Abstracts
OBJECTIVE: To assess incidence and predictors of first pregnancy among women with HIV/AIDS. METHODS: Prospective cohort study was conducted in Rio de Janeiro, southeastern Brazil, between 1996 and 2003. This study comprised 225 women with HIV/AIDS followed up until their first pregnancy or first censored event (hysterectomy, tubal ligation, menopause, 50 years of age, loss to follow-up, death or the end of December 2003). Pregnancy and abortion rates were estimated, and Cox proportional hazards models were used to identify baseline characteristics associated with pregnancy risk. RESULTS: The women were followed up for 565 person/years with a median follow-up of 3 years per women. The mean age was 32 years (SD: 7), and 54.7% were white. There were 60 pregnancies in 39 women, and 18 were terminated (induced abortions), accounting for a rate of 6.9% and 2.1% women/year, respectively. Repeated pregnancies occurred in 33.3% of the women (13/39). Higher pregnancy risk was seen among younger women (HR=3.42; 95%CI: 1.69;6.95) and those living with their partners (HR=1.89; 95%CI: 1.00;3.57). Lower pregnancy risk was associated with higher education level (HR=0.43; 95%CI: 0.19;0.99) and use of antiretroviral therapy (HR=061; 95%CI: 0.31;1.17). CONCLUSIONS: Lower pregnancy rates were found in our cohort than in the general population. Sociodemographic characteristics should be taken into consideration in the management of reproductive health in HIV-positive childbearing age women. Reproductive and family planning counseling must be incorporated into HIV/AIDS programs for women to help preventing HIV transmission to their partners and offspring.
HIV Infections; Pregnancy; Risk Factors; Cohort Studies
OBJETIVO: Identificar incidência e preditores incidência da primeira gestação entre mulheres com HIV/Aids. MÉTODOS: Estudo prospectivo de coorte conduzido entre 1996 e 2003 no Rio de Janeiro, RJ, com 225 mulheres acompanhadas até a primeira gestação ou até o primeiro evento considerado censura (histerectomia, ligadura tubárea, menopausa, 50 anos de idade, perda de acompanhamento, óbito ou final de dezembro de 2003). Taxas de incidência de gestação e de aborto foram estimadas e modelos de riscos proporcionais de Cox foram usados para identificar as características da visita de inclusão associadas com o risco de gestação. RESULTADOS: As mulheres foram acompanhadas por 565 pessoas/ano, com média de acompanhamento de 3 anos por mulher. A idade média foi de 32 anos (DP: 7) e 54,7% eram brancas. Sessenta gestações foram observadas em 39 mulheres e 18 resultaram em abortos induzidos (taxas de incidência de 6,9% e 2,1% mulheres/ano, respectivamente). Gestações repetidas ocorreram em 33,3% das mulheres (13/39). Maior risco de gestação foi observado entre mulheres jovens (HR = 3,42; IC95%:1,69;6,95) e entre aquelas vivendo com seus parceiros (HR = 1,89; IC95%:1,00;3,57). Menor risco de gestação esteve associado à maior escolaridade (HR = 0,43; IC95%:0,19;0,99) e ao uso de terapia anti-retroviral (HR = 0,61; IC95%:0,31;1,17). CONCLUSÕES: A incidência de gestação na coorte foi menor se comparada àquela observada na população geral. Características sociodemográficas devem ser consideradas no manejo dos desejos reprodutivos de mulheres HIV-positivas em idade reprodutiva. Os programas de HIV/Aids devem incluir aconselhamento reprodutivo e contraceptivo para prevenir a transmissão do HIV para seus parceiros e prole.
Infecções por HIV; Gravidez; Fatores de Risco; Estudos de Coortes
OBJETIVO: Identificar incidencia y predictores de la primera gestación entre mujeres con VIH/Sida. MÉTODOS: Estudio prospectivo de cohorte conducido en Rio de Janeiro, Sureste de Brasil, entre 1996 y 2003. El estudio incluyó 225 mujeres acompañadas hasta la primera gestación o hasta el primer evento considerado censura (histerectomía, ligadura tubárica, menopausia, 50 años de edad, pérdida de acompañamiento, óbito o final de diciembre de 2003). Se estimaron las tasas de incidencia de gestación y de aborto, y se usaron modelos de riesgos proporcionales de Cox para identificar las características de la visita de inclusión asociadas con el riesgo de gestación. RESULTADOS: Las mujeres fueron acompañadas por 565 persona/años, con promedio de acompañamiento de 3 años por mujer. La edad promedio fue de 32 años (DP:7), y 54,7% eran blancas. Sesenta gestaciones fueron observadas en 39 mujeres y 18 resultaron en abortos inducidos (tasas de incidencia de 6,9% y 2,1% mujeres/año, respectivamente). Las gestaciones repetidas ocurrieron en 33,3% de las mujeres (13/39). Fue observado el mayor riesgo de gestación entre mujeres jóvenes (HR=3,42; IC 95%:1,69;6,95) y entre aquellas que vivían con sus parejas (HR=1,89; IC 95%: 1,00;3,57). El menor riesgo de gestación estuvo asociado a la mayor escolaridad (HR=0,43; IC95%:0,19;0,99) y al uso de terapia antirretroviral (HR=0,61; IC95%:0,31;1,17). CONCLUSIONES: La incidencia de gestación en la cohorte fue menor al compararse con aquella observada en la población general. Características sociodemográficas deben ser consideradas en el manejo de los deseos reproductivos de mujeres VIH-positivas en edad reproductiva. Los programas de VIH/SIDA deben incluir consejos reproductivos y contraceptivos para prevenir la transmisión del VIH para sus parejas y prole.
