Abstract
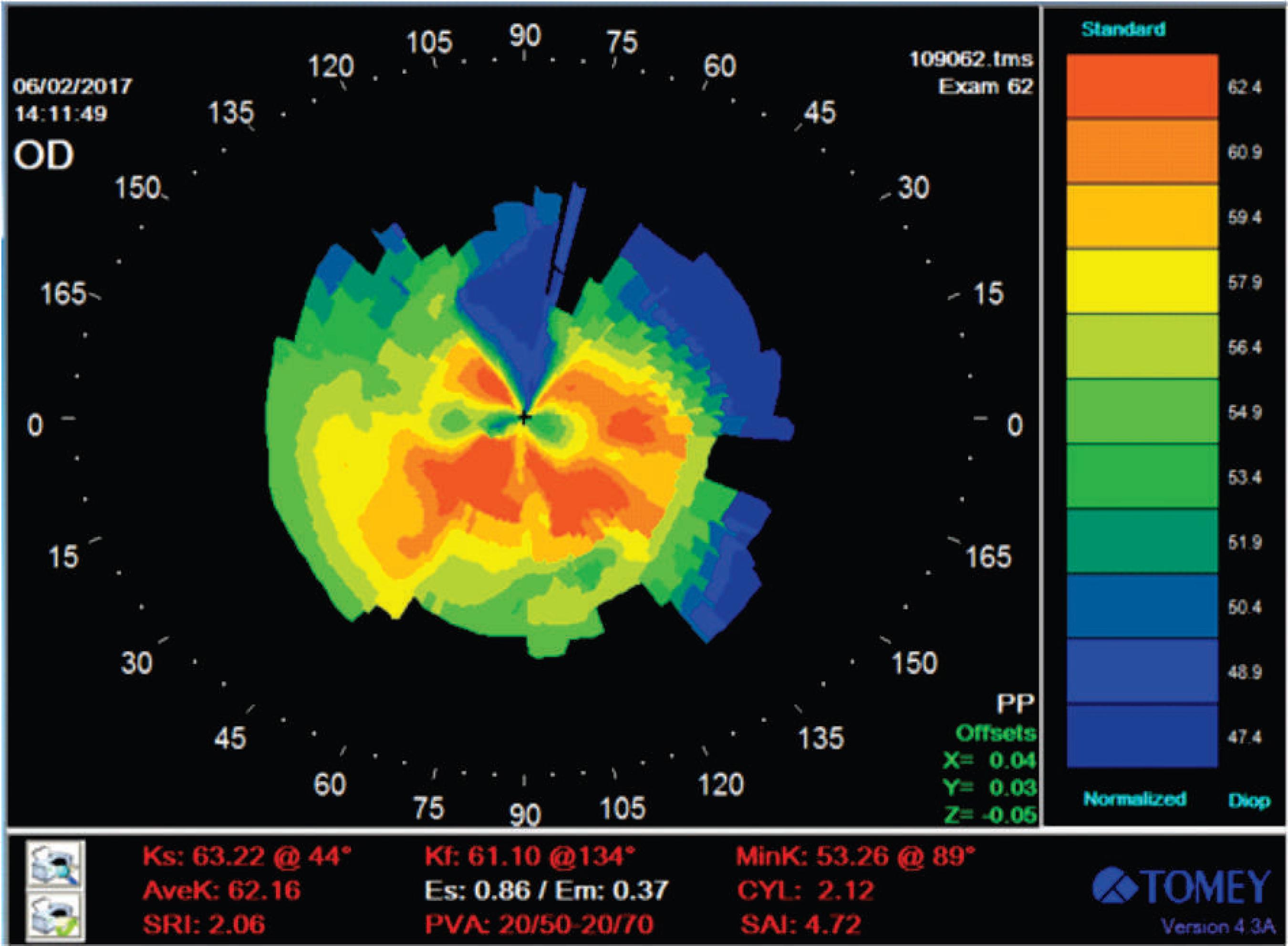
We present a case of a 12-year-old patient with advanced keratoconus in both eyes who received a two-staged treatment in the right eye (OD) to decrease keratoconus progression rate and rehabilitate patient’s vision. At the initial clinical examination, visual acuity without correction in OD was count fingers; cycloplegic refraction was -22.00 - 7,50 x 100° = 20/400; corneal topography demonstrated a curvature of 64.28 x 105° / 55.38 x 15°; and tomography (WaveLight - Allegro Oculyzer) demonstrated a curvature of 68.1 x 114° / 63.3 x 163° Q = -2.67. Initially, the patient received an intrastromal ring segment (210 mm / 200 µm) slightly off center to avoid the thinnest part of the cornea. Six months later a phakic lens was implanted in the anterior chamber. At the follow-up visit 13 months after phakic lens implantation (19 months after ring implantation), visual acuity in OD was 20/20 without correction; cycloplegic refraction was -0.50 -0.75 x 180o = 20/20; and corneal topography showed keratometry of 63.22 x 44o / 61.10 x 134o. The results demonstrated that the associated procedures were successful in decreasing irregular astigmatism and markedly improving patient’s uncorrected visual acuity in OD, postponing the need for corneal transplantation to a more suitable age, if required.
Keywords:
Keratoconus/surgery; Cornea; Implants; Intraocular lenses; Case reports
Resumo
Apresentamos o caso de um paciente de 12 anos de idade com ceratocone avançado em ambos os olhos, que recebeu um tratamento em dois estágios no olho direito (OD) de modo a diminuir a taxa de progressão do ceratocone e reabilitar a visão do paciente. No exame clínico inicial, a acuidade visual sem correção no OD era contar dedos; refração