Abstract
Blunt eye trauma can generate a wide range of intraocular lesions that are dependent on the amount of energy the object transfers to the eye during the impact. Lesions of the iris, trabecular meshwork and ciliary body may influence aqueous humor drainage. The cyclodialysis which is characterized by the detachment of ciliary body from the scleral wall, creating a communication between the anterior chamber to supracoroid space, can cause a several reduction of intraocular pressure. This pressure decrease is responsible for the occurrence of hypotonic maculopathy which may induce a severe impact on visual acuity. There is no consensus in the literature about cyclodialysis treatment. In this report, we describe a case of traumatic cyclodialysis after impact with a firearm projectile treated with argon laser photocoagulation.
Keywords:
Ocular hypotension; Eye injuries; Firearms; Vitreous hemorrhage; Ciliary body; Case reports
Resumo
Um traumatismo ocular contuso pode gerar uma vasta gama de lesões intraoculares que são dependentes da quantidade de energia que o objeto transfere ao olho durante o impacto. As lesões da íris, malha trabecular e corpo ciliar podem repercutir na drenagem do humor aquoso. A ocorrência de uma ciclodiálise caracterizada pelo descolamento do corpo ciliar da parede escleral, criando uma comunicação entre a câmara anterior e o espaço supracoroidiano, pode provocar importante redução da pressão intraocular. Esta diminuição pressórica é a responsável pela ocorrência da maculopatia hipotônica que pode cursar com diminuição irreversível da acuidade visual. Não existe consenso na literatura sobre o tratamento das ciclodiálises. Neste relato, descrevemos um caso de ciclodiálise traumática pós impacto com projétil de arma de fogo tratada com aplicação de laser de argônio.
Descritores::
Hipotensão ocular; Traumatismos oculares; Armas de fogo; Hemorragia vítrea; Corpo ciliar; Relatos de casos
Introduction
The severity of blunt eye trauma is dependent on the amount of energy an object transfers to the eye at the time of contact. The etiology of trauma varies according to the study population and the time of the study. Tongu et al. reported that the main causes of blunt eye trauma in Brazil were domestic accidents and physical aggression (32.5%), trauma during the performance of (22.5%) and occupational accidents (12.5%). (11 Tongu MTS, Bison SHD, Souza LB, Scarpi MJ. Aspectos epidemiológicos do traumatismo ocular fechado contuso. Arq Bras Oftalmol. 2001;64(1):57-61.) Balls, stones, punches, impact with airbags during car crashes and elastic cords have already been described as agents causing blunt eye trauma. (22 Scott IU, Greenfield DS, Parrish RK, 2nd. Airbag-associated injury producing cyclodialysis cleft and ocular hypotony. Ophthalmic Surg Lasers. 1996;27(11):955-7.
3 Chaudhry NA, Flynn HW, Jr., Palmberg PF. Elastic cord-induced cyclodialysis cleft and hypotony maculopathy. Ophthalmic Surg Lasers. 1999;30(8):678-80.-44 Gonzalez Martin-Moro J, Munoz-Negrete FJ, Rebolleda G, Lara Medina J, García-Feijoó J. Ultrasonic biomicroscopic findings after spontaneous resolution of a traumatic cyclodialysis. Arch Soc Esp Oftalmol. 2003;78(4):211-4.)
During impact, the ocular globe undergoes rapid circumferential expansion, leading to various lesions ranging from subconjunctival hemorrhages, corneal abrasions or lacerations, to iris lesions, dislocation of the crystalline, traumatic cataract, vitreous hemorrhage, retinal detachment, retinal and/or choroid detachment (55 Kumar M, Kesarwani S. Post-traumatic cyclodialysis cleft with hypotonic maculopathy. Clin Exp Optom. 2011;94(5):481-3.)
The iris lesions are classified according to the site of tissue rupture. In iridodialysis, there is an avulsion of the iris stroma at its base, allowing the visualization of retroiliary ciliary processes by biomicroscopy of the anterior segment. Angular recession is characterized by the rupture between the longitudinal and circular fibers of the ciliary muscle, with a greater exposure of the ciliary band. (66 Sponsel WE, Gray W, Scribbick FW, et al. Blunt eye trauma: empirical histopathologic paintball impact thresholds in fresh mounted porcine eyes. Invest Ophthalmol Vis Sci. 2011;52(8):5157-66.) In cyclodialysis, the avulsion of part of the ciliary body of the scleral wall occurs. This separation creates a communication between the anterior chamber and the supracoroid space, which may cause decreased intraocular pressure. (77 Gonzalez-Martin-Moro J, Contreras-Martin I, Muñoz-Negrete FJ, Gómez-Sanz F, Zarallo-Gallardo J. Cyclodialysis: an update. Int Ophthalmol 2017;37(2):441-57.)