Infecciones por VIH; Embarazo; Factores de Riesgo; Estudios de Cohortes
ARTIGOS ORIGINAIS
Pregnancy rates and predictors in women with HIV/AIDS in Rio de Janeiro, Southeastern Brazil
Incidência e preditores de gestação em mulheres com HIV/Aids no Rio de Janeiro
Incidencia y predictores de gestación en mujeres con VIH/SIDA en Rio de Janeiro, Sureste de Brasil
Ruth Khalili FriedmanI; Francisco I BastosII; Iuri Costa LeiteIII; Valdiléa G VelosoI; Ronaldo I MoreiraI; Sandra W CardosoI; Ângela C Vasconcelos de AndradeI; Michelle Cristina SampaioI; Judith CurrierIV; Beatriz GrinsztejnI
ILaboratório de Pesquisa em DST/Aids. Instituto de Pesquisa Clínica Evandro Chagas. Fundação Oswaldo Cruz (Fiocruz). Rio de Janeiro, RJ, Brasil
IILaboratório de Informação em Saúde. Instituto de Comunicação e Informação Científica e Tecnológica em Saúde. Fiocruz. Rio de Janeiro, RJ, Brasil
IIIDepartamento de Epidemiologia e Métodos Quantitativos em Saúde. Escola Nacional de Saúde Pública Sérgio Arouca. Fiocruz. Rio de Janeiro, RJ, Brasil
IVCenter for Clinical AIDS Research and Education. David Geffen School of Medicine. University of California. Los Angeles, California, United States
Correspondence Correspondence: Ruth Khalili Friedman Instituto de Pesquisa Clínica Evandro Chagas Fiocruz Laboratório de Pesquisa em DST/Aids Av. Brasil, 4.365 - Manguinhos 21040-900, Rio de Janeiro, Brasil E-mail: ruthkf@fiocruz.br
ABSTRACT
OBJECTIVE: To assess incidence and predictors of first pregnancy among women with HIV/AIDS.
METHODS: Prospective cohort study was conducted in Rio de Janeiro, southeastern Brazil, between 1996 and 2003. This study comprised 225 women with HIV/AIDS followed up until their first pregnancy or first censored event (hysterectomy, tubal ligation, menopause, 50 years of age, loss to follow-up, death or the end of December 2003). Pregnancy and abortion rates were estimated, and Cox proportional hazards models were used to identify baseline characteristics associated with pregnancy risk.
RESULTS: The women were followed up for 565 person/years with a median follow-up of 3 years per women. The mean age was 32 years (SD: 7), and 54.7% were white. There were 60 pregnancies in 39 women, and 18 were terminated (induced abortions), accounting for a rate of 6.9% and 2.1% women/year, respectively. Repeated pregnancies occurred in 33.3% of the women (13/39). Higher pregnancy risk was seen among younger women (HR=3.42; 95%CI: 1.69;6.95) and those living with their partners (HR=1.89; 95%CI: 1.00;3.57). Lower pregnancy risk was associated with higher education level (HR=0.43; 95%CI: 0.19;0.99) and use of antiretroviral therapy (HR=061; 95%CI: 0.31;1.17).
CONCLUSIONS: Lower pregnancy rates were found in our cohort than in the general population. Sociodemographic characteristics should be taken into consideration in the management of reproductive health in HIV-positive childbearing age women. Reproductive and family planning counseling must be incorporated into HIV/AIDS programs for women to help preventing HIV transmission to their partners and offspring.
Descriptors: HIV Infections. Pregnancy. Risk Factors. Cohort Studies.
RESUMO
OBJETIVO: Identificar incidência e preditores incidência da primeira gestação entre mulheres com HIV/Aids.
MÉTODOS: Estudo prospectivo de coorte conduzido entre 1996 e 2003 no Rio de Janeiro, RJ, com 225 mulheres acompanhadas até a primeira gestação ou até o primeiro evento considerado censura (histerectomia, ligadura tubárea, menopausa, 50 anos de idade, perda de acompanhamento, óbito ou final de dezembro de 2003). Taxas de incidência de gestação e de aborto foram estimadas e modelos de riscos proporcionais de Cox foram usados para identificar as características da visita de inclusão associadas com o risco de gestação.