sob cicloplegia era -22.00 - 7,50 x 100° = 20/400; a topografia demonstrou uma curvatura de 64,28 x 105° / 55,38 x 15°; e a tomografia (WaveLight - Allegro Oculyzer) demonstrou uma curvatura de 68,1 x 114° / 63,3 x 163° Q = -2,67. Inicialmente, o paciente recebeu um segmento de anel intraestromal (210 mm /200 µm) ligeiramente fora de centro de modo a evitar a porção mais fina da córnea. Seis meses mais tarde, uma lente fácica foi implantada na câmara anterior. No acompanhamento de 13 meses após a implantação da lente fácica (19 meses após a implantação do anel), OD apresentava uma acuidade visual de 20/20 sem correção; uma refração sob cicloplegia de -0,50 -0,75 x 180o = 20/20; e a topografia da córnea demonstrou ceratometria de 63,22 x 44° / 61,10 x 134°. Os resultados demonstraram que a associação de procedimentos foi bem sucedida na diminuição do astigmatismo irregular, com uma melhora significativa da acuidade visual sem correção no OD, adiando a necessidade de transplante de córnea para uma idade mais adequada, caso necessário.
Descritores:
Ceratocone/cirurgia; Córnea; Implantes; Lentes intraoculares; Relatos de casos
Introduction
Keratoconus is a progressive, noninflammatory disorder which results in the thinning of the corneal stroma, leading to irregular astigmatism, myopia, and corneal protrusion. This condition can result in mild to severe decreased visual acuity. Typically, keratoconus emerges in puberty and progresses until approximately the 4th decade of life, when the rate of progression tend to decrease and may eventually stop. The incidence of keratoconus in the general population is reported to be 1 in 2000. (11 Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: current scenario. Br J Ophthalmol. 2011;95(8):1044-50.)