Persistence of pressure values lower than 6 mmHg induce changes in the posterior segment of the eyeball, including optic disc edema, vascular engorgement, retinal and choroidal folds and detachments. Prolonged maintenance of this condition may lead to a permanent decrease in visual acuity.
The treatment of hypotonic maculopathy consists of reversing the cause of decreased intraocular pressure. In cases of cyclodialysis, it is necessary to block the passage of aqueous humor into the supracoroid space. In this report we describe a case of cyclodialysis treated with argon laser photocoagulation with the aid of a gonioscopy lens.
Case Report
A 39-year-old black female living in a community on the outskirts of Rio de Janeiro sought care at the ophthalmology department of Policlínica Ronaldo Gazolla (Universidade Estácio de Sá) due to decreased visual acuity in the right eye. He reports blunt ocular trauma with a firearm projectile (Figure 1A) during sleep at home for 60 days. She was treated at the emergency service, where upper eyelid edema and burn lesion (Figure 1B), mild hyphema and vitreous hemorrhage were detected. She was medicated with timolol maleate 0.5% and dexamethasone 0.1%.
The firearm projectile (A) was found after the trauma, which produced intraocular changes and burn in the upper eyelid of the right eye (B). [Photographic documentation made by the patient]
Two months after the trauma, the patient presented visual acuity of 20/80 in the RE and 20/20 in the left eye (LE). The biomicroscopic examination showed discrete dyscoria in the RE and LE without alterations. The intraocular pressure was 04 mmHg in the RE and 12 mmHg in the LE. The gonioscopy of both eyes, showed the scleral spur in all quadrants, but the RE presented a 2-hour cyclodialysis area in the upper temporal quadrant (Figure 2A). Fundoscopy revealed hypotonic maculopathy with macular folding, peridiscal choroidal rupture area, posterior vitreous detachment with vitreous hemorrhage and optic disc edema (Figure 2B).
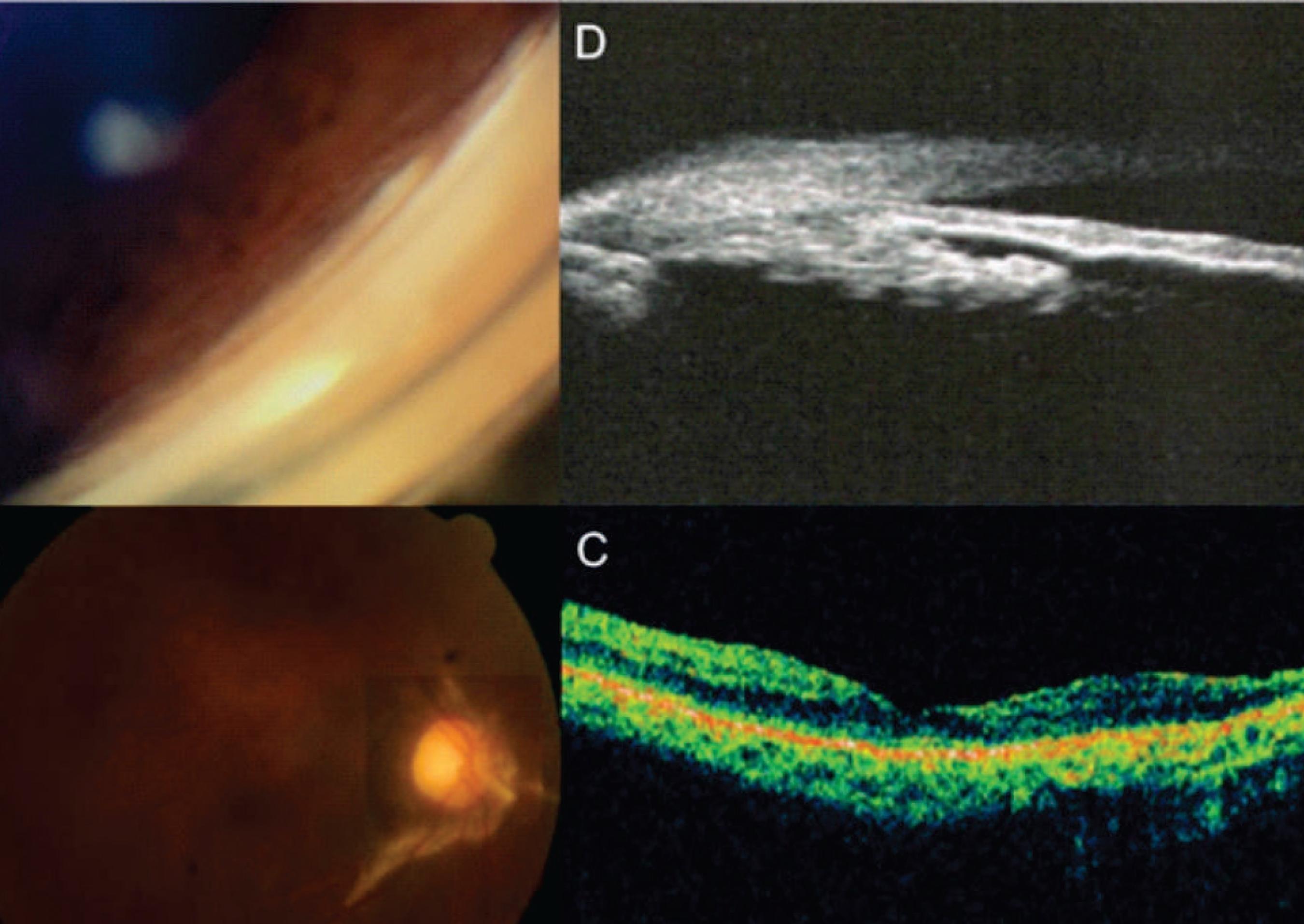
Gonioscopy (A) showing a cyclodialysis area with two hours extension in the upper nasal quadrant. Retinography (B) showing an area of macular folding, papillary edema and peridiscal choroid rupture. Optical coherence tomography (C) of the macular region showing the folding of the deep layers of the retina. Ultrasonic biomicroscopy (D) showing the detachment of the ciliary body (arrow) and the choroidal detachment area (yellow triangle). [Pre-approach complementary examinations]