RESULTADOS: As mulheres foram acompanhadas por 565 pessoas/ano, com média de acompanhamento de 3 anos por mulher. A idade média foi de 32 anos (DP: 7) e 54,7% eram brancas. Sessenta gestações foram observadas em 39 mulheres e 18 resultaram em abortos induzidos (taxas de incidência de 6,9% e 2,1% mulheres/ano, respectivamente). Gestações repetidas ocorreram em 33,3% das mulheres (13/39). Maior risco de gestação foi observado entre mulheres jovens (HR = 3,42; IC95%:1,69;6,95) e entre aquelas vivendo com seus parceiros (HR = 1,89; IC95%:1,00;3,57). Menor risco de gestação esteve associado à maior escolaridade (HR = 0,43; IC95%:0,19;0,99) e ao uso de terapia anti-retroviral (HR = 0,61; IC95%:0,31;1,17).
CONCLUSÕES: A incidência de gestação na coorte foi menor se comparada àquela observada na população geral. Características sociodemográficas devem ser consideradas no manejo dos desejos reprodutivos de mulheres HIV-positivas em idade reprodutiva. Os programas de HIV/Aids devem incluir aconselhamento reprodutivo e contraceptivo para prevenir a transmissão do HIV para seus parceiros e prole.
Descritores: Infecções por HIV. Gravidez. Fatores de Risco. Estudos de Coortes.
RESUMEN
OBJETIVO: Identificar incidencia y predictores de la primera gestación entre mujeres con VIH/Sida.
MÉTODOS: Estudio prospectivo de cohorte conducido en Rio de Janeiro, Sureste de Brasil, entre 1996 y 2003. El estudio incluyó 225 mujeres acompañadas hasta la primera gestación o hasta el primer evento considerado censura (histerectomía, ligadura tubárica, menopausia, 50 años de edad, pérdida de acompañamiento, óbito o final de diciembre de 2003). Se estimaron las tasas de incidencia de gestación y de aborto, y se usaron modelos de riesgos proporcionales de Cox para identificar las características de la visita de inclusión asociadas con el riesgo de gestación.
RESULTADOS: Las mujeres fueron acompañadas por 565 persona/años, con promedio de acompañamiento de 3 años por mujer. La edad promedio fue de 32 años (DP:7), y 54,7% eran blancas. Sesenta gestaciones fueron observadas en 39 mujeres y 18 resultaron en abortos inducidos (tasas de incidencia de 6,9% y 2,1% mujeres/año, respectivamente). Las gestaciones repetidas ocurrieron en 33,3% de las mujeres (13/39). Fue observado el mayor riesgo de gestación entre mujeres jóvenes (HR=3,42; IC 95%:1,69;6,95) y entre aquellas que vivían con sus parejas (HR=1,89; IC 95%: 1,00;3,57). El menor riesgo de gestación estuvo asociado a la mayor escolaridad (HR=0,43; IC95%:0,19;0,99) y al uso de terapia antirretroviral (HR=0,61; IC95%:0,31;1,17).
CONCLUSIONES: La incidencia de gestación en la cohorte fue menor al compararse con aquella observada en la población general. Características sociodemográficas deben ser consideradas en el manejo de los deseos reproductivos de mujeres VIH-positivas en edad reproductiva. Los programas de VIH/SIDA deben incluir consejos reproductivos y contraceptivos para prevenir la transmisión del VIH para sus parejas y prole.
Descriptores: Infecciones por VIH. Embarazo. Factores de Riesgo. Estudios de Cohortes.
INTRODUÇÃO
Most women living with HIV/AIDS worldwide are childbearing age.ª a Joint United Ntions Progrm on HIV/AIDS - UNAIDS. Report on the Globl HIV/AIDS Epidemic - 2008 [Internet]. [cited 2008 Jul 31]. Avilble from: http://whqlibdoc.who.int/unaids/2008/9789291737116_eng.pdf HIV infection in women constitutes a major public health issue beyond its direct impact on women's health. Both the risk of mother-to-child transmission (MTCT) of HIV and transmission to uninfected male sexual partners must be considered in any public health program targeting women with HIV/AIDS. This is particularly important in developing countries where most new cases of HIV infections occurª a Joint United Ntions Progrm on HIV/AIDS - UNAIDS. Report on the Globl HIV/AIDS Epidemic - 2008 [Internet]. [cited 2008 Jul 31]. Avilble from: http://whqlibdoc.who.int/unaids/2008/9789291737116_eng.pdf and where deficient health care infrastructure and constrained budgets may jeopardize the implementation of care and prevention programs.b b Joint United Nations Program on HIV/AIDS - UNAIDS. Where prevention and care meet: voluntary counseling and testing and prevention mother-to-child transmission: Report on the Global HIV/AIDS Epidemic. Geneva; 2005.
With the advent of highly active antiretroviral therapy (HAART), the mortality and morbidity associated with HIV infection have been significantly reduced,6,15,21 improving the quality of life of people with HIV/AIDS.14 In addition, treatment with HAART combined with elective cesarean delivery and the use of milk from milk banks or formula instead of breastfeeding can reduce MTCT to less than 2%.17 In settings where these interventions are available, increasing pregnancy rates among women with HIV/AIDS have been reported.5,11 Reproductive choices, especially childbearing, have become a more complex issue in the development of prevention and care programs.