Clinical signs of keratoconus have been well described, but in its initial stages it may only be detected with corneal topography. (22 Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297-319.) Correction with glasses may be limited by the progressive nature of the corneal irregularity, and the use of rigid contact lenses is usually required. However, contact lenses can also present restrictions due to difficulties with adaptation, discomfort, and sometimes intolerance. (33 Bilgin LK, Yilmaz S, Araz B, Yuksel SB, Sezen T. 30 years of contact lens prescribing for keratoconic patients in Turkey. Cont Lens Anterior Eye. 2009;32(1):16-21.) In cases of severe progressive ectasia, surgical procedures have to be considered. In the last two decades, new surgical techniques for the treatment of keratoconus, such as the implantation of intrastromal ring segments (44 Hamdi IM. Preliminary results of intrastromal corneal ring segment implantation to treat moderate to severe keratoconus. J Cataract Refract Surg. 2011;37(6):1125-32.
5 Barbara R, Barbara A, Naftali M. Depth evaluation of intended vs actual intacs intrastromal ring segments using optical coherence tomography. Eye (Lond). 2016;30(1):102-10.
6 Liu XL, Li PH, Fournie P, Malecaze F. Investigation of the efficiency of intrastromal ring segments with cross-linking using different sequence and timing for keratoconus. Int J Ophthalmol. 2015;8(4):703-8.-77 Lago MA, Ruperez MJ, Monserrat C et al. Patient-specific simulation of the intrastromal ring segment implantation in corneas with keratoconus. J Mech Behav Biomed Mater. 2015;51:260-8.) and corneal collagen crosslinking with riboflavin and ultraviolet light, (88 Elbaz U, Shen C, Lichtinger A, Zauberman NA, Goldich Y, Ziai S, et al. Accelerated versus standard corneal collagen crosslinking combined with same day phototherapeutic keratectomy and single intrastromal ring segment implantation for keratoconus. Br J Ophthalmol. 2015;99(2):155-9.
9 Schuerch K, Tappeiner C, Frueh BE. Analysis of pseudoprogression after corneal cross-linking in children with progressive keratoconus. Acta Ophthalmol. 2016;94(7):e592-e599.
10 Viswanathan D, Kumar NL, Males JJ. Outcome of corneal collagen crosslinking for progressive keratoconus in paediatric patients. Biomed Res Int. 2014;2014:140461.
11 Arora R, Jain P, Goyal JL, Gupta D. Comparative analysis of refractive and topographic changes in early and advanced keratoconic eyes undergoing corneal collagen crosslinking. Cornea. 2013;32(10):1359-64.
12 Sloot F, Soeters N, van der Valk R, Tahzib NG. Effective corneal collagen crosslinking in advanced cases of progressive keratoconus. J Cataract Refract Surg. 2013;39(8):1141-5.
13 Ivarsen A, Hjortdal J. Collagen cross-linking for advanced progressive keratoconus. Cornea. 2013;32(7):903-6.-1414 Arora R, Gupta D, Goyal JL, Jain P. Results of corneal collagen cross-linking in pediatric patients. J Refract Surg. 2012;28(11):759-62.) have been developed as alternative to corneal transplant.
However, in cases of very advanced keratoconus with severe thinning of the cornea and impaired visual acuity, corneal transplant may be the only solution. (11 Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: current scenario. Br J Ophthalmol. 2011;95(8):1044-50.,22 Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297-319.) Unfortunately, in the case of children and young patients, full-thickness corneal transplant has demonstrated a high incidence of rejection. (1515 Gupta PC, Ram J. Results of deep anterior lamellar keratoplasty for advanced keratoconus in children less than 18 years. Am J Ophthalmol. 2016;167:97.) The prognosis of penetrating keratoplasty is limited, and results in children are not as good as they are in adults. (1616 O'Hara MA, Mannis MJ. Pediatric penetrating keratoplasty. Int Ophthalmol Clin. 2013;53(2):59-70.,1717 Huang C, O'Hara M, Mannis MJ. Primary pediatric keratoplasty: indications and outcomes. Cornea. 2009;28(9):1003-8.) Such situation poses a major challenge for surgeons, who need to decide between corneal transplant and its inherent complications, or seek alternative procedures to try to ensure an acceptable level of vision and quality of life until the patient reaches adulthood, when the chances of a successful cornea transplant increases considerably.