Ocular ultrasonography was required, which revealed thickening of the retina and choroid, and the macular optic coherence tomography presented folding of the deep layers of the retina (Figure 2C). Ultrasound biomicroscopy was requested and showed a 5-hour ciliocoroidal detachment area and cyclodialysis in the upper temporal quadrant (Figure 2D).
This moment is the onset of atropine 1% eyedrops, and dexamethasone 0.1% and timolol maleate 0.5% eyedrops were withdrawn. After 90 days, the patient returned with visual acuity of 20/400 in the affected eye, IOP of 02 mmHg and worsening of the macular folding. The argon laser application (Purepoint Laser®, Alcon, USA) was used in the slit created by the detachment of the ciliary body with the aid of Goldmann’s gonioscopic lens (Three mirror, Volk Optical Inc., USA). Four sessions were performed with an average of 90 applications, total energy ranging between 700 and 1200 mW, 500μm sighting and duration of 250 msec. There was no increase in pressure during the first 30 days.
Sixty days after the first photocoagulation session, the patient returned with visual acuity of 20/40, subcapsular cataract 1+/4, decreased cyclodialysis slit opening (Figure 3A), and significant reduction of macular folding as evidenced by fundoscopy (Figure 3B) and optical coherence tomography (Figure 3C). Ultrasonic biomicroscopy demonstrated reabsorption of the previous ciliocoroidal detachment (Figure 3D). The patient is having ambulatory follow up.
A reduction of the area of cyclodialysis is observed with gonioscopy (A). Retinographic reconstruction (B) showing resolution of hypotonic maculopathy and peridiscal choroid rupture scar. Optical coherence tomography (C) of the macular region showing the folding regression of the deep layers of the retina. Ultrasonic biomicroscopy (D) not showing pre-existing ciliocoroid detachment. [Pre-approach complementary examinations]
Discussion
Different lesions of the iris may result from blunt eye trauma. Traumatic iritis, iris atrophy, sphincter rupture, angular recession, iridodialysis and cyclodialysis have already been described. The diagnosis of these lesions should be made by careful evaluation of the anterior segment and gonioscopy. In situations with compromised iris insertion in the scleral wall, the indication of a UBM helps elucidating eventual ciliary body detachments.