According to the Brazilian Ministry of Health, women accounted for 34.2% of 506,499 AIDS cases reported in mid-2008, and more than 12,000 women with HIV/AIDS give birth each year.c c Ministério da Saúde. Aids em pessoas com 50 anos ou mais de idade. Bol Epidemiol AIDS/DST. 2008;5(1):1-58 Despite a comprehensive care program to people living with HIV/AIDS, including widespread free provision of HAART has been implemented since 1996, there are no data available about pregnancy rate or predictors of pregnancy in women with HIV/AIDS in Brazil.
The present study aimed to estimate pregnancy rate and identify baseline predictors of first pregnancy in women with HIV/AIDS.
METHODS
Data from the Instituto de Pesquisa Clínica Evandro Chagas (IPEC) Cohort of Women Living with HIV/AIDS followed up in Fundação Oswaldo Cruz (FIOCRUZ) Rio de Janeiro, southeastern Brazil, were used. This cohort is an ongoing prospective study of the natural history of HIV infection and related health conditions among women with HIV/AIDS. All women aged 18 or older who were receiving primary HIV care at IPEC HIV/AIDS clinic were invited to participate in this cohort study. The women who agreed to participate and signed an informed consent form were prospectively followed up and underwent gynecological/obstetric and behavioral evaluations. Follow-up visits were completed yearly up to 2003 and every six months since then. At each visit, the participants were interviewed confidentially using a standardized questionnaire to collect information on social and reproductive history and sexual behavior. Drug and alcohol use were also assessed. Counseling on reproductive health, safe sex and risk reduction was provided for all participants during routine visits or additional visits as needed. Women were clinically followed up as recommended by the Brazilian Ministry of Health guidelines and were monitored through CD4+ T-lymphocyte cell counts and gynecological examinations. Medical histories and laboratory results were obtained from medical records. The clinical and laboratorial procedures of this cohort have been detailed elsewhere.10
A total of 402 women with HIV/AIDS were enrolled in the cohort between June 1996 and February 2003.
A prospective analysis of pregnancy among childbearing women with HIV/AIDS at the time of enrollment in the cohort was conducted. Women who were not at risk of getting pregnant were not included in this study: those who were pregnant (n=21), post-menopausal (n=21), hysterectomized (n=13) or sterilized (n=70) at baseline, as well as those aged 50 years or older (n=10). Women who attended only one visit during the monitoring period were also excluded (n=42). The final sample comprised 225 women with HIV/AIDS.
The women were followed up from their admission to this cohort up to the end of December 2003, which allowed women enrolled in late 2002 and in the first two months of 2003 to attend a second follow-up visit.
The outcome of interest was evaluated in every follow-up visit through the following question: "Did you get pregnant in the past six months?". Medical records were reviewed to identify inconsistencies and women with missing cohort visits or lost to follow-up. These women were contacted to clarify inconsistencies.
The following baseline explanatory variables were included in the analysis: age (years), skin color/ethnicity (self-reported), level of education (years), monthly family income (in Brazilian minimum wages), number of living children, marital status, number of lifetime partners, age of sexual initiation, history of sexual abuse, history of domestic violence, history of prior sexually transmitted infections (STIs), alcohol use ("When you drink alcohol, how many drinks do you usually have?"), lifetime illicit drug use (inhaled and injected illicit drugs and other drugs used to get high, either prescription and non-prescription drugs), baseline CD4+ T cell count, use of antiretrovirals at baseline and HIV-related conditions prior to the baseline visit.
Pregnancy and abortion rates were estimated as 100 persons/year (PY). We fitted Cox proportional hazards models to identify factors associated with the risk of a woman getting pregnant. Women who underwent hysterectomy (1.3%) or tubal ligation (8.0%) and who reported menopause (5.7%) after entering the cohort were censored. Observations when women turned 50 (2.2%) and were lost to follow-up (4.0%) or died (6.7%) were also censored. Loss to follow-up was defined as no gynecological follow-up visits after December 2002 or no clinical records in their charts. Women were censored at the time of the occurrence of the first of these events.
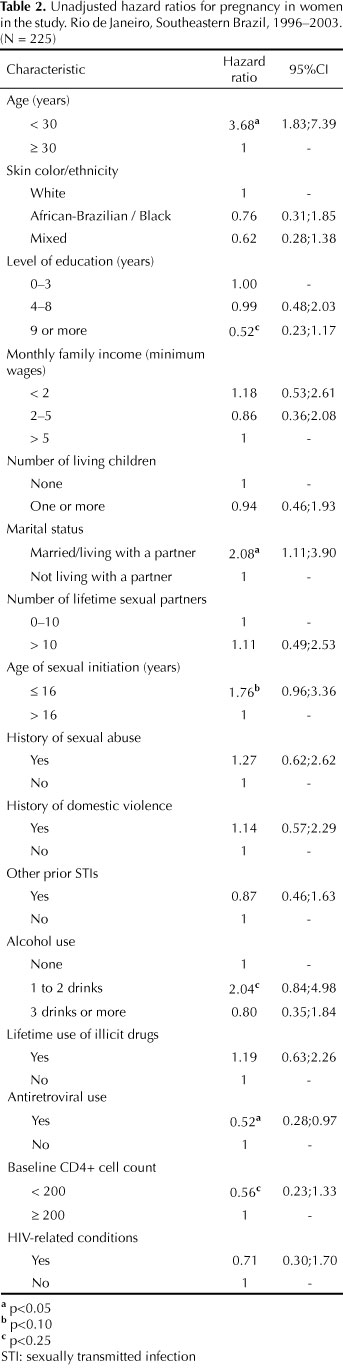
The analysis was performed in two stages. An unadjusted model was fitted and all covariates statistically significant at 25% were selected. In the second stage, a multiple analysis was performed, and the covariates statistically significant at 5% (p-value < 0.05) remained in the model. The variable "use of antiretrovirals" was included in the model, regardless of its statistical significance, as it was our main explanatory variable of interest. The assumption of proportionality in the Cox proportional hazards models was tested by including interactions between the variable "time" and other covariates.1 To validate the final model, an analysis of residuals was conducted. The data were analyzed using SAS.22 The explanatory variables included in the present analysis were assessed at baseline (Table 1).