We present a case of a young patient with advanced keratoconus in both eyes, who received an off-center intrastromal ring segment in the OD, followed by the implantation of a phakic lens in the anterior chamber, with the objective of decreasing keratoconus progression rate and rehabilitating patient’s vision.
Case Report
A 12-year-old white male with extremely poor visual acuity in both eyes was referred to our clinic for keratoconus treatment. As the left eye presented a very thin cornea (290 µm), as well as striae in the central area, it was decided to address the right eye (OD) first, since it had a more favorable prognosis.
At the initial clinical examination, visual acuity without correction in OD was count fingers. Cycloplegic refraction was -22.00 - 7,50 x 100° = 20/400. Preoperative corneal topography (TMS-4, Tomey) demonstrated a curvature of 64.28 x 105° / 55.38 x 15° (Figure 1). While tomography (WaveLight - Allegro Oculyzer) demonstrated a curvature of 68.1 x 114° / 63.3 x 163° Q = -2.67 (Figure 2). Central pachymetry (WaveLight - Allegro Oculyzer) demonstrated cornea thickness of 415 µm (345 µm in its thinnest part). Specular microscopy (Heron, Wavetek) revealed 2893 cells/mm2.
To avoid the thinnest part of the cornea, an intrastromal ring segment (Ferrara® - Ferrara Ophthalmics) 210 mm /200 µm was implanted slightly out of the habitual 5 mm optical zone ring pathway, with an axis of 110º, tunnel depth of 400 µm, and tunnel length of 250 mm. At the 3-month follow-up examination, the patient presented improved visual acuity and refraction. Cycloplegic refraction was -17.75 +1.75 x 90° OD = 20/50, postoperative topography demonstrated a curvature of 64.66 x 91° / 61.14 x 01° (Figure 3), and tomography showed a curvature of 61.1 x 90° / 58.0 x 180° (Figure 4), indicating that the ectatic cornea was stabilized.
With the improvement of the irregular astigmatism, a second surgical procedure was considered to further improve the patient’s vision in OD. Ultrasound examination showed no retinal degeneration that could predispose the eye to retinal detachment. Optical coherence tomography revealed a normal macula. Specular microscopy measured 2655 cells/mm2, and biometry (IOLMaster) measured the anterior chamber distance at 4.55 mm, with a white-to-white corneal diameter of 13 mm. Six months following the implantation of the intrastromal ring segment, a phakic lens (Artisan® - Ophtec USA, Inc) -19.5 D was implanted in the anterior chamber. At the time of the implantation, a 5.5 mm scleral incision was conducted at 90° to help reduce some of the residual with-the-rule (WTR) astigmatism.
One month following phakic lens implantation, visual acuity had improved to 20/25 without correction. The cycloplegic refraction was -1.00 + 0.75 x 90° = 20/20. At the 13-month follow-up after phakic lens implantation, visual acuity was 20/20 without correction, with refraction of -0.75 + 0.50 x 90° = 20/20. Topography demonstrated keratometry of 63.22 x 44° / 61.10 x 134° (Figure 5), while tomography showed 60.7 x 94.6° / 58.9 x 4.6° (Figure 6).
Discussion
To the best of our knowledge this is the first case of a two-staged approach conducted in a young patient with severe keratoconus, using an off-centered intrastromal ring segment, followed by the implantation of a phakic lens in the anterior chamber. The results demonstrated that the procedures were successful in stabilizing the corneal curvature and reducing the refractive error, markedly improving patient’s uncorrected visual acuity in OD.