Post-trauma cyclodialysis can lead to hypotonia regardless of its extent. Its occurrence is due to axial compression and rapid equatorial expansion that distends the ocular tissue leading to the separation of the meridional fibers of the ciliary muscle and its insertion in the wall and in the scleral spur. (88 Murta F, Mitne S, Allemann N, Paranhos Junior A. Direct cyclopexy surgery for post-traumatic cyclodialysis with persistent hypotony: ultrasound biomicroscopic evaluation. Arq Bras Oftalmol. 2014;77(1):50-3.) Communication from the anterior chamber to the supracoroidal space may lead to drainage of aqueous humor through this pathway, culminating in intraocular pressures of less than 6 mmHg.
Hypotonic maculopathy corresponds to a condition in which intraocular pressures of less than 6 mm Hg lead to the occurrence of optic disc edema associated to retinal and choroidal folding in the posterior pole. (99 Costa VP, Arcieri ES. Hypotony maculopathy. Acta Ophthalmol Scand. 2007;85(6):586-97.) This wrinkle is radially centered in the macula and may cause distortion of the sensorineural retina. The treatment of this condition aims at reversing the cause of hypotonia. The prognosis of visual recovery seems to be dependent on the duration of decreased intraocular pressures. (1010 Jampel HD, Pasquale LR, Dibernardo C. Hypotony maculopathy following trabeculectomy with mitomycin C. Arch Ophthalmol. 1992;110(8):1049-50.) Prolonged periods of retinal folding may lead to irreversible fibrosis among these retinal folding during hypotony.
Due to the rarity of the cases, there are no established guidelines for the treatment of post-trauma cyclodialysis. (55 Kumar M, Kesarwani S. Post-traumatic cyclodialysis cleft with hypotonic maculopathy. Clin Exp Optom. 2011;94(5):481-3.) There are several options for approaches described in the literature varying their indication according to the magnitude of the ciliary body detachment, such as surgical cyclopexy, (1111 Kuchle M, Naumann GO. Direct cyclopexy for traumatic cyclodialysis with persisting hypotony. Report in 29 consecutive patients. Ophthalmology. 1995;102(2):322-33.,1212 Agrawal P, Shah P. Long-term outcomes following the surgical repair of traumatic cyclodialysis clefts. Eye (Lond). 2013;27(12):1347-52.) photocoagulation of the argon laser slit, (1313 Han JC, Kwun YK, Cho SH, Kee C. Long-term outcomes of argon laser photocoagulation in small size cyclodialysis cleft. BMC Ophthalmol. 2015;15:123.) pneumocyclopexy associated to cryotherapy, (1414 Ceruti P, Tosi R, Marchini G. Gas tamponade and cyclocryotherapy of a chronic cyclodialysis cleft. Br J Ophthalmol.2009;93(3):414-6.,1515 Pinheiro-Costa J, Melo AB, Carneiro AM, Falcao-Reis F. Cyclodialysis cleft treatment using a minimally invasive technique. Case Rep Ophthalmol. 2015;6(1):66-70.) vitrectomy via pars plana with silicone or gas oil, (1616 Hoerauf H, Roider J, Laqua H. Treatment of traumatic cyclodialysis with vitrectomy, cryotherapy, and gas endotamponade. J Cataract Refract Surg. 1999;25(9):1299-301.) cyclocrytherapy (1717 Krohn J. Cryotherapy in the treatment of cyclodialysis cleft induced hypotony. Acta Ophthalmol Scand. 1997;75(1):96-8.) and facectomy with intraocular lens implant and intracapsular ring. (1818 Gupta S, Sagar P, Gogia V, Khokhar S, Dada T. Dual endotemponade for extensive long-standing cyclodialysis using sulcus-fixated cionni ring and PCIOL. J Glaucoma 2016;25(3):e284-7.)
In the case reported, the patient had a small area of cyclodialysis and did not respond to the initial treatment of suspension of topical corticosteroid use and prescription of atropine. We chose to perform photocoagulation of the slit between the ciliary body and the sclera with argon laser because it is a less invasive treatment than the other options described in the literature. The mechanism by which the laser helps to reduce the slit and interrupt communication with the supracoroidal space remains uncertain. One hypothesis would be that laser application would lead to choroidal edema associated with iritis, thereby closing the slit and disrupting the passage of aqueous humor into supracoroidal space. (1919 Aminlari A, Callahan CE. Medical, laser, and surgical management of inadvertent cyclodialysis cleft with hypotony. Arch Ophthalmol. 2004;122(3):399-404.)