The study protocol was approved by the Research Ethics Committee of IPEC/FIOCRUZ and all participants signed an informed consent form (Process Nr. 0023.0.009.000-3, 08/12/2003).
RESULTS
The mean age of the women included in the analysis was 32 years (standard deviation [SD]: 7), and 60% were 30 years or older (Table 1). Nearly half of the women were self-reported white (54.7%), and 35.1% reported having no more than three years of education. Overall, 49.1% were employed at baseline, and the majority (75.1%) had a monthly family income of five minimum wages. Less than one-third (30.2%) were married/living with a partner at the time of their enrollment in the cohort, and 76.4% had at least one living child. The proportion of women who reported HIV-infected children was 20.1%.
Almost one-third of the women (32.0 %) reported alcohol use, and 81 (36.0%) reported having used illicit drugs; 8.6% (7/81) reported lifetime use of injected drugs. The mean number of lifetime sexual partners reported at baseline was 9.6 (SD: 19.3; median: 4 partners) and the mean age of sexual initiation was 17.9 years (SD: 3.7). Sexual abuse and domestic violence were reported by 20.9% and 24.4% of the women, respectively. About half of the sample reported history of other STIs.
The average CD4+ T-lymphocyte cell count at baseline was 397 cells/mm3, and 27.6% of the women had counts below 200 cells/mm3. History of opportunistic infection was reported at baseline by about one-fourth (24.0%) of the women.
Approximately 90.0% reported at least one previous pregnancy. The average number of pregnancies was 2.6. The mean age of the first pregnancy was 20.6 years (SD: 5.0). Induced and spontaneous abortion was reported by 41.8% and 25.8% of the women, respectively.
The women were followed for a total of 565 person/years with a median follow-up of 3 years per women. Among the 225 women included in this analysis, 17.0% (n=39) got pregnant at least once after their enrollment in the cohort. Repeated pregnancies were seen in 33.3% (13/39) of the women who became pregnant after the baseline assessment. Overall, 60 pregnancies were recorded for 39 women during the study period. The pregnancy rate in this population during the study period was 6.9% (95% CI 5.2;8.6) women/years of follow-up.
Pregnancy outcome data were available for 58 out of the 60 reported pregnancies; there were 31 (53.4%) deliveries (with one set of twins), 9 (15.5%) spontaneous abortions and 18 (31.0%) induced abortions. The rate of induced abortion was 2.1% (95%CI 1.2%;3.0%) women/years of follow-up. Only one baby was born HIV infected.
Pregnancy was seen in 12.2% of the women who were on antiretroviral therapy (ART) at baseline (n=147) and in 26.9% of those who were ART naive (n=78). Among the women who got pregnant during the follow-up period (n=39), 46.1% were on ART at baseline.
The hazard ratios (HR) and their related confidence intervals (CIs) obtained from the unadjusted Cox proportional hazards models are presented in Table 2. Skin color/ethnicity, monthly family income, number of living children, lifetime number of partners, history of sexual abuse, history of domestic violence, other prior STIs, use of illicit drugs and HIV-related condition did not show a clear association with pregnancy. Age, level of education, marital status, age of sexual initiation, alcohol use, use of antiretrovirals and CD4+ T cell count were associated with the risk of pregnancy at a 25% significance level (p<0.25). These variables were included in the multivariate models.
The results of the adjusted Cox proportional hazards model are shown in Table 3. Age, marital status and level of education were found to be independent predictors of pregnancy. Women under 30 were 2.4 times more likely to become pregnant than those aged 30 or older (HR = 3.42; 95%CI 1.69;6.95). A higher risk of pregnancy was also found among women living with a partner (HR = 1.89; 95%CI 1.00;3.57). In contrast, education showed an inverse relationship with the risk of pregnancy. Women with nine or more years of education had a 57% lower risk of pregnancy than those with up to three years of education (HR = 0.43; 95%CI 0.19;0.99). The risk of pregnancy was 39% lower, although not significantly different (p = 0.11), in women receiving ART compared to those not on therapy (HR = 061; 95%CI 0.31;1.17).
DISCUSSION
The pregnancy rate in our cohort was two-third of that seen in same-age Brazilian women in the general population. However, the rate of induced abortion found suggests that pregnancy was not desired in some cases. The study also showed that younger, less educated, and those women living with their spouses/partners were more likely to become pregnant.