More conservative treatments such as the use of glasses or contact lenses may remedy the condition, but usually only for a limited period of time. (1818 Aung YY, McLeod A. Contact lens management of irregular corneas after traumatic aphakia: A pediatric case series. Cont Lens Anterior Eye. 2015;38(5):382-8.) With severe progressive ectasia, surgical procedures must be considered. At this stage, no consensus exists as to which technique should be employed, since none can effectively ensure good visual quality with no further progression of keratoconus. (1818 Aung YY, McLeod A. Contact lens management of irregular corneas after traumatic aphakia: A pediatric case series. Cont Lens Anterior Eye. 2015;38(5):382-8.,1919 Leoni-Mesplie S, Mortemousque B, Touboul D et al. Scalability and severity of keratoconus in children. Am J Ophthalmol. 2012;154(1):56-62.) Thus, each keratoconus case should be analyzed according to its progression, and treatment customized. In some instances, more than one surgical technique or staged surgical techniques should be considered. (1818 Aung YY, McLeod A. Contact lens management of irregular corneas after traumatic aphakia: A pediatric case series. Cont Lens Anterior Eye. 2015;38(5):382-8.)
In cases of advanced keratoconus, such as the one presented here, corneal transplant is the traditionally indicated treatment. (2020 Shi W, Li S, Gao H, Wang T, Xie L. Modified deep lamellar keratoplasty for the treatment of advanced-stage keratoconus with steep curvature. Ophthalmology. 2010;117(2):226-31.
21 Sutton G, Hodge C, McGhee CN. Rapid visual recovery after penetrating keratoplasty for keratoconus. Clin Exp Ophthalmol. 2008;36(8):725-30.-2222 Karadag R, Chan TC, Azari AA, Nagra PK, Hammersmith KM, Rapuano CJ. Survival of primary penetrating keratoplasty in children. Am J Ophthalmol. 2016;171:95-100.) Approximately 12-20% of patients with keratoconus may require a corneal transplant at a relatively young age. (2323 Naacke HG, Borderie VM, Bourcier T, Touzeau O, Moldovan M, Laroche L. Outcome of corneal transplantation rejection. Cornea. 2001; 20(4):350-3.,2424 Ozerturk Y, Sari ES, Kubaloglu A, Koytak A, Pinero D, Akyol S. Comparison of deep anterior lamellar keratoplasty and intrastromal corneal ring segment implantation in advanced keratoconus. J Cataract Refract Surg. 2012;38(2):324-32.) However, in children and young patients with advanced keratoconus, results with corneal transplantation have been unsatisfactory. The prognosis of penetrating keratoplasty in children is, to say the least, reserved, and usually not as good as in adults. (2525 Kusumesh R, Vanathi M. Graft rejection in pediatric penetrating keratoplasty: Clinical features and outcomes. Oman J Ophthalmol. 2015;8(1):33-7.) The main reason for the high rates of donor corneal failure are rejection and infection. Moreover, patients may present a high degree of vision loss due to amblyopia despite a clear donor cornea. (2525 Kusumesh R, Vanathi M. Graft rejection in pediatric penetrating keratoplasty: Clinical features and outcomes. Oman J Ophthalmol. 2015;8(1):33-7.) This is a delicate case of an adolescent who developed severe social dysfunction due to his extremely poor visual acuity. He refused to communicate with anyone other than his mother, which reflected in his school performance and lack of socialization with other children. Waiting until the patient reached adulthood to increase his chances of a successful corneal transplant was unacceptable.
The sequential implantation of intrastromal corneal rings and phakic intraocular lenses has already been shown to be a safe procedure with predictable outcomes. (2626 Ferreira TB, Güell JL, Manero F. Combined intracorneal ring segments and iris-fixated phakic intraocular lens for keratoconus refractive and visual improvement. J Refract Surg. 2014;30(5):336-41.