Conclusion
The application of argon laser with the aid of an indirect visualization gonioscopy lens is an effective procedure, with low cost and few risks for the patient, being a good alternative as the initial treatment for small extension cyclodialysis.
References
-
1Tongu MTS, Bison SHD, Souza LB, Scarpi MJ. Aspectos epidemiológicos do traumatismo ocular fechado contuso. Arq Bras Oftalmol. 2001;64(1):57-61.
-
2Scott IU, Greenfield DS, Parrish RK, 2nd. Airbag-associated injury producing cyclodialysis cleft and ocular hypotony. Ophthalmic Surg Lasers. 1996;27(11):955-7.
-
3Chaudhry NA, Flynn HW, Jr., Palmberg PF. Elastic cord-induced cyclodialysis cleft and hypotony maculopathy. Ophthalmic Surg Lasers. 1999;30(8):678-80.
-
4Gonzalez Martin-Moro J, Munoz-Negrete FJ, Rebolleda G, Lara Medina J, García-Feijoó J. Ultrasonic biomicroscopic findings after spontaneous resolution of a traumatic cyclodialysis. Arch Soc Esp Oftalmol. 2003;78(4):211-4.
-
5Kumar M, Kesarwani S. Post-traumatic cyclodialysis cleft with hypotonic maculopathy. Clin Exp Optom. 2011;94(5):481-3.
-
6Sponsel WE, Gray W, Scribbick FW, et al. Blunt eye trauma: empirical histopathologic paintball impact thresholds in fresh mounted porcine eyes. Invest Ophthalmol Vis Sci. 2011;52(8):5157-66.
-
7Gonzalez-Martin-Moro J, Contreras-Martin I, Muñoz-Negrete FJ, Gómez-Sanz F, Zarallo-Gallardo J. Cyclodialysis: an update. Int Ophthalmol 2017;37(2):441-57.
-
8Murta F, Mitne S, Allemann N, Paranhos Junior A. Direct cyclopexy surgery for post-traumatic cyclodialysis with persistent hypotony: ultrasound biomicroscopic evaluation. Arq Bras Oftalmol. 2014;77(1):50-3.
-
9Costa VP, Arcieri ES. Hypotony maculopathy. Acta Ophthalmol Scand. 2007;85(6):586-97.
-
10Jampel HD, Pasquale LR, Dibernardo C. Hypotony maculopathy following trabeculectomy with mitomycin C. Arch Ophthalmol. 1992;110(8):1049-50.
-
11Kuchle M, Naumann GO. Direct cyclopexy for traumatic cyclodialysis with persisting hypotony. Report in 29 consecutive patients. Ophthalmology. 1995;102(2):322-33.
-
12Agrawal P, Shah P. Long-term outcomes following the surgical repair of traumatic cyclodialysis clefts. Eye (Lond). 2013;27(12):1347-52.
-
13Han JC, Kwun YK, Cho SH, Kee C. Long-term outcomes of argon laser photocoagulation in small size cyclodialysis cleft. BMC Ophthalmol. 2015;15:123.
-
14Ceruti P, Tosi R, Marchini G. Gas tamponade and cyclocryotherapy of a chronic cyclodialysis cleft. Br J Ophthalmol.2009;93(3):414-6.
-
15Pinheiro-Costa J, Melo AB, Carneiro AM, Falcao-Reis F. Cyclodialysis cleft treatment using a minimally invasive technique. Case Rep Ophthalmol. 2015;6(1):66-70.
-
16Hoerauf H, Roider J, Laqua H. Treatment of traumatic cyclodialysis with vitrectomy, cryotherapy, and gas endotamponade. J Cataract Refract Surg. 1999;25(9):1299-301.
-
17Krohn J. Cryotherapy in the treatment of cyclodialysis cleft induced hypotony. Acta Ophthalmol Scand. 1997;75(1):96-8.
-
18Gupta S, Sagar P, Gogia V, Khokhar S, Dada T. Dual endotemponade for extensive long-standing cyclodialysis using sulcus-fixated cionni ring and PCIOL. J Glaucoma 2016;25(3):e284-7.
-
19Aminlari A, Callahan CE. Medical, laser, and surgical management of inadvertent cyclodialysis cleft with hypotony. Arch Ophthalmol. 2004;122(3):399-404.
Publication Dates
-
Publication in this collection
May-Jun 2018
History
-
Received
07 Nov 2017 -
Accepted
16 Jan 2018