International studies, both in the pre- and post-HAART eras, have reported inconsistent findings regarding reproductive decisions of women with HIV/AIDS.4,7-9,13,24 Data are available for both high- and low-income countries, but to date there is limited data from Brazil, a middle-income country where HAART has been widely available at no cost at the point of delivery since 1996.
In our study we found a pregnancy rate of 6.9% women/year. Based on the number of childbearing women, number of live births corrected for underreporting/delays, number of fetal losses including stillbirths,d d Datasus. Rede Interagencial de Informações em Saúde - RIPSA. Indicadores e dados básicos - Brasil - 2006 [Internet]. [cited 2007 May 16]. Available from: http://tabnet.datasus.gov.br/cgi/idb2006/matriz.htm and number of induced or spontaneous abortionse e Monteiro MFG, Adesse L. Estimativas de aborto induzido no Brasil e Grandes Regiões (1992-2005). In: Anais do 15. Encontro Nacional de Estudos Populacionais - ABEP; 2006; Caxambu, Brasil. p.1-10. for the year 2000, we estimated a pregnancy rate of 10.4 pregnancies per 100 childbearing women in the general Brazilian population. This rate was similar to that reported by Ventura et al in the US.25 The pregnancy rate found in women with HIV/AIDS in our study was 66% of the estimated national rate, reflecting the need of giving special attention to reproductive demands of this population.
The pregnancy rate found in our study was substantially lower than the rate of 12.3% women/year seen in a study carried out among 306 HIV-infected women in Burkina Faso, Sub-Saharan Africa,18 but it is comparable to annual pregnancy rates reported in two US studies. In the first one, a pregnancy rate of 5.5% women/year was found by Blair et al (2004) in a longitudinal study of 8,857 women aged 15 to 44 years followed up from 1992 to 2001.5 In the second one, Massad et al (2004)16 reported an annual pregnancy rate of 7.4% women/year in a cohort of 1,271 HIV-infected women. In all three studies, only childbearing women were considered exposed to the risk at baseline. In Massad et al16 study (2004), all women who had had a hysterectomy, bilateral oophorectomy or tubal sterilization, were 50 years of age or reported no vaginal intercourse for 12 months were censored during follow-up16 - all criteria similar to those used in our study.
Unplanned pregnancy is apparently a major event among HIV-infected women, although contraceptive use seems to increase in the context of treatment roll-out.2 It is difficult to assess in some women when a pregnancy is actually desired or not. The rate of induced abortion was remarkable in our study (31.0%) and was higher than the overall rate of 17.7% in childbearing women reported by Barbosa et al3 (2009) in a study conducted in 13 municipalities in Brazil. They reported a rate of induced abortion in southeast Brazil of 23.1%.It is possible that Rio de Janeiro has contributed to the increase in the region's induced abortion rate.3 In our study, we found an induced abortion rate of 31%, 2.1% women/year. Studies in different backgrounds have found a wide range of induced abortion rates (19%-53%).9,23,24 The abortion rate should be interpreted in the context of a developing country where induced abortion is illegal and its complications are a major cause of death.20
As expected, we found a higher pregnancy risk among women younger than 30, consistent to that reported by Levin et al (2004) in a study of adolescents in the US.12 In fact, younger age proved to be a strong pregnancy predictor, which is corroborated in other studies. 4,5,7,8,13,16
Marital stability was also significantly associated with pregnancy. Women living with their sexual partners were more likely to get pregnant than women who did not. A similar finding was described by Maier et al (2009) between 2005 and 2006 in Uganda.13 Van Benthem et al (2000) also reported lower risk of pregnancy among single women as compared to women in stable marriages.24 In contrast, Massad et al (2004) found that single women had a 60% higher risk of pregnancy than married women (OR 1.59; 95%CI 1.02;2.44).16 Although there are some differences in the modeling strategies used in these three studies, the contrasting results may be suggestive of cultural differences in the communities studied. However, we did not assess in the present study the role of women's partners and reproductive desires of men or women, which may contribute to higher pregnancy rates. The role of men and gender differences must be evaluated by health providers providing care to couples living with HIV/AIDS.
Education level was found to be an important pregnancy predictor in the present study: the higher the level of education, the lower the pregnancy risk. According to the 2000 Brazilian census data, the influence of education level on fertility can be seen nationwide. Women with more years of education have fewer children. Those with eight years or more of education had on average 1.7 children while those with less than four years of education had 3.7 children.f f Instituto Brasileiro de Geografia e Estatística. Censo demográfico. Rio de Janeiro, Brazil; 2000. In the context of Brazil's extreme social heterogeneity, education level plays a significant role in determining negative health outcomes to an extent not observed in the US or Western Europe.