27 Alfonso JF, Lisa C, Fernández-Vega L, Madrid-Costa D, Poo-López A, Montés-Micó R. Intrastromal corneal ring segments and posterior chamber phakic intraocular lens implantation for keratoconus correction. J Cataract Refract Surg. 2011;37(4):706-13.-2828 Cakir H, Utine CA. Combined Kerarings and Artisan/Artiflex IOLs in Keratectasia. J Refract Surg. 2010 Apr 28:1-8.) In order to regularize the cornea, and decrease the rate of keratoconus progression and corneal astigmatism, an intrastromal ring was implanted in OD. As the central optical zone was too thin (345 µm), an intrastromal ring was implanted slightly off-center. To compensate for the decentralization, a longer ring (210 mm) was chosen. Despite being off-centered, corneal topography showed that astigmatism decreased from 8.90 D to 3.51 D, while the refraction, whose spherical equivalent was -22.12 D preoperatively, decreased to -16.87 D, three months following ring implantation. With a residual refraction of -17.75 + 1.75 x 90o, the right eye achieved 20/50 vision.
To improve the refractive error, a second procedure was performed with the implantation of a phakic lens six months after ring implantation. Due to astigmatism in the greater curvature at the 90o axis, and the lack of any formal contraindication, an Artisan ® lens was chosen. The incision for lens implantation was placed at the 90 degree meridian in order to minimize WTR residual astigmatism. One month after the phakic lens was implanted, visual acuity in the right eye was 20/25 without correction, while refraction was -1.00 +0.75 x 90o = 20/20, with a spherical equivalent of -0.6 D.
These results are in accordance with those found in the literature, which also showed that significant visual and refractive improvement can be obtained with implantation of intrastromal corneal rings and phakic intraocular lenses in patients with different corneal ectatic conditions. (2626 Ferreira TB, Güell JL, Manero F. Combined intracorneal ring segments and iris-fixated phakic intraocular lens for keratoconus refractive and visual improvement. J Refract Surg. 2014;30(5):336-41.
27 Alfonso JF, Lisa C, Fernández-Vega L, Madrid-Costa D, Poo-López A, Montés-Micó R. Intrastromal corneal ring segments and posterior chamber phakic intraocular lens implantation for keratoconus correction. J Cataract Refract Surg. 2011;37(4):706-13.-2828 Cakir H, Utine CA. Combined Kerarings and Artisan/Artiflex IOLs in Keratectasia. J Refract Surg. 2010 Apr 28:1-8.) In a recent study by Ferreira et al., which included 21 eyes of 16 patients, the authors reported a significant mean uncorrected visual acuity improvement from 20/2000 to 20/35 12 months after the combined procedures. (2626 Ferreira TB, Güell JL, Manero F. Combined intracorneal ring segments and iris-fixated phakic intraocular lens for keratoconus refractive and visual improvement. J Refract Surg. 2014;30(5):336-41.)
However, despite the positive outcome, a question remains whether keratoconus will continue to progress despite the presence of the ring. Corneal crosslinking has been shown to decrease and, in some cases, even halt the progression of ectasia. (88 Elbaz U, Shen C, Lichtinger A, Zauberman NA, Goldich Y, Ziai S, et al. Accelerated versus standard corneal collagen crosslinking combined with same day phototherapeutic keratectomy and single intrastromal ring segment implantation for keratoconus. Br J Ophthalmol. 2015;99(2):155-9.
9 Schuerch K, Tappeiner C, Frueh BE. Analysis of pseudoprogression after corneal cross-linking in children with progressive keratoconus. Acta Ophthalmol. 2016;94(7):e592-e599.
10 Viswanathan D, Kumar NL, Males JJ. Outcome of corneal collagen crosslinking for progressive keratoconus in paediatric patients. Biomed Res Int. 2014;2014:140461.
11 Arora R, Jain P, Goyal JL, Gupta D. Comparative analysis of refractive and topographic changes in early and advanced keratoconic eyes undergoing corneal collagen crosslinking. Cornea. 2013;32(10):1359-64.
