471/rbe.v31i1.16932
» https://doi.org/10.18471/rbe.v31i1.16932 -
25Moreira MADM, Costa SFG, Cunha MLDM, et al. Physician's perceptions for including living will in medical practice. Rev Bioét [Internet]. 2017 [cited 2017 Nov 18];25(1):168-78. Available from: http://dx.doi.org/10.1590/1983-80422017251178
» http://dx.doi.org/10.1590/1983-80422017251178 -
26Burlá C. A aplicação das diretivas antecipadas de vontade na pessoa com demência [Thesis on the Internet]. Porto: Programa Doutoral em Bioética, Faculdade de Medicina da Universidade do Porto - FMUP/Portugal, Conselho Federal de Medicina -CFM/Brasil. 2015 [cited 2017 Nov 26]. 159 p. Available from: https://repositorio-aberto.up.pt/bitstream/10216/82654/2/114101.pdf
» https://repositorio-aberto.up.pt/bitstream/10216/82654/2/114101.pdf -
27Oliveira MLC, Cavalcanti EO, Alves VP, et al. Euthanasia from the perspective of nursing undergraduate students: concepts and challenges. Rev Min Enferm [Internet]. 2014 [cited 2017 Dec 18];18(1):134-141. Available from: doi: http://www.dx.doi.org/10.5935/1415-2762.20140010
» http://www.dx.doi.org/10.5935/1415-2762.20140010 -
28Nunes R. Proposta sobre suspensão e abstenção de tratamento em doentes terminais. Rev Bioética [Internet]. 2009 [cited 2018 Jan 18];17(1):29-39. Available from: http://revistabioetica.cfm.org.br/index.php/revista_bioetica/article/view/77
» http://revistabioetica.cfm.org.br/index.php/revista_bioetica/article/view/77 -
29Pan Chacon J, Kobata C, Liberman S. A mentira piedosa para o canceroso. Rev Assoc Med Bras. 1995;41(4):274-6.
-
30Menezes RA. Em busca da boa morte: antropologia dos cuidados paliativos. Rio de Janeiro: Garamond; 2004. 228 p.
-
31Asai A FS, Lo B. Attitude of Japanese and Japanese-American physicians towards life sustaining treatment. Lancet [Internet]. 1995 [cited 2018 Jan 21];346(8971):356-9. Available from: doi:https://doi.org/10.5555/uri:pii:S014067369592230X
» https://doi.org/10.5555/uri:pii:S014067369592230X -
32Stone J. Advance directives, autonomy and unintended death. Rev Bioethics [Internet]. 1994 [cited 2018 Jan 23];8(3):223-46. Available from: https://doi.org/10.1111/j.1467-8519.1994.tb00256.x
» https://doi.org/10.1111/j.1467-8519.1994.tb00256.x -
33Beauchamp TL. Princípios de ética biomédica. 3 ed. Rio de Janeiro: Loyola. 2002. 576 p.
-
34Nebot C, Ortega B, Mira J, et al. Dying with dignity. A study of living wills. Gac Sanit. 2010;24(6):437-45. doi:10.1016/j.gaceta.2010.09.006
» https://doi.org/10.1016/j.gaceta.2010.09.006 -
35Pithan LH. A dignidade humana como fundamento jurídico das "ordens de não-ressuscitação". 1 ed. Porto Alegre: EDIPUCRS. 2004. 137 p.
-
36Bento LA. Bioética: Desafios éticos no debate contemporâneo. 1 ed. São Paulo: Paulinas, 2008. 462 p.
-
37Kfouri Neto MI. Testamento Vital. Rev Judic Paraná [Internet]. 2006 [cited 2018 Jan 18];1:201-16. Available from: http://www.revistajudiciaria.com.br/portfolio-posts/revista-judiciaria-do-parana-edicao-02-2/
» http://www.revistajudiciaria.com.br/portfolio-posts/revista-judiciaria-do-parana-edicao-02-2/ -
38Parizotto T. Polêmica: Eutanásia à luz do Direito. Rev Jornal da UEM [Internet]. J Univ Est Maringá [Internet]. 2011 [cited 2018 Jan 28];101:[about 2 screens]. Available from: http://www.jornal.uem.br/2011/index.php/edicoes-2011/87-jornal-101-setembro-2011/759-eutanasia-a-luz-do-direito
» http://www.jornal.uem.br/2011/index.php/edicoes-2011/87-jornal-101-setembro-2011/759-eutanasia-a-luz-do-direito -
39Carvalho GM. Aspectos Jurídicos-penais da Eutanásia. São Paulo: IBCCRIM; 2001. 206 p.
-
40Holland S. Bioética enfoque filosófico. São Paulo: Loyola. 2008. 304 p.
-
41Stolz C, Gehlen G, Bonamigo EL, et al. Manifestation of patient's anticipated will as dysthanasia inhibiting factor. Rev Bioét [Internet]. 2014 [cited 2018 Jan 28];19(3):833-45. Available from: http://revistabioetica.cfm.org.br/index.php/revista_bioetica/article/view/679
» http://revistabioetica.cfm.org.br/index.php/revista_bioetica/article/view/679 -
42Sánchez AV, Villalba SF, Romero PMG, Barragán SG, Rufino Delgado MT, Garcia MTM. Documento de voluntades anticipadas: opinión de los profesionales sanitarios de Atención Primaria. Rev Semergen [Internet]. 2009 [cited 2018 Jan 29];35(3):109-162. Available from: doi:10.1016/S1138-3593(09)70717-8
» https://doi.org/10.1016/S1138-3593(09)70717-8 -
43Gusmão A. [Living will]. Arq CRMPR [Internet]. 2013 [cited 2018 Jan 20];30(118):1-2. Available from: http://crmpr.org.br/publicacoes/cientificas/index.php/arquivos/article/view/437
» http://crmpr.org.br/publicacoes/cientificas/index.php/arquivos/article/view/437 -
44Bomtempo TV. A ortotanásia e o direito de morrer com dignidade: uma análise constitucional. Rev Int Direito Cid [Internet]. 2011 [cited 2018 Jan 22];(9):169-182. Available from: http://www.ipebj.com.br/docdown/_7ce.pdf
» http://www.ipebj.com.br/docdown/_7ce.pdf -
45Schiff R SP, Snook J, Rajkumar C, Bulpitt CJ. Living wills and the mental capacity act: a postal questionnaire survey of UK geriatricians. Age Ageing [Internet]. 2006 [cited 2018 Jan 11];35(2):116-21. Available from: https://doi.org/10.1093/ageing/afj035
» https://doi.org/10.1093/ageing/afj035 -
46Martínez K. The living will. An Sis Sanit Navarra [Internet]. 2007 [cited 2018 Jan 26];30(Suppl 3):87-102. Available from: http://scielo.isciii.es/pdf/asisna/v30s3/original6.pdf
» http://scielo.isciii.es/pdf/asisna/v30s3/original6.pdf
Publication Dates
-
Publication in this collection
Jan-Feb 2019
History
-
Received
26 May 2018 -
Accepted
01 Aug 2018