The effect of ART at the time of enrollment in the cohort suggested a lower risk of pregnancy. In a cross-sectional study conducted by Maier et al between 2005 and 2006 in Uganda among 501 HIV-positive women aged 18 to 50 years, ART was significantly associated with reduced odds of pregnancy in the previous three years.13 Massad et al (2004) reported that between 1994 and 2002 the use of non-HAART therapies at the time of inclusion in the cohort was associated with a lower chance of getting pregnant. In their study, only 11 women were on HAART, and no significant associations were found.16 Given that the use of antiretrovirals is associated to more advanced stages of clinical HIV syndrome, the hypothesis that women at advanced stages of disease would be less likely to become pregnant is plausible. In the present study, nonetheless, the univariate analysis did not suggest any significant association between HIV-related manifestations and the risk of pregnancy.
In contrast, Blair et al (2004) found higher pregnancy rates among women on HAART during the previous 6-month interval compared to those on less potent therapeutic regimens.5 This finding suggests that partial reversion of immunodeficiency and improvement in overall health status brought about by antiretroviral therapy may revive reproductive desires among women with HIV/AIDS. The lack of consensus among the studies could be attributed to the way the variable is defined and the stage of disease in the population studied. In our study, and in Massad et al study, antiretroviral use was observed at baseline whereas in Blair et al study it was considered a time-dependent variable. This seems to be the most appropriate method for evaluating this variable given its variability over time and the dynamic of related variables such as CD4+ T-lymphocyte count and viral load.
We did not find a higher risk of pregnancy among women who reported domestic violence and sexual abuse. In Nigeria, Olagbuji et al (2010) described in a cross-sectional study of 502 women both HIV-positive and HIV-negative attending a postnatal clinic a 43.5% prevalence of domestic violence during the 12 months before pregnancy. HIV seropositivity was significantly associated with domestic violence.19 Specific strategies and counseling are needed for women with HIV/AIDS who are victims of domestic violence as they may experience repeated unplanned pregnancies.
Our study has some limitations. As it was based on data from a single center, the results cannot be generalized to other clinical settings or backgrounds in Brazil. However, the characteristics of the study population are comparable to those of women living with AIDS reported to the Brazilian Ministry of Health, which increases their comparability. Women who were using effective contraception were not excluded from this study, although contraception use may have changed over time. Despite data about contraception use in the previous six months was collected in every study visit, the lack of information on start and discontinuation dates did not allow us to take contraception use into account in estimating the pregnancy rate in our cohort. We did not study time-dependent variables, but better understanding baseline characteristics associated with future pregnancy may help the implementation of counseling programs for specific subgroups of women. Although the study ended in December 2003, our results provide an input on future trends in pregnancy and abortion rates, as well as pregnancy predictors in the population studied.
Since sociodemographic factors (age, marital status and level of education) and antiretroviral use are objective measurable variables, further studies are needed to investigate to what degree these variables are associated with and/or are modulated by subjective cultural and psychosocial factors. Family planning and contraceptive counseling must be incorporated into care programs for women with HIV/AIDS with the aim of helping them with their reproductive decisions and preventing HIV transmission to their uninfected partners and offsprings.
ACKNOWLEDGMENTS
We thank all women participating in the IPEC cohort study, Mônica Derrico from Laboratório de Pesquisa em DST/AIDS/Instituto de Pesquisa Clínica Evandro Chagas (FIOCRUZ) for her help in the construction of the baseline database, and Tereza Marques de Oliveira Lima from Universidade Federal Fluminense for her suggestions to this manuscript.
Received: 4/1/2010
Approved: 10/18/2010
Artigo disponível em português e inglês em: www.scielo.br/rsp
This study is part of the research "Coorte de mulheres viviendo com HIV/AIDS: incidência de co-infecções, saúde sexual e reprodutiva", partially funded by the Ford Foundation, Brazil office.
Article based on Friedman RK doctoral thesis submitted to the Sergio Arouca National School of Public Health at Fundação Oswaldo Cruz in 2006.
The authors declare that there are no conflicts of interests.
- 1. Allison PD. Survival analysis using SAS: a practical guide. Cary, NC: SAS Publishing; 1995.
- 2. Andia I, Kaida A, Maier M, Guzman D, Emenyonu N, Pepper L, et al. Highly active antiretroviral therapy and increased use of contraceptives among HIV-positive women during expanding access to antiretroviral therapy in Mbarara, Uganda. Am J Public Health 2009;99(2):340-7. DOI:10.2105/AJPH.2007.129528
- 3. Barbosa RM, Pinho AA, Santos NS, Filipe E, Villela W, Aidar T. Aborto induzido entre mulheres em idade reprodutiva vivendo e não vivendo com HIV/aids no Brasil. Cienc Saude Coletiva 2009;14(4):1085-99. DOI:10.1590/S1413-81232009000400015
- 4. Bedimo AL, Bessinger R, Kissinger P. Reproductive choices among HIV-positive women. Soc Sci Med 1998;46(2):171-9. DOI:10.1016/S0277-9536(97)00157-3
- 5. Blair JM, Hanson DL, Jones JL, Dworkin MS. Trends in pregnancy rates among women with human immunodeficiency virus. Obstet Gynecol 2004;103(4):663-8. DOI:10.1097/01.AOG.0000117083.33239.b5
- 6. Campos DP, Ribeiro SR, Grinsztejn B, Veloso VG, Valente JG, Bastos FI, et al. Survival of AIDS patients using two case definitions, Rio de Janeiro, Brazil, 1986-2003. AIDS 2005;19 (Suppl 4):S22-6.