12 Sloot F, Soeters N, van der Valk R, Tahzib NG. Effective corneal collagen crosslinking in advanced cases of progressive keratoconus. J Cataract Refract Surg. 2013;39(8):1141-5.
13 Ivarsen A, Hjortdal J. Collagen cross-linking for advanced progressive keratoconus. Cornea. 2013;32(7):903-6.-1414 Arora R, Gupta D, Goyal JL, Jain P. Results of corneal collagen cross-linking in pediatric patients. J Refract Surg. 2012;28(11):759-62.) When used in cases diagnosed early, when the patient still has good visual acuity, results have been promising. However, when applied late, when visual impairment is already set, crosslinking can only halt the progression until corneal transplant is deemed safe. (1313 Ivarsen A, Hjortdal J. Collagen cross-linking for advanced progressive keratoconus. Cornea. 2013;32(7):903-6.) After stabilizing the patient’s cornea and improving his vision with the phakic lens, the application of crosslinking in the right eye could be considered. However, as the cornea in OD was excessively thin in the central region, crosslinking may result in the damage and loss of the endothelial cells. (1010 Viswanathan D, Kumar NL, Males JJ. Outcome of corneal collagen crosslinking for progressive keratoconus in paediatric patients. Biomed Res Int. 2014;2014:140461.) We then opted for a more conservative approach with regular follow-ups. If the curvature of the cornea shows signs of progressive ectasia, and corneal thickness allows for a safe treatment, the application of crosslinking may be conducted in the future.
At the follow-up examination performed 13 months after the implantation of the Artisan ® lens, no changes in the cornea curvature or refraction was observed, and the patient had recovered good quality vision in OD, dramatically improving his quality of life and interaction with other people. It is expected that the procedures should suffice until the patient reaches adulthood, at which time the likelihood of cornea transplant complications would decrease considerably. Meanwhile, the patient has been given a chance to lead a normal life. A solution for his left eye is currently underway and should be reported shortly.
-
Institution: Instituto Benjamin Constant, Rio de Janeiro, RJ, Brazil.
Acknowledgements
The authors would like to thank Mr. Antonio Carlos Correa for his assistance in reviewing and translating the text into English.
References
-
1Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: current scenario. Br J Ophthalmol. 2011;95(8):1044-50.
-
2Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297-319.
-
3Bilgin LK, Yilmaz S, Araz B, Yuksel SB, Sezen T. 30 years of contact lens prescribing for keratoconic patients in Turkey. Cont Lens Anterior Eye. 2009;32(1):16-21.
-
4Hamdi IM. Preliminary results of intrastromal corneal ring segment implantation to treat moderate to severe keratoconus. J Cataract Refract Surg. 2011;37(6):1125-32.
-
5Barbara R, Barbara A, Naftali M. Depth evaluation of intended vs actual intacs intrastromal ring segments using optical coherence tomography. Eye (Lond). 2016;30(1):102-10.
-
6Liu XL, Li PH, Fournie P, Malecaze F. Investigation of the efficiency of intrastromal ring segments with cross-linking using different sequence and timing for keratoconus. Int J Ophthalmol. 2015;8(4):703-8.
-
7Lago MA, Ruperez MJ, Monserrat C et al. Patient-specific simulation of the intrastromal ring segment implantation in corneas with keratoconus. J Mech Behav Biomed Mater. 2015;51:260-8.
-
8Elbaz U, Shen C, Lichtinger A, Zauberman NA, Goldich Y, Ziai S, et al. Accelerated versus standard corneal collagen crosslinking combined with same day phototherapeutic keratectomy and single intrastromal ring segment implantation for keratoconus. Br J Ophthalmol. 2015;99(2):155-9.
-
9Schuerch K, Tappeiner C, Frueh BE. Analysis of pseudoprogression after corneal cross-linking in children with progressive keratoconus. Acta Ophthalmol. 2016;94(7):e592-e599.