- 7. Chu SY, Hanson DL, Jones JL. Pregnancy rates among women infected with human immunodeficiency virus. Adult/Adolescent HIV Spectrum of Disease Project Group. Obstet Gynecol 1996;87(2):195-8.
- 8. De Vincenzi I, Jadand C, Couturier E, Brunet JB, Gallais H, Gastaut JA, et al. Pregnancy and contraception in a French cohort of HIV-infected women. SEROCO Study Group. AIDS 1997;11(3):333-8.
- 9. Gray RH, Wawer MJ, Serwadda D, Sewankambo N, Li C, Wabwire-Mangen F, et al. Population-based study of fertility in women with HIV-1 infection in Uganda. Lancet 1998;351(9096):98-103. DOI:10.1016/S0140-6736(97)09381-1
- 10. Grinsztejn B, Bastos FI, Veloso VG, Friedman RK, Pilotto JH, Schechter M, et al. Assessing sexually transmitted infections in a cohort of women living with HIV/AIDS, in Rio de Janeiro, Brazil. Int J STD AIDS 2006;17(7):473-8. DOI:10.1258/095646206777689071
- 11. Kaida A, Lima VD, Andia I, Kabakyenga J, Mbabazi P, Emenyonu N, et al. The WHOMEN's scale (Women's HAART Optimism Monitoring and EvaluatioN Scale v.1) and the association with fertility intentions and sexual behaviours among HIV-positive women in Uganda. AIDS Behav 2009;13(Suppl 1):72-81. DOI:10.1007/s10461-009-9553-y
- 12. Levin L, Henry-Reid L, Murphy DA, Peralta L, Sarr M, Ma Y, et al. Incident pregnancy rates in HIV infected and HIV uninfected at-risk adolescents. J Adolesc Health 2001;29(3 Suppl):101-8.
- 13. Maier M, Andia I,Emenyonu N, Guzman D, Kaida A, Pepper L, et al.. Antiretroviral therapy is associated with increased fertility desire, but not pregnancy or live birth, among HIV+ women in an early HIV treatment program in rural Uganda. AIDS Behav 2009;13(Suppl 1)s:28-37.DOI:10.1007/s10461-008-9371-7
- 14. Mannheimer SB, Matts J, Telzak E, Chesney M, Child C, Wu AW, et al. Quality of life in HIV-infected individuals receiving antiretroviral therapy is related to adherence. AIDS Care 2005;17(1):10-22.
- 15. Marins JR, Jamal LF, Chen SY, Barros MB, Hudes ES, Barbosa AA, et al. Dramatic improvement in survival among adult Brazilian AIDS patients. AIDS 2003;17(11):1675-82. DOI:10.1097/01.aids.0000072649.21517.80
- 16. Massad LS, Springer G, Jacobson L, Watts H, Anastos K, Korn A, et al. Pregnancy rates and predictors of conception, miscarriage and abortion in US women with HIV. AIDS 2004;18(2):281-6.
- 17. Mofenson LM. Advances in the prevention of vertical transmission of human immunodeficiency virus. Semin Pediatr Infect Dis 2003;14(4):295-308. DOI:10.1053/j.spid.2003.09.003
- 18. Nebié Y, Meda N, Leroy V, Mandelbrot L, Yaro S, Sombié I, et al. Sexual and reproductive life of women informed of their HIV seropositivity: a prospective cohort study in Burkina Faso. J Acquir Immune Defic Syndr 2001;28(4):367-72.
- 19. Olagbuji B, Ezeanochie M, Ande A, Ekaete E. Trends and determinants of pregnancy-related domestic violence in a referral center in southern Nigeria. Int J Gynaecol Obstet. 2010;108(2):101-3. DOI:10.1016/j.ijgo.2009.09.024
- 20. Olinto MTA, Moreira-Filho DC. Fatores de risco e preditores para o aborto induzido: estudo de base populacional. Cad Saude Publica 2006;22(2):365-75. DOI:10.1590/S0102-311X2006000200014
- 21. Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med 1998;338(13):853-60. DOI:10.1056/NEJM199803263381301
-
22SAS Online Doc 9.1.3 (USA). Cary, NC; SAS Institute; c2002-2005.
- 23. Thackway SV, Furner V, Mijch A, Cooper DA, Holland D, Martinez P, et al. Fertility and reproductive choice in women with HIV-1 infection. AIDS; 1997;11(5): 663-7.
- 24. Van Benthem BH, de Vincenzi I, Delmas MC, Larsen C, van den Hoek A, Prins M. Pregnancies before and after HIV diagnosis in an European cohort of HIV-infected women. European Study on the Natural History of HIV Infection in Women. AIDS 2000;14(14):2171-8.
- 25. Ventura SJ, Abma JC, Mosher WD, Henshaw S. Estimated pregnancy rates for the United States, 1990-2000: an update. Natl Vital Stat Rep 2004;52(23):1-9.
Publication Dates
-
Publication in this collection
04 Mar 2011 -
Date of issue
Apr 2011
History
-
Received
04 Jan 2010 -
Accepted
2010