-
10Viswanathan D, Kumar NL, Males JJ. Outcome of corneal collagen crosslinking for progressive keratoconus in paediatric patients. Biomed Res Int. 2014;2014:140461.
-
11Arora R, Jain P, Goyal JL, Gupta D. Comparative analysis of refractive and topographic changes in early and advanced keratoconic eyes undergoing corneal collagen crosslinking. Cornea. 2013;32(10):1359-64.
-
12Sloot F, Soeters N, van der Valk R, Tahzib NG. Effective corneal collagen crosslinking in advanced cases of progressive keratoconus. J Cataract Refract Surg. 2013;39(8):1141-5.
-
13Ivarsen A, Hjortdal J. Collagen cross-linking for advanced progressive keratoconus. Cornea. 2013;32(7):903-6.
-
14Arora R, Gupta D, Goyal JL, Jain P. Results of corneal collagen cross-linking in pediatric patients. J Refract Surg. 2012;28(11):759-62.
-
15Gupta PC, Ram J. Results of deep anterior lamellar keratoplasty for advanced keratoconus in children less than 18 years. Am J Ophthalmol. 2016;167:97.
-
16O'Hara MA, Mannis MJ. Pediatric penetrating keratoplasty. Int Ophthalmol Clin. 2013;53(2):59-70.
-
17Huang C, O'Hara M, Mannis MJ. Primary pediatric keratoplasty: indications and outcomes. Cornea. 2009;28(9):1003-8.
-
18Aung YY, McLeod A. Contact lens management of irregular corneas after traumatic aphakia: A pediatric case series. Cont Lens Anterior Eye. 2015;38(5):382-8.
-
19Leoni-Mesplie S, Mortemousque B, Touboul D et al. Scalability and severity of keratoconus in children. Am J Ophthalmol. 2012;154(1):56-62.
-
20Shi W, Li S, Gao H, Wang T, Xie L. Modified deep lamellar keratoplasty for the treatment of advanced-stage keratoconus with steep curvature. Ophthalmology. 2010;117(2):226-31.
-
21Sutton G, Hodge C, McGhee CN. Rapid visual recovery after penetrating keratoplasty for keratoconus. Clin Exp Ophthalmol. 2008;36(8):725-30.
-
22Karadag R, Chan TC, Azari AA, Nagra PK, Hammersmith KM, Rapuano CJ. Survival of primary penetrating keratoplasty in children. Am J Ophthalmol. 2016;171:95-100.
-
23Naacke HG, Borderie VM, Bourcier T, Touzeau O, Moldovan M, Laroche L. Outcome of corneal transplantation rejection. Cornea. 2001; 20(4):350-3.
-
24Ozerturk Y, Sari ES, Kubaloglu A, Koytak A, Pinero D, Akyol S. Comparison of deep anterior lamellar keratoplasty and intrastromal corneal ring segment implantation in advanced keratoconus. J Cataract Refract Surg. 2012;38(2):324-32.
-
25Kusumesh R, Vanathi M. Graft rejection in pediatric penetrating keratoplasty: Clinical features and outcomes. Oman J Ophthalmol. 2015;8(1):33-7.
-
26Ferreira TB, Güell JL, Manero F. Combined intracorneal ring segments and iris-fixated phakic intraocular lens for keratoconus refractive and visual improvement. J Refract Surg. 2014;30(5):336-41.
-
27Alfonso JF, Lisa C, Fernández-Vega L, Madrid-Costa D, Poo-López A, Montés-Micó R. Intrastromal corneal ring segments and posterior chamber phakic intraocular lens implantation for keratoconus correction. J Cataract Refract Surg. 2011;37(4):706-13.
-
28Cakir H, Utine CA. Combined Kerarings and Artisan/Artiflex IOLs in Keratectasia. J Refract Surg. 2010 Apr 28:1-8.
Publication Dates
-
Publication in this collection
May-Jun 2018
History
-
Received
04 Oct 2017 -
Accepted
11 Dec 2017